Diseases of Infancy and Childhood
Question 1. Write a short note on neonatal respiratory distress syndrome.
Answer:
Respiratory distress syndrome (RDS)/hyaline membrane disease
- Seen in preterm infants
- Associated with male gender
- Risk factors: Maternal diabetes, cesarean section
- Predisposing factor—lung immaturity
- The incidence of RDS is inversely proportional to the gestational age
- The fundamental defect in RDS is a deficiency of pulmonary surfactant
- Surfactant synthesis is increased by cortisol, insulin, prolactin, thyroxine, and TGF-β and is suppressed by insulin
- Labor increases surfactant synthesis
- Microscopically, eosinophilic hyaline membranes line the respiratory bronchioles, alveolar ducts, and alveoli
Read and Learn More Preparatory Manual of Pathology Question and Answers
Complications due to treatment of RDS
- High concentration and prolonged oxygen administration lead to retrolental fibroplasia (also called retinopathy of prematurity) and bronchopulmonary dysplasia
Question 2. Write a note on the hemolytic disease of newborns.
Answer:
Hemolytic disease of the newborn (immune hydrous)
- Caused by blood group antigen incompatibility between mother and fetus
- Rh and ABO blood groups antigens can induce clinically significant immunologic reactions
Etiology and Pathogenesis
- Occurs when fetal red cells reach maternal circulation
- Results in antibody response
- Among the Rh antigens, the D antigen is a major cause of Rh incompatibility
- Initial exposure to Rh antigen, results in IgM antibody formation
- Rh disease is uncommon after a first pregnancy
- However, during subsequent pregnancy (due to IgG antibody response), the risk of immune hydrous is increased
How to protect?
- Anti-D antibodies (RhIg) usage has reduced the incidence of maternal Rh isoimmunization
- Administration of RhIg to the mother is done at 28 weeks of pregnancy and within 72 hours of delivery
- RhIg is also administered following abortions
- Immunization to Rh-negative mothers decreases the risk for hemolytic disease in Rh-positive neonates in subsequent pregnancies
Question 3. Write a short note on ABO incompatibility.
Answer:
ABO incompatibility
- Seen in 20% to 25% of pregnancies
- Anti-A and anti-B antibodies produced are of IgM type, which does not cross the placenta
- The disease is milder than Rh incompatibility
- There is no effective protection against ABO reactions
The disease is not as severe as Rh incompatibility because
- Neonatal red cells express blood group antigens A and B poorly
- Cells, other than red cells, express A and B antigens, which absorb some of the transferred antibodies
Whom does it affect and why?
- ABO hemolytic disease affects infants with group A or B, who are born to group O mothers
- For some unknown reasons, group O women possess IgG antibodies directed against group A or B antigens, even without prior sensitization, resulting in affected first child
Question 4. Write a note on erythroblastosis fetal.
Answer:
Erythroblastosis fetal is
- In immune hydrops, the fetus will be severely anemic
- The liver and spleen will be enlarged, due to cardiac failure, secondary to anemia
- In the bone marrow, there occurs compensatory hyperplasia of the erythroid precursors
- Extramedullary hematopoiesis is present in the liver, spleen, and lymph nodes
- Increased hematopoietic activity results in increased numbers of immature red cells, including reticulocytes, norm oblasts, and erythroblasts (erythroblastosis fetal is)
Question 5. Write a note on the etiopathogenesis of cystic fibrosis.
Answer:
Cystic fibrosis
- Disorder of ion transport in epithelial cells
- Affects fluid secretion in exocrine glands and epithelial lining of the respiratory, gastrointestinal, and reproductive tracts
- Results from abnormal function of epithelial chloride channel protein encoded by cystic fibrosis transmembrane conductance regulator (CFTR) gene
- CFTR gene is located on chromosome 7q31.2
- Pulmonary manifestations are associated with the mutation of man nose-binding lectin 2 (MBL2) and transforming growth factor β1 (TGFB1)
Question 6. Enumerate the tumors affecting children.
Answer:
Tumors commonly encountered in childhood
- Leukemia, teratomas, Ewing sarcoma, rhabdomyosarcomas, hepatoblastoma, Wilms’ tumor, estrogenic sarcoma, neuroblastomas, retinoblastoma
Question 7. Discuss neuroblastomas about their clinical features, morphology, and prognostic factors.
Answer:
Neuroblastomas
- The most common extra-cranial solid tumor in childhood
- Associated with germline mutations in the anaplastic lymphoma kinase (ALK) gene
- Sites: Adrenal gland (40%), along the sympathetic chain, paravertebral region of the abdomen (25%), and posterior mediastinum
- Tumors can show spontaneous regression
Gross
- Range in size from minute nodules to large masses
Microscopy
- Tumor cells, arranged in solid sheets, have scant cytoplasm with dark nuclei
- Background demonstrates faintly eosinophilic fibrillary material (neuropil)
Homer Wright pseudo rosettes—tumor cells are concentrically arranged about a central space filled with neuropil - Ganglioneuroblastoma: Composed of ganglion cells (cells with abundant cytoplasm, large vesicular nuclei, and prominent nucleolus) admixed with primitive neuroblasts
- Ganglioneuromas: Better differentiated lesions, with mature ganglion cells and a few neuroblasts
- The maturation of neuroblasts into ganglion cells is accompanied by the appearance of Schwann cells
- Schwann stroma indicates a favorable outcome
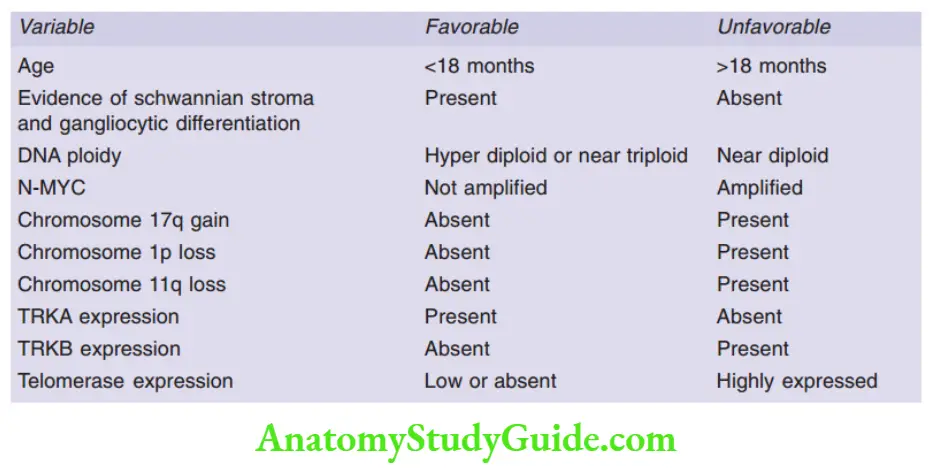
N-MYC amplification—the most important prognostic marker
Question 8. Write a note on the genetics and morphology of Wilms’ tumor.
Answer:
Pathogenesis and genetics
Risk is increased in any of the four groups of congenital malformations
1. WAGR syndrome
- Characterized by Wilms’ tumor, aniridia, genital anomalies, and mental retardation
- Individuals carry germ line deletions of 11p13
- Patients with aniridia show PAX6 gene mutations
2. Deny-Crash syndrome
- Characterized by male pseudohermaphroditism, and diffuse mesangial sclerosis
- Patients show germline abnormalities in WT1
- Increased risk for developing germ cell tumors (gonadoblastoma)
3. Beck with Wiedemann syndrome
- Characterized by enlargement of body organs (organomegaly), macroglossia, hemihypertrophy, omphalocele, and abnormal large cells in the adrenal cortex (adrenal cytometry)
- Chromosomal region implicated—localized to band 11p15.5 (“WT2”)
- Increased risk for developing hepatoblastoma, pancreata, adrenocortical tumors, and rhabdomyosarcoma
Morphology of Wilms’ tumor
Gross
- Present as a large, solitary, well-circumscribed mass
- 10% are bilateral or multicentric at the time of diagnosis
Cut section
- The tumor is soft, homogeneous, and tan to gray with occasional foci of hemorrhage, cyst formation, and necrosis
Microscopy
- Classic tri-physic combination of blaster, stromal, and epithelial cell types are seen
- Blaster component: Sheets of small blue cells
- Epithelial differentiation: In the form of abortive tubules or glomeruli
- Stromal cells: Fibrotic or myxoid in nature
Leave a Reply