Development and Eruption of the Teeth
Tooth Eruption
Timely initiation, development and eruption of teeth are important for a healthy dentition.
Table of Contents
Tooth eruption is a complex process to move the tooth in a three-dimensional space and involves many tissues. It is the only instance where a developing organ, i.e. the tooth, must exit the confines of its bony crypt.
Tooth eruption is defined as the axial or occlusal movement of a tooth from its site of development within the jaws to its position of function in the occlusal plane.
Apart from physiologic tooth movements during the process of eruption, teeth also undergo complex movements to
- Maintain their position in the constantly developing jaws
- Compensate for masticatory wear
Read And Learn More: Oral Histology Notes
Pattern Of Tooth Movements
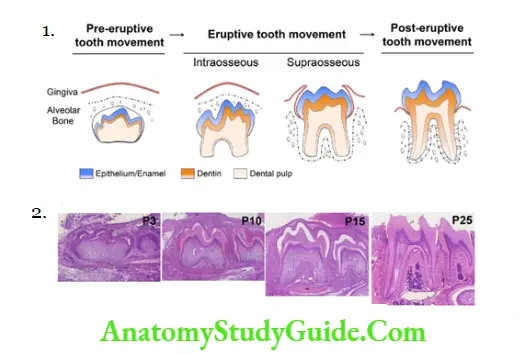
Considerable movement is required for teeth to reach its occlusal plane and become functional. The movements are termed as follows
- Preeruptive tooth movements
- Eruptive tooth movements
- Posteruptive tooth movements
Pattern Of Tooth Movements:
- Preeruptive tooth movements
- Eruptive tooth movements
- Posteruptive tooth movements
Preeruptive tooth movements:
Tooth movements differ for deciduous teeth, succedaneous teeth and permanent molars.
Movements of Deciduous Teeth:
Initially deciduous teeth germs are small in size and widely spaced. Due to growth of teeth germs the size increase and spaces between them are decreased resulting in crowding.
Crowding is relieved by further growth of the jaws in length, which allows mesial drift of anterior teeth and distal drift of deciduous molars. This drifting is due to
- Bony remodelling of crypt wall and bodily outward and upward (or downward, as the case may be) of the tooth germs.
- Increase in length, width and height of the jaws.
Movements of Succedaneous Teeth:
Change in position of succedaneous teeth in relation to their deciduous predecessors is slightly more complicated. The factors affecting this are
- Bodily movement of tooth germ
- Growth of the tooth germ
- Relative change in position of the associated deciduous and succedaneous teeth
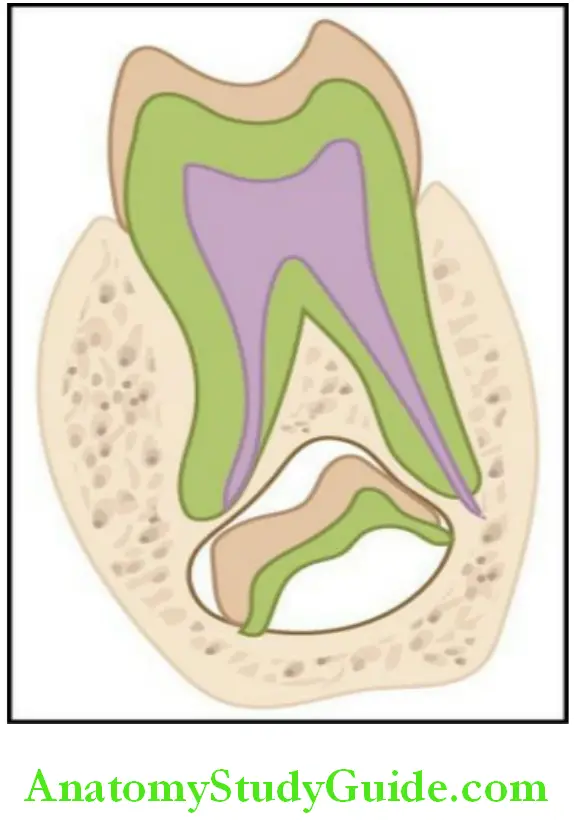
The permanent anterior teeth are:
- Initially lingual to the deciduous incisor
- Their position later changes to being placed more apically but lingually
The permanent premolars are:
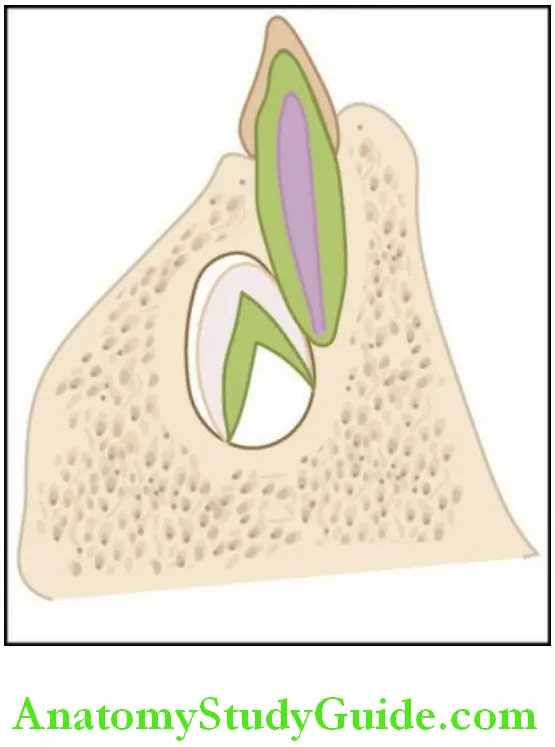
- Initially placed lingual to the primary molars
- Their position later changes to being placed in between the flared roots of the deciduous molars, apically.
Movements of the Permanent Molar:
The germs of the permanent molar do not have any predecessors and develop from the distal extension of the dental lamina. Initially, there is little space to accommodate them.
- The maxillary permanent molars develop in the maxillary tuberosity
- Initially, have their occlusal surfaces facing distally.
- When the maxilla has sufficiently increased in size, the molars swings down to their correct position.
- The permanent mandibular molars develop with their axes having a mesial inclination, and become upright only when sufficient jaw growth is available in the mandible.
Preeruptive tooth movements occur due to a combination of factors:
- Total bodily movement of the tooth germ
- Growth whereby one part of tooth germ remains fixed while the rest of it continues to grow, leading to a change in the centre of the tooth germ
These preeruptive movements made by the deciduous and permanent teeth position them for tooth eruption.
Clinical consideration: If the movement is not in the right direction and rate then it leads to ectopic eruption.
Eruptive tooth movements:
In this phase:
- The tooth moves from its developmental position in the jaws to its functional position in the occlusal plane.
- Axial/occlusal movement is seen.
As the jaw growth is still continuing thus, other movements apart from axial movements are superimposed on the teeth.
This phase can be subdivided into two components
- Intraosseous
- Supraosseous
- Intraosseous events involve resorption of bone and translocation of the tooth within bone.
- Supraosseous events include the movement of teeth once part of the crown is above the alveolar crest.
These stages are admittedly arbitrary and overlapping as all the teeth must have some intraosseous components for support even after eruption.
Posteruptive tooth movement:
Posteruptive tooth movements are tooth movement that serve to
1. Maintain the position of the erupted teeth while the jaw continues to grow
- Movements act in an axial direction to cope with the increase in size of the jaws and stop when jaw growth is completed.
2. Compensate for occlusal and proximal wear.
- Continues throughout life
- Involve axial and mesial migration to compensate the occlusal and proximal wear
Superimposed on these movements is the replacement of primary with the permanent dentition.
Rate of eruption:
It depends on the location of the tooth.
- During the intraosseous phase, the rate averages 1–10 microns per day.
- It increases to 75 microns/day in the supraosseous phase once it escapes its bony crypt. This rate will persist till the tooth reaches the occlusal plane.
Histology Of Tooth Movements
Preeruptive phase:
During this phase there is:
- Either mesial or distal drifting of the tooth germs and
- Growth of jaw bones, which requires remodelling of the bony crypt wall enclosing the tooth germ. This is achieved by selective resorption and deposition of bone by osteoclasts and osteoblasts.
In case of anterior deciduous tooth germs:
- As mesial drift occurs, resorption of bone occurs on the mesial side and deposition of bone on the distal side
In deciduous molars, as distal drift occurs
- Bone is resorbed on the distal side and deposited on the mesial side.
Eruptive phase:
Some key events occur during this phase:
- Formation of roots
- Formation of the periodontal ligament (PDL)
- Development of the dentogingival junction
Formation of roots:
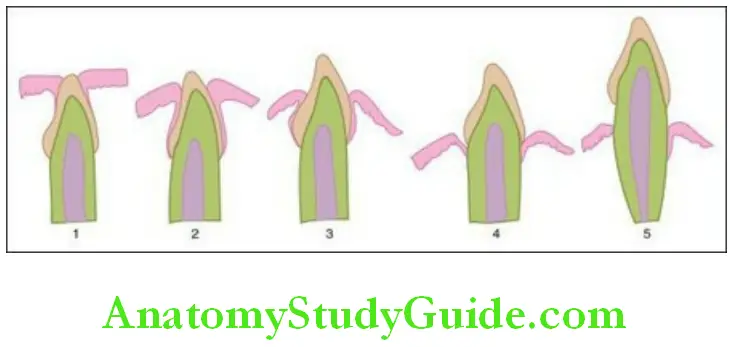
Root formation starts with growth of the Hertwig’s epithelial root sheath which initiates differentiation of odontoblasts from the dental papilla. The odontoblasts then form root dentin and increase of the root length occurs.
Formation of the periodontal ligament:
PDL and alveolar bone lining the crypt wall is formed after formation of root dentin and cementum. Along with formation, structural changes are noticed in the PDL, which might bring about tooth movement. Some of these changes are seen in the fibroblasts which are unique to the fibroblasts of the PDL.
- They contain intermediate filaments consisting of contractile proteins.
- They have adjacent cell to cell contacts of the adherens type.
- They have the ability to ingest and degrade extracellular collagen while forming new collagen fibrils.
Fibronexus: This describes a morphologic relationship between the intracellular filaments of fibroblasts, transmembrane proteins which produce an increased density of the fibroblast cell membrane, extracellular filaments, and fibronectin. (Fibronectin is a sticky glycoprotein that can stick to a number of extracellular components, including collagen.)
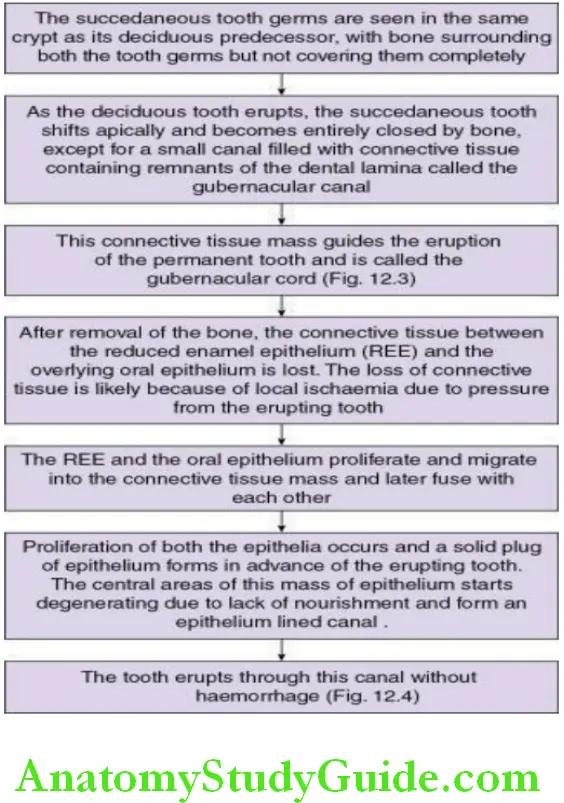
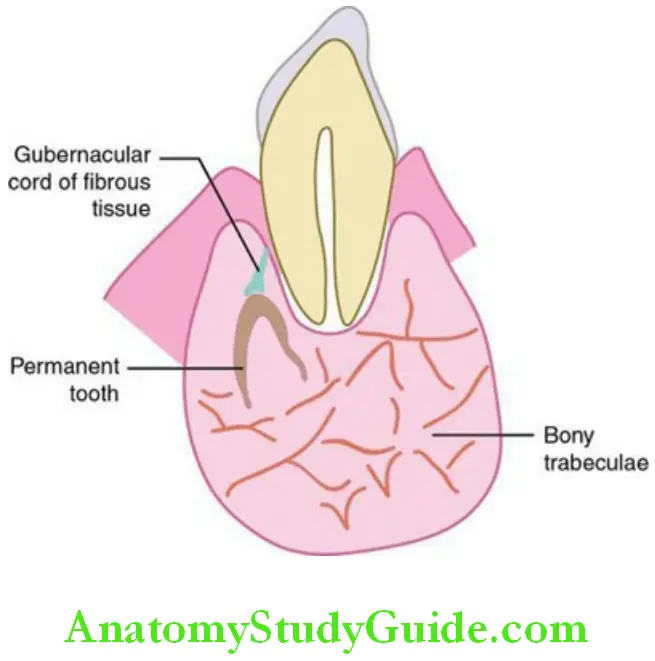
These unique features of PDL fibroblasts along with the cell contacts and fibronexus are thought to help in tooth movement. There are considerable histological changes that take place in the tissue over the erupting tooth which includes bone removal. In a tooth with a predecessor (succedaneous teeth), there is an additional anatomic feature, the gubernacular canal which contains the gubernacular cord (consisting of connective tissue and remnants of dental lamina), that aids in eruption. It happens as described in Flowchart.
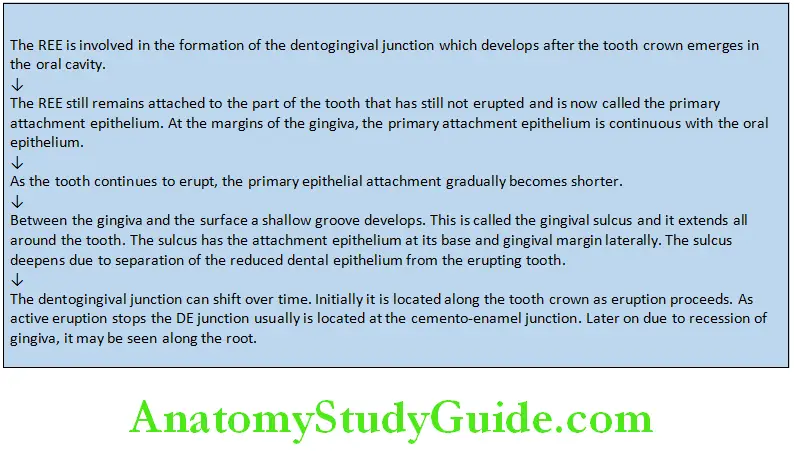
Development of the dentogingival junction:
Development of the Dentogingival Junction:
Posteruptive phase:
Once the teeth reach the occlusal plane, active eruptive movements cease, but passive movements occur in order to compensate for various developments. These movements are to:-
1. Compensate for jaw growth:
The teeth have to maintain their position in the jaws as they continue to grow till about 18 years of age. To compensate for jaw height and to maintain the occlusal contact, the teeth maintain an axial movement into the new occlusal plane. This is done by the same mechanism that causes active eruption.
Compensate for occlusal wear:
As teeth undergo constant friction due to grinding during mastication the occlusal aspect begins to wear away. This is compensated by axial movement of the tooth by the same mechanism that causes active eruption
2. Compensate for wear between proximal surfaces:
Teeth can wear at the contact areas on the proximal surfaces. This is compensated by mesial or approximal drifting of teeth.
- Mesial drift can occur due to several factors which include:
-
- An anterior component of occlusal force
1. As teeth come in contact, an anteriorly directed force is generated due to
1.The mesial inclination of the teeth
2.The summation of intercuspal planes that produces a forward directed force. - Contraction of transseptal fibres between teeth Transseptal fibres that run between adjacent teeth across the alveolar process help to achieve a mesial drift due to its contractile ability.
- Pressure from soft tissues. Cheeks and tongue may exert pressure to help to push teeth mesially.
- An anterior component of occlusal force
Histological changes observed during this phase are deposition of cellular cementum around the root apex; bone deposition at the alveolar crest and base of socket and remodelling of PDL fibres.
Mechanism Of Tooth Movements/Theories Of Eruption
Multiple theories have been proposed on the mechanisms of tooth eruption. Yet the process of tooth eruption is not completely understood. Many factors are thought to play a role in tooth eruption and different theories have been proposed which are not mutually exclusive. Some theories that merit serious considerations are listed in Box.
Theories Of Tooth Eruption:
- Bone remodelling theory
- Dental follicle theory
- Root formation
- Vascular pressure theory
- Periodontal ligament traction theory
Bone remodelling theory:
Bone remodelling theory proposes that:
- Selective deposition and resorption of bone around the developing tooth brings about tooth eruption.
- Formation of bone apical to the erupting teeth is thought the push the tooth to erupt.
- It is also observed that the alveolar process forms during tooth development and will be deficient in areas where primary or permanent teeth fail to develop.
Points in favour of this theory:
- Experimentally, when the tooth germ is removed and the dental follicle is left intact, an eruptive pathway develops in the overlying bone.
- If the tooth germ is substituted by a silicon replica, it erupts.
Drawbacks of this theory:
- No eruptive pathway is formed when the dental follicle is removed. Thus, the dental follicle is needed to achieve bony remodelling and thereby tooth eruption. The dental follicle supplies the source for new bone forming cells and the supply of osteoclasts derived from monocytes from its vascular supply.
- In animals that exhibit a genetic deficiency of osteoclasts, tooth eruption is prevented. It was proposed that osteoblasts secrete collagenase and other proteolytic enzymes to remove the osteoid layer, thereby exposing the newly denuded mineralized bone surface and providing the stimulus to attract osteoclasts to the site. Thus, whether bony remodelling is the cause or is the effect of tooth movement is not known and probably both circumstances may apply.
Dental follicle theory:
This theory suggests that the dental follicle plays an important role in tooth eruption.
The reduced enamel epithelium is known to initiate a cascade of intercellular signals that attract osteoclasts to the dental follicle and also secretes proteases that can break down the connective tissue. Due to this, bony remodelling and connective tissue degradation is facilitated helping in eruption.
The dental follicle is needed for eruption. Osteoclastogenesis and osteogenesis is initiated and regulated by the dental follicle at least for the intraosseous phase of eruption leading to tooth emergence.
For the supraosseous phase of eruption, in which the tooth moves to its final occlusal plane, the follicle may play a lesser role, while biomechanical influences may become more important.
Root formation theory:
This theory proposes that:
- The proliferating root impinges on a fixed base, thus converting an apically directed force into occlusal movement. This is by accommodation of either movement of the crown of the tooth or resorption of bone at the base of its socket as the root grows.
- The growth of the root produces a force that can move a tooth but a fixed base is essential to redirect the force occlusally. The existence of a ligament, the cushion hammock ligament, straddling the base of the socket from one bony wall to the other like a sling was also proposed. But the structure they proposed was actually the pulp-delineating membrane that runs across the apex of the root and has no bony insertion and so it cannot act as a fixed base.
Drawbacks of this theory:
- Some teeth move a distance greater than the length of their roots.
- Eruptive movements are observed even after root completion.
- Resecting of roots, experimentally, did not stop the eruption of teeth.
- Rootless teeth have been observed to erupt.
Vascular pressure theory:
A local increase in tissue fluid pressure in the periapical area is sufficient to move the teeth. As the teeth move in synchrony with the arterial pulse, local volume change can produce limited tooth movement.
Observations in favour of this theory:
Experimentally:
- Increase of hydrostatic pressure induced by hypotensive drugs, increases the rate of eruption.
- Stimulation of sympathetic nerves, which causes vasoconstriction and decrease of the hydrostatic pressure, decreases the rate of eruption.
The number of fenestrated capillaries increases with the eruption rate and their distribution varies; more numbers are seen near the base of the crypt than at the alveolar crest, thus accounting for the difference in hydrostatic pressure.
Drawback: Vascular pressure may play a role in generating an eruptive force but is not enough for the eruption of teeth as it may be a transient event.
Periodontal ligament traction theory:
This theory proposes that the cells and fibres of the PDL pull the tooth into occlusion. Accordingly, eruption of teeth could be brought about by a combination of events involving a force initiated by the fibroblasts. There is much experimental evidence that support the PDL traction as a factor in eruption.
- Drugs that interrupt the formation of collagen in the ligament interfere with eruption.
- Tissue culture experiments have shown that ligament fibroblasts are able to contract a collagen-gel and bring about movement of a disk of root tissue attached to that gel. Thus, fibroblasts of the PDL have the ability to contract and thus transmit a contractile force to the extracellular environment and the collagen fibre bundles in vitro.
- Animal experiments have shown the movement of tooth when only the PDL was present and the effects of vascular pressure and root growth were eliminated.
Thus, eruption could be brought about by a combination of events involving a force initiated by the fibroblasts. This force is transmitted to the extracellular compartment via the fibronexuses and to collagen fibre bundles, which, aligned in an appropriate orientation brought about by root formation, bring about tooth movement. Constant remodelling of the fibre bundles is a prerequisite for eruption to continue, as any interference can hamper eruption.
Drawbacks of this theory:
- Experiments dispute the observation as to the myofibroblastic nature of the fibroblasts.
- Existence of fibronexus has also been questioned.
In summary, though these many theories have their merits and demerits, it can be said that eruptive movements are multifactorial with:
- Traction exerted by the contraction of PDL fibroblasts
- Vascular pressure at the apex
- Bone remodelling and
- Root growth
Clinical Considerations
- Variation in the time of eruption:
Eruption seems to be a programmed process with each tooth following a consistent time line. Eg: Permanent molars are thus called 6-year molars as they are known to erupt at 6 years. Tooth eruption is early in females than in males of the same age and race.
Teeth which do not follow this range may undergo either premature or delayed eruption.- Premature eruption: It is seen in permanent teeth, due to premature loss of deciduous teeth leading to the early eruption of its successor
- Delayed eruption: It is more common.
- Local factors – Increased thickness of the tissues covering the erupting tooth, ankylosed deciduous tooth( A condition where the bone of the jaw is fused with the tooth due to trauma to the dental follicle preventing the eruption of the tooth.
- Systemic factors – decreased secretion of hormones influencing eruption-like growth hormone, thyroid hormones or bone diseases like osteopetrosis can delay eruption of teeth.
- Natal and neonatal teeth:
- The teeth that are present in the oral cavity at the time of birth are
referred to as natal teeth. - The teeth that erupt in the first 30 days of life are called neonatal teeth.
- The natal and neonatal teeth are extracted if they are mobile or are at risk of being aspirated as they are not considered supernumerary teeth. Studies have suggested that these teeth are prematurely erupted deciduous teeth.
- The teeth that are present in the oral cavity at the time of birth are
- Jaw size and impaction:
Evolution has resulted in jaw sizes becoming smaller; however, teeth size has remained the same and the result is crowding of teeth which is a common occurrence presently.- The third molars and maxillary canines have a tendency to become impacted as they are among the last to erupt and the space is limited due to the small jaw size.
- Failure of eruption of teeth:
Failure of eruption of teeth is usually associated with the permanent molars though no identifiable cause, either local or systemic can be found. Orthodontic intervention to force eruption is unsuccessful. A family history of failure of eruption and hypodontia is usually seen in such cases.
- Teething:
As a tooth erupts, an acute inflammatory response is seen in the adjacent connective tissue. Clinically, this is manifested as some pain, slight fever and general malaise. In infants, these symptoms are popularly referred to as ‘teething’.
- Supraeruption:
Teeth that have erupted beyond the occlusal plane are referred to as over erupted or supra erupted teeth. Careful planning is required in treating such teeth. - Orthodontic tooth movement:
The PDL and bone of the jaws possess ‘plasticity’ that enables the teeth to react favourably or unfavourably to its immediate environment. This unique feature is made use of by the orthodontist to move the tooth through the bone to achieve a favourable clinical response. An optimum force exerted on the tooth help it to move in such a way so as to correct maligned teeth.
Tooth Eruption Synopsis:
- Tooth eruption is a process by which the tooth is moved axially or occlusally from its developmental position in the jaws to its functional position in the occlusal plane.
- Tooth movements help position the teeth for eruption.
- The movements differ in deciduous teeth, succedaneous teeth and permanent molars when the teeth are still in the developmental position.
- It is an axial movement while the tooth erupts and there is an axial and mesial movement after the teeth are in the occlusal plane.
- Histologically bone remodelling is seen when teeth are still in the jaws. Development of root, PDL and formation of dentogingival junction is seen in the eruptive phase. In the posteruptive phase, cellular cementum deposition along with bony remodelling at base of socket and alveolar crest as well as PDL remodelling seen.
- Several theories have been put forward for the eruption of teeth. They include theories involving bone remodelling, dental follicle, root growth, vascular pressure and PDL traction. All of these factors can contribute to the eruption of teeth.
Leave a Reply