Blood Vessels and Cardiovascular System
Question 1. Write a short note on heart failure cells and the conditions associated with it.
Answer:
To learn this entity, one should be thorough with left heart failure and its predisposing conditions.
Left heart failure
Causes: Ischemic heart disease, hypertension, aortic and mitral valvular diseases, primary myocardial diseases
Read and Learn More Preparatory Manual of Pathology Question and Answers
Effects of left-sided heart failure
- Blood backing up in the pulmonary circulation
- Stasis of blood in left-sided chambers
- Inadequate perfusion of downstream tissues leads to organ dysfunction
Morphology
Heart
- The left ventricle is hypertrophied and dilated
- Impaired left ventricle function, which predisposes to atrial fibrillation
Lungs
- Peri-vascular and interstitial edema, responsible for the characteristic Kerley B and C lines on chest X-ray
- Accumulation of edema fluid in alveolar spaces and widening of the alveolar septae
- Alveolar macrophages within alveolar spaces engulf hemosiderin and result in the formation of hemosiderin-laden macrophages (heart failure cells)
- Heart failure cells are stained by Perl’s/Prussian blue stain
Question 2. Write a short note on cor pulmonale.
Answer:
Pulmonary (right-sided) hypertensive heart disease (cor pulmonale)
- Occurs due to the right ventricular pressure overload
Chronic cor pulmonale
- Causes: Chronic parenchymal lung diseases such as emphysema, and primary pulmonary hypertension
- Characterized by right ventricular hypertrophy, dilation, and right-sided failure
- The right ventricular wall thickens, up to 1.0 cm or more
Acute cor pulmonale
- Can follow massive pulmonary embolism
- Characterized by marked dilation of the right ventricle without hypertrophy
- Cross-section: The normal crescent shape of the right ventricle is transformed into a dilated ovoid shape
Question 3. Write a short note on the tetralogy of Fallot.
Answer:
Tetralogy of Fallot (TOF)
4 cardinal features of TOF
- Ventricular septal defect
- Obstruction of the right ventricular outflow tract (sub-pulmonary stenosis)
- An aorta that overrides the ventricular septal defect (VSD)
- Right ventricular hypertrophy
Morphology
- Boot-shaped heart—due to marked right ventricular hypertrophy
- Large VSD, with the aortic valve at the superior border
- Right ventricular outflow tract obstruction—due to sub-pulmonic stenosis or pulmonary valvular stenosis
- The right aortic arch is present in 25% of cases
Clinical features
- Classic TOF—severe right ventricular outflow tract obstruction, leads to right-to-left shunting, producing cyanosis
- Pink tetralogy—left to right shunt, mild sub-pulmonary stenosis, does not produce cyanosis
Question 4. Write a short note on the coarctation of the aorta.
Answer:
Coarctation of aorta
- Male:Female:: 2:1
- Two forms: Infantile form and adult form
1. Coarctation of the aorta with PDA (infantile form)
- Produces signs and symptoms immediately after birth
- There occurs tubular hypoplasia of the aortic arch, which occurs proximal to patent ductus arteriosus
- Presents as cyanosis localized to the lower half of the body
2. Coarctation of the aorta without a PDA (adult form)
- Asymptomatic in childhood presents in adult life
- Presents as a ridge-like infolding of the aorta just opposite the closed ductus arteriosus (ligamentum arteriosum)
- Can cause hypertension in the upper extremities and hypotension in the lower extremities
X-ray finding: Development of collateral circulation between pre-coarctation and post-coarctation arteries (through enlarged inter-coastal and internal mammary arteries), thus producing notching of the undersurfaces of ribs.
Question 5. Define atherosclerosis. Discuss the morphology of atheroma, risk factors and complications associated with atherosclerosis.
Answer:
Definition: Atherosclerosis is characterized by intimal lesions called atheromas, or atheromatous or fibrofatty plaques, which protrude into and obstruct vascular lumens and weaken the underlying media.
Risk factors:
- Non-modifiable risk factors: Age: 40–60 years, Sex: M > F, genetic predisposition
- Modifiable risk factors: Hyperlipidemia, hypertension, cigarette smoking, diabetes mellitus
- Inflammation: Increased CRP expression is a risk factor for MI, stroke, and peripheral arterial disease. CRP is produced in the liver and is stimulated by increased IL-6 levels
- Hyperhomocysteinemia (>100 mol/L), sedentary lifestyle, obesity, type A personality
Morphology of an Atheroma
- Fibrous cap: Composed of smooth muscle cells (SMCs), connective tissue, a few leucocytes
- Shoulder (cellular area beneath and to the side of the cap): Composed of smooth muscle cells, macrophages, lymphocytes
- Necrotic zone: Disorganized mass of lipid material, cholesterol clefts, cellular debris, lipid-laden foam cells, fibrin, thrombin
- Neovascularisation at the periphery
Atherosclerotic plaques can undergo the following pathological changes:
- Rupture, ulceration, or erosion in a plaque exposes highly thrombogenic substances and leads to thrombosis which may occlude the vessel lumen
- Hemorrhage into a plaque: Occurs due to the rupture of the overlying fibrous cap, or thin-walled vessels in the areas of neovascularization
- Embolism: Plaque rupture can produce thromboembolism
- Aneurysm formation: Atherosclerosis-induced pressure atrophy of the underlying media
Consequences of atherosclerotic disease:
- Myocardial infarction, cerebral infarction, aortic aneurysms, and peripheral vascular disease (gangrene of the legs)
Question 6. Write a short note on aneurysms.
Answer:
Aneurysm
Definition: Localized abnormal dilation of the blood vessel or heart
Types
1. True aneurysm:
- Aneurysm involving thinning out the intact arterial wall or thinned ventricular wall of the heart
- Examples: Atherosclerotic, syphilitic, congenital vascular aneurysms or the ventricular aneurysms that follow transmural myocardial infarctions
2. False aneurysm (pseudoaneurysm):
- A defect in the vascular wall leads to an extravascular hematoma, which communicates within the intravascular space
- Example: Ventricular rupture after myocardial infarction, contained by a pericardial adhesion
Classification of aneurysms
- Saccular aneurysms: Spherical outpouching involving only a portion of the vessel wall; can vary from 5 to 20 cm in diameter and often contain thrombus
- Fusiform aneurysms: Diffuse, circumferential dilation of a long vascular segment; can vary up to 20 cm in diameter
Causes
- The two most important causes of aortic aneurysms are atherosclerosis and hypertension
- Atherosclerosis is a risk factor for abdominal aortic aneurysms
- Hypertension is the most common etiology associated with ascending aortic aneurysms
- Other causes: Trauma, vasculitis, fibromuscular dysplasia, infections (mycotic aneurysms)
Question 7. A 50-year-old man collapses suddenly while climbing the stairs with severe chest pain and profuse sweating.
1. What is your clinical diagnosis?
2. Enlist the biochemical tests and their role in the diagnosis of this disease.
3. Discuss the evolution of morphologic changes in myocardial infarction.
Answer:
1. Myocardial infarction
2. Lab findings in myocardial ischemia
- Measuring blood levels of proteins that leak out of irreversibly damaged myocytes
- Most useful of these molecules are cardiac-specific troponins T and I (cTnT and cTnI), and CK-MB
- Most sensitive and specific biomarkers of myocardial damage are cardiac-specific proteins, particularly cTnT and cTnI
- Troponins I and T are not normally detectable in the circulation
1. Troponin T:
- Begins to rise within 3–12 hours of the onset of MI, peaks at 12–48 hours, and returns to normal within 5–14 days
2. Troponin I:
- Begins to rise within 3–12 hours of the onset of MI, peaks at 24 hours, and returns to normal within 5–10 days
3. Creatinine kinase MB:
- Begins to rise within 3–12 hours of the onset of MI, peaks at 24 hours, and returns to normal within 48 to 72 hours
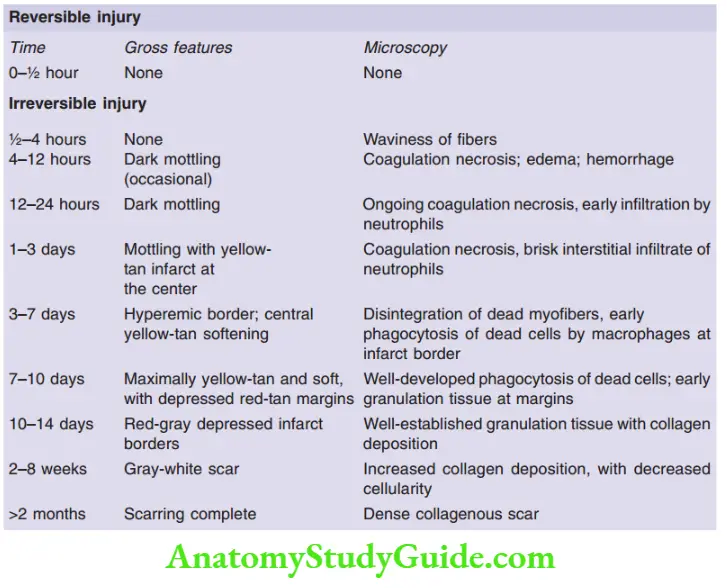
Evolution of morphological changes in myocardial infarction:
Question 8. Enumerate the complications following myocardial infarction.
Answer:
Complications following acute myocardial infarction
- Contractile dysfunction—leads to left ventricular failure, cardiogenic shock
- Arrhythmias—sinus bradycardia, heart block (asystole), tachycardia, ventricular premature contractions or ventricular tachycardia and ventricular fibrillation
- Myocardial rupture—anterolateral ventricular free wall (most common), ventricular septum (less common), and papillary muscle (least common)
- Pericarditis – fibrin hemorrhage pericarditis (Dressler syndrome)
- Mural thrombus and thromboembolism
Question 9. Discuss etiopathogenesis, pathologic lesions, laboratory diagnosis, clinical features, and complications of rheumatic heart disease (RHD).
Answer:
Rheumatic fever (RF)
- Multisystem inflammatory disorder occurring within a few weeks after an episode of group A streptococcal pharyngitis
- Involves most commonly mitral valve
- RHD is the only cause of mitral stenosis
Pathogenesis
- Results from host immune responses to group A streptococcal antigens
- Antibodies and CD4+ T cells against these antigens can cross-react with cardiac self-antigens
- The binding of the antibody can activate complement, macrophages, and neutrophils
- Also seen is the cytokine-mediated macrophage activation (within Aschoff’s body)
Morphology
In acute RF, focal inflammatory lesions are seen
- Aschoff bodies: These consist of T-lymphocytes, plasma cells, and plump activated macrophages called Anitschkow cells (pathognomonic for RF)
- Macrophages have abundant cytoplasm and central round-to-ovoid nuclei in which the chromatin condenses into a central, slender, wavy ribbon (“caterpillar cells”)
- Pancarditis: Inflammation and Aschoff bodies can be seen in the endocardium, pericardium, and myocardium
- Endocardium: 1–2 mm vegetations along the lines of closure of valve called verrucae
- MacCallum plaques: Irregular thickenings seen in subendocardial regions in the left atrium
Clinical features
- Major manifestations
- Migratory polyarthritis of the large joints
- Pancarditis
- Subcutaneous nodules
- Erythema marginate of the skin
- Sydenham chorea (involuntary rapid, purposeless movements)
Minor manifestations:
- Fever, arthralgia, or elevated blood levels of acute phase reactants
Diagnosis requires 2 major manifestations or one major and two minor manifestations, with evidence of preceding group A streptococcal infection
Complications
- The mitral valve in chronic RHD: Leaflet thickening, commissural fusion, thickening and fusion of the chord tendineae
- “Fish mouth” or “buttonhole” stenosis: Of the mitral valve is a characteristic feature of RHD.
Question 10. Discuss etiopathogenesis and morphology of heart lesions in infective endocarditis.
Answer:
Infective endocarditis
- Characterized by microbial infection of the heart valves or the mural endocardium
- Results in the formation of vegetation composed of thrombotic debris and organisms, associated with the destruction of the underlying cardiac tissues
- The most common etiology—bacterial
Etiology and pathogenesis
- Predisposing factors: Rheumatic heart disease (in the past), mitral valve prolapse, calcific valvular stenosis, bicuspid aortic valve
- Staphylococcus aureus can infect healthy or deformed valves
- Staphylococcus aureus is the major offender among intravenous drug abusers
- Streptococcus viridian infects deformed valves or previously damaged valves
- Staphylococcus epidermis—predisposes to prosthetic valve endocarditis
- HACEK group (Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella) and enterococci also lead to IE
Morphology
- Vegetations on heart valves are the classic hallmark of IE
- Vegetations are friable, bulky, potentially destructive lesions containing fibrin, inflammatory cells, and bacteria
- Most common sites of infection: Aortic and mitral valves
- Ring abscess: Vegetations can be single or multiple and can ride into the underlying myocardium and produce an abscess
- Vegetations are prone to embolization
- Septic infarcts or mycotic aneurysms: Abscesses develop at the sites, where the emboli lodge
Question 11. Write a short note on Libman-Sacks endocarditis.
Answer:
Libman-Sacks disease
- Seen rarely in SLE
- Characterized by small, sterile vegetations on mitral and tricuspid valves
- Vegetations are small (1 to 4 mm in diameter), single or multiple, sterile with a warty (verrucous) appearance
- Vegetations are located on the undersurfaces of the atrioventricular valves, on the valvular endocardium, on the chords, or on the mural endocardium of atria or ventricles
- Libman-Sacks endocarditis: When the vegetations are associated with fibrinoid necrosis of the valve substance (valvulitis)
Question 12. Write a note on dilated cardiomyopathy, with a mention of its morphology and complications.
Answer:
Dilated cardiomyopathy (DCM)
- Characterized by progressive cardiac dilation and systolic dysfunction, with concomitant hypertrophy
Pathogenesis
1. Genetic influences
- Mutations in TTN, a gene that encodes titin account for 20% of all cases of DCM
- The most common inheritance pattern is autosomal dominant (AD)
2. Myocarditis
- Coxsackie B virus
3. Alcohol abuse: Alcohol and its metabolite, acetaldehyde is toxic to myocardium
4. Drugs: Doxorubicin, cobalt, tyrosine kinase inhibitors
5. Childbirth
- Peripartum cardiomyopathy can occur late in pregnancy
- Because of ischemic injury to the myocardium
6. Iron overload
7. Supraphysiologic stress: Persistent tachycardia, hyperthyroidism, in the fetuses of insulin-dependent diabetic mothers
Morphology
- The heart is enlarged, heavy (often weighing two to three times normal), and flabby, due to the dilation of all chambers
- Mural thrombi are common
- Most of the muscle cells are hypertrophied with enlarged nuclei
- Interstitial and endocardial fibrosis is present
Question 13. Enumerate the causes of myocarditis. Discuss its morphological features.
Answer:
Major causes of myocarditis
1. Infections
- Viruses (for example coxsackievirus, influenza, HIV, cytomegalovirus)
- Chlamydiae (example Chlamydia psittaci)
- Rickettsiae (for example Rickettsia typhi, typhus fever)
- Bacteria (for example Corynebacterium diphtheriae, Neisseria meningococcus, Borrelia, Lyme disease)
- Fungi (for example Candida)
- Protozoa (for example Trypanosoma Cruz [Chagas disease], toxoplasmosis)
- Helminths (for example trichinosis)
2. Immune-mediated reactions
- Postviral
- Poststreptococcal (rheumatic fever)
- Systemic lupus erythematosus
- Drug hypersensitivity (for example methyldopa, sulfonamides)
- Transplant rejection
3. Unknown
- Sarcoidosis
- Giant cell myocarditis
Morphology
- Active myocarditis: Diffuse, mononuclear cell (lymphocyte) infiltrate is seen
- Hypersensitivity myocarditis: Interstitial infiltrates, composed of lymphocytes, macrophages, and eosinophils
- Giant cell myocarditis: Characterized by a widespread inflammatory infiltrate containing multinucleate giant cells (fused macrophages) interspersed with lymphocytes, eosinophils, plasma cells, and macrophages with focal to extensive necrosis
- Myocarditis in Chagas disease: Myofibers are distended with trypanosomes
Question 14. Write a short note on cardiac myxoma.
Answer:
Myxomas
- The most common primary tumor of the adult heart
- Arises from primitive multipotent mesenchymal cells
- 90% arise in the atria, most commonly in the left atria
Morphology
- Can be single or multiple
- Site: Fossa oval in the atrial septum
- Size: Varies from <1 cm to 10 cm, can be sessile or pedunculated lesions
- Gross: Globular hard masses with hemorrhagic to soft, translucent, papillary, or villous lesions
- Microscopy: Myxomas are composed of stellate or globular myxoma cells, which are embedded in an abundant mucopolysaccharide ground substance. Peculiar vessel-like or gland-like structures are characteristic
- Hemorrhage and mononuclear inflammatory cell infiltrate are present
Question 15. Classify vasculitis and write a short note on Takayasu’s arteritis.
Answer:
1. Large vessel vasculitis
- Giant cell arteritis
- Takayasu arteritis
2. Medium vessel vasculitis
- Polyarteritis nodosa
- Kawasaki disease
3. Small vessel vasculitis
1. ANCA-associated vasculitis: Microscopic polyangiitis, Wegener granulomatosis, Churg-Strauss syndrome
2. Immune complex-mediated vasculitis: SLE, Henoch-Schönlein purpura, cryoglobulin vasculitis, Goodpasture’s disease
Takayasu arteritis
- Age group: Less than 50 years
- Granulomatous vasculitis of medium and larger arteries
- Characterized by ocular disturbances and marked weakening of the pulses in the upper extremities (pulseless disease)
Morphology
- Involves the aortic arch, pulmonary artery, coronary and renal arteries
- Microscopically, tunica media is destroyed by mononuclear inflammatory cells and giant cells
Clinical features
- Reduced blood pressure and weak pulses in carotids and upper extremities, ocular disturbances, total blindness, neurologic deficits
- Claudication of the legs, pulmonary hypertension
Question 16. Write a short note on microscopic polyangiitis.
Answer:
Microscopic polyangiitis
- Also called hypersensitivity vasculitis or leukocytoclastic vasculitis
- Necrotizing vasculitis affecting the capillaries, small arterioles, and venules
- All lesions tend to be of the same age in the patient
- Necrotizing glomerulonephritis and pulmonary capillaritis are common
Associations
- Henoch-Schönlein purpura, essential mixed cryoglobulinemia, and vasculitis associated with connective tissue disorders
Pathogenesis
- Associated with MPO-ANCA
Morphology
- Leukocytoclastic vasculitis: Fragmentation of neutrophils in and around blood vessel walls
- Focal fibrinoid necrosis or transmural inflammation can be seen
Clinical features
- Hemoptysis, hematuria and proteinuria, bowel pain or bleeding, palpable cutaneous purpura
Question 17. Write a short note on Wegener granulomatosis.
Answer:
Granulomatosis with polyangiitis (Wegener granulomatosis)
Triad of:
- Necrotizing granuloma of the upper respiratory tract (ear, nose, sinuses, throat) or the lower respiratory tract (lung) or both
- Necrotizing or granulomatous vasculitis affecting small to medium-sized vessels, in the lungs and upper airways (most common)
- Crescentic glomerulonephritis
Pathogenesis
- PR3-ANCAs are present in 95% of cases, a useful marker of disease activity
Morphology
1. Lung lesion: Large nodular centrally cavitating lesions
2. Renal lesions:
- Focal and segmental necrotizing glomerulonephritis
- Parietal cell proliferation resulting in the formation of crescents (crescentic glomerulonephritis)
3. Arterial lesions: Vasculitis of a small artery with adjacent granulomatous inflammation including epithelioid cells and giant cells
Question 18. Classify vascular tumors. Add a short note on Kaposi sarcoma.
Answer:
Classification of vascular tumors and tumor-like conditions:
1. Benign neoplasms
- Hemangioma: Capillary hemangioma, cavernous hemangioma, pyogenic granuloma
- Lymphangioma: Simple (capillary) lymphangioma, cavernous lymphangioma (cystic hygroma)
- Glomus tumor
- Vascular ectasias: Nevus flammeus, spider telangiectasia, hereditary hemorrhagic telangiectasis
- Reactive vascular proliferations: Bacillary angiomatosis
2. Intermediate-grade neoplasms
- Kaposi sarcoma
- Hemangioendothelioma
3. Malignant neoplasm
- Angiosarcoma
- Hemangiopericytoma
Kaposi sarcoma (KS)
- Caused by human herpesvirus 8 (HHV8)
- Associated with acquired immunodeficiency syndrome (AIDS)
Four forms:
1. Classic KS:
- Presents as multiple red-purple skin plaques or nodules
- Seen in the distal lower extremities
- Tumors are asymptomatic and remain localized to the skin and subcutaneous tissue
2. Endemic African KS
- Involves lymph nodes
- Poor prognosis
3. Transplant-associated KS
- Increased risk in solid organ transplant recipient patients
- Involves lymph nodes, mucosa, and viscera
4. AIDS-associated (epidemic) KS
- Represents the most common HIV-related malignancy
- Involves lymph nodes and disseminates widely to viscera
Pathogenesis
- KS lesions are infected by human herpesvirus 8 (HHV8), also known as Kaposi sarcoma herpesvirus
Morphology
Cutaneous lesions in classic KS progress through three stages:
1. Patches:
- Red-purple macules localized to the distal lower extremities
- Microscopy: Dilated irregular endothelial cell-lined vascular spaces with interspersed lymphocytes, plasma cells, and macrophages
2. Plaques
- From patches, the lesions become larger, violaceous, raised plaques
- Microscopy: Dermis is composed of dilated vascular channels lined by plump spindle-shaped cells
3. Nodules
Microscopy
- Composed of sheets of plump, proliferating spindle cells surrounding small blood vessels in the dermis
- Characterized by marked hemorrhage, hemosiderin pigment, and mononuclear inflammatory cells
- Mitotic figures are common
Leave a Reply