Penis, Testis and Scrotum
Surgicla Anatomy Of The Penis
- It consists of two corpora cavernosa and one corpus spongiosum.
- Corpora cavernosa are vascular spaces into which arterioles open directly. They are corkscrew-shaped (helicine arteries), which allow their elongation during erection.
- Corpus spongiosum contains the urethra which expands distally as the glans.
Read And Learn More: Surgery of Urology Notes
Table of Contents
- Each corpus is enclosed by a tough fibrous membrane (tunica albuginea of the corpus).
- The fused fibrous sheaths are attached to the under surface of the symphysis pubis by a triangular sheet of fibrous tissue (suspensory ligament). This has to be divided during total amputation of the penis.

Blood Supply:
- The artery to the bulb supplies the corpus spongiosum and the glans.
- The deep artery supplies the corpus cavernosum alone—its sole function is erection.
- The dorsal artery supplies skin, fascia and glans.
- The superficial dorsal vein drains into superficial external pudendal veins. The deep dorsal vein enters prostatic venous plexus.
Penile Urethra:
- The entire penile urethra is lined with pseudostratified columnar epithelium, except for the dilated anterior part in the glans (fossa navicularis), which is lined by stratified squamous epithelium.
Lymphatic Drainage:
- Medial group of superficial inguinal nodes.
- Some from the glans pass directly to the node of Cloquet
Nerve Supply:
- Parasympathetic nerves—nervi erigentes: Causes erection of the external genitalia.
- Sympathetic system—hypogastric nerves: Helps in ejaculation.
Phimosis
It is the inability to retract the prepucial skin.
Causes:
1. Congenital: Most common type, seen in young patients.
2. Secondary to chronic balanoposthitis: Balanitis means inflammation of the glans penis, and posthitis means inflammation of the prepuce. Balanoposthitis is common in diabetic patients.
3. Chancre
4. Carcinoma of the penis can present as a recent phimosis.
Clinical Features:
- Inability to retract the prepuce.
- In children, ballooning of the prepuce (second bladder) can be seen, which is diagnostic.
- Balanoposthitis because of inability to clean the glans.
Complications:
- Paraphimosis
- Carcinoma penis
Treatment:
Circumcision: Removal of the prepuce.
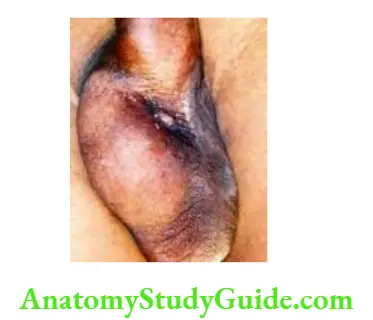
Paraphimosis
In this condition, the retracted skin of the glans penis (prepuce) cannot be pulled forwards. As a result, the retracted skin acts like a tight constricting agent that compresses the corona and causes venous congestion. As venous congestion increases, the glans swell up, resulting in paraphimosis.
Causes:
1. If the retracted prepuce is not pulled forwards during catheterizations.
2. May occur after sexual intercourse.

Clinical Features:
Severe pain in the glans penis
Gross swelling of the retracted prepucial skin and oedema of the distal glans penis.
Treatment:
1. Sedation
2. Injection hyaluronidase 250 units in 10–15 ml of saline is injected into the constriction ring (retracted prepucial skin). After 5–10 minutes, when oedema is reduced, the paraphimosis can be reduced with gentle manipulation.
3. Dorsal slit is given so that reduction can be done. Circumcision follows later.
Complications:
1. Ulcers of the glans
2. Gangrene of glans (later stages).
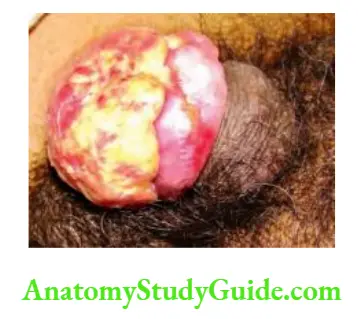
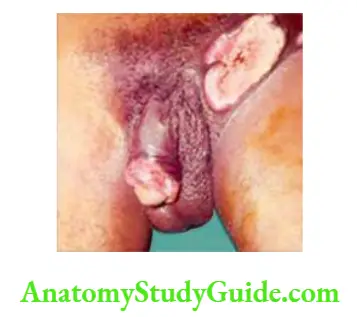
Carcinoma Penis
Most common type—squamous cell carcinomOther varieties—melanoma, adenocarcinoma, basal cell carcinoma (BCC).
Premalignant Lesions:
1. Genital warts: Buschke-Lowenstein tumour is a giant penile condyloma that resembles squamous cell carcinomIt is a cauliflower-like lesion and may have foci of malignancy.
2. Erythroplasia of Queyrat or Paget’s disease of the penis: A persistent, red, raw, precancerous, lesion.
3. Leukoplakia: Persistent nonspecific patch in the glans or prepucial skin. Interestingly, leukoplakic patches are not white in the penis.
4. Bowen’s disease: A small eczematous plaque that may develop carcinoma in situ.
Aetiology:
Phimosis:
1. Extremely rare in Jews who practise circumcision immediately after birth.
2. Rare in Mohammedans who practise circumcision few years after birth.
3. Common in Hindus and Christians who do not practise circumcision. Due to the prepucial skin, smegma collects within, which causes chronic irritation and results in carcinoma penis.
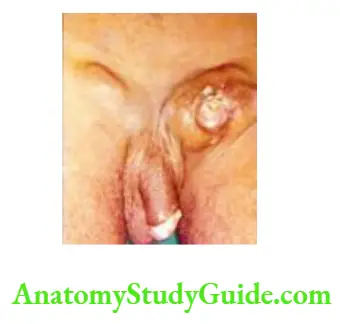
Clinical Features:
1. Carcinoma penis is common in the 6th decade. The majority of patients present with a nonhealing ulcer.
2. Foul-smelling discharge is common and is occasionally blood-stained.
3. Recent phimosis due to growth underneath the prepuce.
4. Haematuria and pain while passing urine indicate locally advanced tumours.
5. On examination, there is often an ulcero-proliferative growth with everted edges and extensive induration (much more than the lesion). Hence, entire shaft has to be examined for evidence of induration.
6. Urethra is rarely involved in carcinoma penis because it is protected by the tough Buck’s fascia, which is part of the pelvic fasciIn large fungating lesions, it may be difficult to identify the external urinary meatus. In such situations, the patient can point to the external urinary meatus.
Spread:
1. Direct spread: Involves the glans, prepucial skin, and shaft.
2. Lymphatic spread: Inguinal nodes are enlarge30% of cases are due to infection. Nodes are firm and tender in infection. Hard nodes suggest metastases. Later, the internal iliac and para-aortic nodes may also get enlargeIn advanced cases, lymph nodes may show fungation.


Cause of Death:
Death may occur due to erosion of the femoral vessels by the inguinal lymph nodes.
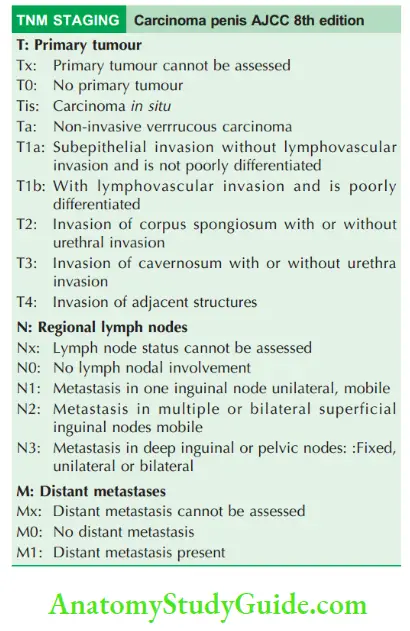
Staging:
- Tumour confined to the glans or prepuce
- Tumour involving the penile shaft or corpora cavernosa
- Mobile regional nodal metastases, with stage I or II
- Tumour beyond the penile shaft, fixed regional lymph node or distant metastases.
- Refer to TNM staging.
Investigations:
1. Wedge biopsy from the edge of the growth, proves the diagnosis of squamous cell carcinoma nodes. Once biopsy is confirmed, metastatic work up is done.
2. Ultrasound-guided FNAC of enlarged inguinal lymph nodes.
3. MRI are helpful in lesions invading the corpora cavernosa (soft tissue details).
4. CT scan is useful in obese patients wherein clinical examination of inguinal nodes is difficult
5. CT-guided FNAC of pelvic nodes
Differential Diagnosis:
1. Condyloma acuminatum
2. Buschke-Lowenstein tumour
3. Balanitis xerotica obliterans
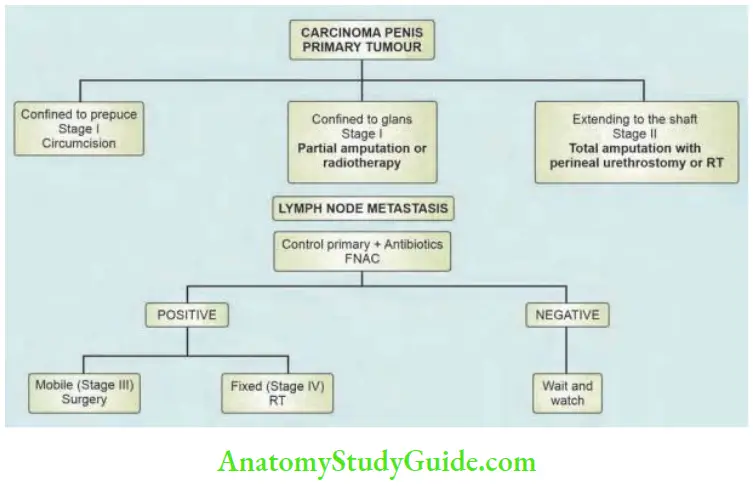
Treatment:
It can be divided into treatment of the primary and treatment of the secondaries.
1. Treatment of the Primary
Stage 1:
1. Growth confined to the prepuce—circumcision.
Regular follow-up is necessary.
2. Growth involving the glans: Partial amputation with at least 2 cm margin from the palpable, indurated edge of the tumour.
Stage 2:
1. Partial amputation: After having a proximal, macroscopic tumour-free, 2 cm margin, if there is adequate length of the penile shaft (minimum 2.5 cm) to carry out sexual functions and direct the urinary stream, a partial amputation can be done.
2. Total penectomy with perineal urethrostomy, if adequate shaft cannot be retaineThis is a major operation, so the patient has to be clearly instructed about the consequences and complications of it.
Complications of perineal urethrostomy:
1. Ammoniacal dermatitis of the scrotum. To prevent this, the patient has to lift the scrotum to pass urine.
2. Stricture of the perineal urethra, which can be dilated by Hegar’s dilators.


Stage 3:
Circumcision, partial amputation or total penectomy followed by ilioinguinal block dissection.
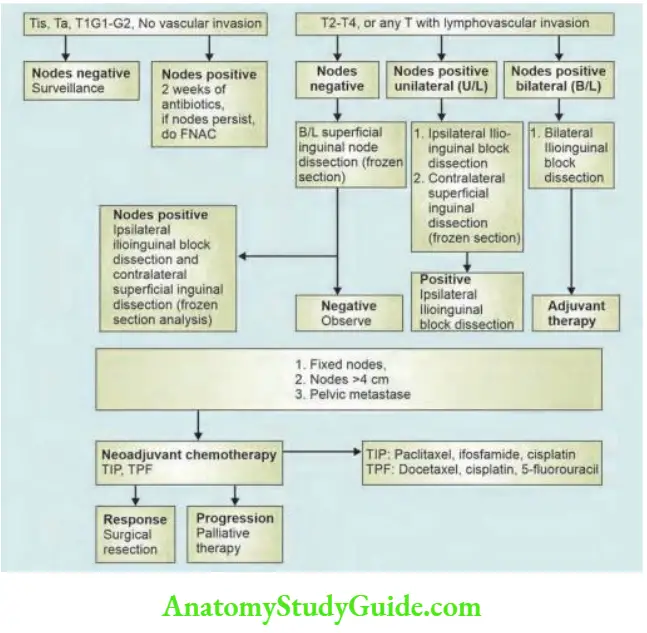
2. Treatment of Inguinal Lymph Node Secondaries:
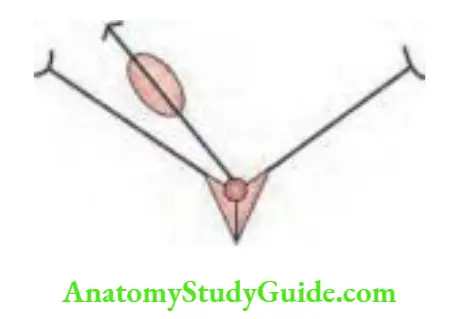
- Before discussing ilioinguinal block dissection, it is necessary to know the concept of sentinel lymph node biopsy (SLNB).
- The concept of SLNB was first described by Cabana in 1977.
- He demonstrated consistent drainage of the penile lymphatics into a sentinel lymph node or groups of lymph nodes, located superomedial to the junction of the saphenous and femoral veins in the area of the superficial epigastric vein. He postulated that this SLN is the first to get involved in the penile malignancy and that if this SLN is negative for tumour, metastasis to other inguinal lymph nodes will not occur. Metastasis to this lymph node will indicate the need for complete ilioinguinal block dissection.
- Technique: Isosulphan blue is injected at the site of the primary tumour. After sometime, inguinal dissection is done to expose the SLN area and the lymph nodes, which take up the dye. These are removed and sent for pathological examination. Based on the report, if the node is positive for malignancy, a complete inguinal block dissection is indicateIn case of negative nodes, nothing else is required, and the patient is kept under regular follow-up.
- Only T1a patients presenting with palpable lymph nodes actually have metastasis in 50% of cases, and the remainder have lymph node enlargement secondary to inflammation. Hence, subjecting all the patients with inguinal lymphadenopathy to surgery is not recommendeTherefore, a course of antibiotics is given and a period of 4–6 weeks are waited for. If the nodes are still palpable, block dissection is carried out in T1a patients.
- However, this antibiotic policy can be followed in low-grade tumours such as in situ carcinoma and T1 lesions. If the lymph nodes regress, wait and watch. If the grade of the tumour is high, do not give antibiotics. FNAC is done, and it is treated accordingly.
- In addition, if the nodes are not palpable, and if the primary tumour is poorly differentiated, superficial lymph node dissection is done. If the nodes are positive, modified inguinal block dissection (Catalona) can be done.
- An algorithm to help in the management of these patients.
Recent Advances In The Treatment Of Carcinoma Penis:
Organ Preservation:
Primary tumours—Tis, Ta, T1; grade 1 and grade 2 tumours—they have favourable histology.
Approaches to organ preservation:
1. Topical ointments such as 5-fluorouracil or imiquimod cream in Tis only
2. Radiation therapy
3. Mohs surgery: Layer-by-layer complete excision of the penile lesion in multiple sessions with microscopic examination of the undersurface of each layer.
4. Limited excision: It can be done in selected patients who have discrete tumours, with well-differentiated carcinoma after doing an intraoperative frozen section.
5. Laser ablation: It is performed in selected patients in conjunction with frozen section biopsies. CO2 laser has been used widely but recurrence rates are higher—about 40–50% for T1 tumours. Treatment with Nd:YAG laser has the least recurrence rates. The advantage of laser treatment is that the rate of resuming sexual activity is high.
6. Modified radical inguinal block dissection (Catalona): To minimise complications of inguinal block dissection, the following modifications are done.
- Good preoperative and postoperative care
- Myocutaneous flap cover
- Preservation of the dermis
- Preservation of Scarpa’s fascia
- Preservation of the saphenous vein
Stage 4:
Radiotherapy + chemotherapy (cisplatin, ifosfamide and paclitaxel are the drugs used commonly).
Radiotherapy:
Indications:
1. Young patients who want to have a sexual life
2. Patient refuses surgery
3. Fixed/ulcerated inguinal metastasis
Types:
1. External Radiotherapy
Dose: 4000–6000 cGy which may also include iliac and inguinal nodes.

2. Interstitial Radiotherapy
Iridium wires/tantalum wires are implanted within the glans.
Complications of Radiotherapy
- Radionecrosis of the penis Summary of treatment
Peyronie’s Disease (Penile Fibromatosis)
Aetiology:
- Past trauma has been considered as one of the causative factors.
- Venereal diseases have also been blamed.
- Association with Dupuytren’s contracture, retroperitoneal fibrosis, and plantar fasciitis.
Clinical Features:
- Hard plaques of fibrosis can be palpated along the length of the penis in the sheath of corpora cavernosa (induration–penis–plastica).
- As a result of hard plaques, erection is not proper, and the erected penis tends to bend towards the side of the plaque.
Treatment
Medical: Steroids, vitamin E, tamoxifen (poor results) colchicine therapy, intralesional verapamil. Watch and observe some cases. It may recur after a few years. Surgical: Straightening of the penis is recommended, if the deformity is distressing.
1. Nesbitt’s operation: Straightening the penis by placing a nonabsorabable suture in the corpora cavernosum opposite the plaque.
2. Gelhard’s operation: Multiple incisions over the fibrous plaques with temporal fascia bridging.
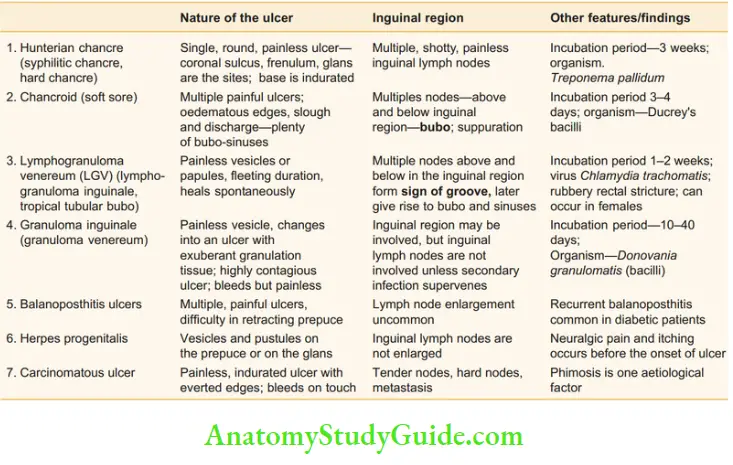
Differential Diagnosis Of Ulcer Penis
- There are many causes of ulcer penis.
- The important ones are carcinoma and sexually transmitted diseases.
- The incubation period is an important clue followed by the nature of the ulcer.


Differential diagnosis of ulcer penis:
Anatomy Of The Testis And Epididymis
Testis:
Size: 4 × 3 × 2.5 cm, one in each scrotal sac.
The functional unit is a lobule: 250 lobules filled with seminiferous tubules.
- Germ cells —→ Sperm production
- Leydig cells —→ Testosterone production
- Sertoli cells —→ Oestrogen production

- The seminiferous tubules converge to form a rete testis, which is connected to the epididymis through 5–7 efferent ductules.
- It is covered by thick, inseparable, fibrous tissue— tunica albuginea.
- The serous space in the front and lateral surface of the testis is the tunica vaginalis.
- Blood supply is by the testicular artery—a branch of the aortae testis gets additional blood supply from artery of the vas and the cremasteric arteries. In case of inguinal surgeries, if the testicular artery is accidentally injured, testicular vascularity is maintained by these two arteries. Veins form the pampiniform plexus in the scrotum.
- Lymphatics: Drain via the para-aortic nodes lying along the side of aorta at the level of origin of the testicular arteries (L2) just above umbilicus.
Epididymis:
- It is 6 m in length (20 feet long), highly coiled and packed, and adherent to the posterior surface of the testis.
- It has the following parts—head, body and tail. Head and body are commonly involved in tuberculosis, resulting in posterior sinus formation.
- It is lined by tall columnar epithelium.
- The head receives vasa afferentia from the rete testis and is firmly attached to the testis.
- From the tail, the vas deferens (ductus deferens), a direct continuation of the canal of the epididymis, passes up medially.
- The epididymis is supplied by a branch of the testicular artery.
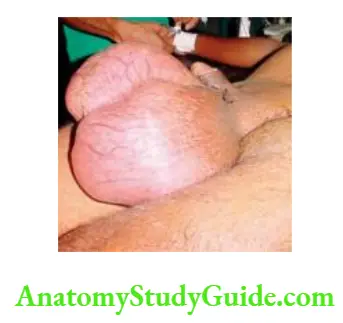
Hydrocoele
A collection of excessive fluid in the tunica vaginalis sac (TV sac).
1. Congenital Hydrocoele:
Occurs due to a complete or partial patent processus vaginalis sac.
Types:
1. Vaginal hydrocoele: This occurs when the hydrocoele sac is patent only in the scrotum.
2. Infantile hydrocoele: The sac from the scrotum is patent up to the deep inguinal ring.
3. True congenital hydrocoele:
- In this condition, the scrotal sac communicates with the peritoneal cavity. It is seen in infants and may be secondary to TB peritonitis. A scrotal swelling appears when the child assumes an erect posture for a long time, and it may not reduce due to the inverted ink bottle effect. Hence, congenital hydrocoele is not reducible. It regresses in size if the child assumes a supine position while sleeping.
4. Encysted hydrocoele of the cord:
- In this condition, the sac is obliterated above (inguinal canal) and below (scrotum) but patent at the root of the scrotum around the spermatic cord.
- It presents as a soft, cystic, fluctuant, transilluminant swelling separate from the testis and well above the testis.
- Diagnosis is established by the traction test: The swelling has free mobility, but when gentle traction is applied, the swelling becomes fixed and moves down when the testis is pulled down. This variety of hydrocoele is treated by excision of the sac.
5. Hydrocoele-en-Bissau (bilocular hydrocoele): In this condition, the scrotal sac communicates with another sac underneath the anterior abdominal wall musculature. The diagnosis is made by eliciting cross-fluctuation.
Various Types Of Hydrocoele:







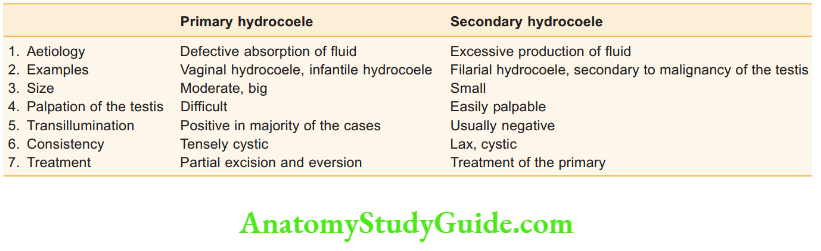
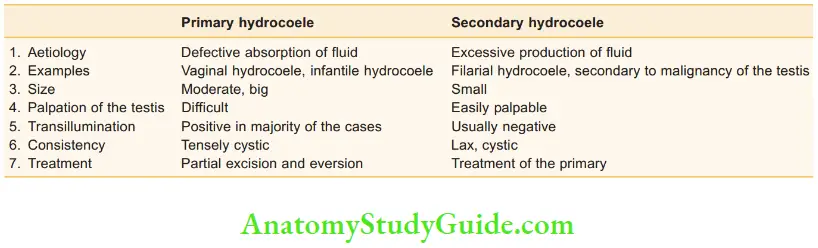
Comparison of primary hydrocoele with secondary hydrocoele:
6. Hydrocoele of the canal of Nuck: It presents as a swelling in the inguinal region in females.
2. Acquired Hydrocoele:
- Primary or idiopathic.
- Secondary hydrocoele.
Primary Vaginal Hydrocoele:
This is the most common type of hydrocoele which is seen in young adults, middle age and beyonIt is due to the following causes:
- Defective absorption of fluid
- Defective lymphatic drainage
Clinical Features:
- Soft, cystic, fluctuant, transillumination positive swelling confined to the scrotum.
- Not reducible
- No impulse on cough
- Can get above the swelling.

Secondary Hydrocoele:
1. Epididymo-orchitis: It is inflammation of epididymis and testis commonly due to infection. It is usually unilateral. Recurrent epididymo-orchitis due to filariasis: Fluid accumulates due to lymphatic obstruction. The fluid is milky white. Such hydrocoeles are called chylocoeles and often do not exhibit transillumination.

Patient may present with acute scrotal pain with or without fever, dysuria or urethral discharge.
Common organisms are E. coli, Chlamydia, N. gonorrhoeae, M. tuberculosis, etMumps also causes epididymo-orchitis. It should be differentiated from testicular torsion especially in young adults. Ultrasound is usually helpful. Urine, urethral discharge culture and sensitivity are often needeTreatment consists of scrotal support, NSAIDs and antibiotics like fluoroquinolones and/or tetracycline. In all cases of epididymo-orchitis, the partner also needs to be evaluated.
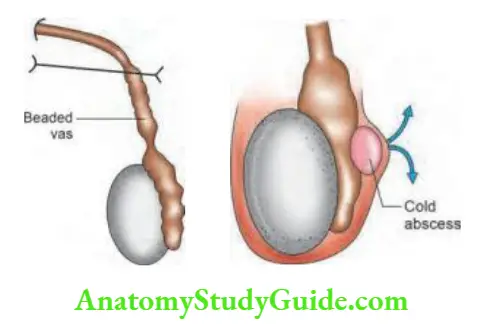
Eventually, it forms a cold abscess which ruptures and results in a sinus posteriorly, in the scrotum.
It never involves the testis proper.
3. Testicular tumours: They can present with a swelling of the scrotum and are, often diagnosed as hydrocoele. Any young patient with a rapidly growing scrotal swelling could be having a testicular neoplasm. Fluid within the sac is haemorrhagic.
4. Pyocoele: Infected hydrocoele. Infection in a hydrocoele is rare because of the tunica vaginalis sac, which is relatively avascular. However, a few cases may get infected, resulting in pyocoele. These patients present with fever, chills and rigors.
5. Haematocoele: Trauma to the hydrocoele or spontaneous bleeding into the sac.
Treatment of Hydrocoele:
1. Lord’s plication is indicated in small hydrocoeles. The sac is opened, and the cut edge of the sac is plicated to tunica albuginea (the reflected portion of the processus vaginalis). As a result, the sac gets crumpled up near the testis. Testicular secretions get absorbed by subcutaneous lymphatics and the venous system.
2. Partial excision and eversion of the sac: Jaboulay’s operation. This is indicated in large hydrocoeles. The thick, large, sac is excised and sutured behind the testis.
3. Aspiration is a temporary method that may introduce infection. It can be done only in high-risk patients and is a procedure to be condemned.
Complications of Hydrocoele:
1. Haematocoele: Occurs due to minor trauma
2. Pyocoele: Infected haematocoele
3. Calcification of the hydrocoele sac
4. Rupture of the hydrocoele sac—very rare
5. Hernia of the hydrocoele sac occurs when there is a small tear in the sac resulting in accumulation of fluid in the subcutaneous planes.

Cystic Swellings In The Scrotum
- Hydrocoele
- Retention cyst
1. Spermatocoele:


Comparison of epididymal cyst with spermatocoele:


2. Sebaceous cyst (skin of the scrotum)
3. Congenital cyst:
- Epididymal cyst
- Cyst of the hydatid of Morgagni
4. Tubercular epididymal-orchitis:
Cold abscess with a sinus in the posterior aspect of scrotum.
Undescended Testis
This occurs when the descent of the testis is arrested somewhere along its normal pathway to the scrotum.
Development:
- The testis develops in the retroperitoneum close to the posterior abdominal wall from the genital tubercles.
- It is guided to the scrotum by the gubernaculum.
- By around the 7th month—it reaches the deep inguinal ring, by the 8th month—inguinal canal and by the 9th month—superficial inguinal pouch. In normal situations, the testis reaches the scrotum at full term.
- As it descends, it is surrounded by the processus vaginalis saThis sac normally gets completely obliterateA persistent processes vaginalis sac causes hernia and hydrocoele.

Causes:
1. Muscular hypotonia: The descent of the testis depends upon muscular contractions of the anterior abdominal wall. Hence, undescended testis is seen in children with poor muscle tone, (e.g. prune-belly syndrome and Down’s syndrome).
2. Gubernaculum dysfunction.
3. Maternal human chorionic gonadotrophin (HCG) which causes development (maturation) of the testis and also helps in descent of the testis. If there is deficiency of HCG, imperfectly developed undescended testis appears.
4. Familial
5. Retroperitoneal adhesions.
Clinical Features:
1. The right side is more often involve Bilateral undescended testis is found in about 20% of cases.
2. Cryptorchidism: When both testes are impalpable as in cases of abdominal testis and inguinal testis.
3. Retractile testis: In this condition, the scrotum is welldeveloped, and the testis is palpable at the root of the scrotum and can be brought down to the scrotum. Retractile testis is harmless and spontaneously gets corrected within 1–2 years of age, without any treatment. The squatting position may help in such cases, in diagnosing the condition and in helping the testis descend to the scrotum.
Complications (can be remembered as Testis):
T Trauma produces pain
E Epididymo-orchitis will mimic an acute abdomen.
S Sterility: Histological changes start at the age of 2 years, and by the age of 12 years, irreversible damage occurs to spermatogenesis, due to testicular atrophy. Endocrine function remains normal.
T Torsion
I Indirect hernia in the majority of cases.
S Seminoma of the testis and other testicular malignancies are more common in undescended testis than in normal testis. (Risk of seminoma in both testes, not only in undescended testis.)
Treatment:
1. The treatment of choice is orchidopexy:
- It can be done by open method or laparoscopic method.
- It can be performed as a one-stage or two-stage procedure.
- Two-stage procedure for undescended testis (Fowler-Stephens technique).
Stage 1—tethering spermatic blood vessels are divided.
Stage 2—The testicle is placed into the scrotum after collateral blood supply to the testicle develops.
Procedure:
- Considering the functional and malignant potential of undescended testis, ideal age of surgery is between 9 months to 1 year. The inguinal canal is explored, and the testis is mobilised by dividing the adhesions, brought down into the scrotum, and fixed using nonabsorbable suture material.
- A dartos pouch can be formed and followed later by narrowing the root of scrotum.
- The associated hernial sac is excised.
2. Orchidectomy is done after the age of 14 years because of malignant potential.
3. Ombredanne’s procedure: Testis is brought down to the opposite scrotum through the scrotal septum and kept in dartos pouch.
4. Silber’s procedure: The testicular artery and vein can be divided and reanastomosed using microvascular techniques.
Ectopic Testis
- Testis is present in an ectopic site (not the route through which it descends).
- Sites of ectopic sites are:
- Superficial inguinal pouch
- Perineum
- The root of the penis
- Femoral triangle (thigh)
- Anatomically, the size is normal. Physiologically, it functions normally.
- Embryology: Testis reaches the scrotum by the scrotal tail gubernaculum. However, if this is weak, the other scrotal tail may pull it in a different direction, resulting in ectopic testis (Lockwood’s theory).
- Complication: It is more prone to injuries.
- Treatment: Orchidopexy in a new scrotal pouch.
Varicocele
Definition:
Dilated and tortuous veins of pampiniform plexus (veins draining the testis and epididymis). It lies posterior and above the testis. This can be totally missed if the examination is done in the supine position. It is the most common surgically correctable cause of subfertility in males.
Anatomy:
- Testicular veins, which drain the testis and epididymis, form multiple veins in the scrotum called the pampiniform plexus of veins. As they travel the inguinal canal, they are reduced to 6–8 in number. At the level of the deep ring, they are 2 in number and in the retroperitoneum, it forms the single testicular vein.
- On the right side, the testicular vein drains into the inferior vena cava directly.
- On the left side, it drains into the left renal vein at right angles where there is a valve.
Aetiology:
1. The most common cause is absence/incompetent valves in internal spermatic or testicular veins.
2. Increased venous pressure in the left renal vein is also a factor. It is due to compression of the left renal vein between the aorta and superior mesenteric artery. The left renal vein can also be compressed by the sigmoid colon. Varicocele is common on the left side (because left testis is at a lower level than the right). The flow of blood from the left side is into the renal vein at an angle of 90°.
3. A recent varicocele on the right side in an elderly patient suggests renal cell carcinoma invading the renal veins. Such varicoceles are rapidly evolving and do not regress in the supine position.
Clinical Features:
- Common in thin, tall patients
- Hot climates, favour the development of varicocele.
- In the standing position, the diseased side appears to be more swollen than the other side. It feels like a bag of worms. On asking the patient to cough, there is fluid thrill, due to regurgitation of venous blooOn the side of varicocele, the scrotum is at a lower level.
- On asking the patient to lie down, it is reducible (disappears).
- Dragging pain in the scrotum is a feature but it is nontender.
- The testis may appear small and soft with diminished testicular sensation.
- Blow test: On blowing, fluid thrill may be felt, and it may increase in size (Valsalva’s manoeuvre). USG demonstrating veins ≥3.5 mm in diameter with reversal of venous flow after Valsalva manoeuvre varicocele.
Grading of Varicocele:
1 (small)—palpable only with Valsalva manoeuvre, not visible
2 (moderate)—palpable without Valsalva manoeuvre, not visible
3 (large)—palpable and visible through scrotal skin.
Effect on Spermatogenesis:
Oligospermia:
This occurs due to the following reasons:
- Venous congestion due to the varicocele results in increased temperature in the scrotum.
- Reflux of blood from the renal vein brings powerful hormones secreted from adrenal glands like corticosteroids and adrenaline.
Treatment
1. Subinguinal microscopic (Joel Marmar’s operation) varicocelectomy for complete ligation.
2. Inguinal approach (Ivanissevich operation): Excision of the pampiniform plexus in the inguinal canal after ligating them. The testis still has venous drainage through the cremasteric veins.
3. Retroperitoneal approach (Palomo’s operation): In the retroperitoneum, the testicular vein is single and separate from the vas deferens. Hence, it is ligated up in the retroperitoneum. This operation was once thought to be better than the inguinal approach since there is no danger of damaging the vas and ligation of testicular vein is easy; however, recurrence rates are high so it is not favoured nowadays.
4. Laparoscopic varicocelectomy is a popular—retroperitoneal approach.
Complications of Varicocele Surgery:
- Hydrocele: It is because of ligation of the lymphatic channels as well. It is least after microscopic ligation.
- Testicular atrophy is seen in ≤1% of patients.
- Recurrence.
Torsion Testis (Torsion Of The Spermatic Cord)
Predisposing Causes:
- Inversion of the testis is the most common cause, where the testis lies horizontally or upside down.
- High investment of tunica vaginalis—bell clapper deformity.
- In cases where the body of the testis is separated from the epididymis.
- Sudden contraction of the spirally attached cremasteric muscle leads to rotation of the testis around its vertical axis during straining (e.g. at stools, lifting heavy weight, coitus).
- A long, redundant spermatic cord allows twisting of the testis on its own axis.
There are two types of testicular torsion:
- Extravaginal torsion: It is diagnosed in newborns and is caused by non-adherence of the tunica vaginalis to the dartos layer. As a result, the spermatic cord and tunica vaginalis are rotated as a unit.
- Intravaginal torsion: It is usually diagnosed in boys 12–18 years of age but can occur at any age.
Clinical Features:
- Age: 10–25 years, sudden agonising pain in the groin and lower abdomen, may be with vomiting.
- The scrotum is empty and oedematous on the side of the lesion.
- Tender lump at the external abdominal ring—the testis is positioned high (Deming’s sign).

- Prehn’s sign: Elevation of the scrotum increases pain in torsion of completely descended testis (decreases pain in epididymo-orchitis).
- Angell’s sign: The opposite testis lies horizontally because of the mesorchium.
Management:
- Best results—if detorsion occurs within 4 hours of the onset of pain.
- Scrotal Doppler to confirm the diagnosis
- In the first hour, untwist the testis manually
- If this is not successful, urgently explore the scrotum and undo the torsion. A viable testis should be fixed to the scrotum to prevent recurrence.
- Gangrenous testis should be removed.
- The testis on the opposite side should be fixed at an early date to prevent torsion as it also has a high risk of undergoing torsion.
Testicular Tumours
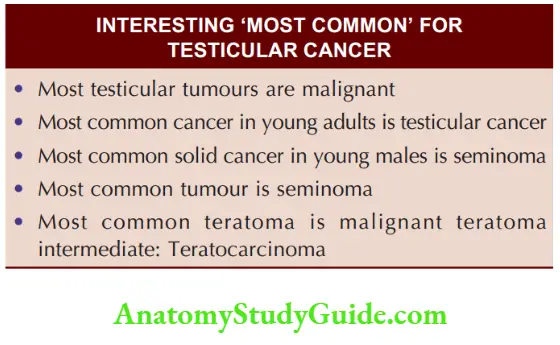
They constitute 1% of all malignant tumours in males, and almost all (>90%) are malignant.
Classification
- WHO Classification
- Other Classification
1. Seminoma is the most common germ cell tumour: 50% incidence
Types:
- Spermatocytic—good prognosis
- Lymphocytic
- Anaplastic
2. Teratoma:
- Incidence: 30% (subtype will be discussed later)
3. Combined:
- 10 to 20%
4. Interstitial cell tumours:
- Leydig cell tumour
- Sertoli cell tumours
5. Lymphoma of the testis: Very rare
Seminoma:
Aetiology:
1. Undescended testis, undoubtedly predisposes to seminoma.
- 1 in 20 abdominal testes, 1 in 60 testes at the level of deep ring and 1 in 80 inguinal testes are prone to testicular tumours.
- However, it should be noted that 25% of testicular cancers in patients with crypto-orchidism occur in normal, descended testis.
2. Klinefelter’s syndrome: These patients are prone to developing of seminomOther features of the disease are testicular atrophy, absence of spermatogenesis, gynaecomastia, etc.
3. Trauma to the testis is a coincidence. This may not precipitate a testicular tumour but draws the attention of the patient to it.
Pathology:
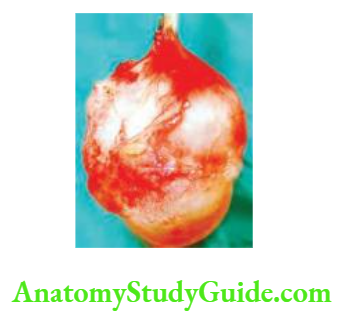
Seminoma arises from the seminiferous tubules. As the tumour grows, it compresses the normal testicular tissue. The cut surface is smooth and homogenous. Microscopy: Round to oval cells with a prominent nucleus. In a few cases, lymphocytic infiltration may be found.

Types of Seminoma:
1. Typical: It is the most common type of seminoma and is also called classic variety. Syncytiotrophoblastic type produces high levels of β-HCG.
2. Spermatocytic type: It occurs in elderly patients. It is slow growing and rarely spreads. Hence, it has good prognosis.
3. Anaplastic: As the name suggests, this variety has a high mitotic index/anaplasia and thus spreads fast and carries poor prognosis.
4. Atypical form
Teratoma:
Teratoma arises from rete testis. The tumour contains totipotential cells, so it may have ectodermal, mesodermal and endodermal elements.
Types of Teratoma:
1. Malignant teratoma differentiated: It is the least common variety (1%). It is almost a benign tumour— Dermoid cyst. Orchidectomy cures the disease.
2. Malignant teratoma intermediate: This is the most common variety (30%) and contains malignant and incompletely differentiated components.
3. Malignant teratoma anaplastic: Highly malignant tumour. Secretes alfa fetoprotein (AFP). Cells are presumed to be from the yolk sac.
4. Malignant teratoma trophoblastic: This is an uncommon tumour (1%) that secretes very high levels of β-human chorionic gonadotropins (β-HCG).
Clinical Features Of Testicular Tumours:
1. Typical Presentation:
Age: Teratoma 20–30 years, seminoma 30–40 years.
Testicular swelling: More often heaviness rather than hypertrophy or if it is infiltrated with tumour but vas is never involveThis is called sign of vas negative (sign of vas positive in TB epididymo-orchitis where there is beading of vas).
Haemospermia: Blood in the semen is rare.
Infertility: Not uncommon.
Gynaecomastia is seen in about 10% of patients.
Secondary hydrocoele is not uncommon. A young adult with a small hydrocoele and enlarged testis should arouse suspicion of testicular cancer.
2. Atypical Presentation:
1. Hurricane variety is the most malignant tumour. The tumour grows rapidly with pulmonary metastasis (cannonball), and death occurs within a few days.
2. Mimicking acute epididymo-orchitis: This variety presents as severe pain along with testicular swelling but does not respond to antibiotics.
3. Symptoms Mainly due to Metastases:
1. Lymphatic spread
- Para-aortic node mass—distension of the abdomen.
- Left supraclavicular node mass—swelling in the neck.
- Iliac node mass—swelling of the leg.
2. Blood spread: Extensive pulmonary secondaries occur from a malignant teratoma.

Spread:
- Seminoma spreads lymphatically. Along the testicular vessels, it spreads to the para-aortic lymph nodes to the thoracic duct, to mediastinal nodes, and then to the left supraclavicular nodes. Spread does not occur to the inguinal nodes, unless the scrotum is incised.
- Malignant teratomatous tumours spread predominantly by blood.
- Tnm Staging Of Testicular Cancer
- Stage 1: Tumour confined to the testis only.
- Stage 2A: Tumour and lymph nodes below the diaphragm—size ≤2 cm.
- Stage 2B: Tumour and lymph nodes below the diaphragm—size ≥2 cm.
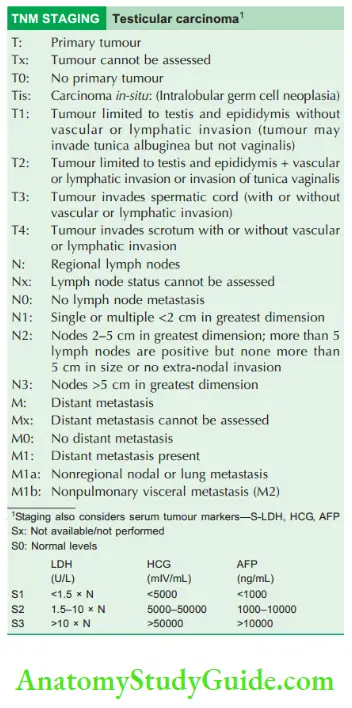
- Stage 3: Tumour and lymph nodes above the diaphragm, mediastinal nodes, pulmonary or liver metastasis, etEach stage can be added letters Smeans tumour markers.
Investigations:
1. Ultrasound of the testis is the first investigation: Seminoma appears as a hypoechoic lesion and nonseminomatous tumours are non-homogenous.
2. Chest X-ray: To rule out cannonball secondaries, as in teratom
3. Abdominal USG to look for enlarged lymph nodes and secondaries in the liver, or to detect a tumour in an undescended testis. However, CT scan is a better investigation.
4. MRI: It is an excellent investigations which can diagnose testicular tumours and can also differentiate from hematoma or orchitis etc.
5. CT scan: Heterogenously enhancing testicular mass with retroperitoneal lymph nodes and liver metastasis can be made out.
6. 24-hours urine sample for HCG:
- Normal levels—≤100 IU
- ≥1000 IU is diagnostic of chorio-carcinoma
- Hence, it is the tumour marker of choriocarcinoma.
7. Human chorionic gonadotrophin: Serum HCG
As the name suggests, it is made by chorionic elements.

- HCG as a whole (α- and β-HCG) may be increased in testicular neoplasm, melanoma, lymphoma, etIt can also be raised in nonmalignant conditions, such as cirrhosis and, peptic ulcer disease.
- β-HCG is more important in diagnosing testicular neoplasms and is also useful in the postoperative period to investigate for residual or recurrent tumour.
- The blood level of β-HCG is 0 ng/ml.
8. α-fetoprotein: Increased in nonseminomatous germ cell tumours.
9. Lactate dehydrogenase (LDH): Increased in nonseminomatous germ cell tumours. LDH levels indicate tumour loaIt is not specific for any tumour.
10. Placental alkaline phosphatase is increased in seminoma testis.
Treatment:
1. Treatment of the Tumour:
- Radical inguinal orchidectomy is the treatment of choice in all testicular tumours irrespective of the histological type and stage. When a patient presents with rapidly growing testicular swelling and the neoplasm is doubtful, the testis is explored through an inguinal incision.
- It is delivered out, and a soft clamp is applied to the testicular vessels at the level of the deep ring while performing the procedure so that tumour embolization does not occur. The testis is split open and the suspicious area is biopsied and sent for a frozen section.
- If the frozen section is positive, the cord and testicular vessels are divided at the level of the deep ring, and the testis is removed this is called high orchidectomy.
- If frozen section is negative, the testis is sutured back and replaced in the scrotum. This type of procedure done through the inguinal route is called Chevasu’s procedure.
2. Treatment of the Retroperitoneum and Metastasis:
1. Seminoma:
Stage 1-2A (low stage): Radiotherapy to the retroperitoneum (2500–3000 cGy) is the treatment of choice:
- The 5-year survival rate is around 95%.
- Relapse after radiotherapy is managed by chemotherapy.
Stage 2B, 3, 4:
- Radical orchidectomy + chemotherapy-PVB regimen—cisplatin, vincristine, bleomycin.
- BEP: Bleomycin, etoposide and cisplatin.
Treatment of residual disease in lymph nodes:
- Stage 2B and 3: If there is residual lymph nodal mass 3 cm in size even after chemotherapy, retroperitoneal lymph node dissection (RPLND) has to be done.
- Stage 2B and 3: 5-year survival rate—75%.
- Stage 4: Poor survival.
2. Teratoma:
- Stage 1, 2A (low stage): Radical orchidectomy ±RPLND 5-year survival–85%.
- Stage 2B, 3: Radical orchidectomy and chemotherapy (PVB), post-chemotherapy residual tumour in the retroperitoneum and if the tumour markers levels regress RPLN5-year survival rate 60%.
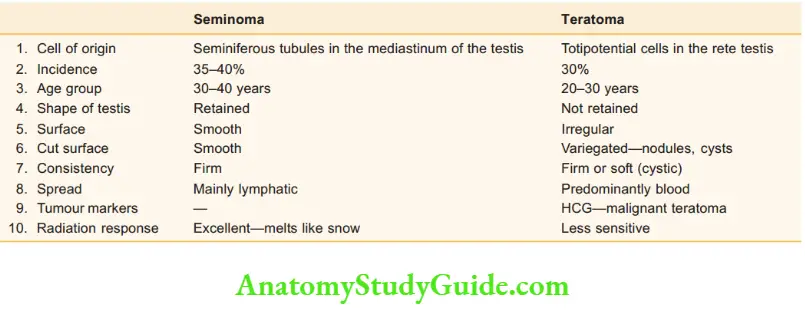
- Comparison of seminoma with teratoma
- Other tumours are given below.
Interstitial Cell Tumours
- Two types are clinically important: Leydig cell tumour and Sertoli cell tumour.
- They should be treated like teratoma.
1. Leydig cell tumour:
- A prepubertal tumour
- Causes masculinisation due to increased androgens—infant Hercules
- Spreads to lymph nodes and lungs
- Good prognosis because it behaves almost like a benign lesion
Comparison of seminoma with teratoma:
2. Sertoli cell tumours:
- Feminizing tumours: Gynaecomastia, loss of libido, and aspermia are other features.
- Increased oestrogen production is responsible for feminisation.
- Postpubertal tumour
- Orchidectomy is the treatment of choice.
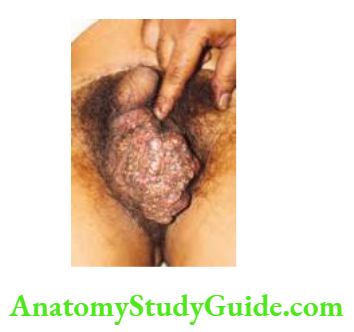
Fournier’S Gangrene (Idiopathic Gangrene Of The Scrotal Skin)
Aetiopathology:
Even though Fournier’s gangrene is called idiopathic gangrene, certain factors precipitate.
- Low socio-economic group patients.
- Unhygienic conditions
It follows perianal abscesses, urogenital instrumentation or a scratch, cut or bruise in the scrotal skin.
Causative Organisms:
- Microaerophilic Haemolytic streptococci
- Staphylococci
- E. coli
- Anaerobes: Clostridium welchii (Can be compared to Meleney’s ulcer—synergistic gangrene—affecting the skin of the abdominal wall. Today it is grouped under necrotizing fasciitis).
Clinical Features:
1. Common in young apparently healthy individuals
2. Sudden appearance of scrotal inflammation—red, swollen, very painful. Patient is toxic with fever and prostration.
3. Within 1–2 days, extensive gangrene of the scrotal skin occurs resulting in sloughing of the scrotal skin which exposes the testicles. In a few cases, the gangrene can involve the skin of the penis, the anterior abdominal wall, the medial side of thigh, and the perianal region. In such situations, it is described as perineal phlegmon.
4. Luckily, the testis does not get involved in Fournier’s gangrene because of thick tunica albuginea.
Treatment:
1. Broad-spectrum antibiotics are started, once pus is sent for culture and sensitivity
- Metronidazole for anaerobe



- Gentamicin for gram-negative organisms
- Ampicillin for gram-positive organisms
- Cephalosporins may have to be added if required.
2. The gangrenous portion of the scrotum has to be excised as soon as possible, which dramatically reverses the general condition of the patient from toxic to near normal.
3. If the testicles are exposed, they can be implanted in the thigh, or once inflammation subsides, skin grafting is done to cover the testicles.
4. If the penile skin is gangrenous, it is excised and covered with a split skin graft later. Surprisingly, results are better than expected

Miscellaneous:
Fracture Of The Penis
It is a misnomer:
- It is the traumatic rupture of the corpora cavernosum. It is considered a urologic emergency.
- Sudden blunt trauma or abrupt lateral bending of the penis in an erect state can break the markedly thin and stiff tunica albuginea.
- One or both corpora may be involved with concomitant urethral (38%) injury if both corpora are involved.
- Causes: Sexual activity, masturbation, gunshot wounds, industrial accidents, mechanical trauma.
- Diagnosed clinically.
- In equivocal cases—cavernosonography or MRI.
- Preoperative retrograde urethrography urethral injury is suspected.
Treatment
1. Medical: Fluids, antibiotics. If surgical therapy is delayed due to urethral injury, initial medical therapy consists of cold compresses, pressure dressings, anti-inflammatory medications and suprapublic cystostomy.
2. Surgical: Evacuate haematoma, identify site of injury, correct the defect in tunica albuginea, repair urethral injury, remove urethral catheter after 2 weeks.
Complications:
Erectile dysfunction, abnormal curvature, painful erections, urethrocutaneous fistula, corpora-urethral fistula, and painful nodules.
Priapism:
- Priapism is a pathologic condition of a penile erection that persists beyond or is unrelated to sexual stimulation.
- It can occur in all age groups including the newborn but the peak incidence is at:
- 5–10 years
- 20–50 years.
Causes:
1. Low flow: Sickle cell trait/disease, chronic myeloid leaukemia, total parenteral nutrition, medications (sildenafil, cocaine), malignant penile infiltration, spinal cord injury, spinal anaesthesia, or general anaesthesia.
2. High flow: Perineal or penile trauma.
Two Types:
Type I: Low flow priapism (veno-occlusive)
- Decreased venous outflow
- Increased intracavernosal pressure
- Painful, fully erect penis
- Local hypoxia and acidosis
- It is the most common variety.
Type 2: High flow priapism
- High inflow and high outflow
- Penis is erect but nontender
- Corporal blood gas analysis can differentiate low flow and high flow priapism.
Treatment:
1. Low flow priapism: Corporal irrigation with normal saline and α-adrenergic intracorporal injections (epinephrine/phenylephrine/ephedrine) every 5 min till detumescence. In severe cases—shunts (corporoglandular, corporospongiosal or corporosaphenous) may be necessary. If patient has sickle cell disease, IV bicarbonate and blood transfusions are required.
2. High flow priapism: Doppler ultrasound is done to identify arterial-lacunar fistul Arterial embolization or open surgical arterial ligation is done.
Male Infertility
Sperms are produced in the seminiferous tubules and are: Stored and matured in epididymis.
- The vas deferens carry the sperm from the epididymis to the prostatic urethra.
- Before opening into urethra, they are joined by the ducts of the seminal vesicles.
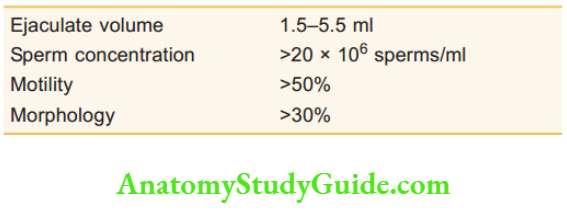
- The seminal vesicles and vas deferens ducts join to form the ejaculatory duct. Semen analysis—minimal standards of adequacy:
If abnormalities are present on semen analysis, causes may include the following:

Evaluation of Azoospermia:

Sperm Retrieval Techniques for Assisted Reproductive Technology (ART):
Useful in cases where transport of sperms is not possible, (e.g. vasal agenesis).
- The pre-requisite is that production should be going on.
- Aspiration can be achieved from
- Testes: Most recent technique—testicular sperm aspiration (TESA), testicular sperm extraction (TESE), micro-TESE.
- Epididymis: Used when the vas is unavailable for aspiration—microsurgical epididymal sperm aspiration (MESA), percutaneous epididymal sperm aspiration (PESA).
- Vas deferens: Most mature/fertilizable sperm present.
Urology Multiple Choice Questions
Question 1. The following are true regarding surgical anatomy of the penis except:
- Corpora cavernosa are vascular spaces
- Arterioles are corkscrew-shaped
- Attached to symphysis pubis by suspensory ligament
- Deep artery supplies the corpus spongiosum alone
Answer: 4. Deep artery supplies the corpus spongiosum alone
Question 2. Balanitis refers to:
- Inflammation of the glans penis
- Inflammation of the prepuce
- Inflammation of glands in the fossa navicularis
- Inflammation of the urethral glands
Answer: 1. Inflammation of the glans penis
Question 3. Dorsal slit is given for which condition?
- Phimosis
- Paraphimosis
- Carcinoma penis
- Balanitis
Answer: 2. Paraphimosis
Question 4. The following are complications of phimosis except:
- Paraphimosis
- Carcinoma penis
- Balanoposthitis
- Buschke-Lowenstein tumour
Answer: 4. Buschke-Lowenstein tumour
Question 5. Which of the following is a rare feature of carcinoma penis?
- Foul-smelling discharge
- Recent phimosis
- Urethral involvement
- Extensive induration
Answer: 3. Urethral involvement
Question 6. Treatment of carcinoma penis confined to the prepuce is:
- Circumcision
- Dorsal slit and excision
- Partial amputation
- Radiotherapy
Answer: 1. Circumcision
Question 7. The following are true for partial amputation of the penis except:
- Partial amputation is the treatment for a growth confined to the glans penis
- At least a 2 cm proximal shaft is necessary
- A long ventral flap is required to cover
- Perineal urethrostomy may be required
Answer: 4. Perineal urethrostomy may be required
Question 8. The following are a few important considerations in total amputation of the penis except:
- Suspensory ligaments have to be divided
- Perineal urethrostomy has to be done
- Severe excoriation of the scrotum is a complication
- The advantage is no stricture urethra after surgery
Answer: 4. The Advantage is no stricture urethra after surgery
Question 9. The following are features of syphilitic chancre of the penis except:
- Single ulcer
- Hard chancre
- Firm painful lymph nodes in the axilla
- Contagious
Answer: 3. Firm painful lymph nodes in the axilla
Question 10. Testosterone is produced by:
- Germ cells
- Sertoli cells
- Leydig cells
- Clear cells
Answer: 3. Leydig cells
Question 11. The testicular artery is a branch of the:
- Aorta
- Common iliac artery
- Internal iliac artery
- External iliac artery
Answer: 1. Aorta
Question 12. The following are true for prostate specific antigen except:
- Released from columnar prostatic acinar epithelial cells
- More than 4 nmol/ml suggests carcinoma prostate
- Prostatitis can also increase its levels
- It does not help in assessing the response to treatment
Answer: 4. It does not help in assessing the response to treatment
Question 13. Which of the following tests differentiates encysted hydrocoele from spermatocoele?
- Fluctuation
- Getting above the swelling
- Cough impulse
- Traction test
Answer: 4. Traction test
Question 14. What is the classical clinical feature of tuberculous epididymal-orchitis?
- Thickened vas
- Atrophy of the testis
- Craggy epididymis
- Anterior sinus
Answer: 3. Craggy epididymis
Question 15. Chinese lantern type of transillumination is classical of:
- Spermatocoele
- Epididymal cyst
- Ranula
- Cystic hygroma
Answer: 2. Epididymal cyst
Question 16. Which of the following is true in cases of retractile testis?
- It is premalignant
- Testis is generally not palpable
- Scrotum is well developed
- Testis cannot be brought down into the scrotum
Answer: 3. Scrotum is well developed
Question 17. In torsion testis, the following are true except:
- Scrotum is empty
- Tender lump at the external abdominal ring
- Elevation of the scrotum increases pain
- Upper abdominal pain and vomiting are features
Answer: 4. Upper abdominal pain and vomiting are features
Question 18. Which of the following is more prone to testicular tumour?
- Gardner’s syndrome
- Down’s syndrome
- Klinefelter’s syndrome
- Sipple syndrome
Answer: 3. Klinefelter’s syndrome
Question 19. Human chorionic gonadotrophin elevation is diagnostic of:
- Choriocarcinoma
- Seminoma
- Leydig cell tumour
- Sertoli cell tumour
Answer: 1. Choriocarcinoma
Question 20. Which of the following is true for seminoma?
- It arises from rete testis
- Undescended testis predisposes to it
- It secretes β-HCG
- It spreads predominantly by blood
Answer: 2. Undescended testis predisposes to it
Leave a Reply