Age Changes In The Oral Cavity And Teeth
Ageing is a progressive, generalized impairment of function resulting in loss of adaptive response to stress. It occurs due to of accumulation of changes in the body with time. It occurs at various levels: Molecular, cellular, physiological, morphological and chronological.
Table of Contents
The oro-dental structures undergo age related regressive alterations which have an impact on an individual’s physical, psychological and social well-being. These agerelated changes in the oral cavity and teeth are to be recognized by the dental professional in order to differentiate the pathologic conditions versus the normal findings that are consistent with ageing.
Read And Learn More: Oral Histology Notes
Theories Of Ageing
Several theories have been proposed to explain the biological basis of ageing.
These Include:
- Immune theory
- Neuroendocrine theory
- Cell ageing theory
- Somatic mutation theory
- Error theory
- Wear and tear theory
- Free radical theory (most accepted theory)
According to the free radical theory:
- Ageing occurs due to the damage caused by the free radicals.
- The antioxidants in the body are not able to neutralize the free radicals which are continuously generated during the life cycle of the cell resulting in cell and tissue damage leading to ageing.
Age Changes In The Oro-Dental Tissues
The maxillofacial complex undergoes a gradation of changes from birth through age to old age.
Facial changes:
- Facial ageing is a dynamic process involving the ageing of soft tissue and bony structures with bone loss in specific areas of the facial skeleton contributing significantly to the features of the ageing face.
- As a human being gets older the natural ageing process involves the following:
- Decrease in collagen production (leads to increased laxity of the skin)
- Decrease in elastin production (leads to inelasticity of the skin).
- Disappearance of fat cells (leads to sagging of the skin).
- Decrease in the tendency of the skin to retain moisture.
- Appearance of frown lines due to small muscle contractions.
- Retention of dead skin cells.
- Lesser turnover of new skin cells.
- Overall decrease in the height and volume of the maxilla and mandible due to the loss of teeth and resorption of bone.
- Loss of normal intermaxillary space could also arise due to abnormal wear of teeth or failure to restore lost dental structures and may place undue stress on the temporomandibular joints resulting in joint dysfunction.
- There is reduction in the ramus height, mandibular body height and length, increase in the bigonial distance and surfacing of the mental foramen near the alveolar bone that occurs as age advances.
- Other changes include protrusion of the chin and wrinkles extending from the corner of the mouth to the angle of the mandible.
Oral changes:
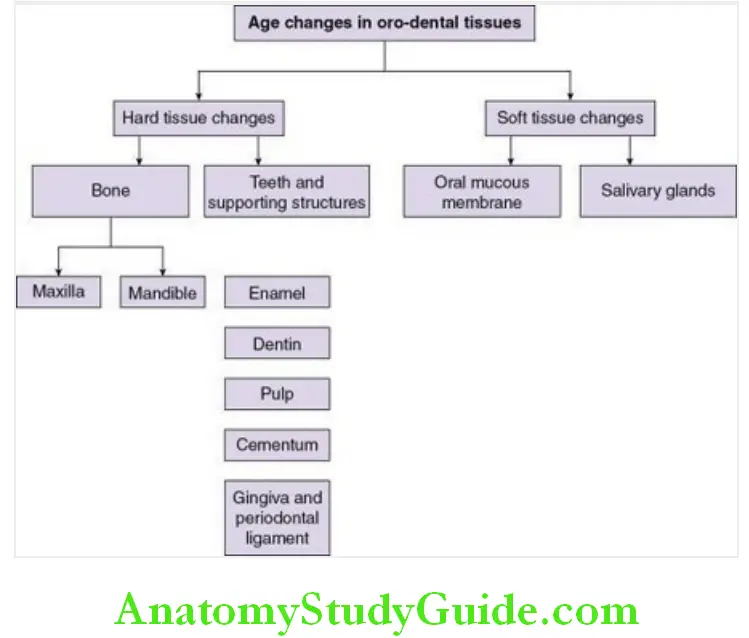
Age changes in the oral cavity occur in hard tissues (teeth, alveolar bone) and soft tissues (oral mucous membrane, salivary glands). The hard and soft tissues of the teeth and its supporting structures are subjected to constant change. These changes can be observed under the microscope or macroscopically.
Age changes in the oro-dental tissues:
Enamel:
- Alteration in the natural smooth contour of the enamel. Appearance of wear facets on the occlusal surfaces of teeth which may further deepen to affect the dentin
- Enamel becomes less calcified on the surface, teeth may become darker and become more resistant to decay.
- There is increase in the size of the hydroxyapatite crystals due to ions acquired from oral fluids and a decrease in pore size between them due to which there is a reduction in the permeability of enamel to fluids.
Dentin:
- Reparative dentin (tertiary dentin or reactive dentin) formation occurs in response to extensive abrasion and caries. This reparative dentin is characterized as having fewer and more twisted tubules than normal dentin.
- Few hydroxyapatite crystals are seen in a dentinal tubule initially but the tubule is eventually occluded with a fine meshwork of crystals. The refractive indices of peritubular and intertubular dentin are equalized and teeth appear transparent. Dentinal sclerosis reduces the permeability of dentin and may help prolong pulp vitality.
Pulp:
- Decrease in the cellular elements with a decrease in size and number of cytoplasmic organelles is seen.
- Fibroblasts in the ageing pulp exhibit less perinuclear cytoplasm and possess long, thin cytoplasmic processes. A gradual increase in the diffuse fibrillar components and bundles of collagen fibres happens gradually, thereby resulting in decrease in the size of the pulp.
- Atherosclerotic plaques within and calcifications may be seen around the pulpal vessels occur with a gradual reduction in the blood flow.
- Pulp stones (denticles) are nodular calcified masses that may be free, attached or embedded with the adjacent dentin. They are structurally similar to dentin and begin to form as small nodules but increase in size by incremental growth on their surface. These denticles may eventually fill substantial parts of the pulp chamber.
Cementum:
- Surface irregularities and an increase in the width of the cementum by 5–10 times occurs in the apical and lingual regions with increasing age.
Gingiva:
- The epithelium of the gingiva gets thinner and less keratinized.
- The connective tissue becomes coarser and denser. There is an increase in the rate of conversion of soluble to insoluble collagen, increase in the strength and stability of collagen due to changes in the macromolecules.
Periodontal ligament:
- Decrease in fibroblast population
- Decreased organic matrix production
- Epithelial cell rests are seen.
- Increased amounts of elastic fibres.
Alveolar bone:
- The surface of the bone becomes irregular.
- Irregular insertion of collagen fibres.
Maxillary sinus:
- The maxillary sinus enlarges with the growing maxilla; it becomes fully developed following the eruption of the permanent dentition.
- In adults, the vertical dimension of the sinus is greatest, reflecting the development of the alveolar processes with the teeth, resulting in enlargement of the sinus.
- When teeth are lost, the sinus reverts to its infantile shape with a decrease in the height.
- Pneumatization of the sinus occurs with tooth loss and may encroach onto the adjacent maxillary alveolar bone.
Temporomandibular joint (TMJ):
- Degenerative changes of the mandibular condyle and articular eminence flattening may occur due to the ageing process.
- There may be displacement of the articular disc due to chronic use of the joint and hence the retrodiscal tissues may eventually take up the function of an articular disc.
- Laxity of the temporomandibular joint ligaments with age leads to joint hypermobility.
Oral mucous membrane:
- Reduction in the thickness of the epithelium and decrease in the salivary secretions leads to the oral mucosa becoming smooth, wax-like and dry.
- The filiform papilla becomes reduced and the tongue appears smooth.
- Nutritional deficiencies may also be a contributing factor.
- Dilated veins may be noted on the ventral aspect of the tongue which are termed as lingual varices.
Salivary glands:
Age changes with the parotid glands includes gradual replacement of the parenchyma with fatty tissue. This results in significant reduction in serous saliva thus contributing to increase in the viscosity of saliva and oral dryness in the elderly.
Clinical Considerations Age Changes Of The Oral Cavity And Teeth
Teeth and supporting structures:
- Attrition is the physiological wearing away of tooth as a result of tooth to tooth contact and occurs on the occlusal, incisal and proximal surfaces of the teeth. It appears as a small or large well- polished facet on the cusp tip or as a flattening of an incisal edge of teeth.
- Severe cases of attrition, in which the enamel is completely worn away in one or more areas result in an extrinsic yellow or brown staining of the exposed dentin due to food substances.
- Dentinal sclerosis (transparent dentin) is characterized by the calcification of dentinal tubules which decreases the conductivity of odontoblastic processes thus preventing dentinal hypersensitivity and also slows down the advancing carious process.
- Pulp stones may impinge on nerves of the pulp resulting in pain that may range from mild pulpal neuralgia to severe excruciating pain. Difficulty may be encountered in extirpating the pulp during root canal treatment if such calcifications are present.
- Apical migration of the junctional epithelium of the gingiva occurs with accompanying gingival recession.
- This migration of the junctional epithelium could be due to the eruption of the tooth through the gingiva to maintain occlusal contact with the opposing tooth (passive eruption) due to the loss of the tooth surface due to attrition.
- Gingival recession also occurs due to cumulative effects of inflammation on the periodontium.
Periodontal inflammation results in resorption of the alveolar process that occurs in episodic spurts in both horizontal and vertical manner. - Maxillary implant placement may require a sinus lift procedure in cases where the maxillary sinus pneumatization is extensive and has involved the adjacent alveolar bone.
- Failure to replace the edentulous areas in the oral cavity with artificial dentures may result in undue stress on the temporomandibular joint.
- Chronic low grade stresses initiate degenerative changes in the bony components of the joint and pain.
Oral soft tissues:
- There is thinning of the oral mucosal epithelium and hence lack of protective keratinized cells which render an oral environment susceptible to mechanical, chemical and microbial irritation.
- Oral mucosa in the elderly is thin and delicate and may be damaged by coarse foods and ill-fitting prosthetic appliances. The epithelium may tear and expose the connective tissue which heals at a slower rate.
- Atrophy of the underlying connective tissue results in loss of resilience and elasticity of oral tissues which may contribute to further difficulties in denture retention.
- Decrease in the salivary flow makes the oral mucosa dry and inelastic causing burning sensation and altered taste sensation (hypogeusia).
- The loss of normal cleansing and protective action of saliva renders the tissues more susceptible to infection.
- Burning and painful tongue (glossopyrosis and glossodynia) may also be reported by some individuals.
- Decrease in the flow of saliva also decreases denture retention. The small, solitary mucous glands of the palate, cheeks and lips secrete a thick, ropy saliva with a high mucin content which also makes denture retention difficult.
Oral changes in an edentulous patient:
Removable partial dentures and complete dentures are the most commonly used artificial prosthesis by elderly individuals. These artificial dental prostheses may result in some changes in the oral cavity. The prosthesis may be ill-fitting, poorly fabricated or a worn out one that may induce certain oral changes or the changes may be secondary to the altered oral environment in older individuals.
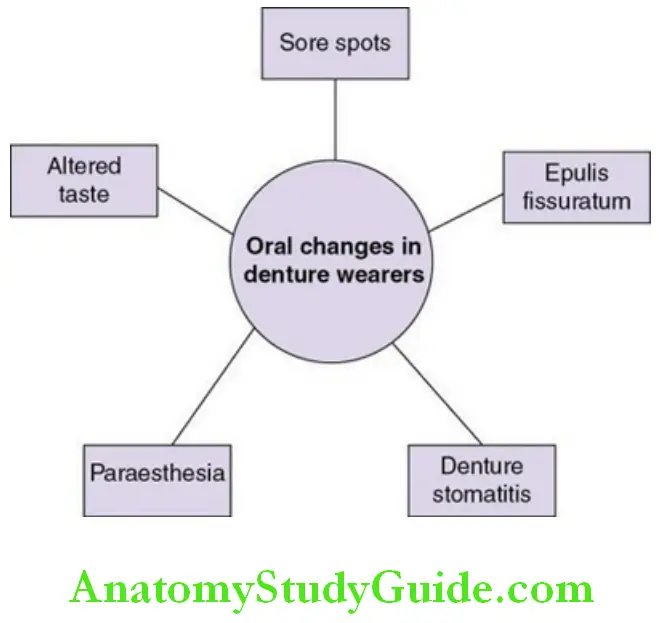
The following changes may be noted:
- Immediately following the insertion of a newly fabricated denture, ‘sore spots’ may develop at areas of excessive pressure when the denture is in position or where the tissues are traumatized during its insertion.
- Chronic irritation from abnormal pressure of the denture flanges on the tissues bounding the buccal sulci may result in varying degrees of tissue hypertrophy and hyperplasia termed as ‘epulis fissuratum or denture flange hyperplasia’ which interferes with the retention and ultimate function of the dentures.
- Oedema, inflammation of the mucoperiosteum and swelling of the minor salivary glandular elements may develop in tissues covered by maxillary dentures. Wearing the denture for years without proper maintenance and ‘round the clock’ wearing are important factors in the causation of these lesions.
- Such lesions are termed as inflammatory papillary hyperplasia and may give a classical ‘over ripened berry appearance’.
- Paraesthesia developing immediately after insertion of newly constructed dentures may be related to errors in impression making or fabrication of the denture base.
- It is not uncommon for individuals to complain of numbness of the mucous membrane and skin of the chin.
- This occurs as a result of undue pressure of the denture on the mental nerves and vessels as they emerge from the mental foramen that has assumed a more occlusal position in an aged mandible.
- Poorly maintained ill-fitting dentures, continuous wearing of dentures at night times may result in candidal colonization and infection termed as ‘denture stomatitis’.
- Old and worn out dentures may exhibit flattened teeth and stained surfaces which may also pose an aesthetic concern.
Age Changes In The Oral Cavity And Teeth Synopsis
- Ageing is a progressive, generalized impairment of function resulting in loss of adaptive response to stress. It occurs at various levels: Molecular, cellular, physiological, morphological and chronological.
- The oro-dental structures also undergo age-related regressive alterations which have an impact on an individual’s physical, psychological and social well-being.
- The free radical theory is the most accepted theory for ageing.
- Facial ageing is a dynamic process involving the ageing of soft tissue and bony structures.
- Alteration in the dentition and resorption of bone of the maxillary and the mandibular arch may result in an overall loss of height and volume.
- With advancing age, the enamel shows alteration in the natural smooth contour; appearance of wear facets on the surfaces of teeth may be seen.
- Reparative dentin (tertiary dentin or reactive dentin) formation occurs in response to extensive abrasion. Pulp stones (denticles) are formed as the pulp tissues become older.
- There is thinning and decreased keratinization of the gingival epithelium.
- Oral mucous membrane exhibits reduction in the thickness of the epithelium and the salivary gland parenchyma is replaced by fatty tissue due to which there is inadequate lubrication of the oral tissues.
- Oral changes in a denture wearer include sore spots, denture flange hyperplasia and candida induced oral lesions.
Leave a Reply