Aminoglycosides Antibiotics
Aminoglycosides with Penicillins↑
Table of Contents
Question 4. What is the rationale for combining aminoglycosides with penicillins
Answer:
Penicillin + aminoglycosides → synergistic combination because:
- Both are bactericidal.
- The combination is synergistic.
- Low pH and an anaerobic environment reduce the uptake of aminoglycosides by active transport because this is an O2 -dependent process. This negative effect is reversed by penicillin.
- Penicillins increase penetration of aminoglycosides by inhibiting bacterial cell wall synthesis.
- Moreover, penicillins are also effective in anaerobes.
Read And Learn More: Pharmacology Question And Answers

Aminoglycosides: Resistance to aminoglycosides is acquired by
- Aminoglycoside inactivating enzymes
- Low affinity of ribosomes—acquired by mutation.
- Decrease in permeability to the antibiotic.
- There is partial cross-resistance among aminoglycosides.
Aminoglycosides Penicillin Pharmacokinetics:
- Aminoglycosides are not absorbed from the gut.
- When instilled into body cavities or applied over large wounds, they get rapidly absorbed.
- They are not bound to plasma proteins and do not enter the cells or cross barriers—mostly remain in the vasculature
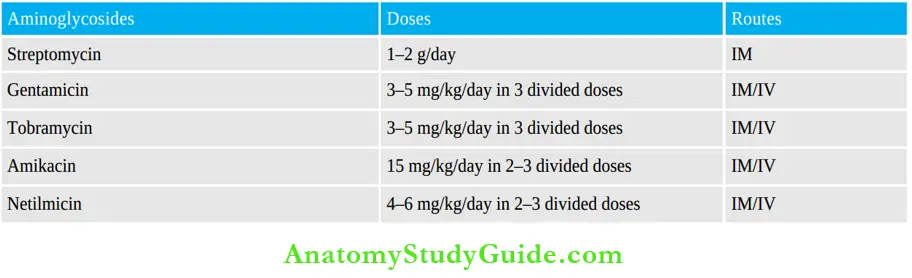
Dose and route of administration of aminoglycosides:
Excreted through the kidneys. Half-life is 2–3 hours but gets prolonged to 24–48 hours in renal impairment—dose should be reduced.
Aminoglycosides Adverse Effects
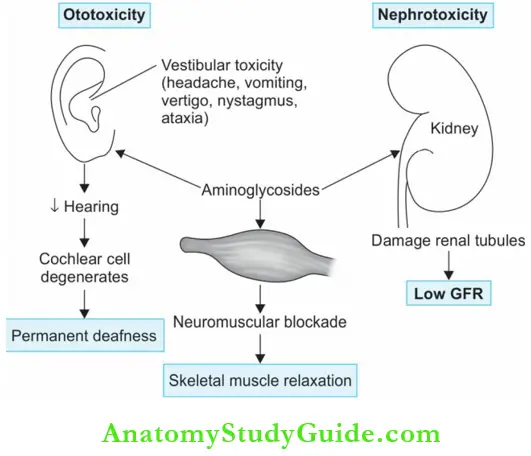
1. Ototoxicity:
- Ototoxicity is the most important toxicity. Both vestibular and auditory dysfunction can occur depending on the dose and duration.
- The aminoglycosides get concentrated in the labyrinthine fluid of the inner ear and damage both cochlear hair cells and vestibular sensory cells. The auditory nerve degenerates.
- As the cochlear cells cannot regenerate, there is progressive, permanent deafness. Tinnitus appears first, followed by deafness; elderly people are more susceptible.
- Stopping the drug can prevent further damage. Vestibular dysfunction is manifested by headache, nausea, vomiting, dizziness, vertigo, nystagmus, and ataxia. Most symptoms subside in 2 weeks except ataxia which may persist for 1–2 years.
- Neomycin, amikacin, and kanamycin are the aminoglycosides that are most likely to cause deafness, while streptomycin and gentamicin are most likely to cause vestibular toxicity.
2. Nephrotoxicity:
- Aminoglycosides attain high concentrations in the renal cortex and cause damage to the renal tubules.
- This results in loss of urine concentrating capacity, low GFR, and albuminuria. These effects are reversible. Gentamicin, neomycin, and tobramycin are the most nephrotoxic.
3. Neuromuscular blockade: Aminoglycosides have curare-like effects and block neuromuscular transmission.
Precautions In Using Aminoglycosides
- Avoid use of other ototoxic drugs like loop diuretics with aminoglycosides.
- Avoid other nephrotoxic drugs like amphotericin B, cephalothin, and cisplatin with aminoglycosides

- Use cautiously in the elderly, in renal dysfunction, and with skeletal muscle relaxants.
- Contraindicated in pregnancy because of the risk of deafness in the child.
- Do not mix aminoglycosides with any other drug in the same syringe.
- Determination of plasma levels of aminoglycosides may be needed in severe infections and patients with renal dysfunction.
Precautions In Using Aminoglycosides Uses
- Infections due to gram-negative bacteria.
- Streptococcal and enterococcal endocarditis with a penicillin → synergistic:
- Tuberculosis—streptomycin, kanamycin, and amikacin are used in tuberculosis.
Streptomycin
- Obtained from Streptomyces griseus
- Effective against aerobic gram-negative bacilli. Dose: 1–2 g/day.
- Least nephrotoxic among aminoglycosides.
Streptomycin Uses:
- Tuberculosis: In combination regimen.
- Subacute bacterial endocarditis (SBE): Streptomycin + penicillin → synergistic in enterococcal and Streptococcus viridans endocarditis.
- Plague, tularemia, and brucellosis: Streptomycin is given with a tetracycline.
Gentamicin
- Obtained from Micromonospora purpurea is more potent and has a broader spectrum of action compared to streptomycin.
- The development of resistance has limited its use. It causes more nephrotoxicity and vestibulotoxicity.
- Dose: 3–5 mg/kg/day in 3 divided doses.
Gentamicin Uses:
- UTI: Uncomplicated UTI—gentamicin is released for a long time from the renal cortex.
- Pneumonia due to gram-negative organisms → gentamicin + penicillin.
- Osteomyelitis, peritonitis, septicemia, abscess, burns — by gram-negative organisms.
- Meningitis due to gram-negative bacilli: Gentamicin + third-generation cephalosporin.
- SBE: Alternative to streptomycin.
- Topical: Gentamicin cream is used topically in burns and other infected wounds. Gentamicin eye drops are used in the prevention and treatment of bacterial conjunctivitis.
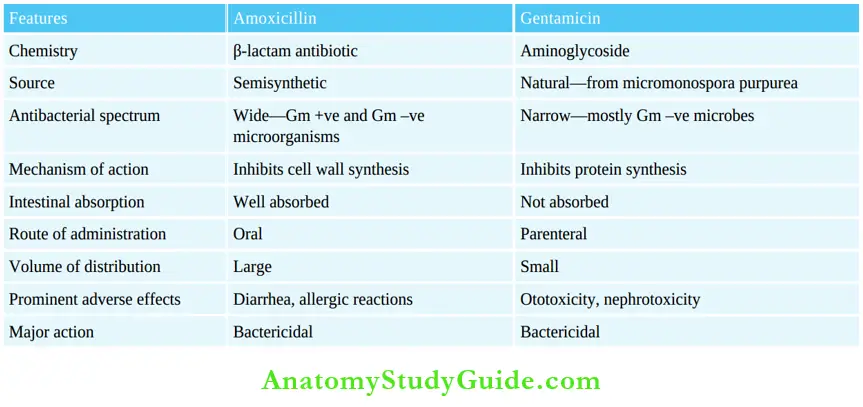
Amoxicillin and gentamicin
Amikacin
- A semisynthetic derivative of kanamycin
- Has widest antibacterial spectrum among the aminoglycosides because it is resistant to aminoglycoside-inactivating enzymes. Dose:15 mg/kg/day in 2–3 divided doses.
Amikacin Uses:
- Nosocomial infections due to gram-negative organisms.
- Tuberculosis: MDR tuberculosis with other drugs.
- Atypical mycobacteria in patients with AIDS.
Netilmicin:
- Like amikacin, netilmicin is resistant to aminoglycoside-inactivating enzymes.
- It is used in serious infections due to gram-negative bacilli.
- Dose: 4–6 mg/kg/day in 2–3 divided doses.
Tobramycin:
- Tobramycin has better activity against it.
- Pseudomonas can be used in place of gentamicin.
- Dose: 3–5 mg/kg/day in 1–3 divided doses.
Kanamycin: Due to its toxicity, its use is limited to multidrug-resistant tuberculosis.
Sisomicin: Sisomicin has actions, toxicity, and uses similar to gentamicin
Neomycin
- Has a wide antibacterial spectrum—effective against gram-positive and gram-negative bacteria.
- It is highly ototoxic → not given systemically → used topically and also used orally for action on the gut.
Neomycin Adverse effects:
- Neomycin can cause skin rashes on topical use.
- Oral use can cause diarrhea, steatorrhea, and malabsorption due to damage to the intestinal villi. Superinfection with candida can also occur.
Dose: Oral 0.25–1g QID. 0.3–0.5% topical; 0.3, 0.5% ointment.
Neomycin Uses:
- Topical: In skin infections, burns, ulcers, and wounds; eye and ear infections.
- Orally:
- Neomycin is not absorbed when given orally. It inhibits the growth of intestinal flora and is excreted in the feces. It is used to prepare the bowel for surgery, i.e. for preoperative gut sterilization 1g 3–4 times a day for 1–2 days with or without 1g erythromycin.

Hepatic coma: Ammonia produced by colonic bacteria is absorbed and converted to urea by the liver. In severe hepatic failure, as liver is unable to handle this NH3, blood NH3 levels rise resulting in encephalopathy. As neomycin inhibits intestinal flora, NH3 production falls. Neomycin is given orally for this purpose. However, lactulose is nowpreferred for this indication.
Macrolides And Other Antibacterial Agents
Macrolides are antibiotics with a large (macrocyclic) lactone ring to which sugars are attached.
Macrolides Include:
- Erythromycin, roxithromycin, clarithromycin, azithromycin.
- Dirithromycin, oleandomycin, troleandomycin, spiramycin.
Erythromycin
Erythromycin is obtained from Streptomyces erythreus.
Antibacterial spectrum:
- Antibacterial spectrum is narrow and effective against aerobic gram-positive bacteria and a few gram-negative organisms.
- Streptococci, pneumococci, staphylococci, gonococci, Legionella, C. diphtheriae, B. pertussis, T. pallidum, C. jejuni, Mycoplasma, Chlamydiae, and some atypical mycobacteria are sensitive.
Antibacterial spectrum Mechanism of action:
- Erythromycin is bacteriostatic at low and tidal at high concentrations. It is more effective in the alkaline pH. It binds to 50S ribosomes and inhibits bacterial protein synthesis.
- Macrolides inhibit the translocation of the growing peptide chain from the A site to P site.
- Hence, A site is not available for binding of the next amino acid (brought by tRNA) and protein synthesis stops.
Erythromycin, chloramphenicol, and clindamycin all bind to 50S ribosomes and the three may antagonize each other’s activity because they compete for the same binding site. Hence, the combination should be avoided.
Resistance is acquired through plasmids. Expressed as:
Low permeability of the bacteria to the antibiotic.
- Production of inactivating enzymes.
- Low affinity of ribosomes to macrolides.

Erythromycin Pharmacokinetics:
- Food interferes with absorption: Erythromycin is destroyed by gastric acid and is, therefore, given as enteric-coated tablets.
- Plasma t½ ~1.5 hours: Good concentration is attained in most fluids except brain and CSF. It also crosses the placenta. Erythromycin is a microsomal enzyme inhibitor. It is mainly excreted through the bile; dose adjustment is not needed in renal failure.
Adult dose and duration of treatment with macrolides:

Erythromycin Adverse Effects:
- Hepatitis with cholestatic jaundice starts after 2–3 weeks of treatment more common with estolate salt—may be an allergic response. The symptoms—nausea, vomiting, and abdominal cramps, mimic acute cholecystitis and may be wrongly treated followed by jaundice and fever. Hepatitis is self-limiting but erythromycin should be avoided in such patients.
- Epigastric distress, nausea, and vomiting. Diarrhea—erythromycin is a motilin receptor agonist due to which it causes increased intestinal motility.
- Allergic reactions include fever and skin rashes.
- Cardiac arrhythmias in patients with cardiac diseases or on other arrhythmogenic drugs.
- Reversible hearing impairment in some patients.
Erythromycin Drug Interactions:
- Erythromycin and clarithromycin are microsomal enzyme (cytochrome P450) inhibitors.
- They inhibit hepatic metabolism and thereby enhance the plasma levels of other drugs resulting in toxicity.

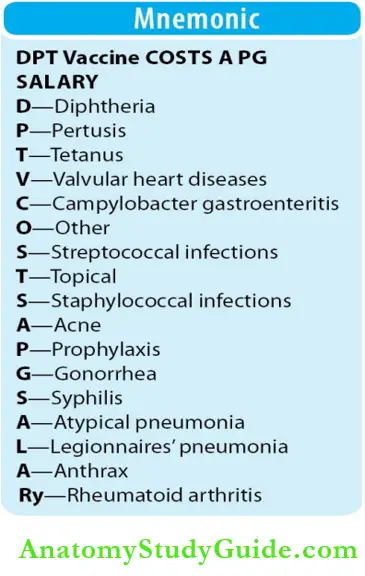
Erythromycin Uses:
Erythromycin is the drug of choice in
- Atypical pneumonia: Due to Mycoplasma pneumoniae.
- Legionnaires’ pneumonia: IV erythromycin 10–14 days/azithromycin.
- Whooping cough (pertussis): Erythromycin is effective both for treatment and prophylaxis of close contacts. Clarithromycin and azithromycin may also be used.
- Streptococcal infections: Pharyngitis, tonsillitis, and scarlet fever respond to erythromycin.
- Staphylococcal infections: Minor infections may be treated but now resistance common.
- Diphtheria: Erythromycin is very effective in the acute stage though antitoxin is life-saving.
Erythromycin also eradicates the carrier state.
- As an alternative to penicillin in:
- Syphilis and gonorrhea: Erythromycin is effective.
- Campylobacter gastroenteritis: As an alternative to fluoroquinolones.
- Tetanus: Erythromycin eradicates carrier state.
- Anthrax: Erythromycin effective.
- Prophylaxis: Alternative to penicillin in valvular heart disease patients undergoing dental and other minor procedures.
- Topical: Erythromycin ointment (2–4%) for skin infections and boils, lotion for acne.
- Other uses:
- Erythromycin is a motilin receptor agonist and stimulates GI motility. This property can be made use of in gastroparesis in postoperative patients and in diabetic gastroparesis.
- Erythromycin also has anti-inflammatory actions and may be of value in rheumatoid arthritis and chronic sinusitis.
Erythromycin can be used as an alternative to penicillin in patients allergic to penicillin.
Roxithromycin
The advantages of roxithromycin over erythromycin are:
- Longer-acting
- Acid-stable
- More potent
- Better absorbed
- Better tissue penetrability
- More potent against Legionella.
- Does not inhibit the metabolism of other drugs—free of drug interactions.
- Roxithromycin should be taken 30 minutes before food because food can interfere with absorption and reduce bioavailability.
Roxithromycin Uses:
- As an alternative to erythromycin.
- Dose: 150 mg BD for 7–10.
Clarithromycin
Compared to erythromycin, clarithromycin is:
- Longer-acting
- Acid-stable
- Better absorbed
- More effective against H. influenzae, Legionella, atypical mycobacteria, H. pylori, and some
- Protozoa.
- Has activity against M. leprae and T. gondii.
- Structurally similar to erythromycin → drug interactions similar to it
- Dose reduction may be required in renal dysfunction
- More expensive.
Clarithromycin Uses:
- As a component of a triple regimen for H. pylori infections in peptic ulcer patients.
- For the prevention and treatment of atypical mycobacterial infections in AIDS patients.
Though clarithromycin is effective in other indications of erythromycin, its higher cost makes it less preferable. Dose: 250–500 mg BD or 1g extended-release preparation OD for 7–14 days.
Azithromycin
The advantages of azithromycin over erythromycin are:
- Acid-stable
- Rapidly absorbed
- Better tissue penetrability
- Longer-acting—once daily. Azithromycin remains in the tissues for a long period and is gradually released from them and therefore, the elimination t½ is almost 3 days. Hence in many infections, it is effective even in a single dose.
- Better tolerated than erythromycin.
- Excellent activity against H. influenzae.
- Also effective against MAC, T. gondii, and H. influenzae.
- Free of drug interactions → does not suppress hepatic microsomal enzymes → does not inhibit hepatic metabolism of other drugs.
Azithromycin Uses:
- Prophylaxis and treatment of atypical mycobacterial infections in AIDS patients.
- Respiratory, genital, and skin infections and in Pneumonias.
- Azithromycin is preferred in Legionella pneumoniae and chlamydial infections.
Dose: Generally given as a single loading dose of 500 mg followed by 250 mg for the next 4 days.
Other Macrolides
- Dirithromycin: Dirithromycin is similar to erythromycin with some minor differences. It has better activity against C. jejuni, is acid-stable, longer acting— may be given once daily. Dose: 500 mg OD.
- Oleandomycin: Oleandomycin and troleandomycin are similar to erythromycin. Both are used in the dose of 200–500 mg QID.
- Spiramycin: Spiramycin is used in T. gondii infection to prevent transmission from the mother to the fetus.
Ketolides
Ketolides are modified macrolides that resemble newer macrolides and are effective against macrolide-resistant pneumococci.
- Telithromycin, a ketolide, is a semisynthetic derivative of erythromycin. It is effective against
- Staphylococcus aureus, S. pyogenes, S. pneumoniae, H. influenzae, H. pylori, M. catarrhalis,
- Mycoplasma, Chlamydia, T. gondii, Legionella, B. fragilis, and some mycobacteria.
Ketolides Mechanism of action:
Similar to macrolides but effective even against organisms resistant to macrolides because:
- It is not destroyed by inactivating enzymes.
- Binds to 50S ribosomes with greater affinity than macrolides.
Telithromycin is well absorbed on oral use given once daily:
- It is well-tolerated—and can cause GI disturbances; raised liver enzymes and hepatic failure have been reported.
- Due to QTc prolongation and increased risk of ventricular arrhythmias, it should be avoided in patients with prolonged QTc or receiving other drugs that prolong QTc.
- Telithromycin inhibits the microsomal enzyme CYP3A4 and can result in drug interactions.
Ketolides Uses: Community-acquired pneumonia, streptococcal pharyngitis, and sinusitis.
Miscellaneous Antibiotics
Spectinomycin:
- Spectinomycin is related to aminoglycosides and is effective against gram-negative bacteria.
- It is used only in gonorrhea (2 g IM single dose) in patients allergic to penicillin and quinolones.
Lincosamides
- Lincomycin and clindamycin are lincosamides. Lincomycin is no longer used clinically.
- Clindamycin a congener of lincomycin binds to 50S ribosomal subunit and suppresses protein synthesis like erythromycin. Streptococci, staphylococci, pneumococci, many anaerobes,
- T. gondii and P. jiroveci are inhibited.
- Well-absorbed on oral administration, attains good concentration in the bone and many other tissues. It is metabolized in the liver and excreted in the urine and bile.
Lincosamides Adverse effects:
- Include diarrhea due to pseudomembranous colitis; skin rashes and neuromuscular blockade. Intravenous use can cause thrombophlebitis.
- Dose: 150–300 mg QID.
Lincosamides Uses:
- Anaerobic infections: Abdominal, pelvic, bone, and joints infections, and aspiration pneumonia due to anaerobes are treated with clindamycin + an aminoglycoside or a cephalosporin.
- Streptococcal and staphylococcal infections: Skin and soft tissue infections including MRSA.
- P. jiroveci infection: Along with primaquine (30 mg/day), clindamycin 300 mg QID for 21 days can be used as an alternative in P. jiroveci pneumonia in AIDS patients.
- T. gondii: Clindamycin + pyrimethamine is used in toxoplasmosis in AIDS patients.
- Prophylaxis: In valvular heart disease patients undergoing minor procedures like dental procedures, clindamycin may be used as an alternative to penicillin for prophylaxis.
Glycopeptide Antibiotics
- Vancomycin and teicoplanin and their derivatives telavancin, dalbavancin, and oritavancin, are glycopeptides.
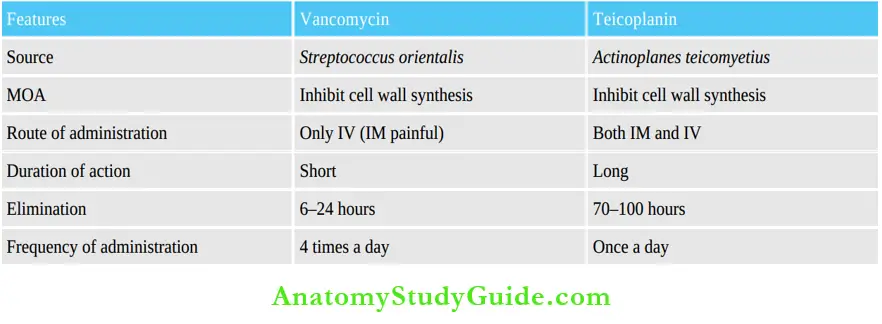
- Vancomycin, produced by Streptococcus orientalis, is active against gram-positive bacteria particularly staphylococci including those resistant to methicillin. It acts by inhibiting cell wall synthesis—it is bactericidal like penicillins.
- In addition, vancomycin also weakens the cell membrane.
Glycopeptide Antibiotics Resistance:
- Vancomycin-resistant enterococci are responsible for several nosocomial infections.
- Vancomycin-resistant S. aureus is also increasing.
Glycopeptide Antibiotics Pharmacokinetics:
- Not absorbed orally → given IV. It can be given orally for pseudomembranous colitis.
- Mostly excreted through the kidneys → ↓ dose in renal impairment.
Glycopeptide Antibiotics Adverse effects:
- Skin rashes, pain at the site of injection, thrombophlebitis, ototoxicity, and nephrotoxicity.
- Use of other ototoxic and nephrotoxic drugs should be avoided; dose should be adjusted in renal dysfunction.
Redman syndrome
- Redman syndrome IV infusion of vancomycin can provoke histamine release resulting in a maculopapular rash over the head, neck, and back with fever and chills— described as ‘Redman or red-neck syndrome’.
- This can be avoided by diluting vancomycin and injecting it as an infusion over 1–2 hours.
Glycopeptide Antibiotics Uses
- MRSA infections: For serious infections like osteomyelitis, endocarditis, and soft tissue abscesses. Dose: 30 mg/kg/day in 2–3 divided doses.
- Enterococcal endocarditis: Vancomycin + gentamicin is effective alternative to penicillin.
- Penicillin-resistant pneumococcal infections: In meningitis and other infections, vancomycin is effective and may be given with a cephalosporin.
- Pseudomembranous colitis due to C. difficile: Oral vancomycin is used 125–250 mg QID as an alternative to metronidazole.

Telavancin:
- Telavancin is a derivative of vancomycin with better efficacy against gram-negative bacteria.
- Dose: 250–750 mg IV once daily.
Teicoplanin:
- Teicoplanin obtained from Actinoplanus teichomyetius has a mechanism of action and antibacterial spectrum similar to vancomycin, but teicoplanin can be safely given intramuscularly. It is also less toxic. Half-life is 70 hours—given once daily (see Compare and Contrast) below.
- It can cause allergic reactions, fever, and ototoxicity.
Teicoplanin Uses:
- Osteomyelitis and endocarditis due to MRSA and enterococci.
- Dose: 200–400 mg/day.
Dalbavancin: Dalbavancin a derivative of teicoplanin, has the advantage of a very long half-life of 6–11 days hence given IV once a week
Ramoplanin: Ramoplanin An analog of teicoplanin, is highly active against enterococci (E. faecium and E. faecalis) and C. difficile. It is given orally (but is not absorbed) to decolonize the gut of enterococci and to treat pseudomembranous colitis due to C. difficile. It is well tolerated.
Vancomyycin and Teicoplanin:
Polypeptide Antibiotics
Polymyxin B And Colistin (Polymyxin E):
- Polymyxin obtained from Bacillus polymyxa and colistin from Bacillus colistinus, are effective against gram-negative bacteria. ‘
- Polypeptide antibiotics are not absorbed orally and are too toxic for systemic use. Hence, they were earlier not used systemically and were used only topically.
- However, due to the emergence of multidrug-resistant microbes, colistin has been used systemically (parenterally) in life-threatening infections as a last resort.
Polypeptide Antibiotics Mechanism of Action:
- Polymyxin and colistin alter the permeability of the cell membrane resulting in leakage of the cell contents.
- They are bactericidal.
Polypeptide Antibiotics Adverse effects:
- Systemic colistin causes nephrotoxicity, and interferes with neuromuscular transmission leading to weakness and apnea; also causes paraesthesias, vertigo, and dysarthria.
- Applied topically, polypeptides may rarely cause skin rashes.
Polypeptide Antibiotics Uses:
- Life-threatening infections: Colistin is used as a last resort.
- Oral colistin is used in children for diarrhea (not absorbed) due to gram-negative bacilli
- Used topically for skin infections, ear, and eye infections.
Other Antimicrobial Agents
1. Bacitracin:
- Bacitracin, produced by Bacillus subtilis, is effective against gram-positive bacteria. It inhibits cell wall synthesis and is bactericidal.
- It is too toxic to be given systemically, not absorbed orally, and is, therefore, used only for topical application— in skin infections, surgical wounds, ulcers, and ocular infections.
2. Sodium fusidate (fusidic acid):
- Sodium fusidate obtained from Fusidium coccineum, is effective against gram-positive organisms, particularly staphylococci. It is bactericidal.
- It is mainly used topically as a 2% ointment. It may be given orally for resistant staphylococcal infections.
3. Mupirocin:
- Mupirocin or pseudomonic acid is obtained from Pseudomonas fluorescens. It is bactericidal against gram-positive and some gram-negative organisms including MRSA.
- Mupirocin acts by inhibiting the enzyme tRNA synthetase. It is used as a 2% ointment for minor skin infections particularly due to staphylococci and streptococci.
- It is also used intranasally as a spray to eradicate the staphylococcal carrier state.
4. Fosfomycin:
- Fosfomycin is an analog of phosphoenol pyruvate, effective against both gram-positive and gram-negative organisms.
- It acts by inhibiting the enzyme endo pyruvate transferase.
- This enzyme is required for the first step in bacterial cell wall synthesis. Thus it inhibits bacterial cell wall synthesis.
- It is available for both oral and parenteral use. It is excreted by the kidneys and attains a high concentration in the urine.
- Fosfomycin is approved for use in uncomplicated lower UTI in women—a single 3 g dose is effective.
- Dose: 3 g in 100 mL water.
5. Cycloserine:
- Cycloserine obtained from Streptomyces orchidaceus inhibits many gram-positive and gram-negative organisms including M. tuberculosis.
- It is used as a second-line drug in tuberculosis.
6. Streptogramins:
- Quinupristin and dalfopristin are obtained from Streptomyces pristinaspiralis (also called pristinamycin).
- A combination of quinupristin (streptogramin B) and dalfopristin (streptogramin A) in the ratio of 30:70 is bactericidal against gram-positive cocci including MRSA.
Streptogramins Mechanism of action:
Streptogramins bind to the 50S ribosomal subunit and inhibit protein synthesis.
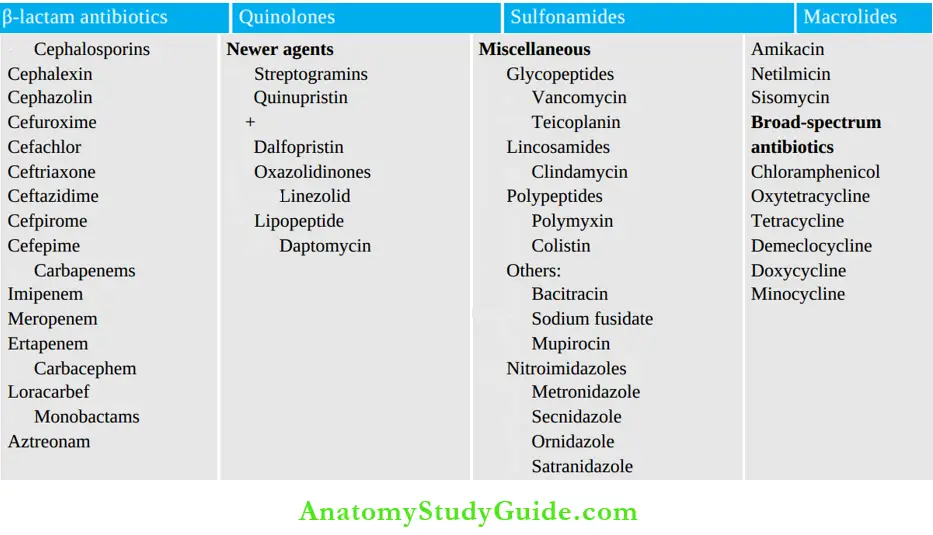
Groups of Antimicrobial agents:

Streptogramins Pharmacokinetics:
- Streptogramins are not effective orally; given IV, they are rapidly metabolized and are excreted largely through feces.
- Hence, dose adjustment is not required in renal insufficiency but in hepatic failure, the dose should be reduced.
- Streptogramins inhibit the microsomal enzyme → hence drug interactions can occur.
Streptogramins Adverse effects: Arthralgia, myalgia, nausea, vomiting, diarrhea, and pain at the injection site.
Streptogramins Uses:
- The combination is used IV in infections due to streptococci, MRSA, enterococci, and vancomycin-resistant E. faecium.
- Dose: 7.5 mg/kg every 8–12 hours.
7. Oxazolidinones:
- Linezolid is effective against gram-positive bacteria including MRSA, gram-positive anaerobes, and tubercle bacillus. It acts by inhibiting protein synthesis on binding to 50S ribosomes.
- Linezolid binds to the 23S ribosomal RNA of the 50S subunit and prevents initiation of protein synthesis—the first step in protein synthesis.
- Though a bacteriostatic agent, linezolid is bactericidal against streptococci.
Oxazolidinones Advantages:
- Good oral bioavailability—completely absorbed
- Food does not interfere with its absorption.
- It can be given orally or by IV.
- Dose: 600 mg BD.
Oxazolidinones Adverse effects:
- Including nausea, diarrhea, dizziness, and prolonged use of >2 weeks can cause myelosuppression with thrombocytopenia (which is reversible), anemia and neutropenia; peripheral neuropathy, and lactic acidosis.
- Cheese reaction—linezolid is an
- MAO inhibitors can cause serotonin syndrome with other drugs that increase serotonin levels or with tyramine-rich food.
Oxazolidinones Uses:
- Nosocomial pneumonia by S. aureus including MRSA 600 mg BD–IV oral.
- Community-acquired pneumonia—due to S. pneumoniae response.
- Skin and skin structure infections and septicemia due to Streptococcus and Staphylococcus.
- Vancomycin-resistant E. faecium infections due to multidrug-resistant bacteria.
- MDR tuberculosis with other drugs.
- Nocardiosis: As an alternative.
- Tedizolid: Is longer acting (once daily dose) and has better efficacy against staphylococci.
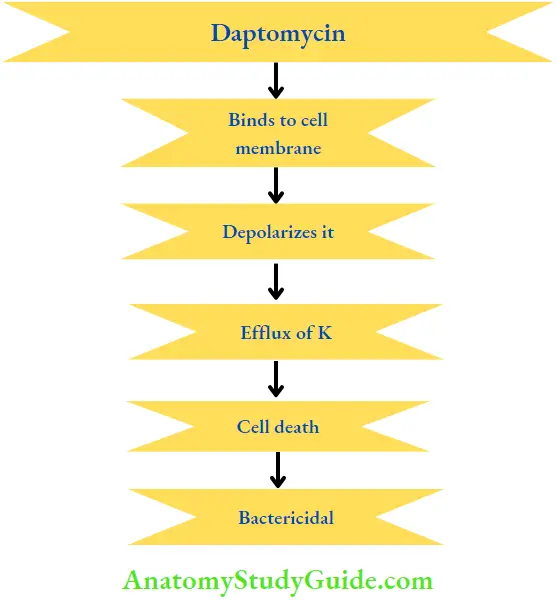
8. Daptomycin:
- Daptomycin is a lipopeptide obtained from Streptomyces roseosporus. It is bactericidal for most susceptible microorganisms and multidrug-resistant streptococci.
- Daptomycin has a unique mechanism of action.
- It binds to the cell membrane and depolarises it. This leads to the outward movement of potassium ions resulting in rapid cell death. Daptomycin is thus bactericidal. It is synergistic with gentamicin.
Oxazolidinones Antibacterial spectrum:
- Aerobic gram-positive microorganisms (including MRSA and VRSA) and anaerobes.
- Because absorption on oral administration is poor, daptomycin is given IV. It is not given intramuscularly as it causes direct toxicity to the muscle.
- Daptomycin can cause myopathy, peripheral neuropathy, headache, insomnia, dizziness, jaundice and GI disturbances. It should not be used to treat pneumonia because surfactant in the lungs antagonizes the effects of daptomycin.
- Dose: 4–6 mg/kg/day.
Oxazolidinones Uses:
- In complicated skin and soft tissue infections.
- As an alternative to vancomycin.
9. Fidaxomicin:
- Fidaxomicin is a narrow-spectrum antibiotic effective against gram-positive bacteria. It binds to RNA polymerase and inhibits protein synthesis.
- Given orally, it is poorly absorbed and is effective in the treatment of colitis due to C. difficile.
- Dose: 200 mg BD.
Drugs Used In The Treatment Of Sexually Transmitted Diseases
Drugs used in the treatment of STDs have all been described in the respective chapters. Some of them have been summarized in Table.
Drugs used in some common sexually transmitted diseases:

Chemoprophylaxis:
- For the postexposure prophylaxis of syphilis and gonorrhea, penicillin 4–8 MU IM into the gluteal region is effective.
- Alternatively, doxycycline 100 mg BD for 15 days can be used for the prophylaxis of gonorrhea, syphilis, granuloma inguinale, LGV, and chancroid.
Chemotherapy Of Tuberculosis:
- Tuberculosis (TB) is a chronic granulomatous disease caused by Mycobacterium tuberculosis.
- India has the highest number of TB cases in the world, accounting for ~1000 deaths everyday, a major public health problem.
- After the spread of AIDS, the problem has become more complex, as tuberculosis and
- Mycobacterium avium complex (MAC) infections are not only more common but also rapidly progressing in these patients.
Leave a Reply