Dentin – Meaning, Development, Structure, Types
Dentin
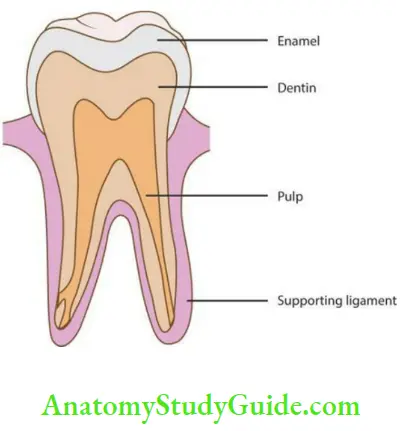
Dentin is the mineralized connective tissue that provides the bulk and form to the tooth. It is covered by enamel in the crown and by cementum in the root
Table of Contents
Salient Features Of Dentin
- Dentin is laid down by odontoblasts. The cell bodies of the odontoblasts are present outside the dentin along the outer border of the pulp lining the pulpal surface of dentin.
- Dentin consists of numerous tubules, which are laid down in a mineralized collagenous matrix. The tubules contain the processes of odontoblasts and thus dentin is considered a living tissue.
- Dentin forms before enamel. It determines the shape of the crown and number and size of the roots.
- It is formed throughout the life.
Read And Learn More: Oral Histology Notes
- Coronal dentin: Dentin present in the crown.
- Radicular dentin: Dentin present in the root.
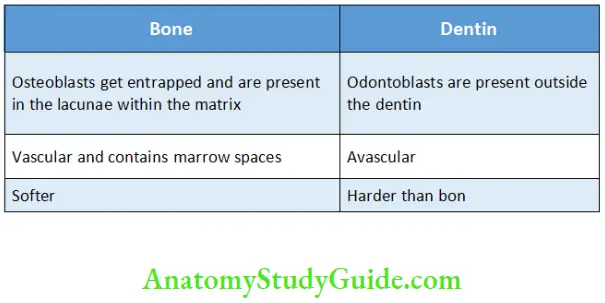
- Dentin is similar to bone and is considered to be vital. However, there are a few differences between the two
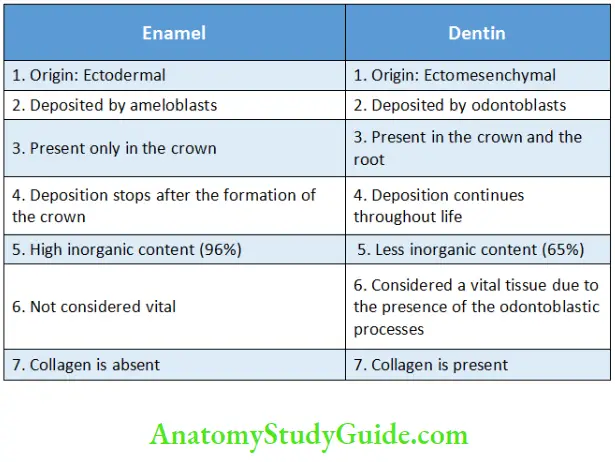
- Even though dentin and enamel are calcified tissues, there are certain differences between them which are described in table
Differences between Dentin and Bone
Differences between Enamel and Dentin
Physical Properties Of Dentin
Dentin Colour:
- Light yellow in colour. The yellow dentin is seen through the
translucent enamel. - Dentin Darkens with age.
Dentin Hardness:
- Dentin is viscoelastic in nature and subject to slight
deformation. The enamel overlying the dentin is brittle but does not fracture due to masticatory forces as dentin acts as a cushion and distributes the forces. - Dentin is harder in the centre than at the periphery.
- It is harder in permanent teeth than in primary teeth.
- Cracks might occur in dentin which is weakened due to caries or due to cavity preparation. The incidence of cracking increases with age.
Dentin Thickness:
- Usually ranges from 3 to 10 mm.
- It varies among teeth and also among surfaces.
- Thicker on the buccal aspect than the lingual aspect.
Dentin Permeability:
- Dentin is permeable, depending on the patency of the dentinal tubules.
- The permeability decreases with age.
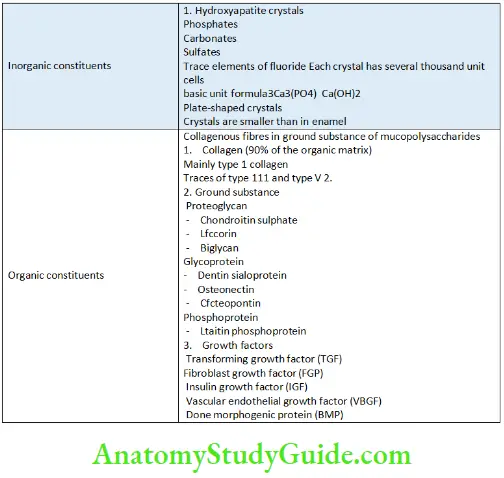
Chemical Properties Of Dentin
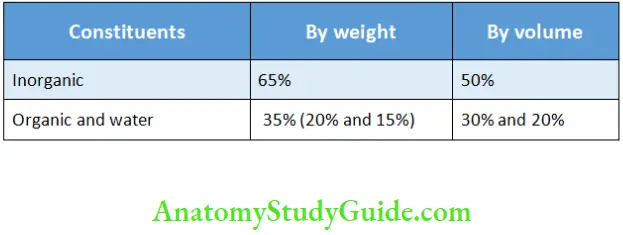
Organic and inorganic constituents of dentin
Chemical Constituents of Dentin
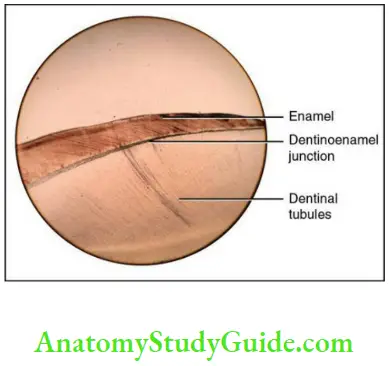
Dentinoenamel Junction
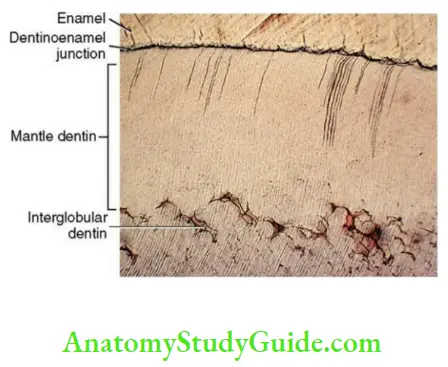
The junction between the enamel and dentin is known as the dentinoenamel junction (DEJ) (Fig. 3.2).
- It is scalloped with convexities facing the dentin. The scalloping is more often noticed in the areas of the tooth under great stress.
- The scalloping increases the surface area between enamel and dentin and helps in increased adhesion between the two tissues.
- The DEJ prevents the shearing of enamel and also the development of cracks along the interface between enamel and dentin.
Chemical Content of Dentin by Volume and Weight
Structure Of Dentin
The collagen fibres of dentin are masked by the hydroxyapatite crystals as dentin calcifies. The collagen fibres can be seen only at the ultrastructural level. The ratio between the outer and inner surface of dentin is 5:1. Dentin consists of dentinal tubules that extend along the entire thickness of dentin. The odontoblasts are
present along the pulp dentin border within the pulp with the odontoblastic processes present within the dentinal tubule in the calcified matrix. Each odontoblast gives rise to one odontoblastic process, which is a cytoplasmic extension, and is present within each dentinal tubule. The tubules end at the cementodentinal junction (CDJ) or the DEJ.
Dentinal tubules
- Dentinal tubules run from the pulp dentin border to the DEJ or the CDJ.
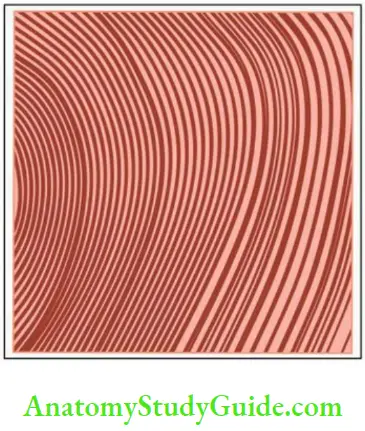
- The tubules are ‘S’ shaped and are at right angles to the pulp and the CDJ and DEJ. Starting from the pulp, the first curvature of the ‘S’ is towards the apex or the root of the tooth. The tubules are almost straight at the cusp tips, incisal edges and in the root. The tubules are circular in cross section.
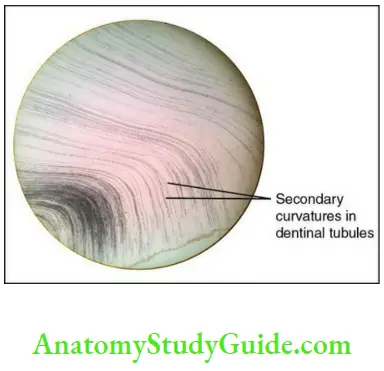
- Primary curvature: The dentinal tubules are gently curved and follow a sigmoid course and are ‘S’ shaped. This curvature is called primary curvature.
- Secondary curvature: During the formation of dentin, the odontoblasts move away from dentin in a spiral manner, which results in minute oscillations/sinusoidal curvatures along the dentinal tubules. These are called secondary curvatures
- Lamina limitans: The wall of the dentinal tubule is lined by an organic lining rich in glycosaminoglycans. This lining is termed as lamina limitans. It is similar to the lining of bone and cartilage.
- Periodontoblastic space: The space between the odontoblastic process and peritubular dentin is called periodontoblastic space.
- Dentinal fluid: The fluid present in the periodontoblastic space is called dentinal fluid. It has high content of K+ ions and low content of Na+ ions.
Dentinal Hypersensitivity Clinical significance
- Dentinal hypersensitivity can be explained on the basis of the movement of this fluid.
- Fracture of a tooth involving dentin causes this fluid to exude from the dentinal surface as droplets, mostly due to outward pulpal pressure. This could help in limiting the diffusion of chemicals and toxins from the dentin into the pulp.
- Terminal branches:
- They are also called Y-shaped dentinal tubules.
- More common in radicular dentin than in the coronal dentin.
- They might terminate blindly or may unite with branches of other
tubules.
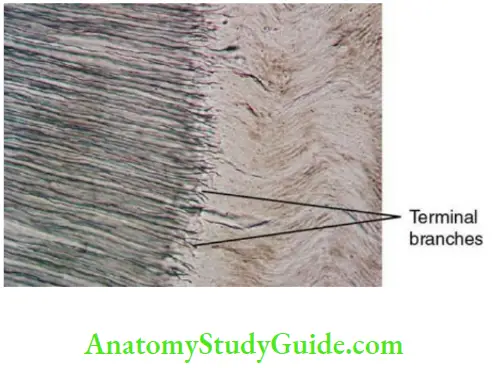
Sensitivity of Dentin Clinical significance
Terminal branches increase the sensitivity of dentin.
- Lateral branches:
- Also called canaliculi or microtubules.
- These are at right angles to the dentinal tubule.
- Diameter: 1 micron.
- These communicate with the adjacent dentinal tubule or end
in intertubular dentin and may contain odontoblastic processes.
Salient features of the dentinal tubules:
- Tubules are farther apart in the periphery than near the pulp.
- Larger in diameter near the pulp (3–4 microns) than at the periphery (1 micron).
- Ratio between the number of tubules per unit area on the outer surface to the inner surface near the pulp is 1:4 (varies between 90,000 and 50,000 per square millimetre).
- More tubules are present in the crown than in the root.
Odontoblast, Odontoblastic Process And Enamel Spindles
- The life span of the odontoblasts is equal to that of the tooth.
- The odontoblasts are 40 microns in length and 7 microns in diameter.
- The odontoblastic processes are cytoplasmic extensions of the odontoblasts. They are largest in diameter near the pulp (4 microns) and smallest (1 micron) at the periphery. They are composed of microtubules and intermediate filaments and may contain mitochondria, micro vesicles and coated vesicles.
- The processes might extend
- Till the outer surface of the tubule.
- Partly along the length of the tubule or degenerate and its remains might become a part of the matrix.
- Enamel spindles: Sometimes the odontoblastic processes cross the DEJ and extend into the enamel. These are called enamel spindles.
Classification Of Dentin
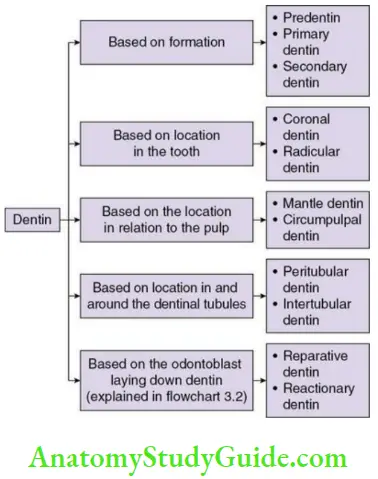
Peritubular dentin and intertubular dentin
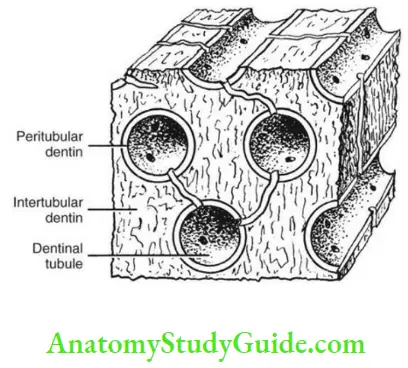
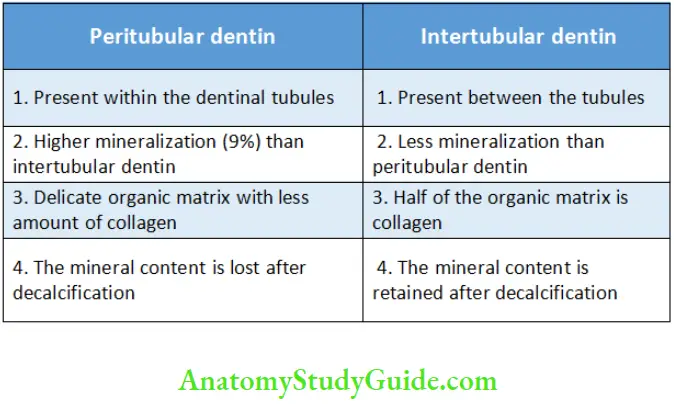
The dentin that surrounds the dentinal tubules is called peritubular dentin. It forms the walls of the tubules in the entire dentin. It is absent in the dentin near the pulp. It is more calcified than the intertubular and also differs in matrix composition.
Peritubular dentin is two times thicker in the outer dentin than in the inner dentin. There is an increased mineral density in the peritubular dentin. Due to the deposition of minerals in the inner wall of the dentinal tubule, intratubular dentin is a more suitable term for this type of dentin.
Intertubular dentin is the dentin present in between the tubules or between the zones of peritubular dentin and forms the main bulk of dentin. It is retained after decalcification just like bone and cementum is, but peritubular dentin is not. The collagen fibres are randomly organized around the dentinal tubules. The hydroxyapatite crystals are arranged parallel to the collagen fibres. The differences between peritubular and intertubular dentin are mentioned in Table.
Differences between Peritubular Dentin and Intertubular Dentin
Predentin
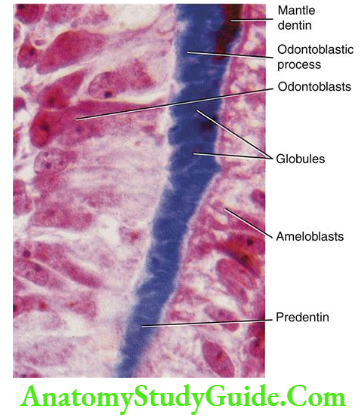
- Predentin a layer of unmineralized dentin located adjacent to the pulp.
- The width of this layer varies from 10 to 40 microns depending on the rate at which it is deposited by the odontoblasts.
- In a demineralized section stained with haematoxylin and eosin, the predentin appears pale. It is due to the difference in the composition of its unmineralized matrix and the mineralized matrix of the circumpulpal dentin.
- A new layer of predentin is laid down circumpulpally as the matrix at the predentin–dentin border is mineralized.
Primary Dentin
The dentin formed before root completion is called primary dentin. There are two types of primary dentin.
- Mantle dentin
- Circumpulpal dentin
Mantle dentin:
The first formed and the outermost layer of primary dentin, which is found below the DEJ is called mantle dentin. It is soft and acts as a cushion for the tooth.
Thickness: 20 microns
Mantle Dentin Organic matrix:
- Large collagen fibres (larger than in circumpulpal dentin) are loosely packed and perpendicular to the DEJ.
- von Korff’s fibres: Large-diameter type III collagen fibrils of 0.1–0.2 microns diameter which are argyrophilic (silver stained) are present in mantle dentin.
- The organic matrix is less mineralized than circumpulpal dentin
Mantle Dentin Mineralization:
Mineralization of mantle dentin is by the matrix vesicles and happens in a globular or linear pattern. The defects are lesser than in circumpulpal dentin. The mineralization front appears uniform if the rate is slow and the pattern of mineralization is said to be linear.
Circumpulpal dentin:
Circumpulpal dentin forms the rest of the bulk of primary dentin.
Organic matrix:
- The collagen fibres are smaller in diameter (0.05 micron) and closely packed.
- It is more mineralized than mantle dentin.
Secondary Dentin
The dentin formed after root completion is called secondary dentin. There is a change in direction of dentinal tubules at the interface with primary dentin. It differs from primary dentin as
- It is formed throughout life.
- It is formed slowly.
- It contains lesser dentinal tubules.
- Tubular pattern is less regular.
- It is not formed uniformly. Greater quantity is formed on the roof and floor of the pulp chamber, which protects the pulp from the exposure in older teeth.
- Incremental lines are closer.
- In older individuals, the pulp chamber becomes smaller and the root canals narrow due to continuous deposition of secondary dentin.
Regular secondary dentin: The secondary dentin has regular arrangement of dentinal tubules.
Tertiary Dentin
When dentin is formed due to caries, trauma or damage to the pulp during cavity preparation, it is termed as tertiary dentin. The formation of tertiary dentin is described in Flowchart
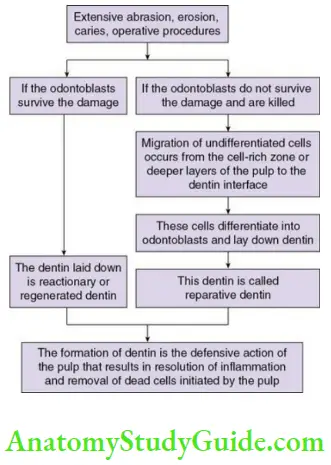
Reparative dentin has lesser and more twisted tubules.
Osteodentin: The dentin wherein the odontoblasts might be trapped within the intercellular substance is called osteodentin.
Irregular secondary dentin: The dentin which contains both osteodentin and tubular dentin is called irregular secondary dentin. It has irregular dentinal tubules.
Incremental Lines Of Von Ebner
The incremental lines in dentin are fine striations perpendicular to the dentinal tubules and are called incremental lines ofvon Ebner. The lines are 4–8 microns apart.
- They are indicative of the daily rhythmic deposition of dentin.
The deposition of dentin decreases after the tooth reaches its functional position.
Contour Lines Of Owen
Accentuated incremental lines are called contour lines ofOwen
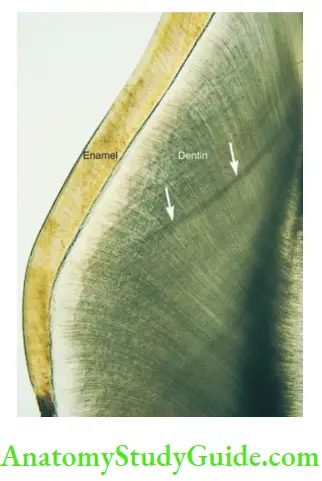
Concept Of The Contour Lines Of Owen:
1. Contour lines of Owen are formed due to the disturbance in the mineralization of the matrix. Longer the disturbance, wider are the lines. They may be considered hypocalcified structures.
2. They are also considered to be formed due to the coincidence of the secondary curvatures.
Neonatal Line
The accentuated incremental line that separates prenatal dentin and postnatal dentin is termed neonatal line. The line is formed due to abrupt change in environment at birth.
- Commonly seen in deciduous teeth and permanent first molar.
- Prenatal dentin is of better quality.
- The neonatal line is considered to be a zone of hypocalcification.
Interglobular Dentin
During the mineralization of dentin, the minerals are deposited in globules or calcospherites, which later fuse to form a uniformly homogenous calcified mass. Sometimes when these globules fail to fuse, the zones of hypomineralization between the globules are called interglobular spaces or interglobular dentin. The dentinal
tubules pass through interglobular dentin. This proves that the defect is in the mineralization rather than matrix formation.
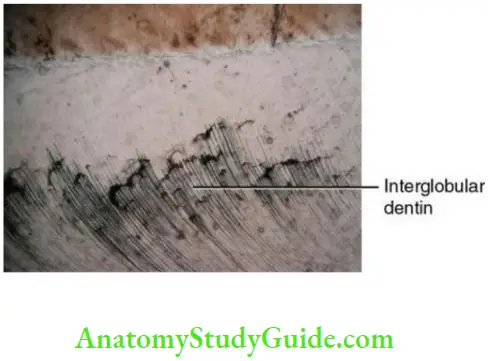
Interglobular Dentin Appearance:
- In transmitted light, the interglobular dentin appears dark due to internal reflection of light in ground sections.
Interglobular Dentin Location:
- Circumpulpal dentin.
- Seen in the cervical and middle third of the root and in the coronal one-third of the crown in decreasing order of occurrence.
Tomes Granular Layer
The peripheral zone of dentin in the root next to the cementum appears granular. This is called the Tomes’ granular layer. This area is unmineralized and rich in calcium and phosphorus.

Tomes Granular Layer Cause:
- It is due to the profuse branching and further coalescing and looping of the terminal portion of the dentinal tubules due to the turning of the odontoblasts on themselves. Recent studies suggest that the special arrangement of collagen and noncollagenous matrix at the CDJ is the cause for the granular layer.
Tomes Granular Layer Appearance:
- In transmitted light, the air spaces between the loops cause internal reflection leading to a granular appearance.
Dead Tracts
The empty dentinal tubules with the absence of the odontoblastic process are filled with air and appear black in transmitted light and white in reflected light. These are called dead tracts
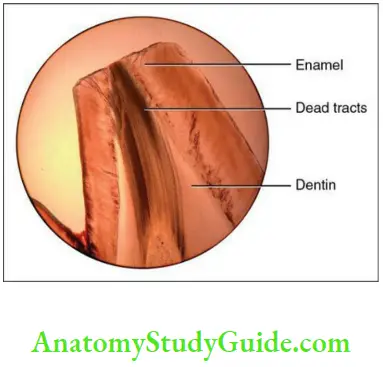
Dead Tracts Cause: The dentinal tubules in a vital tooth might be empty due to
- The loss of the odontoblast process due to caries, abrasion, attrition or cavity preparation or
- Retraction of the odontoblasts before the dentinal tubule is occluded by the peritubular dentin.
The tubules are then filled with air.
Dead Tracts Appearance:
- Dead tracts appear black in transmitted light and white in reflected light.
Dead Tracts Occurrence: Older individuals.
Clinical significance: Decreased sensitivity of dentin. Dead tracts may lead to sclerotic dentin in the future.
Sclerotic Dentin Or Transparent Dentin
The dentin especially in roots sometimes appears transparent and this is called transparent or sclerotic dentin.
Transparent Dentin Reason: As a defensive response to caries, abrasion, attrition, toxins and cavity preparation, the apatite crystals and collagen fibres appear within the dentinal tubules. The tubules are eventually occluded.
Transparent Dentin Appearance:
- Transparent in transmitted light as the refractive index of dentin in
which the tubules are blocked are equalized. They appear dark in reflected light.
Transparent Dentin Location: Mostly in roots.
Transparent Dentin Occurrence: Older individuals, slow progressing caries.
Physical and chemical properties:
- More mineralized and harder than normal dentin.
- Decrease in fracture toughness.
- Crystals are smaller than normal dentin.
Transparent Dentin Clinical significance:
- The formation of sclerotic dentin decreases the permeability of dentin and preserves the vitality of the pulp.
- It requires longer etching time due to the increased mineral density.
Nerves In Dentin
Nerve bundles enter the pulp from the apical foramen and terminate as free nerve endings in the subodontoblastic zone. Axons which lose their Schwann cell sheath enter the dentinal tubules and pass next to the odontoblastic process. It is suggested that there
is a communication between the odontoblastic process and the nerve endings by means of a synapse-like junction. The nerve endings may not be seen in all the dentinal tubules and may not extend throughout the thickness of dentin.
Dentin Hypersensitivity
This is also called dentin sensitivity or cervical sensitivity.
Definition of dentin hypersensitivity: Dentin hypersensitivity is ‘characterized by a short, sharp pain arising from exposed dentin in response to stimuli typically thermal, evaporative, tactile, osmotic, or chemical and that cannot be ascribed to any other form of dental defect or pathology’ (Holland).
Theories of dentin hypersensitivity:
There are three theories that explain the conduction of pain in dentin:
- Direct neural stimulation
- Transduction theory
- Fluid or hydrodynamic theory
Direct neural stimulation theory:
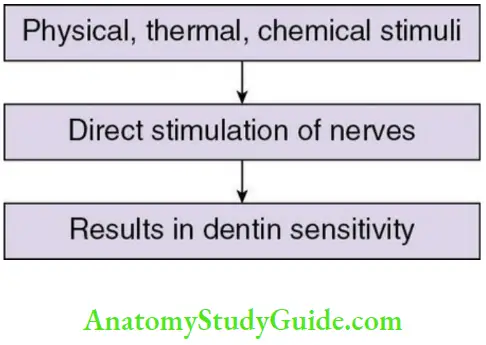
- Drawbacks of this theory Nerve fibres do not extend through the entire thickness of dentin.
- Application of a local anaesthetic agent topically does not reduce the sensitivity.
Transduction theory:
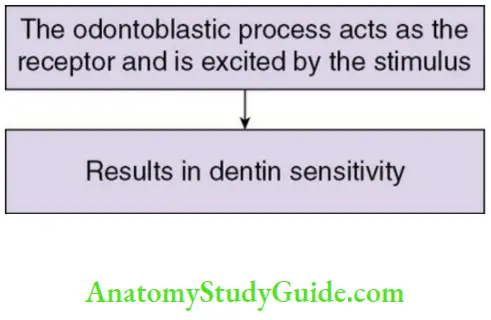
Points in favour of this theory:
1. Odontoblasts originate from neural crest cells and might retain transducing and propagating properties.
Transduction Theory Drawbacks:
1. The membrane potential is too low to conduct and transmit an impulse.
Fluid or hydrodynamic theory (most accepted theory)
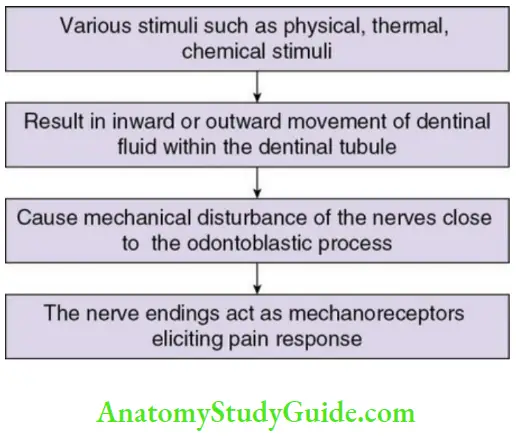
Points in favour of this theory
- It explains the inability of a local anaesthetic agent to reduce pain.
- It also explains the increased sensitivity of dentin near the DEJ. This could be due to extensive branching of dentinal tubules near the DEJ and displacement of a huge volume of dentinal fluid due to any stimuli.
Dentinogenesis
The process of formation of dentin is called dentinogenesis.
- Dentin is laid down by odontoblasts.
- It begins in the late bell stage.
- It begins at the cusp tips below the folds of the inner enamel epithelium (IEE).
- Dentin formation continues till the entire coronal dentin is formed (4 microns).
Dentinogenesis can be explained under the following steps
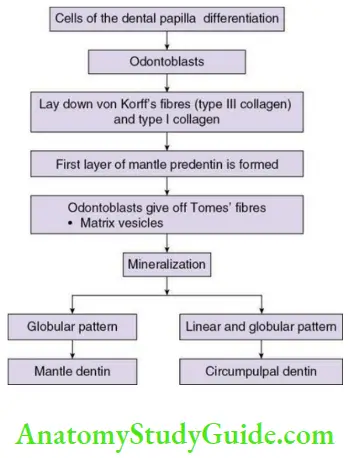
- Differentiation of odontoblasts.
- Formation of mantle dentin.
- Formation of circumpulpal dentin.
- Mineralization of dentin.
Differentiation of odontoblasts:
Cells of the dental papilla are separated from the inner enamel epithelium (IEE) by an acellular zone that contains fine collagen fibres. Changes occur in the cells of the dental papilla after the cells of the IEE undergo reversal of polarity.
The cells of the dental papilla differentiate into odontoblasts in three stages:
- Induction
- Competence
- Terminal differentiation
Dentinogenesis Induction:
- The IEE secretes growth factors that bind to the heparin sulfate in the basal lamina. The basal lamina now has the capacity to induce.
Dentinogenesis Competence:
- The cells of the dental papilla assume competence after a certain number of divisions after which they attain receptors for growth factors.
- Mitotic spindles are formed perpendicular to the basal lamina that lead to the formation of the daughter cells that are superimposed.
Dentinogenesis Terminal differentiation:
- The ectomesenchymal cells close to the acellular zone enlarge and differentiate into preodontoblasts and then odontoblasts. They change shape from ovoid to columnar. The amount of cytoplasm increases to accommodate the increasing number of cell organelles such as the Golgi apparatus, ribosomes, mitochondria and the rough endoplasmic reticulum.
- The odontoblasts increase in size and occupy the acellular zone, which is thus eliminated. The nuclei of the newly differentiated cells are away from the IEE.
Formation of mantle dentin:
Once differentiation of the odontoblasts is complete, the organic matrix of dentin is laid down.
- The appearance of distinctly large-diameter type III collagen fibres (0.1–0.2 mm) known as von Korff’s fibres is the first sign of dentin formation. These fibres originate deep among the odontoblasts. They extend towards the IEE and are seen in the structure-less ground substance below the epithelium.
- The odontoblasts produce type I collagen fibres as they increase in size, which get oriented parallel to the future DEJ. Thus, a layer of mantle predentin is formed.
As the deposition of collagen happens:
- The odontoblasts adjacent to the ameloblasts extend processes into the extracellular matrix. Some of these processes are termed enamel spindle when they lie between the cells of the IEE and cross the DEJ.
- The odontoblasts then give off matrix vesicles which are small membranebounded vesicles, which lie near the basal lamina.
- The odontoblasts start moving backwards towards the pulp and develops a cellular process called the Tomes’ fibre, which is a odontoblastic process found within the dentinal tubule.
The mineral phase is initiated within the matrix vesicles. The crystals within the vesicles grow. Once the vesicles rupture, the crystals are spread in the matrix which later fuse to form a layer of continuous mineralized matrix.
- Mineralization lags the deposition of organic matrix.
- A layer of organic matrix is always found between the odontoblasts and the mineralization front called the predentin.
- After mineral seeding, the odontoblasts produce the noncollagenous matrix that regulates mineral deposition.
Thus, a 15–20-micron thick layer of mantle dentin is laid down. The circumpulpal dentin is laid over the primary mantle dentin.
Formation of circumpulpal dentin:
The formation of circumpulpal dentin is similar to that of mantle dentin with the following exceptions:
- The collagen fibres are smaller in diameter (0.05 micron) than in mantle dentin. They are closely packed and are perpendicular to the DEJ.
- The ground substance is exclusively laid down by the odontoblasts (in mantle dentin, part of the ground substance is incorporated from the dental papilla).
- Mineralization does not involve matrix vesicles as it spreads from the preexisting mineralized mantle dentin.
Mineralization of dentin:
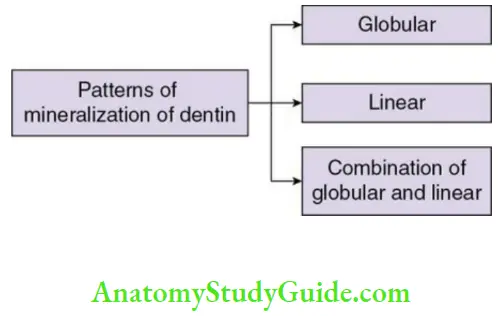
The patterns of mineralization depend on the rate of dentin formation.
1. Globular pattern:
- Seen in mantle dentin.
- The crystals are deposited in discrete areas of the matrix.
- These crystals then fuse with each other and form globular masses that further enlarge to form a calcified mass of tissue.
2. Linear pattern:
- When the rate of mineralization slows down then the mineralization front appears uniform. This pattern is referred to as linear.
In the circumpulpal dentin, both globular and linear patterns are seen. It is globular in the dentin adjacent to the mantle dentin and in the rest of the bulk of circumpulpal dentin it is a combination of both.
Thus, the dentinal matrix is laid down and mineralized.
Clinical Considerations
- Exposure of dentinal tubules:
- Caries, restorative procedures, tooth wear and fractures lead to
exposure of dentinal tubules. One square millimetre of exposed dentin may lead to damage of 30,000 odontoblasts. - Treatment: Seal the exposed dentin with a protective nonirritant substance.
- Caries, restorative procedures, tooth wear and fractures lead to
- Rapid spread of caries:
- Caries might lead to undermining of the enamel when it reaches the DEJ due to the spaces created at the DEJ by enamel tufts, enamel spindles and the opening and branching of dentinal tubules at the DEJ.
- The dentinal tubules might act as a passage for the caries causing bacteria.
- Dentinal tubules in caries/trauma/erosion:
-
- In areas of carious dentin, the tubules might be enlarged due to the microorganisms. Pain is experienced once the pulp is infected resulting in pulpal inflammation or pulpitis.
- Trauma from motor-driven instruments might damage the pulp.
- Air-driven instruments might cause aspiration of the odontoblasts from the periphery of the dentinal tubules.
- The sensitivity of dentin is increased in patients with periodontal problems.
Teeth involved: Maxillary premolars, maxillary molars and incisors. - Acidic soft drinks lead to erosion of peritubular dentin and removal of smear plug and increase in sensitivity. Brushing after consumption of acidic drinks induces smear layer formation and decreasing sensitivity.
- Treatment of sensitivity aims at
– blocking the dentinal tubule
– blocking pulpal nerve response
– Lasers such as Nd: Yag and Er:Yag lasers may be used (success rate: 5.2%–100%).
- Radicular dentin:
- The radicular dentin near the pulp and its outer surface is less
permeable than coronal dentin. Thus, it acts as a barrier to bacteria and fluids and decreases sensitivity.
- The radicular dentin near the pulp and its outer surface is less
- Smear layer:
-
- The crystalline debris generated during operative procedures such as cavity preparation is known as the smear layer. It also contains small dentinal shavings, microorganisms, saliva and sometimes blood and its pigments. This layer interferes with the bonding of the restorative material.
- Hence, acid etching helps in removal of the smear layer and improves
bonding by creating a rough porous surface.
Dentin Synopsis
- Dentin is the mineralized connective tissue that provides the bulk and form to the tooth. It is covered by enamel in the crown and by cementum in the root. It is laid down by the odontoblasts. Dentin forms before enamel. It is laid throughout life and determines the shape of the crown and number and size of the roots.
- Dentin is similar to bone and is considered to be vital. It is light yellow in colour, viscoelastic in nature and subject to slight deformation. It has 65% inorganic
content. - Dentin contains dentinal tubules that run from the pulp dentin border to the CDJ
and the DEJ. The tubules are at right angles to the pulp and the CDJ and DEJ. Dentinal tubules have primary and secondary curvatures. - The space between the odontoblastic process and the peritubular dentin is called periodontoblastic space. Dentinal fluid is present in the periodontoblastic space is called dentinal fluid. Dentinal hypersensitivity can be explained on the basis of the movement of this fluid.
- The dentin that surrounds the dentinal tubules is called the peritubular dentin. Intertubular dentin is the dentin present in between the tubules or between the zones of peritubular dentin.
- Predentin is a layer of unmineralized dentin located adjacent to the pulp.
- Primary dentin is the dentin formed before root completion.
- Mantle dentin is the first formed and the outermost layer of primary dentin, which is found below the DEJ.
- Circumpulpal dentin forms the rest of the bulk of primary dentin.
- Secondary dentin is the dentin formed after root completion.
- Tertiary dentin is the dentin formed due to caries, trauma and damage to the pulp during cavity preparation.
- The incremental lines in dentin are fine striations perpendicular to the dentinal tubules and are called incremental lines of von Ebner.
- Accentuated incremental lines are called contour lines of Owen.
- Neonatal line is the accentuated incremental line that separated prenatal dentin and postnatal dentin.
- Sometimes during mineralization when globules fail to fuse, the zones of hypomineralization between the globules are called interglobular spaces or interglobular dentin.
- The peripheral zone of dentin in the root next to the cementum appears granular. This is called Tomes’ granular layer.
- The empty dentinal tubules with the absence of the odontoblastic process are filled with air and appear black in transmitted light and white in reflected light. These are called dead tracts.
- The formation of dentin is called dentinogenesis. The organic matrix is initially laid down, which is later mineralized.
Leave a Reply