Pulp Capping
Pulp capping is the procedure used in dental restorations to prevent pulp from degeneration after being exposed or accidental exposure during tooth preparation. It can be of two types: indirect and direct pulp capping.
Table of Contents
Indirect Pulp Capping (IPC)
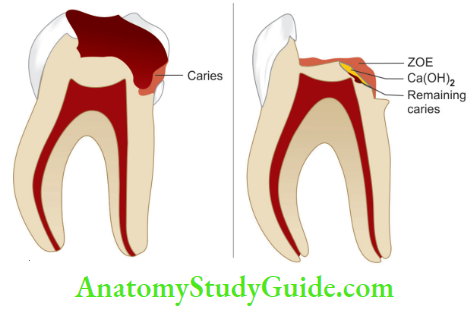
Indirect pulp capping is a procedure performed in a tooth with a deep carious lesion adjacent to the pulp. In this procedure, caries near the pulp is left in place to avoid pulp exposure and is covered with a biocompatible material. According to Cohen, indirect pulp therapy avoids pulp exposure in teeth with deep carious lesions in which there is no evidence of pulp degeneration or periapical disease.
Read And Learn More Endodontics Notes
1. Indirect pulp capping Rationale
- Decalcification of the dentin precedes bacterial invasion within the dentin
- Removal of outer carious dentin removes the majority of bacteria reducing further decalcifiation of deeper dentin
- Sealing the lesion to allow the pulp to generate reparative dentin
2. Indirect pulp capping Objective
- Arrest carious process
- Promote dentinal sclerosis
- Stimulate the promotion of reactionary dentin
- Remineralization of carious dentin while preserving pulp vitality
3. Indirect pulp capping Indications
- Deep carious lesion near the pulp tissue but not involving it
- No history of spontaneous toothache or history of mild discomfort from chemical and thermal stimuli
- No tenderness to the percussion
4. Indirect pulp capping Contraindications
- Presence of pulp exposure
- Radiographic evidence of pulp pathology
- History of spontaneous toothache
- Tooth sensitive to percussion
- Mobility present
- Root resorption or radicular disease is present radiographically
5. Indirect pulp capping Clinical Technique
In 1938, Bodecker introduced the stepwise excavation (SWE) technique for the treatment of teeth with deep caries for the preservation of pulp vitality where exposure of
pulp is probable.
-
- Indirect pulp capping is done in cases when carious lesion is quite close to the pulp;
- Placement of calcium hydroxide and zinc oxide eugenol dressing after excavation of soft caries;
- Permanent restoration of tooth.
6. Indirect pulp capping Two-appointment Technique
- First sitting
- Anesthetize the tooth and apply rubber dam to isolate it
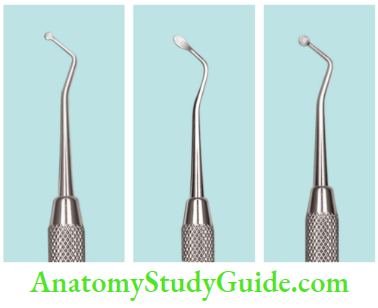
- Remove soft, necrotic, and infected caries either with a spoon excavator or round bur using a slow-speed handpiece. Use the fissure bur and extend it to sound tooth structure
- Leave a thin layer of dentin and some amount of caries to avoid exposure
- Place calcium hydroxide paste on the exposed dentin
- Cover calcium hydroxide with durable interim restoration
- Evaluate the tooth after 6–8 weeks
- Second visit (6–8 weeks later)
- If a tooth has been asymptomatic, the surrounding soft tissues are free from swelling and the temporary filling is intact, the second step can be performed.
- Obtain bitewing radiograph to assess the presence of reparative dentin
- Give local anesthesia and apply rubber dam
- Take care while removing restoration and calcium hydroxide dressing
- Remove the remaining affcted carious dentin which appears hydrated and flky. Th area around the potential exposure should appear whitish and may be soft (predentin) and should not be disturbed
- Gently clean and dry the cavity
- Cover the entire flor with a hard-setting calcium hydroxide dressing
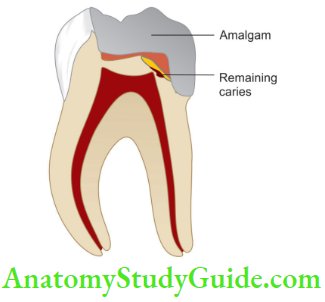
- Place reinforced zinc oxide eugenol or glass ionomer cement over calcium hydroxide and give fial restoration with composite or amalgam over it
7. One-appointment Technique
- Anesthetize the tooth and apply a rubber dam to isolate it
- Remove soft, necrotic, and infected caries either with spoon excavator or large round bur using a slow-speed handpiece. Remove all soft moist and leathery textures of dentin
- Leave a thin layer of dentin and some amount of caries to avoid exposure
- Place calcium hydroxide paste on the exposed dentin
- Cover the calcium hydroxide with durable interim restoration. Ensure proper seal of the restoration
- The removal of bacteria and substrate together with an effective seal of restoration provides a suitable environment for pulp to recover by laying down secondary dentin.
- It is difficult to state which treatment approach is better because no high-quality randomized clinical trials are available.
- The need to uncover the residual dentin to remove dehydrated dentin and view the sclerotic changes has been questioned. The second entry subjects the pulp to the potential risk of exposure owing to overzealous re-excavation.
8. Factors Affecting the Success of IPC
- If the remaining dentin thickness is approximately 0.5–2 mm, the prognosis is better
- Choice of indirect pulp capping agent; though many new materials have been introduced, calcium hydroxide has been used successfully due to its high pH and hard tissue formation
9. Ideal Requirements of a Pulp Capping Agent
Cohen and Combe gave the following requirements of an ideal pulp capping agent:
- Should maintain pulp vitality
- Should be bactericidal or bacteriostatic in nature
- Should be able to provide a bacterial seal
- Should stimulate reparative dentin formation
- Should be radiopaque in nature
- Should be able to resist the forces under restoration
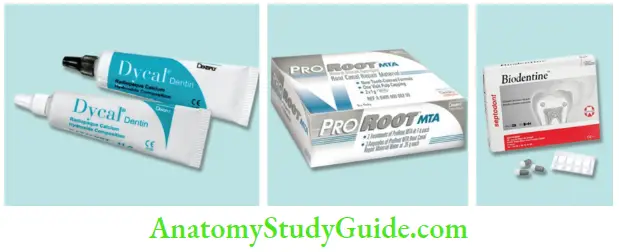
10. Materials used for Pulp Capping
- Calcium hydroxide
- Mineral trioxide aggregate (MTA)
- Biodentine
- BioAggregate
- Bonding systems
- Tricalcium phosphate
11. Calcium hydroxide
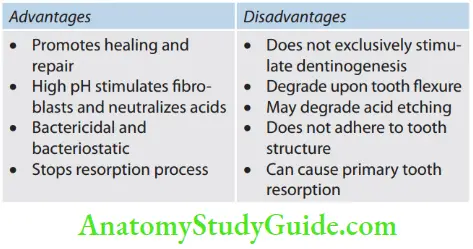
It was introduced by Hermann in 1920. It is most commonly used for pulp capping because, along with blocking the dentinal tubules, it helps in neutralizing the attack of inorganic acids from restorative materials.
- Mechanism of action of calcium hydroxide
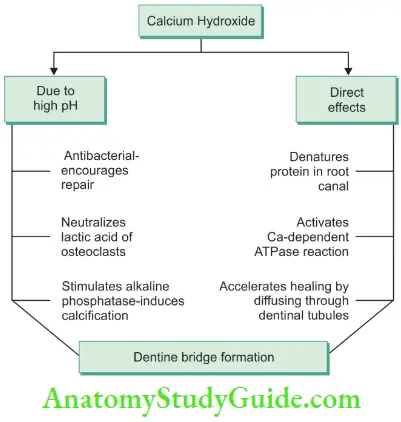
Calcium hydroxide has a high alkaline pH of 12.5 which is responsible for its antibacterial activity and its ability to form hard tissue. Though calcium ions from calcium hydroxide do not directly contribute to the formation of hard tissue, they stimulate the repair process. The mechanism of hard tissue formation is not known but can be considered due to a combination of its direct effects and indirect effects due to high pH.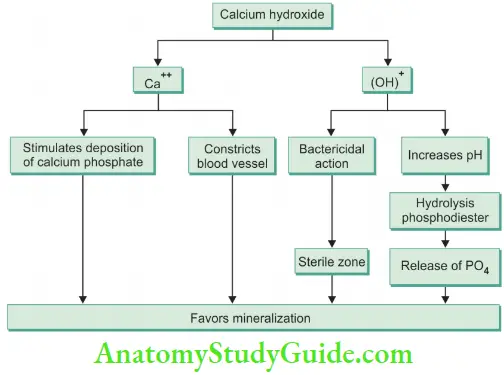
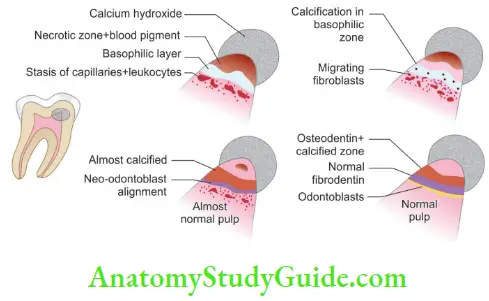
12. Histology of healing with calcium hydroxide Zone of obliteration
- Pulp tissue immediately in contact with calcium hydroxide is completely distorted because of the caustic effect of the drug
- This zone consists of debris, dentinal chips, blood clot, and particles of calcium hydroxide
13. Zone of coagulation necrosis
- A weaker chemical effect reaches subjacent, more apical tissue and results in zone of coagulation necrosis and thrombosis
- This is also called as Stanley’s mummified zone and Schroder’s layer of film necrosis
14. Line of demarcation
- This line forms between the deepest level of zone of coagulation necrosis and adjacent vital pulp tissue
- This is formed by the reaction of calcium hydroxide with tissue proteins to form proteinate globules
15. MTA
It was developed by Torabinajad in the 1990s. It contains
- Tricalcium silicate
- Dicalcium silicate
- Tricalcium aluminate
- Bismuth oxide
- Calcium sulfate
- Tetracalcium aluminoferrite
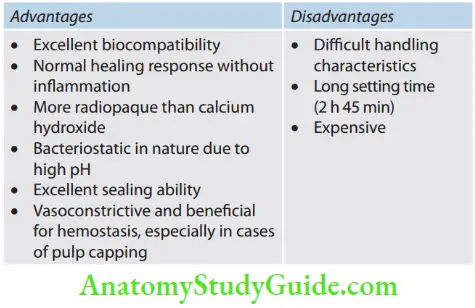
16. Properties
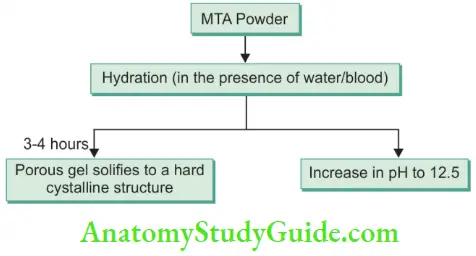
- pH of MTA is 12.5 and sets in a moist environment (hydrophilic in nature)
- In contrast to calcium hydroxide, it produces a hard-setting non-resorbable surface and low solubility
- It is antibacterial
- Induces pulpal cell proliferation and stimulates hard tissue formation The mechanism of action is not yet known.
- It is thought that when tricalcium oxide comes in contact with tissue fluids it releases calcium
- Hydroxide which causes hard tissue formation.
17. Tricalcium phosphate
- It is used in bone regeneration procedures. It shows the formation of the dentinal bridge by direct apposition on the pulpal wall.
18. Biodentine
- Its powder consists of tricalcium silicate, dicalcium silicate, calcium carbonate, and zirconium oxide. Liquid consists of hydrosoluble polymer and calcium chloride. Hydration of tricalcium silicate causes formation of hydrated calcium silicate gel and calcium hydroxide. It stimulates the release of TGF-β from pulp cells which causes dentine bridge formation. Biodentine is both a dentin substitute base and a cement for maintaining pulp vitality and stimulating hard tissue formation.
19. Bioaggregate
- It consists of bioceramic nanoparticles. Its powder and liquid are mixed to form a thick paste like consistency for use.
Direct Pulp Capping
Direct pulp capping (DPC) involves the placement of biocompatible material over the site of pulp exposure to maintain vitality and promote healing. When a small mechanical exposure of pulp occurs during cavity preparation or following a trauma, an appropriate protective base should be placed in contact with the exposed pulp tissue to maintain the vitality of the remaining pulp tissue.
- Direct pulp capping Rationale
To encourage young and healthy pulp to initiate a dentin bridge and form a wall over the exposure site. - Direct pulp capping Objective
The objective of DPC is to seal the pulp against bacterial leakage, protect the pulp from the thermal stimulus, encourage the pulp to wall of the exposure site by initiating a dentin bridge, and maintain the vitality of the underlying pulp. - Direct pulp capping Indications
- Small pinpoint (<1 mm) mechanical exposure of pulp surrounded by sound dentin during tooth preparation
- Traumatic injury (<24 h) with pinpoint exposure
- No or minimal bleeding at the exposure site
- Direct pulp capping Contraindications
- Carious or wide pulp exposure
- Spontaneous and nocturnal toothache
- Uncontrolled bleeding at the exposure site
- Radiographic evidence of pulp pathology
- Excessive tooth mobility
- Purulent or serous exudates from the exposure site
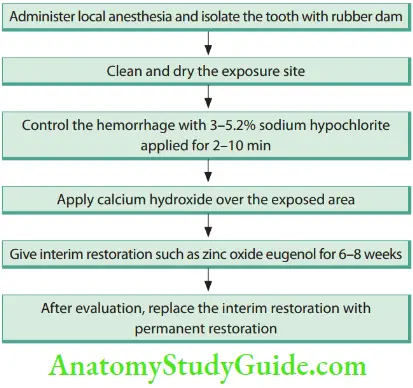
- Direct pulp capping Clinical Procedure
Factors Affecting Success of pulp capping
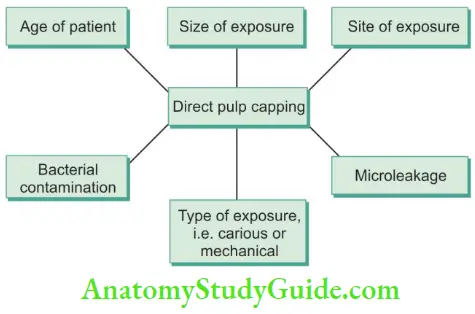
- Type of exposure: Prognosis is good if exposure is mechanical. In case of carious exposure, opt for endodontic treatment
- Type of restoration: Restoration which provides a hermetic seal shows better results when compared to temporary restoration
- Area of exposure: The prognosis of pulp capping is inversely proportional to the area of mechanical exposure. If exposure is <1 mm, go for DPC, if it is 1–2 mm, the choice is pulpotomy
- Class of restoration: Better prevention of microleakage in class 1 restoration shows better prognosis than class 2, 3, 4, and MOD restorations
- Choice of pulp capping agent: Calcium hydroxide is tried and tested material for successful capping procedures due to its high pH and the ability to form a dentinal bridge
- Time-lapse between exposure and treatment: If the time gap is up to 48 hours, perform partial pulpotomy; if it is >48 hours, opt for complete pulpotomy or pulpectomy
- Bacterial contamination: Prognosis is poor in case of bacterial contamination of exposure
- Why DPC is not Recommended in Primary Teeth?
Many researchers have given different reasons for not indicating DPC in primary teeth. Following are some of the reasons:
- McDonald’s (1956): Localization of infection and inflmmation in primary teeth is poorer than in permanent teeth
- Rayner and Southam (1979): Effects of dentinal caries are seen very rapidly in primary teeth than the permanent teeth
- Kennedy and Kopel (1985): Due to the presence of thin enamel and dentinal layers, the primary pulp gets rapidly affected by caries. Once the pulp gets exposed by caries, the prognosis for DPC is poor
- Kennedy (1985): Undifferentiated mesenchymal cells may differentiate into osteoclasts in response to pulp capping material resulting in internal resorption
- Stanley (1985): Primary teeth show incidences of increased resorption because of the already happening root resorption process
Leave a Reply