Degeneration And Regeneration Of Nerve Fibers Introduction
When a nerve fiber is injured, various changes occur in the nerve fiber and nerve cell body. All these changes are together called degenerative changes. The injury occurs due to the obstruction of blood flow, local injection of toxic substances, crushing of nerve fiber, or the transection of the fiber.
Table of Contents
Degrees Of Nerve Fibers Injury
Sunderland had classified the injury to nerve fibers into five categories depending upon the order of severity.
Read And Learn More: Medical Physiology Notes
First Degree Of Nerve Fibers Injury
- First-degree injury is the most common type of injury to the nerves. It is caused by applying pressure over a nerve for a short period leading to occlusion of blood flow and hypoxia.
- By the first degree of injury, the axon is not destroyed but mild demyelination occurs. It is not a true degeneration. The axon looses its function temporarily for a short time, which is called a conduction block. The function returns within few hours to few weeks. First degree of injury is called Seddon’s neuropraxia.
Second Degree Of Nerve Fibers Injury: It is due to the prolonged severe pressure which causes Wallerian degeneration (see below). However, the endoneurium is intact. Repair and restoration of function take about 18 months. The second degree of injury is called axonotmesis.
Third Degree Of Nerve Fibers Injury: In this case, the endoneurium is interrupted. Epineurium and perineurium are intact. After degeneration, the recovery is slow, and poor or incomplete. The third, fourth, and fifth degrees of injury are called neurotmesis.
Fourth Degree Of Nerve Fibers Injury: This type of injury is more severe. The epineurium and perineurium are also interrupted. The fasciculi of nerve fibers are disturbed and disorganized. Regeneration is poor or incomplete.
Fifth Degree Of Nerve Fibers Injury: Fifth degree of injury involves complete transaction of the nerve trunk with loss of continuity. Useful regeneration is not possible unless the cut ends are rearranged and approximated quickly by surgery.
Degenerative Changes In The Neuron
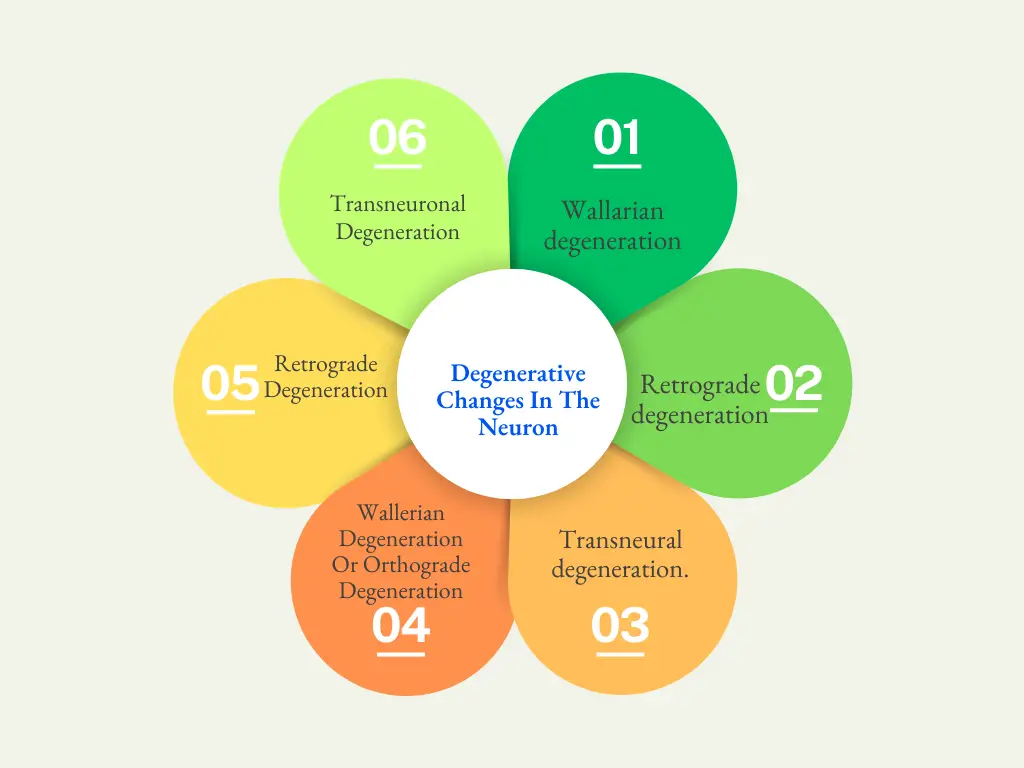
Degeneration refers to deterioration or impairment or pathological changes of an injured tissue. When a peripheral nerve fiber is injured, degenerative changes occur in the nerve cell body and the nerve fiber same neuron, and the adjoining neuron. Accordingly, the degenerative changes are classified into three types:
- Wallarian Nerve Fibers degeneration
- Retrograde Nerve Fibers degeneration
- Transneural Nerve Fibers degeneration.
- Wallerian Nerve Fibers Degeneration Or Orthograde Nerve Fibers Degeneration: Wallerian degeneration is the pathological change that occurs in the distal cut end of the nerve fiber (axon). It is named after the discoverer Waller. It is also called orthograde degeneration. Wallerian degeneration starts within 24 hours of injury. The change occurs throughout the length of the distal part of nerve fiber simultaneously.
- The Axis cylinder swells and breaks up into small pieces, After few days, the broken pieces appear as debris in the space occupied by the axis cylinder.
- The myelin sheath is slowly disintegrated into fat droplets. The changes in myelin sheath occur from 8th to 35th day.
- The neurilemmal sheath is unaffected, but the Schwann cells multiply rapidly. The macrophages invade from the outside. The macrophages remove the debris of axis cylinder and the fat droplets of the disintegrated myelin sheath. So, the neurilemmal tube becomes empty. Later it is filled by the cytoplasm of the Schwann cell. All these changes take place for about 2 months from the day of injury.
- Retrograde Nerve Fibers Degeneration: Retrograde degeneration is the pathological changes that occur in the nerve cell body and axon proximal to the cut end.
- Changes in the Nerve Cell Body: The changes in the nerve cell body commence within 48 hours after the section of nerve. The changes are:
- First, the Nissl granules disintegrate into fragments by chromatolysis
- The Golgi apparatus is disintegrated
- The cell body swells due to the accumulation of fluid and becomes round
- The neurofibrils disappear followed by displacement of the nucleus towards the periphery
- Sometimes, the nucleus is extruded out of the cell. In this case, death of the neuron occurs and regeneration of the injured nerve is not possible.
- Changes in the Axon Proximal to Cut End: In the axon, the changes occur only up to the first node of Ranvier from the site of injury. The degenerative changes that occur in proximal cut end of axon are similar to those changes occurring in distal cut end of the nerve fiber.
- Changes in the Nerve Cell Body: The changes in the nerve cell body commence within 48 hours after the section of nerve. The changes are:
- Transneuronal Nerve Fibers Degeneration: If an afferent nerve fiber is cut, degenerative changes occur in the neuron with which the afferent nerve fiber synapses. It is called transneuronal degeneration.
- Transneuronal Nerve Fibers Degeneration Examples:
- Chromatolysis in the cells of the lateral geniculate body occurs due to the sectioning of optic nerve
- Degeneration of cells in dorsal horn of the spinal cord occurs when the posterior nerve root is cut
- Degeneration of cells in ventral horn of spinal cord occurs when there is tumor in the cerebral cortex.
- Transneuronal Nerve Fibers Degeneration Examples:

Regeneration Of Nerve Fiber
The term regeneration refers to the regrowth of lost or destroyed part of a tissue. The injured and degenerated nerve fiber can regenerate. It starts as early as 4th day after injury, but, becomes more effective only after 30 days and is completed in about 80 days.
Criteria For Nerve Fibers Regeneration: Regeneration is possible only if certain criteria are fulfilled by the degenerated nerve fiber:
- The gap between the cut ends of the nerve should not exceed 3 mm
- The neurilemma should be present. As neurilemma is absent in CNS, the regeneration of nerve does not occur in CNS
- The nucleus must be intact. If it is extruded from nerve cell body, the nerve is atrophied and. regeneration does not occur
- The two cut ends should remain in the same line. Regeneration does not occur if any one end is moved away.
Stages Of Nerve Fibers Regeneration
- First, some pseudopodia-like extensions grow from the proximal cut end of the nerve. These extensions are called fibrils or regenerative sprouts. The number of fibrils is up to 100
- The fibrils move toward the distal cut end of the nerve fiber
- Some of the fibrils enter the neurilemmal tube of distal end and form axis cylinder
- Schwann cells line up in the neurilemmal tube and actually guide the fibrils into the tube. Schwann cells also synthesize nerve growth factors which attract the fibrils form proximal segment
- The axis cylinder is fully established inside the neurilemmal tube. These processes are completed in about 3 months after the injury
- The myelin sheath is formed by Schwann cells slowly. The myelination is completed in one year
- The diameter of the nerve fiber gradually increases. However, the degenerated nerve fiber obtains only 80% of its original diameter. The newly formed internodes are also shorter than the original ones
- In the nerve cell body, first, the Nissl granules appear followed by the Golgi apparatus
- The net loses the excess fluid. The nucleus occupies ins central portion
- Though anatomical regeneration occurs in the nerve, functional recovery occurs after a long period.
Leave a Reply