Alveolar Bone Oral Histology Notes
Alveolar Bone
Bone is a mineralized connective tissue which is one of the hardest structures in the body and makes up the body’s skeleton.
Table of Contents
- It possesses a certain level of elasticity and toughness.
- It gives shape and support to the body.
- It provides attachment to muscles and tendons.
- It stores minerals and contains the marrow spaces where the blood cells are formed and stored
Read And Learn More: Oral Histology Notes
Bone Classification
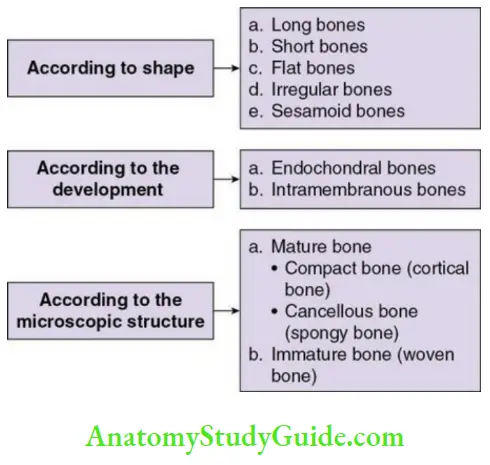
Bone Composition
The bone matrix comprises
- Inorganic material: 65%
- Organic material: 25%
- Water: 15%
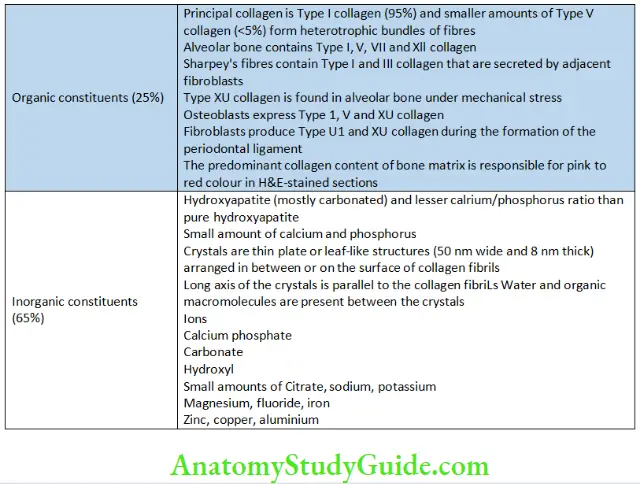
Organic And Organic Constituents Of Bone
About 10% of the organic matrix is noncollagenous proteins.
- Most of them are endogenously derived from bone cells and blood (albumin, globulin) which get incorporated into the bone during bone formation.
- Important noncollagenous proteins are osteocalcin, osteopontin, osteonectin and bone sialoprotein.
- Proteoglycans found are biglycan and decorin.
- Bone also contains bone morphogenic proteins, growth factors like platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), and insulin-like growth factor.
Organic and Inorganic Constituents of Bone
Histology Of Bone
The unmineralized bone matrix on the surface of the bone where active bone formation is still occurring is called osteoid.
- Thickness: 5–10 microns before mineralization begins.
- It contains Type I collagen fibres arranged parallel to the surface of the bone. The fibres are embedded in ground substances containing proteoglycans, glycoproteins and proteins.
Adult bones
The dense outer sheet is called compact bone, and a medullary cavity is in the centre. The cavity contains yellow or red bone marrow. The cavity has a rich network of bony trabeculae. This network is called trabecular, spongy or cancellous bone
Periosteum
The outer surface of the compact bone is covered by a condensed fibro-collagen layer called the periosteum. It has
- Outer/fibrous layer comprising dense irregular connective tissue layer
- The inner/osteogenic layer consists of bone cells and their precursors and is rich in vascular supply
Periosteum Clinical significance:
- The periosteum is active during fetal development.
- Helps in the repair of fractures.
The thin cellular layer that lines the inner surface of compact bone is called the endosteum.
- It is a reservoir of new osteoblasts for remodelling and repair.
- In resting adult bone the osteoblasts and osteoprogenitor cells are in a quiescent state.
There are three types of lamellae in compact and trabecular bone:
- Circumferential lamellae
- Concentric lamellae
- Interstitial lamellae
Circumferential lamellae:
The lamellae that are arranged in parallel layers around the bony surface at the periosteal and endosteal surfaces are called the circumferential lamellae.
Concentric lamellae:
Deep to the circumferential lamellae, there are lamellae that are small and arranged in concentric layers around a central neurovascular canal called the Haversian canal (50 microns diameter). The concentric lamellae and the Haversian canal together are called the Haversian system or the osteon. It is considered the basic metabolic unit of the bone.
- Twenty concentric lamellae may be seen within one Haversian system.
- The Haversian system is delineated by a strongly basophilic line called the reversal line.
- It marks the point of bone erosion before the formation of the osteon.
- It is very irregular as it is formed by the scalloped outline of the Howship’s lacunae.
- The reversal line contains little or no collagen and is rich in glycoproteins and proteoglycans.
- The reversal line is different from the resting line.
- The resting line represents the period of rest during bone formation.
- It is more regular than the reversal line.
The collagen fibres along the length within each lamella have different orientations compared with the adjacent lamellae and this arrangement helps withstand stresses. Volkmann’s canals connect the longitudinally running Haversian canals with each other. They contain a rich network of vessels throughout the compact bone.
- At the junction of the lamellae, the osteocytes are present in the lacunae. The lacunae have small canaliculi radiating into the Haversian canal. The canaliculi thus connect each of the osteocytes in an osteon. This helps in the passage of nutrients and wastes.
Interstitial lamellae:
The lamellae between adjacent concentric lamellae are called interstitial lamellae.
- They are considered to be the remnants of osteons which are left behind after remodelling.
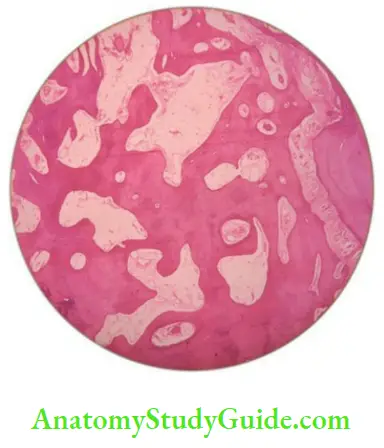
Spongy bone
The cells and the intercellular matrix of spongy bone and compact bone are the same but the components are arranged differently.
- Spongy bone is not as well organized as compact bone.
- Large, slender spicules called trabeculae form the substance of the bone.
- The trabeculae are 50 microns in thickness.
- They are arranged along the lines of stress and are able to withstand the forces.
- Large marrow spaces are present through which the trabeculae derive nutrition.
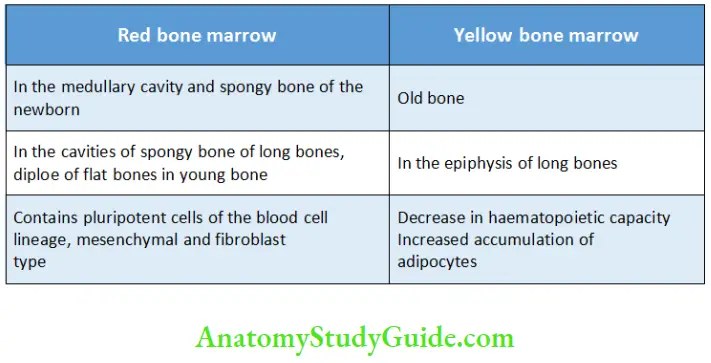
Marrow Tissues In Bone
The bone is lined outside by the periosteum and inside by the endosteum. The periosteum is a connective tissue membrane with an outer dense and irregular fibrous layer and an inner layer lined by bone cells and vessels. Its role is crucial during fetal development and fracture healing. The endosteum is a loose connective tissue separating bone surface and marrow. It contains quiescent osteoblasts and osteoprogenitor cells that serve as reservoirs for new bone-forming cells during remodelling. The periosteum plays a greater role in bone formation compared to the endosteum.
Marrow Tissues in Bone
Cells Of The Bone
- Osteoblasts
- Osteocytes
- Osteoclasts
Osteoblasts
Morphology:
- Mononucleated, basophilic, cuboidal or partly flattened cells
Osteoblasts Origin:
- Undifferentiated mesenchymal stem cells
- The osteoprogenitor cells are of two types:
- Determined osteoprogenitor cells
- Inducible osteoprogenitor cells
The determined cells from the bone marrow, periosteum and endosteum, differentiate into osteoblasts due to systemic and bone-derived growth factors and the inducible cells differentiate when stimulated.
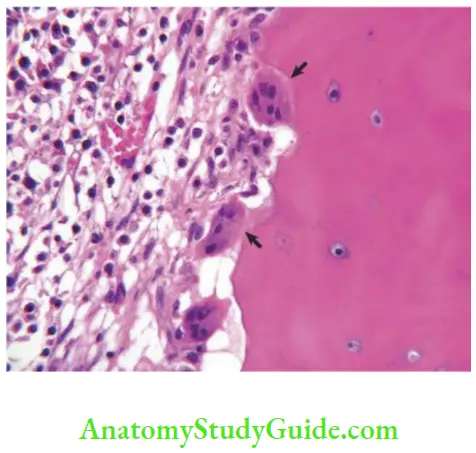
Osteoblasts Microscopic features:
- Abundant synthetic organelle that secrete proteins.
- Intensely basophilic cytoplasm due to the presence of numerous rough endoplasmic reticulum (RER). The RER synthesizes the organic components that are converted to secretory granules by the Golgi apparatus. The contents of the granules are then released along the cell surfaces near newly formed bone that assemble to form osteoid.
- Canaliculi are formed due to the deposition of the organic matrix around the cells and their cytoplasmic extensions. These canaliculi communicate with each other and the processes of osteocytes.
Osteoblasts Function:
- New bone formation
- Regulation of remodelling of bone and mineral metabolism
- Mineralization of the osteoid
- Secretion of Type I collagen and osteocalcin
- Secretion of small amounts of Type V collagen, osteonectin and osteopontin
- High levels of alkaline phosphatase on the outer surface
- Expression of receptors for hormones such as parathyroid hormone, vitamin D and oestrogen
- Identification of resorptive signals and conveying them to osteoclast cells
Osteoblasts Bone-lining cells: The osteoblasts are entrapped in the matrix of the bone and are called osteocytes once their function is completed or may flatten and remain on the surface and are called bone-lining cells. These have fewer organelles.
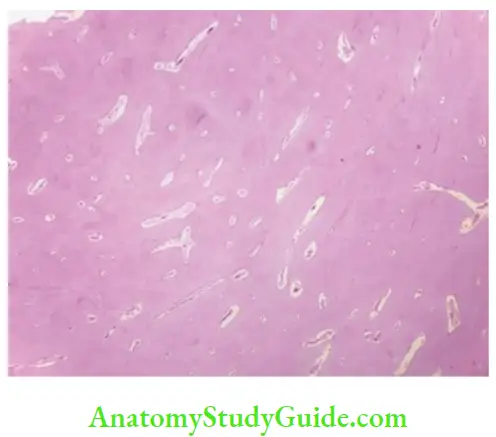
Osteocytes:
Osteoblasts get entrapped within the bone matrix and form osteocytes.
- The number of osteoblasts transforming into osteocytes depends on the rate of bone formation. The number of osteocytes is higher in woven bone. They repair bone faster than lamellae bone due to rapid formation.
- The ratio of osteocytes to osteoblasts in bone is 10:1.
- The average half-life is approximately 25 years.
- Osteocytes are lost while preparing ground sections and debris fills up their spaces which appear black under transmitted light.
- Osteocytes are surrounded by spaces called the osteocytic lacunae, which are lined by uncalcified tissue. Narrow extensions from these lacunae called the canaliculi communicate with the adjacent cells, osteoblasts and bone-lining cells. Diffusion of gases and nutrients occurs between the blood vessels and osteocytes through the canaliculi. Any failure of the communication system between the osteocytes and osteoblasts can lead to sclerosis and bone death.
- Mature osteocytes:
- Elliptical shape
- Oval nucleus with scanty faint basophilic cytoplasm
- Less number of organelle
- Secrete matrix proteins
Fate of osteocytes:
- Resorption of the matrix by osteoclasts
Osteoblasts to osteocytes
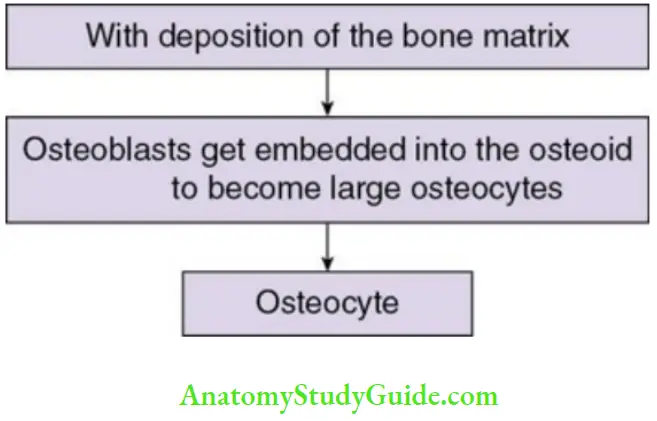
After the formation of new bone, the fate of the osteoblasts could be any of the below-mentioned:
- Embedded in bone to become osteocytes
- Get inactive to become bone-lining cells
- Apoptosis
- Differentiate into cartilage-laying cells
Osteoclasts:
Osteoclasts are multinucleated cells that cause the removal of the bone by removal of the calcified matrix of bone.
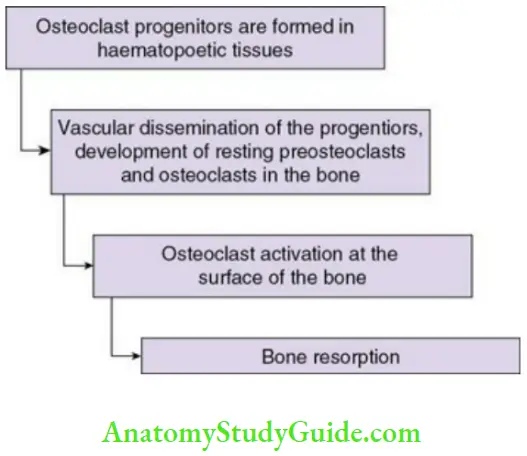
Osteoclasts Origin:

- Haematopoietic cells of monocyte-macrophage lineage.
- The committed precursors fuse to form multinucleated giant cells.
- RANK ligand (receptor activator of nuclear factor kB) and M-CSF (macrophage colony-stimulating factor) produced by adjacent stromal cells and osteoblasts are needed.
Osteoclasts Microscopic features:
- Size: large cell (40–100 microns diameter)
- Contain 15–20 nuclei; more the nuclei, the higher the rate of resorption.
- High content of acid phosphatase in the cytoplasm in vesicles and vacuoles.
Formation of osteoclast:
- Microtubules help transport vesicles between Golgi apparatus and the ruffled border of the osteoclasts.
- Extensive mitochondria except near the ruffled border.
- Sparse RER.
- Cathepsin-containing vesicles adjacent to the ruffled border indicating the resorption function of these cells.
Osteoclasts Ultrastructure:
- There are deep folds in the cell membrane adjacent to the resorbing surface of bone. The ruffled border increases the surface area.
- The cytoplasm in the ruffled border contains no organelle and thus this zone is called the clear zone.
- Numerous actin filaments are seen in the ruffled border.
Osteoclasts Location:
- Found in resorption bays known as Howship’s lacunae, which are shallow troughs with irregular shape reflecting the activity and mobility of the osteoclast during bone resorption.
Formation Of Bone
Bone may be formed by
- Intramembranous ossification
- Endochondral ossification
Intramembranous Ossification
Intramembranous ossification begins in the second month of intrauterine life in flat bones and clavicle. It is the process of direct formation of bone within sheets of condensed mesenchyme. The steps in intramembranous ossification are
- Bone matrix formation within fibrous membrane
- Woven bone formation
- Compact bone formation
- Osteon formation
Bone matrix formation within fibrous membrane:
- Loose mesenchyme with pale staining cells possessing interconnected process seen at the site of requirement of new bone formation.
- A centre of osteogenesis forms in the mesenchyme. The mesenchymal cells gradually become rounded and basophilic and transform into osteoblasts which secrete the bony matrix and further get entrapped forming osteocytes.
- The matrix later calcifies due to crystals from the matrix vesicles given off by osteoblasts. Osteocytes continue to obtain nutrients through the bony canaliculi by diffusion process.
Woven bone formation:
- Irregularly shaped spicules form a small mass of bone matrix that gradually lengthens into interconnecting structures called trabeculae.
- Adjacent trabeculae connect in a radial pattern forming a network called spongy bone. They enclose blood vessels and this new membranous bone is called woven bone.
- The trabeculae and spicules appear pink with large, round osteoblasts with a basophilic cytoplasm on H&E-stained sections.
Appositional growth and compact bone formation:
- The osteogenic cells present on the surface of spicules and trabeculae add new layers of bone matrix on the existing bone surface resulting in a process called appositional growth.
- The new osteocytes remain connected (to the bone surface above and below to osteocytes) through canaliculi. Adjacent capillaries are added to provide nutrition to osteocytes in deeper layers.
- Remodelling of trabeculae is characterized by simultaneous deposition and resorption of bone to maintain size and shape of the bone structure. The result is conversion of cancellous bone to compact bone.
- The central part of the bone is cancellous as the trabeculae do not increase in size. Red bone marrow is formed in the cancellous bone from the vascular tissue.
Osteon formation:
- The marrow spaces become narrower, the trabeculae thicken and narrow canals appear to carry vessels in the spaces of cancellous bone and thus the cancellous bone is transformed into compact bone.
- Numerous narrow canals are formed which enclose vessels of the marrow of the cancellous network. The addition of consecutive lamellae to the bony walls of spaces is termed osteon or Haversian systems. The osteons are shorter and thus called primitive osteons compared to the ones in long bones.
- A condensation of vascular mesenchyme happens around the woven bone is termed the periosteum.
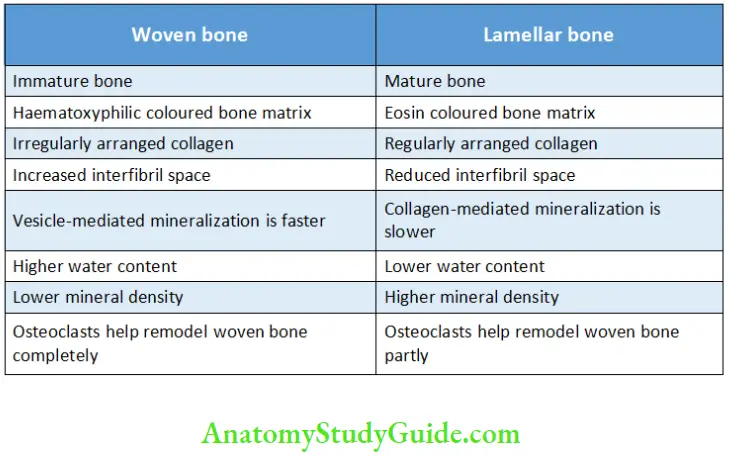
Difference between woven bone (immature bone) and lamellar bone (mature bone)
Difference between Woven Bone and Lamellar Bone
Endochondral Or Intracartilaginous Ossification
Endochondral ossification is a process of replacement of cartilage by bone and occurs in all long bones, vertebrae, ribs, articular surface of mandible and base of skull. It involves five steps:
- Cartilaginous model formation
- Bone collar formation
- Periosteal bud formation
- Medullary cavity formation
- Secondary ossification centre formation
Cartilaginous model
- At the site of requirement, mesenchymal cells condense (at the site of future limb in the embryo) to differentiate into chondroblasts and secrete a cartilaginous matrix to form hyaline cartilage surrounded by a layer of perichondrium.
- The perichondrium has an outer dense fibrous layer (fibroblasts form collagen) and an inner chondrogenic layer (osteoblasts are not formed in this layer due to avascularity).
- The increase in width of cartilage occurs by appositional growth by addition of matrix to the periphery (by the chondrocytes of chondrogenic layer of perichondrium) and the increase in length occurs by interstitial growth by addition of matrix by daughter cells (by chondrocytes).
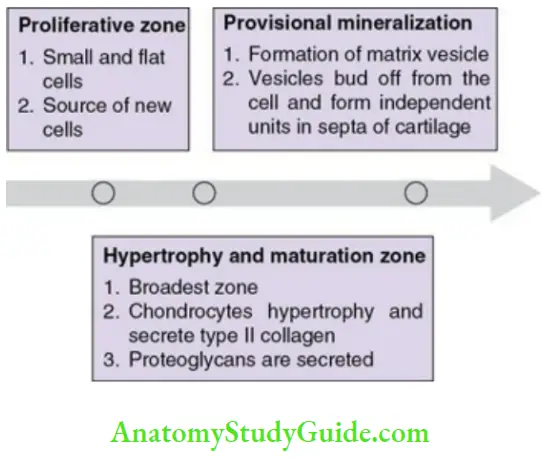
These differentiated cartilage cells migrate (towards the metaphysis of long bones) and are arranged in longitudinal columns as three zones:
- Proliferative zone
- Hypertrophy and maturation zone
- Provisional mineralization (Flowchart 7.4)
Bone collar formation:
- In the mid-section of cartilaginous model, capillaries grow into perichondrium.
- A thin collar of bone matrix is formed (around the mid-region) by
differentiation of cells of the inner layer of perichondrium to osteoblasts, transforming the perichondrium to periosteum. - As mineralization proceeds, chondroclasts resorb most of the cartilage matrix within, and the weakened (by resorption of cartilage) shaft is supported purely by the bone collar surrounding it. The middle of the cartilage undergoes vascularization.
Periosteal bud formation:
- The calcified cartilage is invaded by periosteal capillaries and osteogenic cells in the middle of the model to supply the interior part. The osteogenic cells and the periosteal capillaries are together referred to as the periosteal bud.
- The development of a primary ossification centre begins due to the invasion by periosteal capillaries.
- Osteoblasts arise from the osteogenic cells of the periosteal bud. They deposit bone on the residual calcified cartilage. This cancellous bone with the residual calcified cartilage is called the primary spicule. The network of mixed spicules is the primary spongiosa.
Medullary cavity formation:
- In the centre of the shaft, osteoclasts convert spongy bone to medullary spaces, into which haematopoietic cells invade and form myeloid tissue.
- The primary centre of ossification spreads towards the proximal and distal directions, but the ends of bones remain cartilaginous in nature.
- The mid-section of the shaft becomes diaphysis.
- The cartilaginous ends become epiphysis.
Thus, the primary centre of ossification is the diaphyseal region.
Secondary ossification centre formation:
- Before or after birth, chondrocytes in the mid-section of epiphysis hypertrophy, and the matrix calcifies between lacunae, forming secondary ossification centres.
- Spongy bones in the medullary spaces are retained and the epiphysis contains no medullary space.
- The ossification spreads in all directions resulting in replacement of the cartilage by cancellous bone.
- After secondary ossification, the hyaline cartilage is retained in two regions:
- Articular surface and termed articular cartilage.
- The junction of epiphysis and diaphysis, termed the epiphyseal plate.
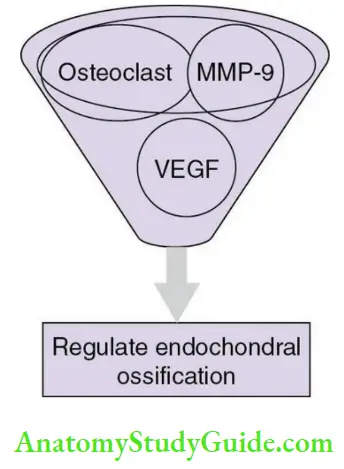
The epiphyseal plate of long bones contributes to bone lengthening by forming new cartilage and possesses two centres of ossification compared to short bones that possess only one centre of ossification. The epiphyseal line is formed by fusion of the primary and secondary ossification centres. The regulation of endochondral bone formation/ossification is by three factors as given in Flowchart.
Bone Calcification
Calcification is a process of adding insoluble calcium salts into a bone tissue.
Bone Mechanism:
- The first formed amorphous phase is converted to hydroxyapatite. The amorphous calcium spheres are 30–100 nm in diameter, containing randomly packed (0.95-nm diameter) hydroxyapatite crystals.
- The simultaneous crystallization and precipitation of calcium phosphate depends on sufficient amounts of serum calcium and phosphates. The (Ca)2+ x (Pi) ion product is the critical factor (where Pi is free orthophosphate) for the separation of calcium phosphate from solid phase to crystalline form. This process of calcium phosphate crystallization proceeds even in regions where (Ca2+ x Pi ion) product does not exceed plasma levels.
Theories Of Calcification
- Nucleation theory
1. Ground substance
2. Collagen
3. Mitochondria - Matrix vesicle theory
- Alkaline phosphatase theory
Bone Nucleation Theory:
According to this theory, a nucleus is capable of accumulating calcium and phosphate ions closer to collagen, and growth of hydroxyapatite crystals occurs by further addition of ions from surrounding fluids. This theory was based on the concept of seeding or epitaxy proposed by Neumann and Neumann in 1953. The various nucleation sites are
1. Ground substance
The changes in the sulphated glycosaminoglycans and proteoglycans of the cartilaginous matrix act as nucleation sites before mineralization.
2. Collagen
- Minerals are deposited in or on collagen fibres.
- The gaps between the molecules of collagen are filled with proteoglycans that bind to calcium (which is released by the enzymatic degradation of proteoglycans). The phosphoproteins attached to the collagen are broken down by alkaline phosphatase, releasing the phosphatase ions. These ions combine to form hydroxyapatite crystals between the gaps of collagen.
3. Mitochondria
Amorphous calcium phosphate (from the mitochondria) is released during cell damage or released indirectly as ions that support crystal growth extracellularly with the help of matrix vesicles.
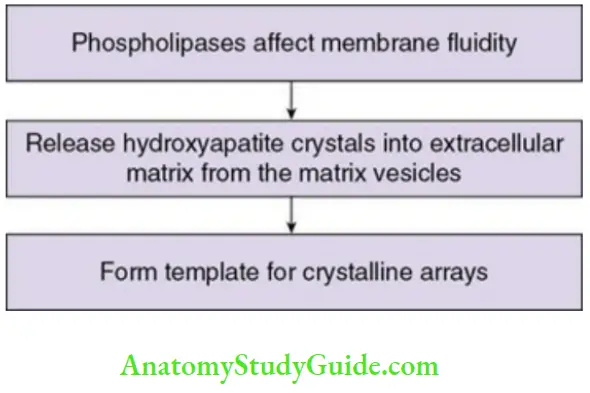
Matrix vesicles theory:
Osteoblasts, chondrocytes and odontoblasts bud off rounded (25–250 nm diameter) cell membrane outgrowths called ‘matrix vesicles’, rich in phospholipids, especially phosphatidyl serine (high calcium affinity), and annexins. Annexins form calcium channels to allow addition of calcium ions into matrix vesicles. The vesicles accumulate Ca2+, with its membranes creating binding sites for hydroxyapatite nucleation.
Thus, mineralization begins inside these vesicles and they create an environment for initial amorphous mineral complex deposition and form needle-like hydroxyapatite crystals on the inner surface of these vesicles.
Steps in calcification
Bone Nucleation Theory Drawbacks:
- Crystals are not always seen on the mineralization fronts of mature bone.
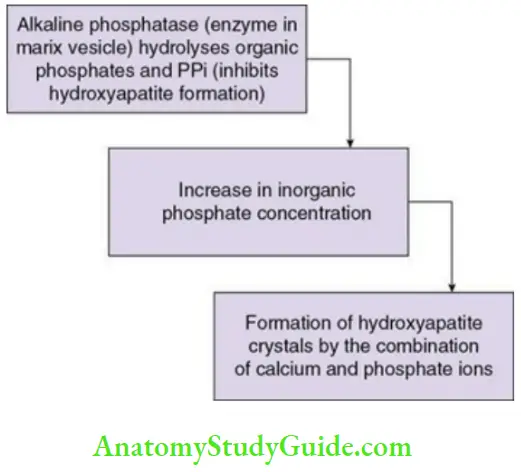
Alkaline phosphatase Theory:
Alkaline phosphatase is an enzyme that takes part in mineralization.
- It is present within the matrix vesicles.
- It hydrolyses different organic phosphatase-containing substances.
- It increases the concentration of local inorganic phosphate.
- It is a marker for active bone tissue mineralization.
The sequence of enzyme action is explained below in Flowchart.
Alkaline phosphatase Theory Drawbacks:
- Tissues that do not calcify also contain alkaline phosphatase.
- Inhibitors of enzymes other than alkaline phosphatase are seen to prevent mineralization.
Calcification inhibitors:
Inhibitors of calcification prevent the formation of hydroxyapatite from amorphous calcium phosphate. They include
- Pyrophosphate
- Diphosphonates
- ATP
Few of the other potential inhibitors are
- Magnesium
- Citrate
- Albumin
Bone Resorption
Bone resorption is the process of removal of the calcified and organic bone matrix by osteoclasts and osteolytic cells.
- Rate of turnover: 30%–100% per year in rapidly growing children
- Slow in adults
- Faster in trabecular bone and endosteal surface of cortical bone than in cortical bone
The sequence of events is mentioned in Flowchart.
1. Osteoclast morphology and structure:
Before resorption begins:
Osteoclasts develop a ruffled border and a sealing zone in their plasma membrane adjacent to bone surface. The ruffled borders are cytoplasmic finger-like projections that increase the contact area between bone and cell.
The plasma membrane is smooth at the periphery of the ruffled border. The cytoplasm adjacent to the ruffled border contains actin microfilaments surrounded by two vinculin rings and is devoid of cell organelles and thus called the clear/sealing zone. This area attaches the cell closely to the bone surface and prevents diffusion of hydrolytic enzymes into adjacent tissue.
The attachment is facilitated by integrins expressed by resorbing osteoclasts, especially αVβ3 (vitronectin receptor). Integrins bind to the amino acid sequence of bone matrix proteins.
2. Hydroxyapatite removal:
- Dissolution of the bone mineral is carried out by HCl. The protons of HCl are released by the osteoclasts across the ruffled border into the area of resorption by the proton pump, leading to a decrease in the pH.
3. Organic matrix removal:
- Osteoclasts synthesize proteolytic enzymes such as cathepsin-K and MMP-9. The enzymes are released into the sealed compartment through extracellular lysosomes.
- Cathepsin-K is collagenolytic and MMP-9 helps in the migration of osteoclasts.
4. Degradation product removal from the lacunae:
- Osteoclasts endocytose (free organic and nonorganic) bone matrix into membrane-bound vesicles (in the cytoplasm) once they are across the ruffled border.
- They fuse with the functional secretory domain (FSD) of the basal membrane and are released by the process of exocytosis. It is indicated by changes in cytoplasmic framework and cluster of matrix fragments.
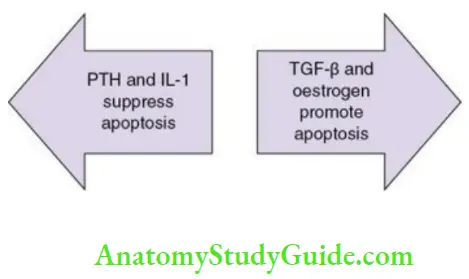
- The rate-limiting step in the process is apoptosis of osteoclasts at the end of resorption.
Role of TRAP in bone resorption:
Tartrate-resistant acid phosphatase (TRAP) is a latent inactive proenzyme. It is converted to active form by cysteine proteinase. It plays a crucial role in bone resorption.
- Extracellular role of TRAP
- Intracellular role of TRAP
Extracellular role of TRAP:
TRAP is seen near the ruffled border of the resorbing osteoclast in the bony matrix.
- It may regulate the adhesion of the osteoclasts to bone and their migration to the sites of bone resorption.
- It may initiate the resorption of bone by the osteoclasts.
Intracellular role of TRAP:
- Vesicles containing TRAP transport the degraded organic matrix from the ruffled border to the FSD of osteoclasts.
Bone Remodelling
Remodelling of bone is by basic multicellular units (BMUs), which are clusters of osteoclasts and osteoblasts that are arranged in temporary anatomical structures.
An active BMU contains
- Leading front of osteoclasts.
- Osteoblasts occupy the tail.
Coupling of bone:
The synthesis and breakdown of bone is simultaneous and the net result is due to the balance between the two. This is called coupling ofbone.
Functions of remodelling:
- Regeneration of new bone to prevent fatigued and damaged bone accumulation
- Accommodation of changes in the bone to forces
- Homeostasis of minerals
Sequence of bone remodelling:
It consists of three stages:
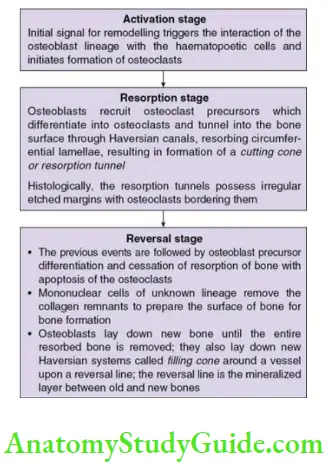
- Activation stage
- Resorption stage
- Reversal stage
Mediators of bone remodelling
The remodelling process is affected in pathologic conditions like
- Osteoporosis
- Osteopetrosis
- Malignant bone tumours
- Inflammatory joint disease
- Hyperparathyroidism
- Paget disease
- Hyperthyroidism
Factors Mediating Bone Formation
Factors favouring bone formation
- Growth hormone
- Vitamin D
- Insulin
- PTH (low doses)
Factors decreasing bone formation
- Glucocorticoids
Factors Mediating Bone Resorption
Factors favouring bone resorption
- PTH
- Glucocorticoids
- Vitamin D in high doses
Factors decreasing bone resorption
- Calcitonin
- Oestrogen
Alveolar Process And Alveolar Bone Proper
The part of the maxilla and the mandible which forms and supports the sockets of the tooth where the teeth are anchored is called the alveolar process. There is no definite boundary between the alveolar processes and the body of the maxilla and the mandible. It might be partly masked or fused with the bone not related to the teeth.
- The palatine process of the maxilla fuses with the oral part of the alveolar process in the anterior maxilla.
- The oblique line is superimposed laterally onto the bone alveolar process in the posterior mandible.
Thus, the parts of the alveolar bone are
- Alveolar bone proper
- Supporting alveolar bone
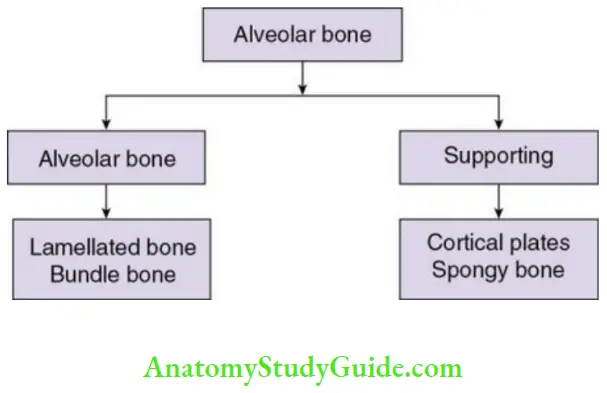
Alveolar Bone Proper
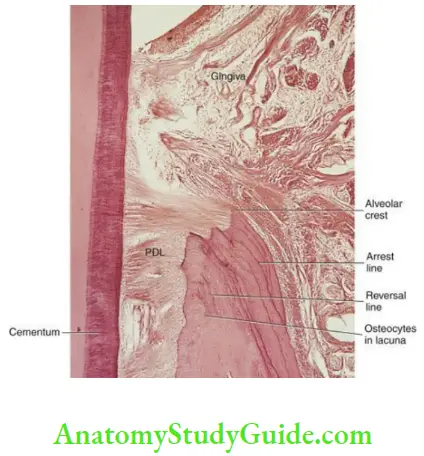
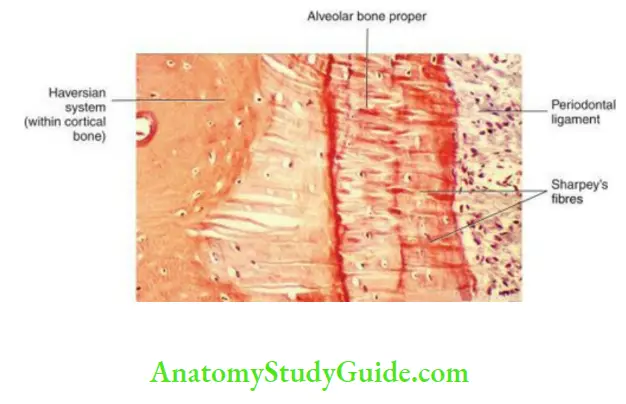
- Alveolar bone proper is also called the cribriform plate due to the perforations for the passage of the interalveolar nerves and vessels into the PDL.
- It forms the inner wall of the socket of the tooth.
- Its thickness is 0.1–0.4 mm.
- It surrounds the root.
- It provides attachment to the principal fibres of the PDL.
Alveolar bone proper consists of
- Lamellated bone
- Bundle bone
Lamellated Bone
- The lamellae are arranged parallel to the surface of the adjacent marrow spaces.
- Some lamellae form the Haversian system or the osteon.
Bundle Bone
The bone where the bundles of the principal fibres from the periodontal ligament are attached is called the bundle bone.
- Less number of collagen fibrils are seen in the intercellular substance.
- The fibrils are arranged perpendicular to the Sharpey’s fibres.
- It contains less number of fibrils than the lamellated bone and appears dark in H&E-stained sections.
- The fibrils are larger in diameter at the periphery and also mineralized.
- The fibres are lesser in number and less mature than in the cementum.
- The bone formed in areas of recent bone apposition is the bundle bone.
- Resting lines are also seen in the bundle bone.
Radiographically
- It is called lamina dura.
- It appears as radiopaque lining of the socket.
- It is continuous with the buccal and lingual cortical bone of the alveolar crest.
- It appears radio-opaque as the X-rays cannot pass through the thick bone without trabeculae. (It is not due to the mineral content.)
Interdental And Interradicular Septum
- The bone between the teeth entirely composed of the cribriform plate is called interdental septum.
- The bone between the roots of the teeth is called the interradicular septum.
- Both the septa contain the canals Zuckerkandl and Hirschfeld that contain the interdental and interradicular lymph vessels, nerves, arteries and veins.
Supporting Alveolar Bone
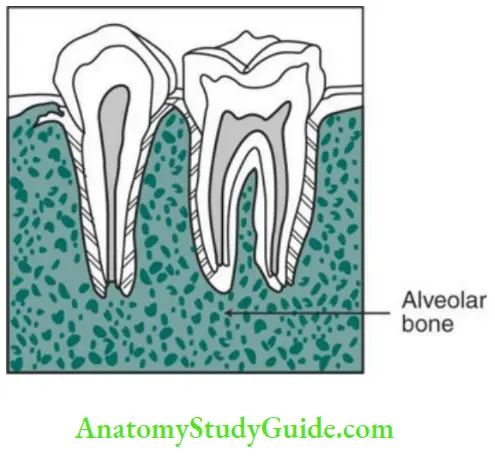
- Cortical plates
- Spongy bone
Cortical plates:
- Cortical plates are made up of compact bone.
- They form the outer and inner plates of the alveolar process.
- Cortical plates are thinner in the maxilla than in the mandible. They are thickest in the buccal surface of the mandible in the premolar and molar regions.
- They consist of longitudinal lamellae and Haversian system. Perforations in the outer cortical plate allow blood and lymph vessels.
- In maxilla, the cortical plates fuse with the alveolar bone proper in anterior regions, with no spongy bone. The premolar and molar regions are more prone to outer alveolar wall defects. The periodontal tissues fuse with the covering mucosa in those defects but do not hamper the attachment and function of the teeth.
- In mandible, the circumferential lamellae extend between cortical plates to the body of mandible.
The bone below the gingiva is the cortical plate. The cortical plate and cribriform plate are compact bones separated by spongy bone.
Spongy bone:
Spongy bone is the cancellous bone which occupies the space between cortical plates and alveolar bone proper.
- Spongy bone contains trabeculae of lamellar bone.
- It is surrounded by marrow spaces rich in adipocytes and pluripotent cells.
- Osteocytes are seen on the interior of the trabeculae whereas osteoblasts and osteoclasts are seen on the surface.
- The trabeculae absorb occlusal forces exerted on alveolar bone proper.
- The maxilla contains more spongy bone compared to the mandible.
The spongiosa is classified into two types based on radiographic appearance
Type I
Type II
Types of Spongiosa
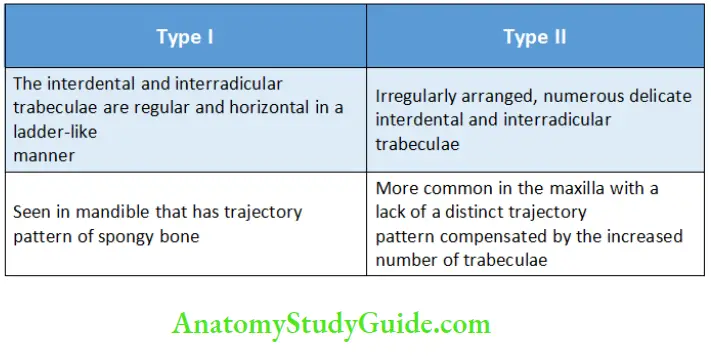
The trabeculae might radiate in distal direction from the apical portion of the socket of the lower molars. Due to the proximity to the nasal cavity and the maxillary sinus, these trabeculae are less prominent in the maxilla.
Crest of alveolar septa:
- The outline of the crest of the alveolar septa depends on the position of the adjacent teeth.
- The alveolar crest is obliquely inclined when the adjacent teeth are inclined. The inclination is greater in the premolar and molar regions in most of the individuals as the teeth are mesially tipped. The alveolar crest of the mesial tooth slopes distally as the CEJ of the mesial tooth is more occlusal to that of the distal tooth.
- The cortical and alveolar bones fuse at the alveolar crest. It is about 1.5–2 mm below the CEJ of the tooth it envelops.
Alveolar bone function:
- Provides space for the roots of the teeth
- Insertion of Sharpey’s fibres into the alveolar bone, and thus anchors the teeth
- Provides little movement to the teeth for better occlusion
- Acts as a shock absorber by distributing and absorbing the occlusal forces
- Provides vessels to the PDL
- Protects the developing teeth of the permanent dentition and also supports the deciduous teeth
- Helps in the eruption of the deciduous and permanent teeth
Development: Alveolar process
- The development of the alveolar process starts during the development and eruption of the teeth and decreases in height with the loss of the teeth.
- The maxilla and the mandible form a groove which opens towards the surface of the oral cavity at the end of the second month of fetal life.
- Bony septa and bridge begin to form around the tooth germs developing within the bone at the late bell stage. They separate the tooth germs and place them in separate compartments lined by bone. The alveolar nerves and vessels are also incorporated with the tooth germ.
- At this stage, each tooth germ is surrounded by the dental follicle which is present between the tooth germ and its bony compartment.
- Before the formation of the root, the tooth germs in the bony compartments exhibit bodily movements to adjust with jaw growth. The movements induce remodelling of the bone of the compartment.
- The alveolar bone increases in height as the roots develop. Some cells of the dental follicle differentiate into osteoblasts and the formation of alveolar bone proper begins; some dental follicle cells also start deposition of cementum and formation of the PDL.
- Part of the alveolar process is incorporated within the body of the maxilla and the mandible during growth whereas rapid growth is seen at its free borders.
- At the alveolar crest, a tissue chondroid bone may be formed during this rapid growth. This has features of bone and cartilage.
Clinical Considerations
Plasticity of bone:
Bone is a vascularized connective tissue. The capacity of bone to remodel throughout life helps the teeth reposition itself during orthodontic treatment.
It is sensitive to pressure and tension. Pressure causes resorption and tension leads to bone deposition.
Orthodontic tooth movement without changing the relationship of the tooth with the bone is due to the plasticity of the bone. Resorption and deposition of bone allows the alveolus to shift the tooth.
As the osteoclasts may not fully differentiate between dentin, cementum and bone excess forces may lead to root resorption or destruction of a major portion of the root.
Adaptation of bone:
It is qualitative and quantitative.
Increased function increases new bone formation and vice versa. This may be seen in teeth without their antagonists.
Healing of fractures and wounds:
- Initially immature/coarse fibrillary bone is formed which is later replaced by mature bone. The immature bone contains larger number, size and irregular arrangement of osteocytes compared to mature bone.
Clinical consideration:
-
- Immature bone is more radiolucent than mature bone and thus bony callus are not seen in the radiographs even though microscopic examination might reveal union between fragments.
- An extraction socket appears empty on a radiograph, even though entirely filled with immature bone.
Periodontal disease:
- It leads to the symmetrical resorption of bone or localized alveolar bone loss.
- It is frequent in posterior teeth.
- The loss of bone is vertical and horizontal.
- It is related to the bacterial plaque and periodontal pocket formation. The endotoxins produced by the Gram-negative bacteria increase the levels of cAMP which increase osteoclastic activity.
Resorption after tooth loss:
The principal site is the labial aspect of the alveolar crest which decreases in width and then in height.
Maxilla: The alveolar ridge resorbs upwards and inwards.
Mandible: The alveolar ridge resorbs downwards and outwards.
Significance of lamina dura:
Decrease in density is indicative of
- Infection
- Inflammation
- Resorption of the bony socket
Bone grafts:
Autografts
- Patient’s own bone from extraoral or intraoral sites is used.
- Most suitable material
- Lead to faster rate of bone formation
- No risk of transmission of disease
- No immune reaction
Autografts Drawback:
- Discomfort due to an additional procedure
Allografts
- Bone from another individual or processed bone powder from cadavers
- Bone growth is induced and an environment to increase the regenerative capacity of the body is provided by allografts
- They might be available as demineralized or nonmineralized
- Osteoinductive growth is possible as they contain growth factors
Allografts Drawbacks:
- Risk of transmission of disease
- Rejection of the graft
Bone grafts are used to fill bony defects and provide structural support and to promote healing of bone.
Bone or substitutes of bone are placed within the bony defects to promote new bone formation or even regeneration of cementum and the periodontal ligament in cases of periodontal disease.
Xenografts:
- From animal sources such as cow and/or pigs
- They include processed bone from the animals with growth factors
- Higher risk of disease transmission and rejection
Alveolar bone Synopsis:
- Bone is a mineralized connective tissue which is one of the hardest structures in the body and makes up the body skeleton.
- The bone matrix comprises inorganic material (65%), organic material (25%) and water (15%).
- The unmineralized bone matrix on the surface of the bone where active bone formation is still occurring is called osteoid.
- In adult bones, the dense outer sheet is called compact bone and there is a medullary cavity in the centre. The cavity contains yellow or red bone marrow.
- The cavity has a rich network of bony trabeculae. This network is called trabecular, spongy or cancellous bone.
- The outer surface of the compact bone is covered by a condensed fibrocollagen layer called the periosteum. There are three types of lamellae in compact and trabecular bone: circumferential lamellae, concentric lamellae and interstitial lamellae.
- Bone is lined outside by periosteum and inside by endosteum. Periosteum is a connective tissue membrane with an outer dense and irregular fibrous layer and inner layer lined by bone cells and vessels.
- Cells of the bone include osteoblasts, osteocytes and osteoclasts.
- Bone may be formed by intramembranous ossification and endochondral ossification.
- Intramembranous ossification begins in the second month of intrauterine life in flat bones and clavicle. It is the process of direct formation of bone within sheets of condensed mesenchyme.
- Endochondral or intracartilaginous ossification is a process of replacement of cartilage by bone and occurs in all long bones, vertebrae, ribs, articular surface of mandible and base of skull.
- Bone calcification is a process of adding insoluble calcium salts into a bone tissue.
- Theories of calcification include nucleation theory, matrix vesicle theory and alkaline phosphatase theory.
- Bone resorption is the process of removal of the calcified and organic bone matrix by osteoclasts and osteolytic cells.
- Synthesis and breakdown of bone is simultaneous and the net result is due to the balance between the two. This is called coupling of bone.
- The part of the maxilla and the mandible which forms and supports the sockets of the tooth where the teeth are anchored is called the alveolar process. There is no definite boundary between the alveolar processes and the body of the maxilla and the mandible.
- The parts of the alveolar bone are alveolar bone proper and supporting alveolar bone.
- Alveolar bone proper is also called the cribriform plate due to the perforations for the passage of the interalveolar nerves and vessels into the PDL.
- Alveolar bone proper consists of lamellated bone and bundle bone.
- The bone between the teeth entirely composed of the cribriform plate is called interdental septum. The bone between the roots of the teeth is called the interradicular septum.
- Supporting alveolar bone is made up of cortical plates and spongy bone.
- The outline of the crest of the alveolar septa depends on the position of adjacent teeth.
- The development of the alveolar process starts during the development and eruption of the teeth and decreases in height with the loss of the teeth.
Leave a Reply