Bone
Bone Infections — Osteomyelitis
Write a short note on the etiology of osteomyelitis.
Table of Contents
Definition of osteomyelitis: Osteomyelitis is defined as inflammation of the bone and marrow.
Classification of osteomyelitis:
- Primary: Where bone is the primary solitary focus of disease.
- Secondary: Develop as a complication of any systemic infection.
Any infection (bacteria, viruses, parasites, fungi) may cause osteomyelitis, but infections by certain pyogenic bacteria and mycobacteria are the most common.
Read And Learn More: Pathology for Dental Students Notes
Bone Pyogenic Osteomyelitis
Write a short note on the morphology of pyogenic osteomyelitis.
Etiology of Pyogenic Osteomyelitis:
It is usually caused by bacteria.
- The most common pathogens are Staphylococcus species (aureus in 80–90% of the cases).
- Other organisms:
- Escherichia coli, Pseudomonas, Klebsiella, Neisseria gonorrhoeae,
- Haemophilus influenza and Salmonella species.
- Escherichia coli in patients with genitourinary tract infections or intravenous drug abusers.
- Neonatal period: Haemophilus inflenzae and group B streptococci.
- Patients with sickle cell disease: Salmonella infection.
- Mixed bacterial infections: It is due to direct spread or surgery or open fractures.
- In about 50%, no organisms can be isolated.
Portal of Entry of Organism:
Causative organisms may reach the bone through the bloodstream, directly or extend from a contiguous site.
1. Hematogenous spread:
- The source of organisms may be a focus of infection anywhere in the body (e.g. skin pustule or infected teeth and gums, intestinal mucosa).
- Minor injuries to the mucosa (vigorous chewing of hard foods, brushing of teeth), or minor infections of the skin, release these organisms into the blood → causing temporary bacteremia → reaching the bone.
- In children (5 to 15 years) and drug addicts (infected needles), it develops in the long bones.
2. Direct implantation: Organisms may enter into bone by penetrating wounds, open fractures, or surgical procedures (staphylococci, streptococci, anaerobic organisms).
3. Spread from adjacent (contiguous) site: For example, Infections of the feet may spread into the bone in diabetics.
Location of infection: It varies with age.
- Children: With hematogenous spreadMetaphysis of long bones (knee, ankle, and hip).
- Neonate: Metaphysis, epiphysis, or both.
- Adult: Epiphysis and subchondral regions.
Pathogenesis and Morphology:
Write a short note on the pathogenesis and morphology of pyogenic osteomyelitis.
The sequence of events and morphological features in osteomyelitis are described together.
- Transient bacteremia: Mild injury or trauma can initiate bacteremia by organisms (for example, Staphylococcus aureus).
- The infection reaches the metaphysis long bone: Because in the metaphysis capillaries form loop → Which slows the blood flow → Provides time for bacteria to penetrate blood vessel walls and establish infective foci within the marrow.
- Inflammatory reaction: Once in bone, the bacteria grow and induce an acute inflammatory reaction with exudates.
- Necrosis of bone: Exudate increases the pressure on the adjacent vessels and further decreases the blood supply → producing bone necrosis. The necrotic areas coalesce and allow further bacterial proliferation.
Formation of sequestrum:
Write a short note on sequestrum.
- Bacterial infections and pus spread into the cortex and collect beneath the periosteum → may lift the periosteum → reduces the blood supply to the affected region → results in segmental necrosis of the bone due to both suppuration and ischemia.
- The fragment of a dead necrotic piece of bone, which is embedded in the pus, is known as a sequestrum.
Draining sinus:
- The pus penetrates the periosteum and leads to a soft-tissue abscess → may penetrate the skin → form a draining sinus. The hole formed in the bone during the formation of a draining sinus is known as the cloaca.
- The sinus tract may become epithelialized and may remain open, continually draining pus, necrotic bone, and bacteria.
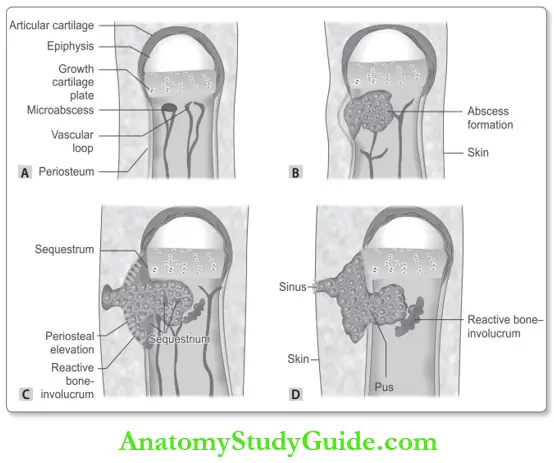
Involucrum: After the first week, chronic inflammatory cells become more numerous and the cytokines released stimulate osteoclastic bone resorption and deposition of reactive bone in the periphery. Reactive new bone forms a sheath around the necrotic (segment of devitalized infected bone) sequestrum. The reactive new bone formed is known as the involucrum.
Morphology of Osteomyelitis:
The morphologic features depend on the stage (acute, subacute, or chronic) and the location of the infection.
- Gross: Sequestrum appears as a fragment of bone with ragged brownish to black colored margins.
- Microscopy :
- In the initial stages, only the neutrophils are seen. As the disease becomes chronic, neutrophils admixed with chronic inflammatory cells (lymphocytes and plasma cells) are seen.
- Sequestrum does not show osteocytes and has empty lacunae.
Morphologic Variants of Osteomyelitis
- Brodie abscess: It is a distinctive form of subacute pyogenic osteomyelitis.
- It appears as a small, solitary, intraosseous abscess localized to the metaphysis and is surrounded by reactive bone.
- It may be due to inadequate treatment of infection by less virulent organisms.
- Sclerosing osteomyelitis of Garré: It is characterized by extensive new bone formation, which obscures the underlying structure of the bone and typically develops in the jaw.
Complications of Osteomyelitis:
Write a short note on complications of pyogenic osteomyelitis.
- Septicemia: From infection in the bone, organisms may disseminate through the bloodstream and cause septicemia.
- Acute suppurative arthritis: Infection may spread through the articular surface into a joint
- Producing suppurative arthritis → may lead to the destruction of the articular cartilage and permanent disability. It is more common in infants.
- Pathologic fractures.
- Squamous cell carcinoma: It may arise from the epithelialized sinus tract, rarely sarcoma of bone may develop.
- Secondary amyloidosis.
- Chronic osteomyelitis: It may develop due to delay in diagnosis, extensive bone necrosis, and inadequate therapy.
Clinical Course of Osteomyelitis:
- Present with malaise, fever, chills, leukocytosis, and throbbing pain over the affected region.
- Diagnosis:
- Radiography: Lytic focus of bone destruction surrounded by a zone of sclerosis.
- Blood cultures are positive.
- Biopsy and bone cultures.
Bone Tuberculous Osteomyelitis
Write a short note on tuberculous osteomyelitis.
Tuberculous osteomyelitis is usually solitary but in patients with acquired immunodeficiency syndrome, it is frequently multifocal. It tends to be more destructive and resistant to control than pyogenic osteomyelitis.
- Age: Usually adolescents or young adults in developing countries.
- Source of infection: Pulmonary or extrapulmonary tuberculosis.
- Predisposing factors: Diabetes, elderly, immune compromised states, and general debility
- Route of infection:
- Bloodborne: Usually blood-borne infection, which is from a focus of active pulmonary or extrapulmonary disease.
- Direct extension: From
- Lung into a rib
- Tracheobronchial nodes into adjacent vertebrae.
- Sites:
- The spine (thoracic and lumbar vertebrae) is commonly known as Pott disease. The infection breaks through intervertebral discs to involve multiple vertebrae and extends down into the soft tissues forming abscesses (cold abscess-psoas abscess).
- Knees and hips.
Microscopy of Tuberculous Osteomyelitis:
It shows a dead bone surrounded by tuberculous granuloma. The granuloma consists of a central area of caseous necrosis surrounded by epithelioid cells and Langhans giant cells, which in turn is surrounded by lymphocytes.
The epithelioid cells have a pale pink granular cytoplasm with indistinct cell boundaries, often appearing to merge into one another. The nucleus is oval or elongate.
Clinical Course of Tuberculous Osteomyelitis
- Low-grade fever with an evening rise in temperature
- Pain in motion, localized tenderness
- Weight loss.
Complications of Tuberculous osteomyelitis:
- Spine:
- Destruction of vertebrae: Causes severe scoliosis or kyphosis and neurologic defects due to spinal cord and nerve compression.
- Psoas abscess: Infection from the spine may rupture into the soft tissue anteriorly and pus and necrotic debris may drain along the spinal ligaments and form a cold abscess, i.e. an abscess lacking acute inflammation. Psoas abscess is the condition in which infection from lower lumbar vertebrae dissects along the pelvis, and appears as a draining sinus of the skin in the inguinal region. It may be the first manifestation of tuberculous spondylitis.
- Tuberculous arthritis
- Sinus tract formation
- Amyloidosis.
Bone Osteoporosis
Osteoporosis is a disease of the bone characterized by low bone mass (quantitative reduction) which leads to the porosity of bones.
Types of Osteoporosis: Osteoporosis may be:
- Localized: It is usually due to disuse and is seen as a complication of some other disease.
- For example, local immobilization following fracture due to other causes.
- Generalized: Involves the entire skeleton. It may be primary or secondary.
- Primary osteoporosis occurs without any known cause. These include senile and postmenopausal.
- Secondary osteoporosis develops due to a large variety of conditions. These include endocrine disorders (hyperparathyroidism, hyperthyroidism, etc.), gastrointestinal disorders, for example, Malabsorption, vitamin D deficiency, malnutrition), drugs (for example, Corticosteroids), tumors (multiple myeloma) reduced physical activity, hormonal disturbances and other causes (for example, Immobilization).
Etiology and Pathogenesis:
- Age: Peak bone mass is achieved between 25 and 35 years of age and gradually declines from the age of 50 years onwards.
- Sex: It is generally seen in the elderly and women. Genetic/hereditary factors also play an important role.
Pathogenesis of Osteoporosis:
In normal bone, there is a balance between bone formation and resorption. In osteoporosis, the balance is upset due to diminished bone formation, excessive bone resorption or both.
Morphology of Osteoporosis:
- The entire skeleton is involved in postmenopausal and senile osteoporosis but certain regions are more severely involved than others.
- The involved bones are thin and brittle. Microscopically, it is composed of the lamellar bone which is discontinuous and has thin trabeculae.
Clinical Features of Osteoporosis:
- Depend on the bones involved. Loss of bone mass predisposes the bone to fracture which results in bone pain.
- Fractures are most common in the vertebra in the thoracic and lumbar region, neck of the femur and
- Colles’ fracture (fracture of distal radius).
Complications of Osteoporosis;
- Pulmonary embolism and pneumonia as a complications of fractures of the femoral neck, pelvis or spine.
- When fractures of the vertebra are multiple, it may lead to lumbar lordosis and kyphoscoliosis (forward bending).
Diagnosis of Osteoporosis:
- Plain X-ray: Not reliable till 30– 40% of the bone mass is lost.
- Dual-energy X-ray absorptiometry and quantitative computed tomography.
- Bone biopsy.

Bone Tumors
Classify bone tumors.
Fibrous Dysplasia:
Fibrous dysplasia is a benign tumor. It is a localized developmental arrest in which all of the components of normal bone are present, but they do not differentiate into mature structures.
Types of Fibrous Dysplasia:
It arises during skeletal development. There is several distinctive types sometimes with overlapping clinical patterns:
- Monostotic: Affects a single bone and most common type (~70%).
- Polyostotic: Affcts multiple bones and constitutes 25% of cases.
- Mazabraud syndrome: Characterized by fibrous dysplasia (usually polyostotic) and soft tissue myxomas.
- McCune-Albright syndrome: It is a polyostotic disease, associated with café-au-lait skin pigmentations and endocrine abnormalities (for example, Precocious puberty).
Pathogenesis of Fibrous Dysplasia:
- Fibrous dysplasia is due to somatic gain-of-function mutation during development in GNAS1, the gene.
- The mutations produce a constitutively active Gs-protein that promotes cellular proliferation.
Morphology of Fibrous Dysplasia:
- Gross:
- The lesions are well-circumscribed, intramedullary, and vary greatly in size (2 to 5 cm).
- Larger lesions expand and distort the bone. The lesion is tan-white and gritty.
Microscopy of Fibrous Dysplasia:
- It is composed of curvilinear trabeculae of woven bone (nonlamellar) surrounded by moderately cellular fibroblastic tissue.
- The curvilinear shapes of the trabeculae mimic Chinese characters, and the bone lacks prominent osteoblastic rimming.
Clinical Course of Fibrous Dysplasia:
- Monostotic fibrous dysplasia: Most patients are between 20 to 30 years of age and occurs equally in boys and girls.
- It often stops enlarging at the time of growth plate closure. It commonly affects the femur, tibia, ribs, jawbones, calvarium, and humerus. It is usually asymptomatic and discovered incidentally.
- Radiologically, it has a typical ground-glass\ appearance and well-defined margins. Symptomatic lesions are cured by curettage.
- Polyostotic fibrous dysplasia: It manifests at a slightly earlier age than the monostotic type.
- The bones affected, in descending order of frequency, are the femur, skull, tibia, humerus, ribs, fibula, radius, ulna, mandible, and vertebrae.
- Polyostotic disease results in severe, progressive disease including crippling deformities and fractures.
- Rarely, it may be complicated by malignant transformation into a sarcoma.

- Mazabraud syndrome: It presents with skeletal features with multiple skeletal deformities during childhood. The intramuscular myxomas often develop in the same anatomic region as existing fibrous dysplasia.
- McCune-Albright syndrome: Most common presentation is precocious sexual development, which occurs most often in girls.
- The bone lesions are usually unilateral, and the skin pigmentation is usually limited to the same side of the body.
- The skin macules are large; dark to café-au-lait in color; have irregular serpiginous borders.
- They are found usually on the neck, chest, back, shoulder, and pelvic region.
Aneurysmal Bone Cyst
An aneurysmal bone cyst (ABC) is a tumor characterized by multiloculated blood-filled cystic spaces.
- Age: ABC affects all age groups but usually manifests during the first 2 decades of life and has no sex predilection.
- Site: Most frequently involves metaphysis of long bones and the posterior elements of vertebral bodies.
Clinical features of Aneurysmal bone cyst:
- Most commonly presents with pain and swelling.
- ABC of the vertebrae can compress nerves and produce neurologic symptoms.
Radiography of Aneurysmal bone cyst:
- ABC is usually an eccentric, expansile lesion with well-defined margins. They are mostly osteolytic lesions and contain a thin shell of reactive bone at the periphery.
- Computed tomography and magnetic resonance imaging may show internal septa and characteristic flid-flid levels.
Microscopy of Aneurysmal bone cyst:
- Aneurysmal bone cyst shows multiple blood-filed cystic spaces separated by thin, tan-white septa.
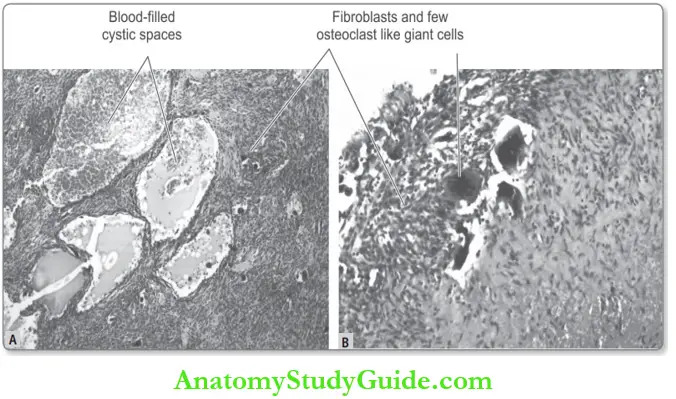
- The septa consist of plump uniform fibroblasts, multinucleated osteoclast-like giant cells, and reactive woven bone.
- The bone is lined by osteoblasts.
Clinical course Bone Aneurysmal Bone Cyst:
- The treatment is surgical, usually curettage or, in certain cases, en bloc resection.
- The recurrence rate is low.
Classification of Bone Tumors:
Major primary tumors of bone:
Bone Osteosarcoma
Write a short note on osteosarcoma.
Osteosarcoma (osteogenic sarcoma-OS) is the most common (20%) primary malignant bone tumor, excluding myeloma and lymphoma.
Definition of osteosarcoma: Osteosarcoma is a highly malignant bone tumor characterized by the formation of bone matrix or osteoid (unmineralized bone) by malignant tumor cells.
- Age group: Osteosarcoma has a bimodal age distribution.
- The fourth occurs in between 10 and 20 years of age.
- Secondary osteosarcoma (following Paget disease, bone infarcts, irradiation, etc.) develop in the elderly after 40 years of age.
- Sex: Affects boys more commonly than girls (2:1).
Pathogenesis of osteosarcoma:
Based on the pathogenesis, OS is divided into primary and secondary.
1. Primary Osteosarcomas:
In this type, the underlying bone is unremarkable. About 70% of osteosarcomas have acquired genetic abnormalities such as ploidy changes and chromosomal aberrations.
- Mutations in tumor suppressor gene:
- RB, the retinoblastoma gene (a cell cycle regulator) mutations is associated with a 1000-fold increased risk of osteosarcoma and its mutation is found in about two-thirds of patients.
- Patients with Li-Fraumeni syndrome (germline p53 mutations) have a greater incidence of osteosarcoma
2. Secondary Osteosarcoma:
Osteosarcomas in older persons almost always develop in association with pre-existing bone disorders. These include:
- Paget disease of bone.
- Radiation exposure
- Chemotherapy: Children treated with alkylating agents (other malignancies) have an increased risk.
- Pre-existing benign bone lesions: For example, Fibrous dysplasia, osteomyelitis, and bone marrow infarcts. Trauma may call attention to existing osteosarcoma rather than causing the tumor.
Classification of osteosarcoma:
Write a short note on the morphology and radiological appearance of osteosarcoma.
It can be classified in different ways:
1. Anatomic site of origin:
- Conventional (classical, medullary, intramedullary, textbook)
- Intracortical
- Surface osteosarcoma
- Parosteal (juxtacortical): Thy arise on the surface of the cortex.
- Periosteal: They arise on the surface of the periosteum.
2. Degree of differentiation:
- Well-differentiated
- Moderately differentiated
- Poorly differentiated.
3. Number of tumors:
- Solitary
- Multicentric
- Synchronous
- Metachronous.
4. Pathogenesis (described above):
- Primary
- Secondary to pre-existing disorders
5. Histologic features (described below)
Morphology
- Most Common Subtype:
- Primary
- Solitary
- Conventional/intramedullary
- Poorly differentiated.
- Location: Usually arises in the metaphyseal region of the long bones of the extremities.
- Sites: It usually arises near the knee or shoulder.
- The common site is:
- Lower femur
- Upper tibia, or fibula
- Proximal humerus.

- Gross: Gross appearance varies depending on the proportions of bone, cartilage, stroma, and blood vessels.
- Size: Usually big bulky tumors.
- Cut surface: Gray-white in color, gritty, shows areas of hemorrhage and cystic degeneration.
Microscopy of Osteosarcoma:
- Malignant tumor cells:
- Tumor cells vary in size and shape.
- Nucleus: Usually shows large hyperchromatic nuclei and often shows mitotic figures.
- Bizarre tumor giant cells are common.
- Matrix component: Production of osteoid (unmineralized/noncalcified) or bone (calcified osteoid) by malignant tumor cells is the single diagnostic feature of conventional OS.
- Osteoid: It appears as a dense, uniform, eosinophilic glassy intercellular material.
- Neoplastic bone: It usually has a coarse, lace-like architecture.
- Histological subtype: Most tumors contain a mixture of cells with varying amounts of matrices mentioned below. Depending on the one predominant matrix, conventional OS is divided into:
- Osteoblastic: A large amount of osteoid and bony trabeculae.
- Chondroblastic: Abundant malignant cartilage.
- Fibroblastic/fibrohistiocytic: They appear similar to malignant fibrous histiocytoma.
- Telangiectatic: Large cavernous dilated vascular channels and it is more aggressive.
- Small cell: The tumor cells are small in size, uniform, and simulate the appearance of Ewing’s sarcoma and malignant lymphoma.
- Giant cell: This subtype contains numerous giant cells.
- Vascular invasion and necrotic areas may be conspicuous.
- Immunohistochemistry: The malignant tumor cells stain prominently for alkaline phosphatase and osteonectin.
Clinical Course of Osteosarcoma:
- Usually present as painful, progressively enlarging masses around the knee or other involved sites.
- The involved area is swollen and tender and the function adjacent joint becomes reduced.
- Serum alkaline phosphatase is increased.
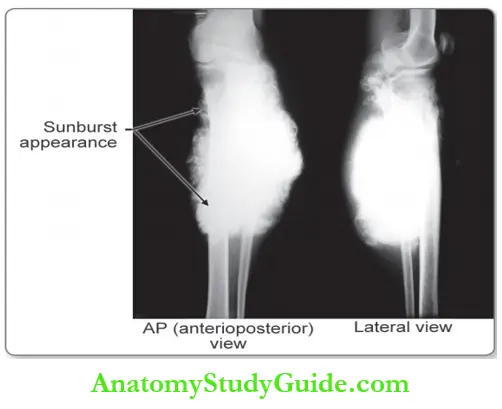
Radiological Appearance of Osteosarcoma:
OS shows a large destructive, mixed lytic (bone destruction) and blastic mass (neoplastic bone formation) with infiltrative margins.
- Codman triangle:
- The tumor frequently infiltrates the cortex lifts the periosteum, and produces a space between the cortex and lifted ends of the periosteum.
- Radiologically, this space appears as a triangular shadow and is known as the Codman triangle (characteristic but not diagnostic of this tumor).
- The space mainly contains reactive new bone, which is arranged perpendicular to the bone surface, but it may also contain malignant tumors.
- Sunburst appearance: When the malignant tumor extends into soft tissue, parallel lines of mineral deposition in the periosteal region gives an appearance of rays of sun → called a “sunburst” appearance
Spread of Osteosarcoma:
- Local spread:
- Invasion of the adjacent cortex destroys the nearby cortex.
- Elevation or perforation of the periosteum by tumor tissue.
- Spread along the medullary (marrow) cavity.
- Extension into the epiphysis:
- The articular end of the bone is generally not involved in the initial stage.
- Later, it may infiltrate the epiphyseal plate and may even involve the joint space.
- Extension into the soft tissues may involve the skin.
- Blood spread: It is an aggressive tumor, which may spread through the bloodstream to the lungs. Less commonly, it may metastasize to other bones, the pleura, the brain, and the heart.
Bone Giant-Cell Tumor
Write a short note on giant cell tumor/osteoclastoma.
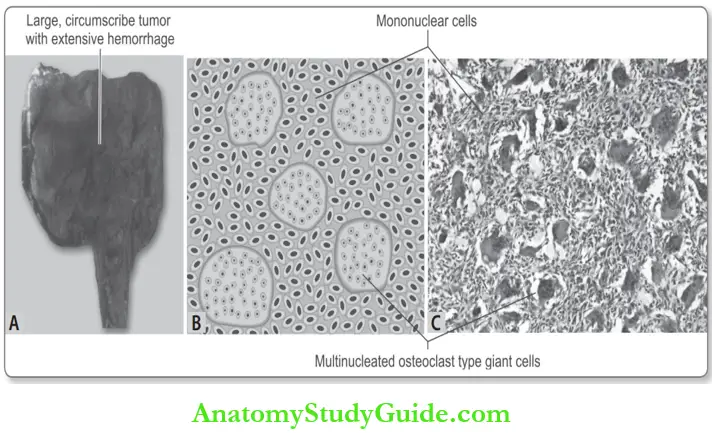
Definition of Giant cell tumor: Giant-cell tumor (GCT synonym osteoclastoma) is characterized by multinucleated osteoclast-type giant cells randomly and uniformly distributed in a background of mononuclear cells.
- Giant cell tumor is a relatively uncommon, locally aggressive, and potentially malignant neoplasm.
- Age: Usually seen between 20 to 40 years. In the elderly, it may be secondary to irradiation.
- Sex: Slight predilection for women.
- Cell of origin: Primitive stromal cells.
Morphology Giant cell tumor:
Write a short note on the morphology of osteoclastoma.
X-ray of the knee joint. Osteosarcoma of proximal tibia extending into the soft tissue with parallel lines of mineral deposition giving rise to sunburst appearance
- Site: Giant-cell tumors in adults involve both the epiphyses and the metaphyses of a long bone, but in adolescents, they are limited to the metaphysis.
- Bones involved:
- Knee area: Distal femur and proximal tibia.
- The lower end of the radius, humerus, and fibula.
- Gross: Large tumor, clearly circumscribed.
- Cut surface
- Soft and red-brown without bone or calcification
- Numerous hemorrhagic areas give the appearance of a sponge full of blood.
- Cut surface
Microscopy Giant cell tumor:
Two types of cells
1. Mononuclear (stromal) cells: They are of two types.
- Neoplastic mononuclear cells: They are uniform oval and plump with large nuclei and scanty cytoplasm. Tumor mostly consists of these neoplastic cells.
- Mitotic activity is common in these cells but not found in the giant cells. Diagnosis of malignancy depends upon the morphology of
the mononuclear cells rather than that of the multinucleated giant cells. - Non-neoplastic: These are mononuclear cells derived from macrophage monocytes.
2. Multinucleated (osteoclastic) giant cells:
- The background shows numerous large osteoclast-type giant cells throughout the richly vascularized stroma.
- These cells have 100 or more nuclei, which resemble those of mononuclear cells.
- Area of cystic degeneration and necrosis.
Secondary features: These include areas of hemorrhage, necrosis, hemosiderin deposition, and reactive bone formation.
Radiological Appearance:
Write short notes on clinical features, radiological findings, and morphology of osteoblastoma
It produces a lytic lesion and grows slowly, expands the bone, and destroys the overlying cortex.
The tumor produces a bulging soft tissue mass surrounded by a thin, shell of reactive bone due to periosteal reaction. This on radiology has a multiloculated or soap bubble appearance.
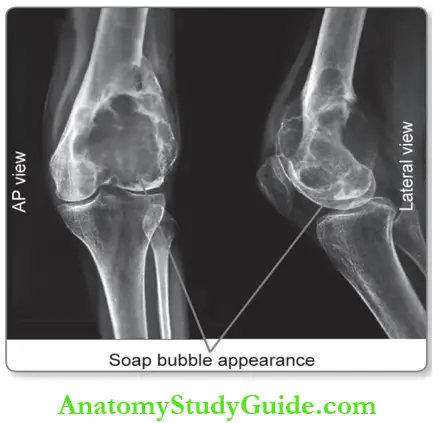
Clinical Course of Radiological Appearance
- Commonly seen near knee joints.
- Pain (usually in the joint adjacent to the tumor) and arthritis-like symptoms.
- Microfractures and pathologic fractures may develop due to thinning of the cortex.
Biologic Behavior Bone X-ray Of The Knee Join
- The majority of GCTs behave benignly, but locally aggressive tumors may recur.
- However, all GCTs must be considered as potentially malignant, because they may metastasize.
Spread Bone X-ray Of The Knee Join:
- Local spread: Tumor is usually restricted within the involved bone surrounded by periosteum.
- Aggressive tumors may penetrate the cortex and the periosteum and may involve the joint capsule and the synovial membrane.
- Hematogenous spread: The common site is the lung.
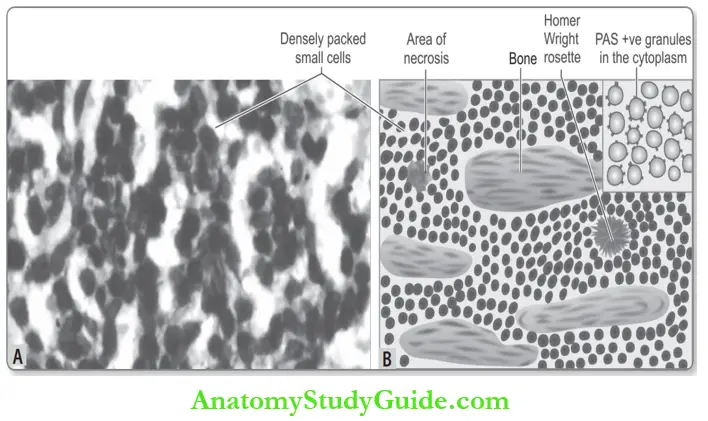
Ewing Sarcoma/Primitive Neuroectodermal Tumor
Write a short note on Ewing sarcoma.
Definition of Ewing sarcoma: The Ewing sarcoma family of tumors is primary malignant small round-cell tumors of bone and soft tissue.
- Uncommon tumors constitute ~ 6–10% of primary malignant bone tumors.
- Age: Mostly seen between 10 to 15 years of age, and about 80% are seen in patients younger than 20 years.
- In children, it is the second most common group of bone sarcomas, the first being osteosarcoma.
- Sex: More frequent in boys than girls (2:1).
Categories of Ewing sarcoma:
It consists of two tumors that differ only in their degree of neural differentiation. This distinction has no clinical signifiance.
- Ewing sarcoma (EWS): Undifferentiated tumors.
- Primitive neuroectodermal tumor (PNET): With neural differentiation.
Etiology and Pathogenesis:
- Origin: It arises from multipotent mesenchymal stem cells.
- Chromosomal abnormalities:
- Translocation of the EWS gene on chromosome 22 (22q12) with a gene encoding an ETS family transcription factor (FLI-1 or ERG gene).
- The fusion of the EWS1 gene to the FLI-1 gene (more common) resulting in the fusion protein, EWS/FLI-1 → Produces chimeric/aberrant transcription factors → activation of C-myc promoter → abnormal cell proliferation and survival.
- A less common translocation produces an EWS/ERG fusion gene → produces a variant of EWS with a significantly worse prognosis.
Morphology of Ewing sarcoma:
Write a short note on the morphology of Ewing sarcoma.
- Location: Arise in the diaphysis of the medullary cavity of long bones.
- Site: Ewing sarcoma and PNET involve the long tubular bones in childhood.
- Long bones: Humerus, tibia, and femur.
- Flat bones: Pelvis.
- Gross:
- Arise in the diaphysis and may infiltrate the medullary spaces without destroying the bony trabeculae.
- Diffusely infiltrate the cortex and the tumor may also penetrate the periosteum and spread into the soft tissues.
- Soft, grayish-white/tan-white, and frequently show areas of hemorrhage and necrosis.
Microscopy of Ewing sarcoma:
- Tumor cells: They are uniform, small, and round.
- Size: Tumor cells are about twice the size of a lymphocyte.
- Cytoplasm: Scant or little and appears clear because it is rich in glycogen, which is an
- important diagnostic feature. This stain is positive with the periodic acid-Schiff (PAS) stain.
- Arrangement: Closely packed sheets of cells.
- Homer-Wright rosettes: They may be seen. They consist of tumor cells arranged in a circle about a central fibrillary space. This is indicative of neural differentiation.
- Mitoses are infrequent even though the tumor is highly cellular.
- Interstitial stroma: Little or absent the fibrous strands separate the sheets of tumor cells into irregular nests or sheets. Necrosis may be prominent.
- Immunohistochemistry: EWS cells express characteristic antigens, some of which are part of the translocation product (for example, FLI-1 and CD99).
Radiographic Appearance:
- It produces destructive lytic lesions in which the border between normal bone and the tumor is indistinct.
- The tumor may extend into the surrounding soft tissues.
- Characteristic circumferential, discontinuous layers, of periosteal new bone formation produce an onionskin pattern.
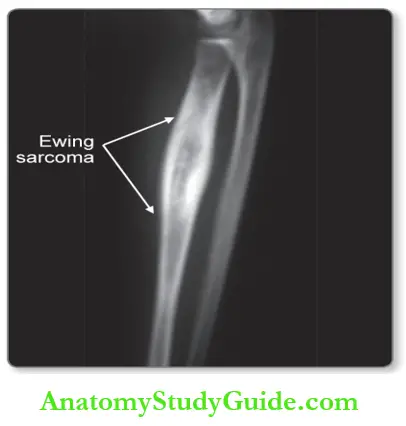
Clinical Features of Radiographic Appearance
- Painful enlarging masses and the affected site is tender, warm, and swollen.
- Systemic features: It may develop in some and be mistaken for an infection like osteomyelitis.
- Fever, weakness, and bone pain.
- Hematological findings: Anemia, leukocytosis, and raised erythrocyte sedimentation rate.
Spread of Radiographic Appearance
- Local spread: It may spread from the medullary cavity into the cortex, periosteum, and surrounding soft tissue.
- Blood spread: Lungs, brain, and other bones (skull).
- Treatment includes chemotherapy and surgical excision with or without irradiation.

Leave a Reply