Clinical Diagnosis Of Periodontal Disease
- Diagnosis of periodontal disease is not a mere identification of its presence but also of its extent and severity so that it provides a clue to its management.
- Recording The History: A detailed history may lead to an indication to the presence of modifiable and non-modifiable risk factors that could have contributed to periodontal disease.
Question 1. Describe the clinical examination of periodontium.
Answer:
Extra-oral Examination: It involves an examination of the temporomandibular joint for pain, clicking and deviation, facial asymmetry due to swellings, lymph node, and parafunctional habits such as clenching, bruxism, etc.
Read And Learn More: Periodontology Important Question And Answers
Intra-oral Examination:
- Hard Tissue Examination
- All tooth-related factors that may contribute to plaque accumulation such as dental caries, and open contacts are to be examined as are any potential iatrogenic factors such as restorations.
- Occlusal relationships of the maxillary and mandibular teeth at rest and function must be determined.
- Evidence of occlusal trauma is indicated by occlusal wear facets in the posterior teeth and by fremitus in the anterior teeth.
- Fremitus is felt through the index finger placed lightly on the buccal surfaces of the teeth while the patient makes incursive mandibular movements and closes repeatedly in the center occlusion.
- Fremitus is a functionally induced form of mobility that is reflective of past and present disease and/or adaptive changes.
Fremitus may be classified (Ingervall classification) as:
- Class 1: Fremitus—mild vibrations detected.
- Class 2: Fremitus—easily palpable vibration but no visible movements.
- Class 3: Movements visible to the naked eye.
- Correction of occlusion must be incorporated into the treatment plan if necessary and occlusal rehabilitation instituted.
- Soft Tissue Examination
- After an initial examination of the buccal mucosa, the tongue, palate, and floor of the mouth for any obvious pathologies, the periodontium is then thoroughly examined.
- The accumulation of plaque and calculus is assessed either visually or by using a calibrated probe.
- Gingival Examination:
- All the clinical features that have been outlined in the previous chapter as indicative of chronic gingivitis are assessed.
- However, the most objective sign of gingivitis is bleeding on probing. Probing the sulcus for bleeding is done using a probe with a blunt tip, without undue use of force.
- The area probed should be rechecked for bleeding after 30–60 seconds to check for delayed bleeding.
- Periodontal Examination:
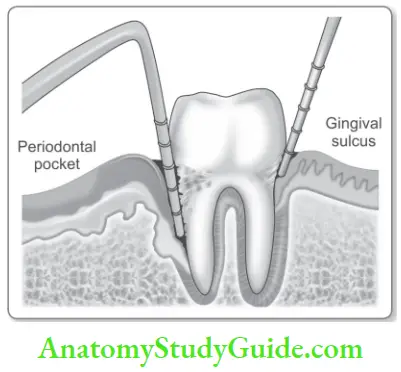
- Probing depth and clinical attachment level. Probing depth and clinical attachment levels are assessed simultaneously.
- Increased probing depth with normal clinical attachment level is indicative of gingivitis.
- An increase in both probing depth and clinical attachment level is the hallmark of periodontal disease.
- Normal probing depth and an increase in clinical attachment level is indicative of a gingival recession.
- Probing is done at the initial appointment before scaling or soon after scaling to determine whether the tooth can be saved or needs to be extracted.
- Probing is done again after phase 1 therapy and checked for a reduction in probing depth. Following periodontal treatment probing is done to determine changes in pocket depth and to determine the healing progress.
- It is done after 3–4 weeks after therapy.
- Subgingival Temperature:
- Subgingival temperature is increased in gingival inflammation and thus it has been proposed as a diagnostic aid.
- A commercially available device PERIOTEMP – is available which resembles a periodontal probe and is used to measure subgingival temperature to a precision of 0.1°C.
- Gingival Examination:
Question 2. Write a note on tooth mobility.
Answer:
- Tooth mobility should be recorded because mobile teeth show increased attachment loss and a poorer prognosis after surgery.
- Mobility is caused by loss of supporting tissues, trauma from occlusion, an extension of gingival inflammation into the periodontal ligament, following periodontal surgery, and pathologic processes of the jaw.
- It is recorded by moving the tooth in a buccolingual and an occlusoapical direction with a metal instrument and one finger or two instruments.
- Mobility beyond the physiologic limit is considered Grade 1. Mobility is more than grade 1 but where the tooth cannot be depressed apically is Grade 2 and Grade 3 is where the tooth can be depressed pico-occlusal as well.
Miller classified mobility as:
- Degree 1: Mobility of crown of the tooth 0.2–1 mm in horizontal direction.
- Degree 2: Mobility exceeding 1 mm in horizontal direction.
- Degree 3: Mobility in vertical direction as well.
- The causes of tooth mobility are many like periodontal disease, trauma from occlusion, periodontal surgery cysts, and tumor of the jaw, and during pregnancy and menstruation, there is transiently increased tooth mobility.
- Electronic devices such as the periotest are available to record the mobility of a tooth. Single-rooted teeth exhibit mobility faster and more often than not due to lesser root surface area as compared to multirooted teeth.
Transgingival Probing
- This is also called the sounding of bone. This is a clinical procedure or diagnostic technique which is performed under local anesthesia.
- The periodontal probe is forced through the supra-alveolar connective tissue to make contact with bone.
- This helps understand the underlying osseous topography. The distance from the tip of the bone to the cementoenamel junction is measured in millimeters.
- Interdental craters can be detected by placing the probe obliquely from the facial and lingual surfaces.
Question 3. Describe the conventional and advanced radiographic techniques of diagnosing periodontal disease.
Answer:
Radiographic Investigation
- Radiographs have been the cornerstone of diagnosis of periodontal disease and have proved to be of invaluable aid clinically.
- The intraoral periapical radiograph (IOPA) is the standard radiograph that is usually available in most dental operatories.
- The IOPA will show two/three posterior teeth or five/six anterior teeth in one film. The quality and depth of the picture in an IOPA is the best available.
- The orthopantomogram (OPG) provides a comprehensive picture of the entire dentition and supporting structures in one single film. The detail and size however do not remain consistent.
Radiological Features of Periodontal Defects: A variety of periodontal defects may or may not be visualized on a radiograph. The relevant features to check for with regard to periodontal disease are:
- The crestal bone, the integrity of Lamina Dura
- The trabecular pattern and type of bone loss
- The crown/root ratio
- Endodontic involvement in a periodontal lesion.
Advanced Radiographic Analysis
- Xeroradiography: This consists of an X-ray imaging system that uses a xerographic copying process to record X-ray images. Compared to the IOPA, it gives better images of fie structures like bony trabeculae and also gives a reduced radiation exposure.
- Iodine 125 absorptiometry: This is actually a non-radiographic method but is the most sensitive for analyzing periodontal bone mass change. It is based on the absorption of a low-energy beam by the bone.
- Photodensitometric analysis technique: It is based on the absorption of a beam of light by radiographic film which also shows an image of an aluminum scale and transformation of the density readings into millimeters of mercury.
- Computer-assisted densitometric image analysis system (CADIA): A video camera measures light transmitted through a radiograph and signals from the camera are converted into gray levels.
- Nuclear medicine techniques: The radionucleotide is given intravenously and allowed for clearance. Then a semiconductor probe detector is placed on the buccal aspect of tooth. This can be performed in a single visit. This is done using a bone-seeking pharmaceutical diphosphonate compound which is Tc 99m diphosphonate.
- Digital radiography:
- It eliminates the need for film processing and allows immediate image acquisition and the ability to electronically store and print images.
- It allows for detection of as little as 0.54 mm of change at specific sites and an average of 0.1 mm full mouth changes from one visit to another.
Magnetic resonance imaging:
- MRI is found on the principles of nuclear magnetic resonance. In the presence of an external magnetic field, the spinning atomic nuclei tend to line up in the direction of the field.
- After excitation by an external resonance frequency (RF) radiation pulse, RF radiation is emitted by the lined-up vibrating nuclei.
- It is possible to construct an MRI image based on this emitted radiation. In biological tissues, hydrogen nuclei protons are the only nuclei present in concentrations high enough to allow the mathematical reconstruction of images with a reasonable degree of spatial resolution.
- The protons in water molecules in soft tissue are the primary contributors to the detected MRI signal.
- In contrast to conventional radiographs that detect osseous structures with a high degree of contrast, with MRI bone and teeth are observed as black areas of minimal contrast.
- By varying the parameters used to create the image, differences in contrast can readily be observed between various soft tissues and between tumor or edematous tissue.
- MRI offers great promise for the investigation of salivary activity and for imaging the TMJ meniscus, but unless its resolution is further enhanced, its use for the detection of periodontal destruction is limited.
Computer tomography (CT):
- Tomography is a process by which an image of a layer within the body is produced while the images of structures above and below that layer are made invisible by blurring.
- The blurring of images of structures outside the plane of interest is achieved by the simultaneous movement of the X-ray tube and film during the exposure.
- The computer tomography system consists of an X-ray source that scans the patient, a radiation detector, a digital computer, and a device for converting the computed image into a visible 3-dimensional format.
- In recent years, a new cone beam CT has been introduced for maxillo-facial use which is less expensive and produces less radiation.
- It uses a cone-shaped X-ray beam which is detected by a 2-D flat panel detector. CT is used for diagnosis and treatment planning.
Subtraction radiography:
- This radiographic method uses a series of radiographs. The computer subtracts structures present in the previous radiograph from those in the present, leaving only bone loss and bone gain.
- Local bone changes can be seen by superimposing the subtracted image over the original radiograph.
- Radiographic examination is useful in the diagnosis and treatment planning of periodontal diseases in spite of its limitations.
- Used along with clinical periodontal examination they complement each other. Radiographs provide us with information about the type, extent, and distribution of bone loss.
- Following treatment bone gain may also be assessed.
Microbiological tests:
- Microbiological testing and antibiotic sensitivity tests are not indicated in the majority of periodontal patients except in cases of juvenile, refractory, and rapidly progressing forms of periodontitis.
- There are a variety of methods of assessing the bacterial flares of patients with periodontal disease.
- Plaque samples are collected using a curette or paper point and analyzed using phase contrast or dark field microscope, bacterial enzyme analysis, immunoassays, DNA probes, polymerase chain reaction, or traditional microbiological culturing and sensitivity.
Conclusion
- Advanced diagnostic aids have been outlined in a later chapter.
- In the absence of a single cost-effective, reliable marker, diagnosis of periodontal disease is largely based on clinical examination.
- The importance of clinical diagnosis cannot be over-emphasized as it is the basis for treatment planning.
Leave a Reply