Pathogenesis Of Cell Injury
Injury to the normal cell by one or more of the etiologic agents listed above may result in a state of cell injury which may be reversible or irreversible. The underlying alterations in biochemical systems of cells for reversible and irreversible cell injury by various agents are complex and varied.
However, irrespective of the type of cell injury, following general features characterise most forms of cell injury by various agents:
Read And Learn More: General Pathology Notes
1. Factors pertaining to etiologic agent and host:
Following parameters pertaining to etiologic agent or host determine the outcome of cell injury:
- Type, duration and severity of injurious agent: The extent of cellular injury depends upon type, duration and severity of the stimulus for example,Small dose of chemical toxin or short duration of ischaemia cause reversible cell injury while large dose of the same chemical agent or persistent ischaemia cause cell death.
- Type, status and adaptability of target cell: The type of cell as regards its susceptibility to injury, its nutritional and metabolic status, and adaptation of the cell to hostile environment determine the extent of cell injury for example,Skeletal muscle can withstand hypoxic injury for longtime while cardiac muscle suffers irreversible cell injury after persistent ischaemia due to total coronary occlusion for >20 minutes.
Read And Learn More: General Pathology Notes
2. General underlying mechanisms:
Regardless of other factors, following general intracellular biochemical phenomena underlie most forms of cell injury:
- Mitochondrial damage causes ATP depletion.
- Cell membrane damage disturbs the metabolic and trans-membrane exchanges.
- Release of reactive oxygen-derived free radicals.Reduced protein synthesis and nuclear damage.
3. Usual morphologic changes:
Biochemical and molecular changes underlying cell injury from various agents become apparent first and are associated with the appearance of ultrastructural changes in the injured cell.
- However, eventually, morphologic changes in the gross appearance of organs and light microscopic changes in cells appear.
- The morphologic changes of reversible cell injury (for example, Hydropic swelling) appear earlier while morphologic alterations of cell death occur later (for example, In myocardial infarction).
4. Functional implications and disease outcome:
Eventually, cell injury affects cellular function adversely which has a bearing on the body.
- Consequently, clinical features in the form of symptoms and signs would appear. Further course or prognosis will depend upon the response to treatment versus the biological behaviour of the disease.
- The interruption of blood supply (i.e. ischaemia) and impaired oxygen supply to the tissues (i.e. hypoxia) are the most common forms of cell injury in human beings.
- Pathogenesis of hypoxic and ischaemic cell injury is, therefore, described in detail below followed by a brief discussion on the pathogenesis of chemical and physical (principally ionising radiation) agents.
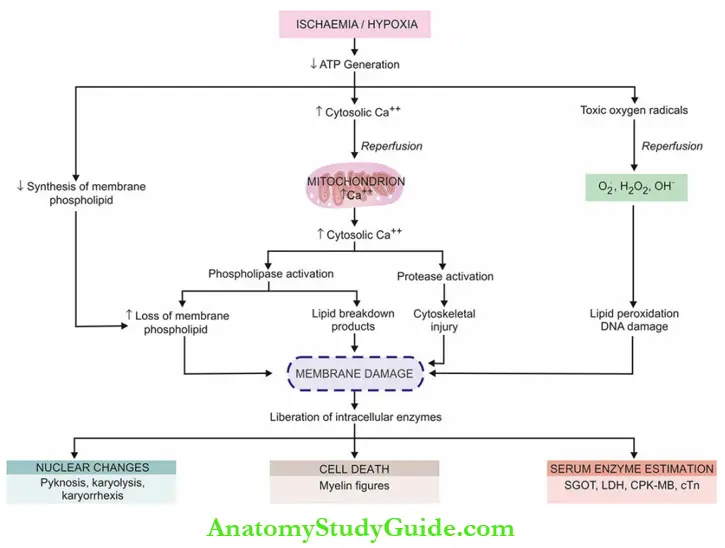
Pathogenesis Of Ischaemic-Hypoxic Injury:
Ischaemia and hypoxia are the most common forms of cell injury. Although underlying intracellular mechanisms and ultrastructural changes seen in reversible and irreversible cell injury by hypoxia-ischaemia (depending upon the extent of hypoxia and type of cells involved) are a continuation of the process, these mechanisms are discussed separately below and illustrated diagrammatically in.
Reversible Cell Injury:
If the ischaemia or hypoxia is of short duration, the effects may be reversible on rapid restoration of circulation for example, In coronary artery occlusion, myocardial contractility, metabolism and ultrastructure are reversed if the circulation is quickly restored.
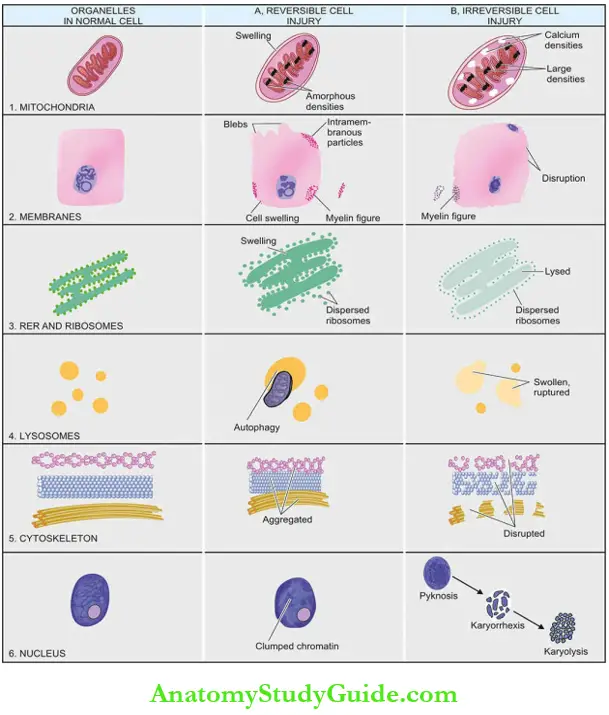
The sequential biochemical and ultrastructural changes in reversible cell injury are under
1. Decreased generation of cellular ATP: Damage by ischaemia from interruption versus hypoxia from other causes:
All living cells require a continuous supply of oxygen to produce ATP which is essentially required for a variety of cellular functions (for example, Membrane transport, protein synthesis, lipid synthesis and phospholipid metabolism).
ATP in human cells is derived from 2 sources:
- Firstly, aerobic respiration or oxidative phosphorylation occurs in the mitochondria.
- Secondly, cells may subsequently switch over to anaerobic glycolytic oxidation to maintain a constant supply of ATP (in which ATP is generated from glucose/glycogen in the absence of oxygen).
Ischaemia due to interruption in blood supply and hypoxia from other causes limit the supply of oxygen to the cells, thus causing decreased ATP generation from ADP:
- In ischaemia from interruption of blood supply, aerobic respiration as well as glucose availability are both compromised resulting in more severe and faster effects of cell injury.
- Ischaemic cell injury also causes the accumulation of metabolic waste products in the cells. On the other hand, in hypoxia from other causes (for example, RBC disorders, heart disease, lung disease), anaerobic glycolytic ATP generation continues, and thus cell injury is less severe.
It has been found that human cells exert a protective response to hypoxia by release of a transcription factor, hypoxia-inducible factor 1 (HIF-1), which increases anaerobic glycolysis and stimulates cell survival.
However, highly specialised cells such as myocardium, proximal tubular cells of the kidney, and neurons of the nervous system are dependent solely on aerobic respiration for ATP generation and thus these tissues suffer from ill effects of ischaemia more severely and rapidly.
2. Intracellular lactic acidosis:
Nuclear clumping Due to low oxygen supply to the cell, aerobic respiration by mitochondria fails first. This is followed by a switch to an anaerobic glycolytic pathway for the requirement of energy (i.e. ATP).
This results in rapid depletion of glycogen and accumulation of lactic acid lowering the intracellular pH. Early fall in intracellular pH (i.e. intracellular lactic acidosis) results in clumping of nuclear chromatin.
3. Damage to plasma membrane pumps:
Hydropic swelling and other membrane changes Lack of ATP interferes in the generation of phospholipids (which are a major constituent of cell membranes) from the cellular fatty acids which are required for continuous repair of membranes.
This results in damage to membrane pumps operating for the regulation of sodium-potassium and calcium as under:
- Failure of sodium-potassium pump: Normally, the energy (ATP)-dependent sodium pump (also called Na+-K+ ATPase) operating at the plasma membrane allows active transport of sodium out of the cell and diffusion of potassium into the cell.
- Lowered ATP in the cell lowers the activity of the sodium pump and consequently interferes with this membrane-regulated process.
- This results in intracellular accumulation of sodium and diffusion of potassium out of the cell. The accumulation of sodium in the cell leads to an increase in intracellular water to maintain isoosmotic conditions (i.e. hydropic swelling occurs, discussed later in this chapter).
- Failure of calcium pump: Membrane damage causes disturbance in the calcium ion exchange across the cell membrane. Excess of calcium moves into the cell (i.e. calcium influx), particularly in the mitochondria, causing its swelling and deposition of phospholipid-rich amorphous densities.
4. Reduced protein synthesis:
Dispersed ribosomes As a result of continued hypoxia, membranes of the endoplasmic reticulum and Golgi apparatus swell up. Ribosomes are detached from granular (rough) endoplasmic reticulum and polysomes are degraded to monosomes, thus dispersing ribosomes in the cytoplasm and inactivating their function.
Similar reduced protein synthesis occurs in the Golgi apparatus.
Ultrastructural evidence of reversible cell membrane damage is seen in the form of loss of microvilli, intramembranous particles and focal projections of the cytoplasm (blebs).
Myelin figures may be seen lying in the cytoplasm or present outside the cell; myelin figures are derived from membranes (plasma or organellar) enclosing water and dissociated lipoproteins between the lamellae of injured membranes.
Lysosomes may engulf damaged organelles and form autophagic
vacuoles. Up to this point, withdrawal of acute stress that resulted in reversible cell injury can restore the cell to a normal state.
Irreversible Cell Injury:
Persistence of ischaemia or hypoxia results in irreversible damage to the structure and function of the cell (cell death). The stage at which this point of no return or irreversibility is reached from reversible cell injury is unclear but the sequence of events is a continuation of reversibly injured cells. Two essential phenomena always distinguish irreversible from reversible cell injury
- The inability of the cell to reverse mitochondrial dysfunction on reperfusion or reoxygenation.
- Disturbance in cell membrane function in general, and in plasma membrane in particular.
In addition, there is a further reduction in ATP, continued depletion of proteins, reduced intracellular pH, and leakage of lysosomal enzymes into the plasma.
These biochemical changes have effects on the ultrastructural components of the cell:
1. Calcium influx:
Mitochondrial damage As a result of continued hypoxia, a large cytosolic influx of calcium ions occurs, especially after reperfusion of irreversibly injured cells.
- Excess intracellular calcium enters and accumulates inside the mitochondria disabling its function.
- Its morphological changes are expressed in the form of vacuoles in the mitochondria and deposits of amorphous calcium salts in the mitochondrial matrix.
2. Activated phospholipases:
Membrane damage Damage to membrane function in general, and plasma membrane in particular, is the most important event in irreversible cell injury.
- Increased cytosolic influx of calcium in the cell activates endogenous phospholipases. These, in turn, degrade membrane phospholipids progressively which are the main constituent of the lipid bilayer membrane.
- Besides, there is also decreased replacement synthesis of membrane phospholipids due to reduced ATP. Another lytic enzyme, ATPase, is activated, thus causing further depletion of ATP.
3. Activate intracellular proteases:
Cytoskeletal damage The normal cytoskeleton of the cell (microfilaments, microtubules and intermediate filaments) which anchors the cell membrane, is damaged due to degradation by activated intracellular proteases or by physical effect of cell swelling, producing irreversible cell membrane injury.
4. Activated endonucleases:
Nuclear damage DNA or nucleoproteins are damaged by the activated lysosomal enzymes such as proteases and endonucleases.
Irreversible damage to the nucleus may occur in the following three forms:
- Pyknosis Condensation and clumping of a nucleus which becomes dark basophilic.
- Karyorrhexis Nuclear fragmentation into small bits dispersed in the cytoplasm.
- Karyolysis Dissolution of the nucleus.
Damaged DNA activates pro-apoptotic proteins leading the cell to death.
5. Lysosomal hydrolytic enzymes:
Lysosomal damage, cell death and phagocytosis The lysosomal membranes are damaged and ruptured which results in the escape of lysosomal hydrolytic enzymes. These enzymes are activated due to a lack of oxygen in the cell and acidic pH.
- These hydrolytic enzymes (for example, Hydrolase, RNAase, DNAase, protease, glycosidase, phosphatase, lipase, amylase, cathepsin etc), on activation, bring about enzymatic digestion of cellular components and hence cell death.
- The dead cell is eventually replaced by masses of phospholipids called myelin figures which are either phagocytosed by macrophages or there may be the formation of calcium soaps.
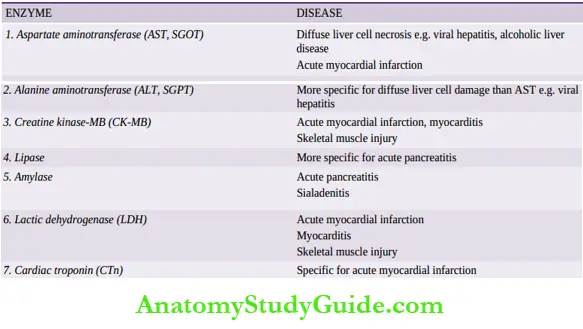
- Liberated enzymes just mentioned leak across the abnormally permeable cell membrane into the serum, the estimation of which may be used as clinical parameters of cell death.
- For example, in myocardial infarction, estimation of elevated serum glutamic oxaloacetic transaminase (SGOT), lactic dehydrogenase (LDH), isoenzyme of creatine kinase (CK-MB), and cardiac troponins (cTn) are useful guides for death of heart muscle.
- Some of the common enzyme markers for different forms of cell death are given below.
- While cell damage from oxygen deprivation by the above mechanisms develops slowly, taking several minutes to hours, the cell injury may be accentuated after the restoration of blood supply and subsequent events termed ischaemic-reperfusion injury and liberation of toxic free radicals (or reactive oxygen species), discussed below.
Ischaemic-Reperfusion And Free Radicalmediated Cell Injury:
Depending upon the duration of ischaemia/hypoxia.
Restoration of blood flow may result in the following 3 different consequences:
- From ischaemia to reversible injury: When the period of ischaemia is of short duration, reperfusion with the resupply of oxygen restores the structural and functional state of the injured cell i.e. reversible cell injury.
- From ischaemia to irreversible injury: Another extreme is when a much longer period of ischaemia has resulted in irreversible cell injury during ischaemia itself i.e. when so much time has elapsed that neither blood flow restoration is helpful nor has reperfusion injury developed.
- Cell death in such cases is not attributed to the formation of activated oxygen species.
- But instead, on reperfusion in such a case there is further marked intracellular excess of sodium and calcium ions due to persistent cell membrane damage.
- From ischaemia to reperfusion injury: When ischaemia is for somewhat longer duration, then restoration of blood supply to injured but viable cells (i.e. reperfusion), instead of restoring structure and function of the cell, paradoxically deteriorates the already injured cell and leads it to cell death.
This is termed ischaemia-reperfusion injury. Examples of such forms of cell injury are irreversible cell injury in myocardial and cerebral ischaemia.
Common enzyme markers of cell death:
Leave a Reply