Salivary Glands Introduction
- There are three pairs of salivary glands—parotid, submandibular and sublingual. In addition to these, there are many (450) minor salivary glands located in the cheek, mucosa, lips, palate and base of the tongue.
- Parotid, the “big brother of 3”, suffers mainly from three diseases—infection, enlargement and tumour. Submandibular salivary gland suffers from mainly two diseases sialoadenitis and tumours.
Read And Learn More: General Surgery Notes
Table of Contents
- Other salivary glands are of minor importance. However, it should be remembered that the commonest tumour of minor salivary glands is malignancy.
Describe surgical anatomy of the salivary glands, pathology and clinical presentation of disorders of salivary glands.
Enumerate the appropriate investigations and describe the principles of treatment of disorders of salivary glands.
Surgical Anatomy Of The Parotid Gland
- Parotid gland is present on the lateral aspect of the face, divided by the facial nerve into superficial lobe and deep lobe.
- Superficial lobe overlies the masseter and the mandible. Deep lobe is wedged between the mastoid process and the styloid process, ramus of the mandible and medial pterygoid muscle.
- The superficial lobe also receives a duct from the accessory lobe which is in the region of zygomatic arch/ zygomatic process.
- The duct of parotid, Stensen’s duct, 2–3 mm in diameter, receives tributaries from superficial, deep and accessory lobes, passes through the buccinator muscle and opens in the mucosa of the cheek opposite the upper 2nd molar tooth.
- Parotid gland is covered by a true capsule which is a condensation of fibrous stroma of the gland and a false capsule formed by parotid fascia, a part of the deep cervical fascia.
Surgical Anatomy Of The Parotid Gland Facial Nerve:
- After emerging from stylomastoid foramen, it hooks around the condyle of mandible, enters the substance of the parotid and divides into 2 major branches, zygomaticotemporal and cervicofacial.
- Facial nerve along with retromandibular vein (which is formed by the union of superficial temporal vein and maxillary vein, formed from branches of pterygoid plexus of veins) is present in this plane. This plane is called the fasciovenous plane of Patey.


- The facial nerve then gives rise to 5 branches which are interconnected like the foot of a goose, called Pes anserinus.
- Branches of facial nerve in the face and the muscles supplied by these nerves are given.
Facial nerve and its branches:


Recurrent Parotitis Of Childhood
- Children between ages of 3 and 6 years are commonly affected.
- Aetiology is unknown, may be due to sialectasis (dilatation of branches of salivary duct).
- Recurrent pain and swelling of one or both parotids is common.
- Each attack may last for 3 to 7 days.
- It is self-limiting (if the attack is minor).
- Sialography shows punctate sialectasis, called snowstorm appearance.
- A short course of antibiotics has to be given to cover Streptococcus viridans.
- Rarely, superficial parotidectomy may be necessary.
Surgical Anatomy Of The Submandibular Salivary Gland
- Submandibular salivary gland is located in the submandibular triangle. It lies partly below and partly over the mandible.
- It is in very close contact with the belly of the digastric muscle. At surgery, once the deep fascia is opened, the intermediate tendon of digastric is located and when it is retracted downwards, mobilisation of the gland becomes easy.
- Submandibular salivary gland is divided into a superficial part and a deep part by the mylohyoid muscle which forms the oral diaphragm. During excision of the gland, a few fibres of mylohyoid are also removed.
- When submandibular salivary gland enlarges, it is bidigitally palpable because the deep portion is deep to mylohyoid and it is in the floor of the mouth.
- Facial artery enters the gland from its posterolateral surface and deeply grooves the gland. It is ligated at this place first during excision of the gland.
- After grooving the gland, it ascends laterally and curls around the lower border of mandible to enter the face. It is ligated at this place also.
- Main duct of submandibular gland, Wharton’s duct arises from deep part of gland and opens on a papilla beside the frenulum of the tongue in the oral cavity.

- In a deeper plane, the gland is related to two nerves— lingual and hypoglossal.
Chronic Submandibular Sialoadenitis
- Obstruction is the most important cause of submandibular sialoadenitis. Trauma to the floor of the mouth is another cause.
- Obstruction can be due to stone, disease, stricture of the duct, or fibrosis of the papilla (calculus—most common).
- The causative organism is Staphylococcus.
Sialoadenitis Due To Calculi
- The disease starts with acute bacterial sialoadenitis which occurs secondary to obstruction. The submandibular gland has a poor capacity for recovery following infection.
- Despite control of acute symptoms with antibiotics, the gland becomes chronically inflamed.
- Calculi (80% of them occur in the submandibular salivary gland) commonly occur in the duct and also within the gland and produce recurrent sialoadenitis.
Calculi are more common in the submandibular salivary gland than in the parotid gland because of the following reasons:
- Higher mucin content in the submandibular salivary gland secretions.
- Calcium and phosphate content in the secretion is high. Hence, 80% of them are radiopaque and are detected by plain X-ray.
- Nondependent drainage of the secretions. Gland is in the neck and opening of the duct in the oral cavity.
- Kinking or hooking of submandibular duct by lingual nerve.

Chronic Submandibular Sialoadenitis Clinical Features:
Submandibular Salivary Gland Enlargement:
-
- Location—submandibular region
- Lobular, firm swelling
- Bidigitally palpable
- Stone may be palpable within the duct, intraorally
- Salivary colic: It is a severe pricking type of pain which is exaggerated at the time of meals. Salivary secretions are induced by a meal or lemon (lemon juice test). As a result of blockage due to a stone, the tension within the gland increases, resulting in pain.
- Lingual colic: If a calculus is situated within the submandibular duct where it is hooked by lingual nerve, the pain can radiate to the tongue as a result of irritation to the lingual nerve.
- Enlargement of salivary gland during meals is the characteristic feature of salivary calculus. Classically submandibular salivary gland swelling is located in the submandibular region.
- It is firm in consistency with a lobular surface. It is tender and both lobes are enlarged. It is bidigitally palpable (submandibular lymph node is palpable only in the neck) both inside the oral cavity and in the neck. The swelling reduces in size once the stimuli are withdrawn (after meals).
- The stone may be palpable within the gland (in the neck), within the duct (intraorally), or sometimes it may be seen at the orifice of the submandibular duct on the side of lingual frenulum.
- It is not uncommon to get severe septic sialoadenitis with gross swelling of the gland and inflammatory oedema almost like Ludwig’s angina.
Chronic Submandibular Sialoadenitis Investigations:
Ultrasound can easily detect the stone as hypoechoic areas, enlargement of gland and location of the stone. More common is stones are located in the distal part of the duct.
Chronic Submandibular Sialoadenitis Treatment:
An oblique lateral or posterior oblique occlusal radiography may demonstrate a stone.
1. Stone in the submandibular duct:
This can be removed by incising the mucosa over the floor of the mouth, after stabilising the stone. Removal of the stone is followed by gush of old dirty contents of the submandibular gland.


2. Chronic sialoadenitis:
This requires excision of submandibular salivary gland. Three steps of dissection of the gland include incision, mobilisation and excision.
- Incision: It should be a skin crease incision over the lower pole of the gland, the posterior limit of the incision should be at least 2 cm away from the angle of the mandible, to avoid damage to the cervical branch of facial nerve. The incision is deepened till the deep fascia is opened.
- Mobilisation of the gland: Division of the facial artery twice, once in a deeper plane on the posterolateral aspect and another at the superolateral aspect close to the lower border of the mandible is an important step which permits mobilisation of the gland. Separation of the gland from fibres of mylohyoid muscle by dividing small arteries completes the mobilisation.
- Excision of the gland: It is done by ligating and dividing submandibular duct.
Chronic Submandibular Sialoadenitis Complications:
- Damage to lingual nerve, marginal mandibular nerve or even to hypoglossal nerve. Seroma and infection are the other complications.
- Transection of the nerve to mylohyoid muscle produces anaesthesia of the submental skin.
Submandibular salivary gland excision:


Salivary Gland Tumours
International Classification
- Epithelial tumours
- Nonepithelial tumours.
1. Epithelial Tumours:
1. Adenoma
- Pleomorphic adenoma
- Monomorphic adenomas
- Adenolymphoma (Warthin’s tumour)
- Oxyphilic adenoma (oncocytoma)
- Other types
2. Mucoepidermoid tumours
3. Acinic cell tumour
4. Carcinoma
- Carcinoma in pleomorphic adenoma
- Adenoid cystic carcinoma
- Undifferentiated carcinoma
- Adenocarcinoma
- Epidermoid carcinoma
- Acinic cell tumour
- Mucoepidermoid carcinoma
- Malignant mixed tumour
2. Nonepithelial Tumours:
- Lipoma
- Lymphoma
- Neurofibroma
- Lymphangioma
- Sarcoma
Salivary gland tumours are not uncommon. There are dozens of histological types of salivary gland tumours. However, pleomorphic adenoma and adenolymphoma are the common benign types.
- Carcinoma arising in pleomorphic adenoma, mucoepidermoid tumours and adenoid cystic carcinoma are important malignant tumours.
- Incidence: 80% of salivary gland tumours are found in the parotid gland. Out of these, 80% are benign, of which 80% are pleomorphic adenomas. In the submandibular salivary gland, 50% are benign and 50% are malignant.
- In the minor salivary glands, 90% are malignant. Thus, the incidence of malignancy increases from major to minor salivary glands.
Pleomorphic Adenoma Of Parotid Gland (Mixed Tumour)
It is the most common benign salivary gland neoplasm.
Pleomorphic Adenoma Of Parotid Gland Pathology:
- Epithelial cells proliferate in strands, or may be arranged in the form of acini or cords.
- There are also myoepithelial cells which proliferate in sheets. They are called spindle-shaped cells.
- The tumour produces mucoid material, which displaces and separates the cells resembling cartilage in histological section.
- Because of the presence of epithelial cells, myoepithelial cells, mucoid material, pseudocartilage and lymphoid tissue, the tumour is called pleomorphic adenoma.
- As the tumour grows, it compresses the normal parotid tissue and the branches of the tumour penetrate the thin capsule and enter the substance of the parotid.
- Simple enucleation will result in a recurrence. Hence, superficial parotidectomy has to be done.
Pleomorphic Adenoma Of Parotid Gland Clinical Features:
- Middle-aged women, around 40 years, are commonly affected (female, fifth decade and fullness near ear lobule).
- Typically, a history of very slow-growing swelling (for a few years) is usually present.


- The swelling is painless. Any painless swelling near the ear is best assumed to be parotid gland neoplasm unless proved otherwise
Pleomorphic Adenoma Of Parotid Gland Signs:
- Clinical Examination of Parotid Tumours
- Benign Malignant
- Firm – Firm/hard
- Nodular – Irregular/nodular
- Not fixed – Restricted mobility(fixity to masseter)
- No lymph nodes – Lymph nodes palpable
- Facial nerve is not – Facial nerve paralysis involved
1. Parotid swelling has the following classical features:
- It presents as a swelling in front, below and behind ear.
- Raises ear lobule
- Retromandibular groove is obliterated.
- However, big is the parotid swelling, the upper border is confined (limited) to lower border of zygomatic process because of the attachment of parotid fascia. This is called curtain sign.

2. It is rubbery or firm. Soft areas indicate necrosis. In long-standing cases, it can be hard. Surface can be nodular or sometimes bosselated.
- Skin is stretched and shiny. However, being a benign tumour, it is neither adherent to the skin nor to the masseter.
3. After a few years, pleomorphic adenoma may show features of transformation into malignancy (carcinoma expleomorphic adenoma).
- It should be suspected when
- It starts growing rapidly
- Skin infiltration occurs
- Facial nerve paralysis occurs
- Gets fixed to masseter muscle
- Red, dilated veins over the surface
- Presence of lymph nodes in the neck
- Tumour feels stony hard.
Carcinoma ex Pleomorphic Adenoma (Ca ex PA):
- Presents as a firm mass
- Features of infiltration of facial nerve, masseter muscle, skin or bone may be present
- It occurs due to progressive change: Loss of heterozygosity (LoH) at chromosomal arms 8q, then 12Q and 17Q.
- Mutation of p53—a tumour suppressor gene is also implicated in the malignant transformations of Ca ex PA.
- In high-grade Ca ex PAs, epidermal growth factor receptor (EGFR) is overexpressed. Thus, it may have a role in ‘invasive’ Ca ex PAs.
Intraoral Examination
- Approximately 10% of the parotid tumours are behind the facial nerve in the deep lobe.
- This is appreciated by intraoral examination wherein the tumour presents with a parapharyngeal mass which displaces the tonsil or soft palate medially.
- Deep lobe tumours present as dysphagia. Such tumours may not show gross swelling on the outer aspect but as they grow, they pass through the stylomandibular tunnel of Patey and push the pharyngeal wall, tonsil and soft palate. These tumours are called dumbbell tumours.




Differential Diagnosis of Swelling in the Parotid Region:
1. When it involves the preparotid region and angle of mandible:
- Preparotid lymph node enlargement: It may be enlarged due to tuberculosis, metastasis or in nonHodgkin’s lymphoma. Sebaceous cyst in preparotid region
- Preauricular dermoid cyst (young patients)
- Mesenchymal tumours such as lipoma, neurofibroma
- Haemangioma, lymphangioma
2. When it involves lower pole of parotid:
- Upper jugular chain lymph node enlargement metastatic or tubercular
- Branchial cleft cyst
- Epithelial inclusion cyst
Pleomorphic Adenoma Of Parotid Gland Investigations:
Slow-growing parotid tumours should not be subjected to biopsy for two reasons:
- Injury to the facial nerve.
- Seeding of tumour cells in the subcutaneous plane
Which causes recurrence in about 40–50% of cases:
- Ultrasound is the first investigation. It can recognise the organ of origin and can detect solid areas. It can assess neck lymph nodes also. Cystic areas represent necrosis. Thus ultrasound-guided fine needle. Fine needle aspiration cytology (FNAC) is done to confirm the diagnosis and rule out malignancy.
- CT scan is done when the tumour is arising from the deep lobe. It helps to define the extraglandular spread, the extent of parapharyngeal disease, cervical lymph nodes and bony infiltration. Indications for CT scan
- Suspected bone destruction at skull base
- Suspected involvement of mandible
- To assess neck nodes
- FNAC of the lymph nodes that are palpable in the neck in cases of malignancy of the parotid gland.
- X-ray of the bones (mandible and mastoid process) to look for bony resorption, if malignancy is suspected.

MRI is a better investigation. However, it is expensive—CT scan and MRI lack specificity for differentiating between benign and malignant lesions.
Indications for MRI:
- Delineating the interface between tumour and normal salivary gland.
- Better imaging of the parapharyngeal space.
- Evaluating perineural spread, e.g. adenoid cystic carcinoma.
- Facial nerve status may be better appreciated.

Before we discuss treatment, let us study a few terminologies of parotidectomy. Parotidectomy:
- Superficial: When superficial lobe is removed (superficial to facial nerve).
- In cases of deep lobe enlargement, whole gland has to be removed—total parotidectomy.
- Superficial (partial) adequate: Only tumour with small portion of cuff of parotid gland is removed. Entire lobe is not removed.
- Total: Removal of the entire parotid gland.
- Radical: Total parotidectomy with or without removal of skin, petrous temporal bone, temporomandibular joint, facial nerve with selective neck dissection.
- Extended: Total parotidectomy + sacrifice facial nerve + removal of adjacent structures which are infiltrated such as mandible or masseter muscle, etc.
Extracapsular Dissection:
- It is an alternative method of dissection of parotid gland
- Here, nerve is not dissected
- Hence, less invasive
- Temporary facial nerve paralysis is also very less—less than 10%
- Dissection is started in the plane just above parotid fascia (shining)
- After raising skin flaps, a cruciate incision is made over the surface of the tumour, flaps raised, tumour is dissected all around 2 mm.
Treatment of Pleomorphic Adenoma:
Superficial parotidectomy.

Superficial Parotidectomy:
- Indicated in pleomorphic adenoma and other benign neoplasms.
- Tumour along with the normal lobe is removed.
- Preserve the facial nerve, even in malignant tumours unless grossly involved.
- Avoid rupture of the gland.
- Enucleation should not be done as it causes recurrence.
It is the standard surgery done for benign pleomorphic adenoma. It means removal of the entire lobe containing the tumour which is superficial to the facial nerve.
- Facial nerve should always be preserved. Enucleation should never be done as it causes recurrence and can injure facial nerve. It is difficult to remove a recurrent tumour.
Some Important Steps of Superficial Parotidectomy:
1. Adequate exposure by an incision which starts in front of tragus of ear, vertically descends downwards, curves round the ear lobule up to the mastoid process and is carried downwards in the neck (‘Lazy S’ incision).
2. Recognising the facial nerve at surgery:
- Facial nerve lies 1 cm inferomedial to the bony cartilaginous junction of external auditory canal (Conley’s pointer).
- In very difficult cases, identify styloid process and nerve is superficial to it.
- Trace the posterior belly of digastric up to the mastoid process. Facial nerve is in between the muscle and tympanic plate (immediately above the muscle).
- A nerve stimulator may be used.
3. Developing a plane: Facial nerve and retromandibular vein divide the parotid gland into superficial and deep lobes. Benign tumours do not invade this faciovenous plane of Patey.
4. Gentle handling, good suction and perfect haemostasis help in clear recognition of the nerve.
5. In toto removal—the tumour along with the lobe to avoid spillage (which is one of the causes of recurrence).
6. Good suction drainage of the wound is necessary to avoid haematoma, wound infection, etc.
What should be Done in Parotid Surgery?
- Wide exposure by an adequate skin flap.
- Always identify facial nerve (best way to avoid injury).
- Minimum surgery to be done is superficial parotidectomy (enucleation can cause recurrence and injury to facial nerve).
- Always try to preserve facial nerve even in malignancies unless it is directly infiltrated.
- If facial nerve is excised, try to reconstruct immediately by nerve graft—greater auricular or sural nerve.
- Always ‘drain’ the cavity.
- Buccal nerve can be excised without any repair.

Total conservative parotidectomy: Excision of superficial and deep lobe of parotid gland while preserving the facial nerve.
Complications of Parotidectomy:
- Flap necrosis—avoid acute bending of the incision and to use gentle retraction
- Facial nerve palsy—careful identification
- Fluid collection: Blood or seroma—perfect haemostasis and drain should be used
- Fistula salivary duct should be ligated
- Frey syndrome—occurs in 10% of the cases Observe 5 Fs. “Details are given later”
Indications for Postoperative Radiotherapy:
- If the deep lobe is involved
- If the lymph nodes are involved
- High grade tumours
- If margins are positive
- Perineural invasion
- Lymphovascular invasion
Postoperative Radiotherapy:
T3/T4 cancer: Adenoid cystic carcinoma recurrent tumours.
Adenolymphoma (Warthin’S Tumour, Papillary Cystadenoma Lymphomatosum)
- Adenolymphoma is not a lymphoma. It is a misnomer (vide infra).
- It is a benign parotid tumour and next common to pleomorphic adenoma. It constitutes about 10% of parotid tumours.
- Origin of adenolymphoma: During development, some parotid tissues get included within lymph nodes (preparotid) which are present within the parotid sheath.
Adenolymphoma Histology:
- It is composed of double-layered eosinophilic epithelium. The inner cells are columnar.
- Presence of lymphatic tissue in the stroma and lymph follicles is characteristic of adenolymphoma (hence the name).
Adenolymphoma Clinical Features:
- Middle-aged or elderly males are commonly affected—usually they are smokers.
- Can be bilateral, in some cases (10%).
- It has smooth surface, round border with soft, cystic consistency.
- Classically, situated at the lower pole of parotid elevating the ear lobule. Sometimes it may be multicentric.
- This tumour affects only parotid gland (very, very rarely other glands may be affected).

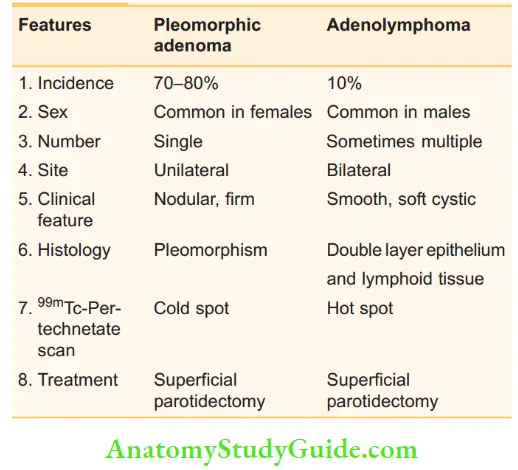
Comparison between pleomorphic adenoma and adenolymphoma:
Adenolymphoma Treatment:
It has got a well-defined capsule. Hence, enucleation used to be done earlier but not now. Superficial parotidectomy is the treatment of choice.
Mucoepidermoid Tumour
- As the name itself suggests, it consists of sheets of epidermoid cells and cystic spaces lined by mucus secreting cells.
- In childhood, it is the commonest parotid tumour. It is benign, slow growing but hard in consistency. (Adenolymphoma and mixed tumours are firm but mucoepidermoid tumour is hard.)
- Parotid is the commonest site. In cases of minor salivary glands, palate is the commonest site.

- Mucoepidermoid tumours can infiltrate local tissues, lymph nodes or skin. Hence, a few consider that mucoepidermoid tumours are always carcinomatous.
- Well-differentiated tumours behave like benign tumours, intermediate ones are aggressive and undifferentiated tumours metastasise early.
- Mucoepidermoid carcinoma is the most common malignant epithelial neoplasm of salivary gland.
- The low grade tumours are composed of predominantly mucus secreting cells. High grade tumours have predominantly epidermoid cells.
- Benign tumours need excision and malignant tumours need radical parotidectomy. Radiation is required in the postoperative period.
Other Tumours
Acinic Cell Tumour:
- These are the uncommon parotid tumours. Commonly occur in women.
- The cells resemble those of serous acini and this tumour also has properties of invasion such as mucoepidermoid tumour. It tends to be soft and sometimes cystic.
Oxyphil Adenoma:
Also called oncocytoma. It occurs exclusively in the parotid gland. It is a solid tumour and occurs in the sixth decade of life.
Adenoid Cystic Carcinoma:
- It is a highly malignant tumour consisting of cords of dark staining cells with cystic spaces containing mucin. It also consists of myoepithelial cells and duct epithelium.
- Even though slow growing, it spreads along the perineural tissue, may invade periosteum or medullary bone at a distance. This bone resorption results in bony tenderness.
- These tumours have a high incidence of distant metastasis but in general, they display indolent growth.
- Skin lesions are common as it spreads along the nerve tissue, which leads to treatment failure.
- Local infiltration, lymphatic and blood spread, and local recurrence are important features.
- It is hard and fixed and can produce anaesthesia of the skin overlying the tumour.
- Early cases are treated by radical parotidectomy with block dissection of the neck. However, many cases present late to the hospital.
- Thus, palliative radiotherapy is given to reduce pain and to arrest progress of the disease.
Summary of Malignant Salivary Gland Tumours:
- To find out the exact type of malignant tumour is of interest to pathologists. Clinically, one can suspect malignancy when a salivary tumour has one of the following features:
- Rapidly growing neoplasm.
- Change in consistency (the tumour tends to be hard).
- Fixity to underlying muscle such as masseter as in parotid tumours.
- Fixity to mandible as in parotid or submandibular tumour.
- Involvement of facial nerve as in 80% of cases of malignant parotid tumours.
- Resorption of adjacent bone such as mastoid, tenderness as in adenoid cystic carcinoma.
- Significant hard nodes in the neck.
- They are treated by radical sialoadenectomy with radical block dissection of the neck. Radiotherapy is used as a palliative treatment.
Malignant Parotid Tumours





Comparison between submandibular and parotid tumours:

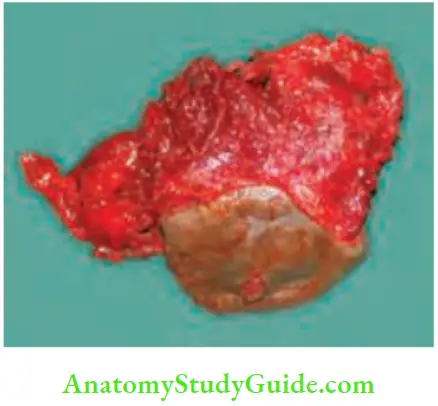
Operative Photographs



Frey’s Syndrome – Gustatory Sweating
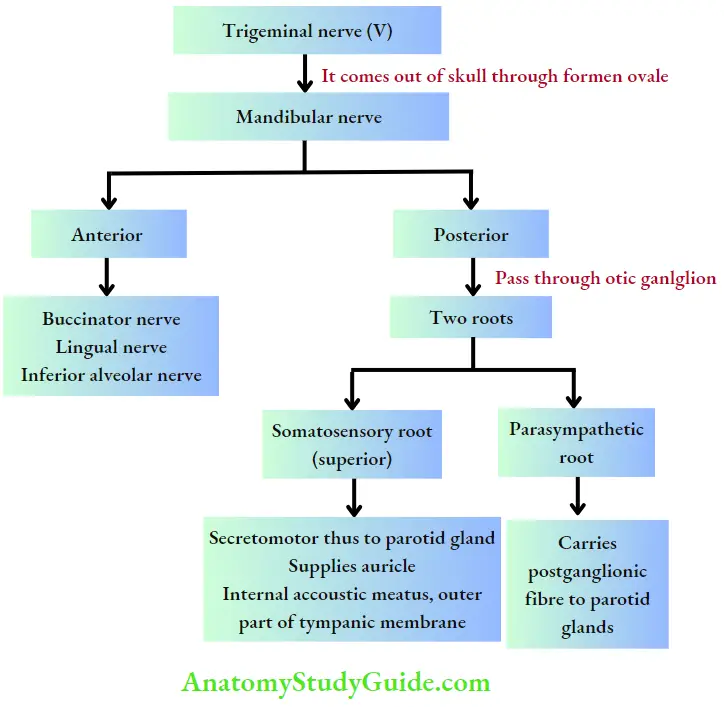
- The auriculotemporal nerve passes through the fork of the common carotid artery, passing between the neck of the mandible and the sphenomandibular ligament.
- Here it supplies the parotid gland and ascends and supplies the auricle. Lastly, it crosses the root of the zygomatic process of temporal bone.
- Frey’s syndrome occurs after surgery for parotid tumours, surgery in the region of temporomandibular joint or due to injury to the parotid gland.
- Injury to the auriculotemporal nerve can occur at a site where it turns around the neck of the mandible. The injury manifests at a later date, e.g. 2–3 months.
- Because of the injury, postganglionic parasympathetic fibres from otic ganglion unite with sympathetic fibres of superior cervical ganglion which supplies the vessels and sweat glands over the skin overlying parotid region.
Parts Supplied by Auriculotemporal Nerve:
1. Auricular part:
- External acoustic meatus
- Tympanic membrane surface
- Skin of auricle above external acoustic meatus
2. Temporal part: Hairy skin of the temple
As a result of this, whenever the act of chewing or mastication is started, there is increased sweating and hyperaesthesia in the region supplied by auriculotemporal nerve (cutaneous branch of mandibular division of trigeminal nerve). Hence, it is called auriculotemporal syndrome.
Diagnosis: Starch iodine test—paint the affected area with iodine and allowed it to dry before applying the dry starch.
The starch turns blue on exposure to iodine in the presence of sweat.

Frey’s Syndrome – Gustatory Sweating Prevention:
Principle is to provide a barrier between the skin and parotid bed by using temporalis fascial flap or sternomastoid muscle flap.
Frey’s Syndrome – Gustatory Sweating Treatment:
- Reassurance, aluminium chloride—antiperspirant which is a useful astringent
- Denervation by tympanic neurectomy
- Latest treatment includes injection of botulinum toxin into the affected skin.
Rare Causes Of Salivary Gland Enlargement
1. Sjogren’s Syndrome:
It is the diffuse infiltration of salivary and lacrimal glands with lymphocytes resulting in enlargement of glands and slow destruction of acini. Thus, clinical features include dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia). These along with a third component rheumatoid arthritis, form the triad of Sjögren’s syndrome (primary).
- 30% of patients with systemic lupus erythematosus and all patients with primary biliary cirrhosis develop Sjögren’s syndrome. This is termed secondary Sjögren’s syndrome.
- Other features: This disease is 10 times more common in females and presents with painful enlargement of the glands.
- Complications:
- Lymphomatous transformation (high in primary).
- Oral candidiasis.
2. Mikulicz Disease:
- Due to autoimmune mechanism, symmetrical enlargement of all salivary glands and lacrimal gland enlargement occur.
- Dry mouth and narrow palpebral fissures are diagnostic of this condition.
3. Drugs:
Carbimazole and thiouracil can cause enlargement of salivary glands.
4. Metabolic Disorders:
Diabetes and acromegaly are the other causes.
5. Granulomatous Sialoadenitis:
These are rare, painless swellings. Following are the causes:
- Tuberculosis
- Sarcoidosis—commonly affects parotid gland wherein it is called pseudotumour
- Toxoplasmosis
- Cat-scratch disease
- Wegener’s granulomatosis
Parotid Fistula
It is an uncommon condition which commonly occurs after surgery on the parotid gland.
Parotid Fistula:
- Any surgery on the parotid gland—superficial parotidectomy, drainage of abscess, surgery for carcinoma
- cheek, facio-maxillary trauma are the causes.
- Discharging watery fluid, exaggerated by keeping lime in the mouth.
- Fistulogram confirms the diagnosis.
- Exploration and excision of fistula and ligation of duct is required.
Minor Salivary Gland Tumour
- Even though they are called minor, numberwise they are major (many), about 450 in number.
- They are mucus secreting.
- They can present as mucus retention cyst (common in lip) or as malignant tumour.
- 90% of minor salivary gland tumours are malignant.
- Since they are submucosal, they start as a submucous nodule (very important point in the history) to differentiate from carcinoma buccal mucosa/lip, etc.
- As they grow, they ulcerate. Ulceration is a feature of malignancy.
- Slowly lymph nodes get enlarged.
- Treatment of benign cyst/tumour is by simple excision and malignant tumour is by wide excision.
Surgery For Facial Nerve Palsy
Indications For Different Types Of Surgery
1. Early immediate nerve repair, in case of injury to the nerve.
2. Late nerve crossing by suturing peripheral branches of facial nerve to one of the following nerves:
- Hypoglossal nerve, spinal accessory nerve
- Phrenic nerve.

3. Surgery to achieve movement in longstanding facial palsy (usually after 1 year).
1. Static Procedures:
- Suspension of lips, cheek and angle of mouth to zygomatic bone or temporal fascia using fascia lata, palmaris longus tendon or other alloplastic materials.
- Medial canthoplasty to reduce epiphora.
- Lateral tarsorrhaphy (canthoplasty) to prevent exposure keratitis due to widened palpebral fissure.
2. Dynamic Procedures:
- Muscle transfer with carefully preserved muscle nerve and vessel, e.g. temporalis muscle transfer, masseter muscle transfer.
- Cross face nerve transplantation using sural nerve. Using microscope, sural nerve is sutured to the two or three relatively insignificant branches of facial nerve (selected by intraoperative electric stimulation) on normal side.
- Other end of the sural nerve is sutured to distal end of the divided facial nerve on paralysed side.
- Free neurovascular gracilis muscle graft using microvascular techniques.
Peripheral Nerve Repair And Transfers
Principles Of Nerve Repair
- Preoperative assessment of motor and sensory system.
- Microsurgical tools should be available.
- Tension-free repair should be done. If tension-free repair is not possible, then nerve graft can be used.
- Primary repair when conditions permit.
- Delayed repair should be done in case of extensive injury.
Microsurgical Techniques:
- 4X magnification needed.
- 9–0/10–0 nylon is used for repair.
- Ends prepared with microscissors. First suture to be loose to ease the alignment of other sutures.
- Avoid postural manoeuvre to avoid tension. Nerve can be mobilised 1–2 cm proximally and distally for tension-free suturing but not more than that.
Peripheral Nerve Repair And Transfers Conduits:
- To place a polyglycolic acid tube to bridge the gap rather than to perform nerve grafting.
- Indications
- Donor nerve harvest not possible due to availability and associated morbidity
- Patients who decline autogenous nerve graft harvest
- Nerve gap of not more than 3 cm.
Principle of conduits:
Nerve regeneration and proximal and distal axonal matching result from a combination of neurotropism and contact guidance.
Peripheral Nerve Repair And Transfers Types:
1. Nerve Grafting:
Indications:
- If a tension-free repair is not possible
- If the nerve gap is more than 3 cm
- Can be used in place of conduits
Principle:
- The graft should be oriented in a reverse fashion from its native position so that the regenerating fibres are not diverted from the distal neurorrhaphy site and distal stump. Misalignment should be avoided.
- If the nerve gap is small, fascicular matching can be done
- If the nerve gap is long, techniques of awake stimulation or histochemical staining may be used.
- Donor sources for nerve grafting: Posterior interosseous nerve, medial antebrachial cutaneous nerve for small digital nerves, sural nerve for nerve gaps involving larger nerves, greater auricular nerve.
2. Nerve Transfer:
- It is used for reconstruction of proximal nerve injuries.
- Drawbacks of nerve graft that become the merits of nerve transfer:
- Grafting across a proximal nerve injury has poor functional outcomes.
- Timely re-innervation may not be possible if the target muscle is too far from the regenerating site.
- A nerve transfer converts a high level nerve injury to a low level nerve injury by recruiting expendable nerve fascicles from the donor nerve to innervate critical nerves close to their target end organs.
- Donor nerves are preferentially selected according to their proximity to the target site.
- Criteria for nerve transfers
- An expendable donor nerve
- Donor nerve with a large number of pure axons
- Donor nerve near the target organ
- Donor motor nerve that innervates a muscle that is synergistic to the target muscle
- Nerve transfers are done for both motor and sensory nerves.
Intersting most common:
Most Common for Salivary Gland Tumours:
- Most common benign parotid tumour in adults—pleomorphic adenoma.
- Most common benign parotid tumour in children— haemangioma.
- Most common type of cancer arising in the parotid glands is mucoepidermoid cancer.
- Most common malignant tumour in submandibular gland—adenoid cystic carcinoma.
- Most common minor salivary gland tumour is adenocarcinoma.
- Most common site of squamous cell carcinoma is sub-mandibular salivary gland.
- Most common response to radiotherapy among malignant tumours is adenoid cystic carcinoma.
Leave a Reply