Atresia And Stenosis
- Commonly, it affects the duodenum, followed by ileum and jejunum
- There may be single/multiple atresia.
- Incidence: 1 in 10,000 live births.

Table of Contents
Duodenal Atresia
Duodenal Atresia Types
Type 1:
- Complete atresia—it is the commonest atresia.
- The proximal dilated segment and distal collapsed segment are completely separated.
Type 2:
- There is no separation of the two parts.
- However, a fibrous band is in between.
Type 3: It is incomplete obstruction: There may be a web or stenosis.
Duodenal Atresia – Associated Lesions
- Annular pancreas, incomplete rotation of the gut
- Down’s syndrome (trisomy 21)
- Maternal hydramnios
- Congenital heart disease
- Anorectal malformation
Windsock deformity: An incomplete diaphragm, with central aperture (hole) with proximal dilatation
- Anastomosis: A special anastomosis named after Kimura is being described. It is a diamond-shaped anastomosis between upper pouch (duodenum) which is opened transversely and lower pouch (distal duodenum) which is opened longitudinally.
- Needless to mention here that general condition has to be taken care of with supportive therapy including fluid and electrolytes, total parenteral nutrition, nasogastric decompression and adequate urinary output.
- Clinical features of obstruction manifest within 48–72 hours in the form of obstruction.
- Atresia means imperforation; stenosis means narrowing.
- Duodenal atresia presents as vomiting with or without bile, minimal distension and visible gastric peristalsis.
- Jaundice
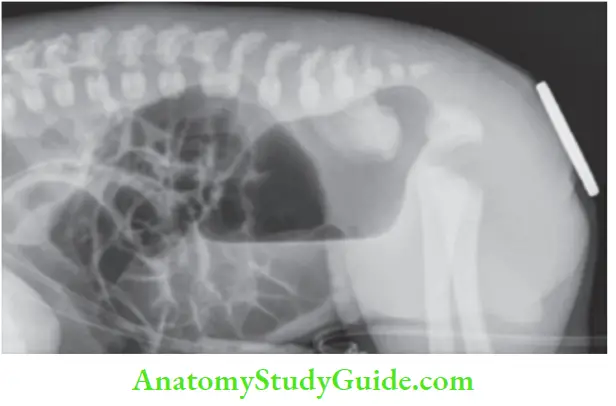
- X-ray abdomen erect: Double-bubble in duodenal atresia.
Duodenal Atresia Treatment
- Duodenal atresia: Duodenojejunostomy by anastomosing dilated duodenum above the atresia to the jejunal loop.
Small Intestinal Atresia
Salient Features:
- It can affect the jejunum (common) or ileum.
- Like duodenal atresia, it can be associated with maternal hydramnios or malrotation of the gut.
- Exact reasons for atresia are not known. However, vascular variations in the mesentery such as
- V-shaped mesentery or due to occlusion of vessels in the intrauterine life are the possible factors.
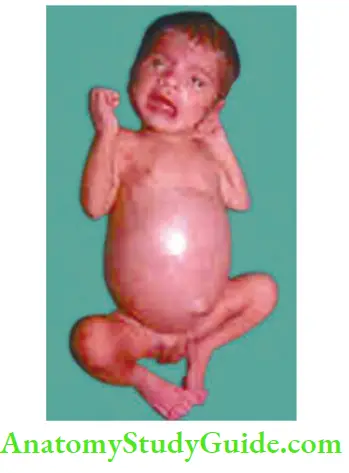
- Like any obstruction, the proximal bowel is dilated and distal bowel is collapsed. The colon is very small— microcolon.
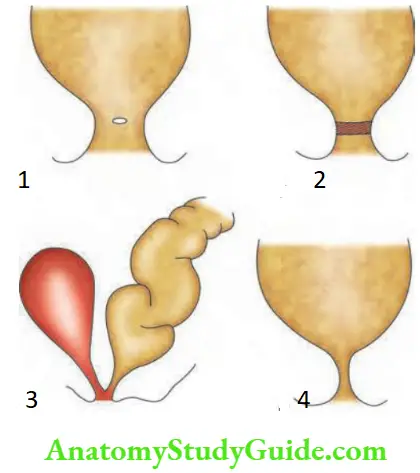
Gries Field Modification Of Martin’S Classification
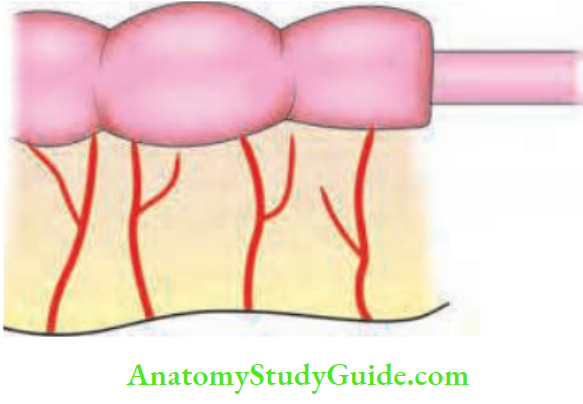
- Type 1: Simple stenosis. Mesentery is normal. It is mucosal atresia.
- Type 2: Proximal and distal bowels are connected by a fibrous band which has no lumen—atretic segment. Here again, mesentery is normal
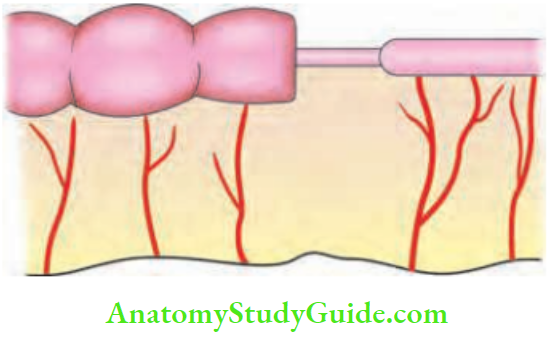
- Type 3: Further divided into 2 types. 3a refers to atresia with V-shaped loss of mesentery in between,3b refers to complete jejunal atresia with coiled ileum. It has been called Christmas tree deformity.
- Type 4: Multiple atretic segments including mesentery.


Please note:
- Apple-peel or Christmas tree deformity. Here, obstruction is usually in the proximal jejunum, which is supplied by the entire superior mesenteric artery (SMA).
- This results in a gap in the mesentery. So, rest of the small intestine is coiled around the ileocolic branch of the SMA.
Martin’s Classification Treatment: Laparotomy, division of band and fixation of the caecum in the right iliac fossa.
Arrested Rotation With Bands
- It is a congenital anomaly wherein the caecum and right colon are found on the left side.
- As a result of this, there are peritoneal bands which run across from left to right and cause intestinal obstruction (duodenal obstruction).
- One such band is called the transduodenal band of Ladd which compresses the second part of the duodenum and gives rise to obstruction (features similar to duodenal atresia).
- Differential diagnosis is duodenal atresia.
Arrested Rotation With Bands Treatment: Laparotomy, division of band and fixation of the caecum in the right iliac fossa.

Volvulus Neonatorum
Volvulus neonatorum—it is a complication of arrested rotation with bands which pre-disposes to midgut volvulus (small bowel). These unfortunate infants undergo massive resection of the bowel if it is gangrenous.
Such massive resections give rise to short gut syndrome. Thus, the patient becomes a digestive cripple. If the loop is not gangrenous, it is treated by laparotomy, untwisting of bowel and division of bands.

Meconium Ileus
Meconium ileus—it is a neonatal manifestation of mucoviscidosis of the pancreas wherein the mucus is thick and viscid. This, along with meconium, produces obstruction. There may be ileal atresia, which might have precipitated meconium ileus.
- The majority of meconium ileus is coupled by complications such as gangrene, perforation and peritonitis. As a sequel to peritonitis, calcification and adhesive meconium obstruction develop.
- Infants present with abdominal distension, bilious vomiting and failure to pass meconium.
- Plain X-ray shows distended bowel and mottling due to calcification.
- Soap bubble sign or Neuhauser’s sign: Ground glass appearance in the right lower quadrant due to viscid meconium mixed with air.
- Ultrasonography: Dilated loops of bowel filled with echogenic material are highly suggestive of meconium ileus rather than ileal atresia.
- If perforation is ruled out, barium enema can be done which shows microcolon.
Meconium ileus Treatment
1. Conservative Treatment:
- It is indicated if there is no peritonitis, the general condition of the child is reasonably good or if there is partial obstruction. Dilute gastrograffin is introduced into the colon as enema.
- It fills up terminal ileum. It absorbs fluid from the interstitial space into the lumen because it is hyperosmolar.
- Consequently, the meconium becomes soft and it is rejected naturally. Hypervolaemia is to be corrected during this.
2. Nonresectional Procedures:
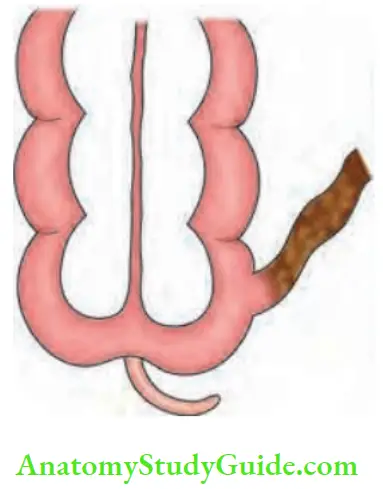
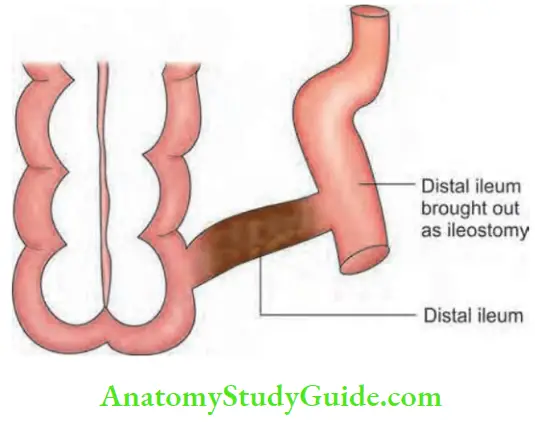
Bishop-Koop operation:
- Ileum is divided in the proximal healthy part.
- This proximal ileum is anastomosed to the ascending colon to relieve obstruction—end-to-side anastomosis.
- Distal ileum containing thick meconium pellets is brought outside as a fistula and regular saline washes are given to dilute the meconium. Mucous fistula needs to be closed after a few weeks.
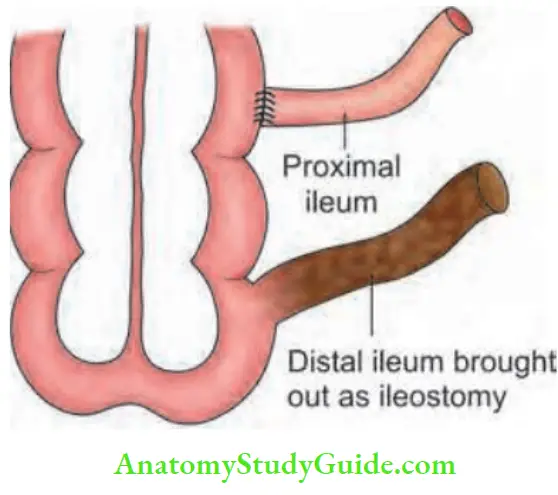
Santulli operation :
- In this operation, the proximal ileum is brought out as ileostomy.
- Distal ileum is anastomosed to proximal ileum as end-to-side anastomosis.
Resection:
- Resection is the surgery of choice today as more cases present with short segment obstruction.
- Long-term results and complications are much less than in nonresectional procedures.
Anorectal Anomalies
Developmental Anatomy
- To start with, there is a common chamber called the cloaca, which is later divided into 2 chambers, anteriorly allantois gives rise to the urinary bladder and posteriorly, postallantoic gut gives rise to rectum and upper 2 cm of anal canal.
- Postallantoic gut fuses with proctodeum, thus giving rise to anal canal. If there is a defective fusion of this, it results in imperforate anus.
Imperforate Anus
Incidence: 1:4500 live births. Common in female children.
Imperforate Anus Types:
1. Low anomalies: It refers to the termination of the bowel below the anorectal bundle.
- Covered anus: The anal orifice is covered by a tag of skin.
- Membranous anus: Covered with a thin membrane.
- Anterior ectopic anus: Anus is situated anteriorly.
- Stenosed anus: Anal orifice is microscopic.

2. High anomalies: They are supra levator—the bowel terminates above the anorectal bundle.
- Anorectal and agenesis, with fistula: Rectovesical, rectovaginal, rectourethral fistulae
Imperforate Anus Diagnosis
- 12 hours after birth, the child is put in the prone position (12 hours is the time for the gas shadow to reach the distal portion of the gut). A metal coin is strapped to the site of anus and an X-ray is taken. If the gas shadow is above the pubococcygeal line, it is a high anomaly.
- If the distance between the coin and gas shadow is more than 2.5 cm, it is a high anomaly. If the gas shadow is below the pubococcygeal line, it is a low anomaly. Pubococcygeal line is called Stephen’s line.
Imperforate Anus Treatment
- Low anomaly: Easy to treat, division of membrane or skin followed by dilatation is all that is required with some amount of plastic reconstruction (anoplasty is necessary)
- High anomaly: Repaired by 3-stage procedure:
- 1st stage: Preliminary transverse colostomy to relieve intestinal obstruction.
- 2nd stage: When the child is 8–10 kg of weight, a “pull-through” operation is done with the division of fistula.
- 3rd stage: After 2 months, colostomy is closed.
Causes Of Intestinal Obstruction As Per Age
Neonates: o To 7 days:
- Atresia and stenosis
- Hirschsprung’s disease
- Arrested rotation with bands
- Volvulus neonatorum
- Meconium ileus
- Imperforate anus
Young Patients: Up to 30 Years:
- Obstructed hernia
- Adhesions
- Tuberculous stricture ileum
- Crohn’s disease of the ileum
- Tuberculous peritonitis with adhesions
- Meckel’s diverticulum with band
- Adult intussusception
Middle-aged Patients: 30–60 Years:
- Adhesions
- Obstructed hernia
- Carcinoma left colon
- Diverticulosis with stricture left colon
- Gallstone ileus
- Sigmoid volvulus
- Mesenteric vascular occlusion
- Adult intussusception
Paralytic Ileus (Neurogenic Ileus)
In this condition, there is a failure of transmission of parasympathetic impulses from one segment to the other. That means, there is a failure of the parasympathetic mechanism, which results in paralysis of the bowel. It gives rise to a large collection of fluid and gas within the bowel resulting in distension.
Paralytic Ileus Causes/ Etiology
- During surgery, stimulation of sympathetic nerves that inhibits gastrointestinal movement results in autonomic nervous system dysfunction(s) causing ileus.
- In sepsis, a few inflammatory mediators like nitric oxide, prostaglandins, and vasoactive intestinal peptide-VIP are released.
- They cause some motility problems to the gut. Inflammation also results in leukocyte infiltration and this factor also adds to paralytic ileus.
- Hypokalaemia: Potassium is responsible for depolarization in nerve cells that innervate muscle of the small intestines, hence hypokalemia causes paralytic ileus.
- Hypocalcaemia: Calcium is associated with smooth muscle contraction, hence hypocalcaemia can give rise to paralytic ileus (it is uncommon).
- Metabolic: Uraemia, diabetes (gastropathy).
- Drugs: Central-acting drugs—loperamide, phenothiazine, tricyclic antidepressants, and anti-Parkinson’s drugs. Peripherally acting drugs—anticholinergic group, calcium-channel blocker group (example, verapamil), alpha-2 adrenergic agonist group (example, clonidine), etc.
Paralytic Ileus Clinical Features
- Abdominal distension is gross: Tympanitic note all over is a feature. Respiratory and cardiac functions are impaired.
- No colicky pain abdomen: (In dynamic obstruction, colicky pain is a feature). Dull pain occurs due to distension of the abdomen.
- Failure to pass flatus: Effortless vomiting is also characteristic of paralytic ileus.
- On auscultation: Tinkling sounds are heard due to shift of fluid from one coil of bowel to the other
- Severe fluid: Electrolyte and protein depletion occur.
Paralytic Ileus Investigations
- Plain X-ray abdomen demonstrates distended loops of bowel.
- Electrolyte study and correction of any abnormality.
Paralytic Ileus Treatment:
Basic principle of treating paralytic ileus is drip and suction.
The cause of paralytic ileus has to be treated first, example if there is hypokalaemia, supplement potassium.
- If there is pus in the peritoneal cavity, drain it.
- Ryle’s tube aspiration, to give rest to the gut.
- Intravenous fluids, supplementation of ions, correction of dehydration, oliguria, etc. Such treatment is continued for 3–4 days.
- Ryle’s tube is removed when abdomen is soft, bowel sounds are heard and the patient has passed flatus. Clear oral fluids are started for 2–3 days followed by soft diet.
- Small bowel activity returns within 12–18 hours, followed by colon which starts functioning within 36– 48 hours.
- However, gastric functions may return ranging from 18 hours to 4 days.







Three Types of Bowel Sounds:
- Normal: Once in 20 seconds, low pitch.
- Borborygmi: Loud, noisy, which occurs once in 5–10 seconds.
- Tinkling sounds: Mild metallic sounds as in paralytic ileus.
Leave a Reply