Diseases of Pulp And Periapical Tissues Pathology Question And Answers
Question 1. What is dental pulp?
Answer. Pulp is the soft delicate connective tissue that occupies the central portion of the tooth and it has got two parts, namely the pulp chamber (the coronal portion) and the root canals (the radicular portion).
Question 2. What are the cellular constituents of pulp?
Answer. The cellular constituents of pulp include the following:
- Odontoblasts cells (which form dentin)
- Fibroblasts (which form collagen and maintain the pulp matrix)
Read And Learn More: Oral Pathology Short Notes Question And Answers
- Undifferentiated mesenchymal cells (from the connective tissue cells of the pulp)
- Macrophages and lymphocytes (defence cells to protect the pulp).
Question 3. What are functions of macrophages and lymphocytes in pulp?
Answer. The macrophages remove bacteria from pulp and interact with other inflmmatory cells during inflmmation. The lymphocytes (mainly T-lymphocytes) in the dental pulp are associated with immune defense systems.
Question 4. What types of collagen fiers are mainly found in pulp?
Answer. The fiers found in the pulp are mainly the type I and type III collagen in the ratio of about 55:45.
Question 5. What is the composition of ground substance of the pulp?
Answer. The ground substance in pulp is composed of glycosaminoglycans, hyaluronic acid, chondroitin sulfate, glycoproteins and water.
Question 6. What are the functions of the ground substance of pulp?
Answer. The function of ground substance is to support the pulpal cells and to act as the medium of transport for nutrients and metabolites.
Question 7. Name the types of nerve fiers present in pulp.
Answer. The nerve bundle entering the pulp consists mainly of sensory fiers of the trigeminal (fith cranial nerve) and sympathetic branches from the superior cervical ganglion. Each bundle contains both myelinated and non-myelinated axons.
Question 8. How many types of myelinated fiers are present in pulp?
Answer. The myelinated fiers are of two types namely the Aδ fiers and Aβ fiers.
Question 9. What type of pain is transmitted by the Aδ fiers?
Answer. Aδ fires are responsible for transmitting the sharp localized pain in the pulp.
Question 10. What type of pain is transmitted by the Aβ fiers?
Answer. The Aβ fibers are responsible for transmitting the mechanical, thermal and tactile sensations in the pulp.
Question 11. What are the non-myelinated nerve fiers present in pulp?
Answer. The non–myelinated nerve fiers of pulp are designated as C-fiers.
Question 12. What type of pain is transmitted by the C-fiers?
Answer. The C-fibers are associated with the transmission of dull, diffuse pain in the dental pulp.
Question 13. What is dentin-pulp complex?
Answer. Dentin is the vital and cellular hard tissue of tooth, ultimately and inseparably related to the dental pulp. Normally the dentin and pulp together act as a unit called the dentin– pulp complex, while responding to the injurious stimuli of various nature in the tooth.
Question 14. How dentin-pulp complex responds to injurious stimuli in pulp?
Answer. It protects the pulp by forming the layer of reparative dentin.
Question 15. Why the pulp tissue is called an extra-vulnerable organ?
Answer. Since the pulp tissue is lying within the solid confiement of dentinal walls and its entire blood supply depends upon the tiny blood vessels passing through the narrow apical foramina; a moderate degree of injury to pulp often elicits an exaggerated amount of damage with subseQuestionuent necrosis. That’s why pulp is often called an extra vulnerable organ.
Question 16. Degree of damage in the pulp tissue to injurious stimuli depends on what factors?
Answer. Degree of damage to any tissue including pulp tissue depends upon following factors:
- Anatomy of the tissue where injury occurred
- Intensity of the injurious stimulus
- General immunity or defense capacity of the body.
Question 17. Enumerate the etiological factors causing injury to pulp.
Answer. There are three major factors:
- Physical Factors
- Chemical Factors
- Microbial Factors.
Question 18. Name the physical factors causing acute injury to the pulp.
Answer.
- Accidental blow to tooth
- Heating due to grinding
- Cavity preparation without cooling
- Vigorous polishing with rotary instruments
- Root planning in periodontal therapy
- Large metallic restoration with inadeQuestionuate insulation.
Question 19. Name the physical factors causing chronic injury to the pulp.
Answer.
- Attrition due to abrasive foods or bruxism
- Abrasion due to abnormal tooth brushing.
Question 20. How chemical factors cause damage to pulp?
Answer. Medicaments or materials (e.g. acidic etchants) applied to dentin surface may cause damage to the pulp by diffusion through the dentinal tubules.
Question 21.How microbial agents enter into the pulp?
Answer.
- Dental caries with bacterial invasion of dentin and pulp
- Bacterial invasion into the pulp from a fractured tooth, where the dental pulp is exposed to the oral environment
- Anachoretic infection of the pulp.
Question 22. What is anachoretic infection of the pulp?
Answer. Anachoretic infection of the pulp occurs when bacteria present in the circulating bloodstream tend to accumulate in the pulp and cause infection.
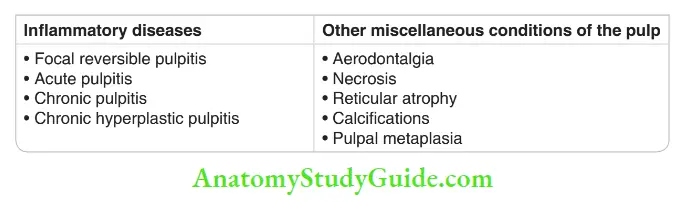
Question 23.Describe the classifiation of the pulpal diseases.
Answer.
Question 24. What is focal reversible pulpitis?
Answer. Focal reversible pulpitis is a mild, transient, localized inflmmatory reaction in the pulp, which can be treated by conservative means, without involving any form of direct pulp therapy.
Question 25. What is the other name of focal reversible pulpitis?
Answer. Pulp hyperemia.
Question 26. Name the etiological factors in focal reversible pulpitis.
Answer.
- Slowly progressing chronic caries
- Stimuli of short duration, e.g. cutting dentin while cavity preparation
- Metallic restoration without proper thermal insulation
- Chemical irritation to the pulp (e.g. acid etching in cervical margin of tooth)
- Excessive pressure by orthodontic appliances
- Severe attrition or abrasion of tooth with minimal dentin thickness.
Question 27. What are the common clinical manifestations of focal reversible pulpitis.
Answer. Tooth with focal reversible pulpitis is sensitive to thermal changes, especially to cold.
- Pain often results while drinking cold flids or when ice or cold air is applied to the tooth.
- The involved tooth often has large carious lesions or restoration with improper insulation.
Question 28. What is the duration of pain in focal reversible pulpitis?
Answer. The pain is of very short duration and it disappears as soon as the thermal irritant is withdrawn.
Question 29. People of which age group often develop focal reversible pulpitis?
Answer. Young people develop focal reversible pulpitis more often than the older individuals.
Question 30.Why focal reversible pulpitis occurs more often in young individuals?
Answer.
- Because of the more reparative capacity of pulp tissue in younger people
- Moreover, pulpal stimuli, which cause reversible pulpitis in young people often causes irreversible pulpitis to the older individuals because of the less viability of pulp.
Question 31. Describe the histology of focal reversible pulpitis.
Answer.
- Acute inflmmatory reaction in the odontoblastic or subodontoblastic regions
- Dilatation of pulpal blood vessels with increased vascular permeability
- Edema in the pulp with infitration by the polymorphonuclear leukocytes in the area
- Thrombosis of pulpal blood vessels may occur in some cases.
Question 32. Describe the changes in the odontoblast cells, in the histological study of focal reversible pulpitis.
Answer. Odontoblast cell nuclei may be displaced into the dentinal tubules due to either increased local tissue pressure or due to abnormal dentinal flid movements during injury. Few odontoblast cells could be damaged in the localized area of injury.
Question 33. What is the treatment of focal reversible pulpitis?
Answer. Treatment of focal reversible pulpitis is mostly directed towards elimination of the primary irritating factors and restoration of tooth wherever necessary.
Question 33a. Mention the characteristic change in pulp, when reversible pulpitis turns into irreversible pulpitis.
Answer. Bacterial invasion occurs in the pulp in irreversible pulpitis.
Question 34. What is acute pulpitis?
Answer. Acute pulpitis is an irreversible condition characterized by acute, intense inflmmatory reaction in the pulpal tissue with severe pain.
Question 35. What are the pathways of development of acute pulpitis?
Answer. Acute pulpitis can occur in the following pathways:
- As an extension of the focal reversible pulpitis
- As a de novo condition, where the inflmmation is acute from the beginning
- As an acute exacerbation of the chronic pulpitis.
Question 36. Name the etiological factors of acute pulpitis.
Answer.
- Caries with pulp exposure
- Pulp exposure due to faulty cavity preparation
- Blow to tooth with subsequent damage to pulp
- Pulp necrosis due to excessive heating of tooth during cavity preparation
- Chemical irritation to the pulp
- Cracked tooth syndrome
- Tooth or teeth coming in the line of fracture when the jaw is traumatized
- Anachoretic infection to the pulp (blood borne infection)
- Recurrent caries around a pre-existing restoration
- Metallic restoration in a tooth without proper thermal insulation.
Question 36a. What is the earliest symptom of acute pulpitis in a tooth?
Answer. Sensitivity in tooth to thermal change.
Question 37. In acute pulpitis how does the tooth respond to thermal stimuli?
Answer. The tooth is extremely sensitive to hot and cold stimuli; however, the pain in acute pulpitis can start spontaneously in the absence of any stimulus. Interestingly the pain persists for a longer duration even after the stimuli are removed.
Question 38. What name is given to the typical acute pain felt in acute pulpitis?
Answer. The pain is called lancinating type of pain.
Question 39. What ‘lancinating’ type of pain actually means?
Answer. In acute pulpitis patients often feel a lancinating type of horrible pain in tooth, which is equivalent to one that could be caused by stabbing or by a piercing knife or by a sharp instrument.
Question 40.Name the factors responsible for pain during pulpitis.
Answer.
- Pulpal inflmmation with compression of the intrapulpal nerves
- Nerve irritation from chemical mediators of inflmmation.
Question 40a. Why the pain gets so severe in acute pulpitis?
Answer. As the dental pulp is located within the solid confiement of dentinal walls, there is no escape route for inflmmatory exudates in acute pulpitis; and as the intra pulpal pressure builds-up quickly within the pulp, there is tremendous compression of the nerves resulting in lancinating type of pain.
Question 41. Why does the pain in acute pulpitis increases particularly at night?
Answer. The intensity of pain increases during sleep at night because there is an increase in the local blood pressure in head and neck region in supine position; which results in increased flw of blood in the pulp chamber. More flw of blood in the pulp chamber causes more compression of the nerves resulting in more pain.
Question 41a. In acute pulpitis why there is transient relief of pain as the patient keeps some cold water in mouth?
Answer. Because cold water causes contraction of intrapulpal exudates, which reduces the pressure inside pulp. Moreover cold water can also desensitize the nerve endings for a while. Also, cold desensitizes the pulpal nerve endings for a while.
Question 41b.Can the patient identify the offending tooth in acute pulpitis?
Answer. In the early stages of acute irreversible pulpitis the pain can be localized or rather the patient can identify the offending tooth.
However, in the later stages of acute pulpitis the pain is not only more severe but it becomes diffuse (involving a larger area); as a result, the patient is unable to identify the offending tooth.
Question 42. What is pulp strangulation?
Answer. In acute pulpitis the intrapulpal pressure often becomes very high as the acute inflmmatory exudates can’t escape from the solid confiement of pulp chamber. It can cause collapse of the apical blood vessel, resulting in circulatory collapse of the pulp and this phenomenon is known as pulp strangulation.
Question 42a. What is the immediate consequence of acute pulpitis?
Answer. Acute pulpitis not only causes excruciating pain, it helps in quick spreading of the inflmmation throughout the pulp tissue with subsequent necrosis. Thus acute pulpitis often leads to micro-abscess formation in the pulp along with liquefaction degeneration.
Question 43. Is the affected tooth tender to percussion in acute pulpitis?
Answer. The tooth is neither mobile and nor tender to percussion in acute pulpitis (tenderness in a tooth can only be felt when the pulpal inflmmation passes beyond the apical foramen and reaches the periapical tissues).
Question 44. If the tooth is tender to percussion, what can be the probable condition?
Answer. When the pulpal inflmmation spreads beyond the root apex into the periapical region, the tooth becomes tender to percussion and the condition is called apical periodontitis.
Question 45.In acute pulpitis, how does the offending tooth responds to electric pulp vitality tester?
Answer. The affected tooth responds to a lower level of current when electric pulp tester is used.
Question 46. In acute pulpitis how can the pain be relieved quickly?
Answer. Pain subsides quickly when drainage is established in a tooth with acute pulpitis; as pus and exudates come out of the pulp chamber causing release of pressure from the intrapulpal nerves.
Question 47. Describe the histopathological appearance of acute pulpitis.
Answer.
- Severe edema in the pulp with vasodilatation
- Moderate to dense infitration of polymorphonuclear leukocytes
- Focal or complete destruction of the odontoblast cells at the pulp dentin border
- Many micro-abscess formations in the pulp.
Question 48. What is acute suppurative pulpitis?
Answer. In case of severe pulp abscess, there may be complete liquefaction necrosis of the pulp with total destruction of the odontoblastic cell layer. This phenomenon is known as acute
suppurative pulpitis.
Question 49. What is dry gangrene of pulp?
Answer. In acute pulpitis, sometimes the death of pulp may be accompanied by tissue dehydration; this condition is known as dry gangrene of the pulp.
Question 50. What are the treatments of acute pulpitis?
Answer.
- Drainage of exudates or pus from the pulp chamber
- Direct pulp capping
- Root canal treatment (RCT)
- Extraction of tooth.
Question 51. What is chronic pulpitis?
Answer. Chronic pulpitis is a condition characterized by low grade, persistent inflmmatory reaction in the pulp with little or no constitutional symptoms.
Question 52. Describe the clinical features of chronic pulpitis.
Answer. The teeth in chronic pulpitis are usually asymptomatic and often there may be an intermittent dull and throbbing pain in the tooth. Even if the pulp is exposed to the oral environment through a large open cavity in the tooth, still a very little pain is felt.
Question 53. In chronic pulpitis, how the tooth responds to electric pulp vitality tester?
Answer. The tooth usually responds to a higher level of current when electric pulp tester is used. It happens due to degeneration of most of the nerve fires in the chronically inflmed pulp.
Question 54. Describe the histopathology of chronic pulpitis.
Answer.
- Chronic inflmmation in the pulp with cellular infitration by lymphocytes, plasma cell and macrophages, etc
- Blood capillaries are prominent and few microorganisms are also found in the pulpal tissue
- Prolonged chronic inflmmation may encourage firoblastic activity in the pulp
- Persistent chronic pulpitis may cause diffuse or solitary calcifiations in the pulp.
Question 55. What is the treatment of chronic pulpitis?
Answer. Root canal treatment or extraction of tooth.
Question 56. What is pulp polyp?
Answer. Pulp polyp is an unusual type of hyperplastic granulation tissue response in the pulp,
which is characterized by an overgrowth of the tissue outside the boundary of the pulp chamber as a protruding mass.
Question 57. What is the other name of pulp polyp?
Answer. Chronic hyperplastic pulpitis.
Question 58. How does pulp polyp develops?
Answer. Pulp polyp develops in a tooth in presence of low grade sustained inflmmation in a highly vascularised pulp; mainly in young individuals. This leads to an intense proliferation of the pulpal connective tissue with hyperplastic growth; as a result the pulp becomes so large that it protrudes outside the tooth cavity and hence called pulp polyp.
Question 59. Name the factors that favor the development of pulp polyp.
Answer.
- Persistence of balance between injurious agents and tissue resistance in pulp
- Presence of a low grade sustained inflmmation
- Pulp tissue should be well-vascularized with excellent tissue reactivity
- The carious cavity should be wide open
- The patients must be young with good body resistance
- The apical foramen of the affected tooth must be wide so that pulpal strangulation and complete necrosis due to inflmmation does not occur.
Question 60. Describe the clinical features of pulp polyp.
Answer. Pulp polyp clinically appears as a small, pinkish-red, lobulated mass, which protrudes from the pulp chamber and often fils up the carious cavity. The polyp is a soft painless mass, which bleeds upon provocation.
Question 61. Pulp polyp commonly occurs in relation to which teeth?
Answer. It commonly develops in relation to deciduous molars and fist permanent molars.
Question 62. What is the common age of occurrence of pulp polyp?
Answer. The condition is seen either in children or young adults.
Question 63. In what type of cavity in the affected tooth does the pulp polyp develops?
Answer. The affected tooth always has a large open carious cavity which is present for a long duration.
Question 64. Describe the histopathology of pulp polyp.
Answer.
- Pulp polyp histologically presents a mass of hyperplastic tissue with features of a typical granulation tissue
- It consists of numerous proliferating firoblasts and young blood capillaries with edema and hyperemia
- Focal areas of pulp necrosis with chronic inflmmatory cell infitration by the lymphocytes, plasma cells and sometimes polymorphonuclear neutrophils, etc. are common
- Occasionally stratifid squamous type epithelial lining is found on the surface of the pulp polyp, which resembles oral epithelium.
Question 65. How pulp polyp can have epithelium on its surface?
Answer. Although pulp is mesenchymal tissue and an internal organ of tooth, it comes in contact with the oral environment as pulp polyp develops; desquamated epithelial cells present in saliva often get implanted on the surface of pulp polyp because of persistent rubbing of buccal mucosa against the lesion.
Question 66. From where do the epithelial cells on the surface of pulp polyp come?
Answer. The epithelial cells on the surface of the polyp are believed to be the desquamated epithelial cells, which came either from the buccal mucosa, gingiva or from the salivary gland ducts, etc. These cells are carried via saliva and are transplanted on to the surface of the pulp polyp.
Question 67. What is the treatment of pulp polyp?
Answer. Treatment is done either by root canal treatment or by extraction of the affected tooth.
Question 68. What is aerodontalgia?
Answer. Aerodontalgia is an unusual type of dental pain, which occurs as an effect of changes in the altitude.
Question 69. At what times, the pain due to aerodontalgia appears?
Answer. People experience the pain due to aerodontalgia in the tooth mostly during high altitude flght, high mountain climbing or during deep sea diving. However at ground levels, they never experience the same pain in the tooth.
Question 70. What may be the underlying cause of aerodontalgia?
Answer. The condition may be related to subclinical pulpitis.
Question 71. In relation to which other teeth pain similar to aerodontalgia can also occur?
Answer. Sometimes pain due to aerodontalgia may occur in an endodontically treated tooth with improper obturation of the root canals.
Question 72. How pain due to aerodontalgia occurs in endodontically treated tooth?
Answer. The entrapped air in improperly obturated root canals may expand during flght or during diving (due to alteration in the atmospheric pressure) which creates pressure in the periapical nerve bundles and produce pain.
Question 73. Name another interesting fact about aerodontalgia?
Answer. In some cases of aerodontalgia, the pain may not start particularly during flght or at the time of diving; instead, it may occur few hours or days later.
Question 74. How necrosis of pulp occurs?
Answer. Pulp necrosis may occur either due to pulpitis or due to injury and subsequent occlusion of the apical blood vessels.
Question 75. How coagulative type of necrosis of the pulp occurs?
Answer. A coagulative type of necrosis of the pulp occurs due to ischemia.
Question 76. Name one hematological condition, which can cause pulp necrosis?
Answer. In sickle cell anemia, blockage of the pulpal vessels by sickled or defective RBCs may result in pulp necrosis.
Question 77. Name the pulp vitality tests.
Answer.
- Heat test
- Cold test
- Percussion of tooth
- Palpation of tooth
- Pressure on tooth
- Electric pulp vitality tests
- Laser doppler flwmetry.
Question 78. What is heat test of pulp?
Answer. This test is done to determine the sensitivity of tooth to heat in order to evaluate the vitality of the same tooth.
Question 79. How heat test can be done on a tooth?
Answer. Sensitivity to heat may be tested by application of hot water or heated gutta-percha stick on the suspected tooth.
Question 80.How the result of heat test on a tooth can be evaluated?
Answer. A tooth having pulpitis will respond to a lower level of heat as compared to a normal tooth.
Therefore, it is always important that the response gathered from a suspected tooth should always be compared with a normal tooth from the some arch or the opposing arch.
Question 81. What is cold test for evaluation of tooth vitality?
Answer. This test is done by selective application of cold water or water ice or dry ice to evaluate the pulp vitality.
Question 82. How percussion can help in indicating the vitality of a tooth?
Answer.Sensitivity to percussion indicates periapical inflmmation in a tooth, this can happen in pulpitis only when the inflmmatory process has extended beyond the tooth apex into the periapical area.
Question 83. How percussion in a tooth should be carried out?
Answer. Percussion in a tooth to evaluate the sensitivity should be carried out both in vertical and in horizontal direction.
Question 84. How palpation can help in indicating the vitality of a tooth?
Answer. Palpation of the apical tissues may elicit tenderness or it may reveal soft or hard tissue swelling, which are indicative of periapical inflmmations. A tooth with periapical inflmmation is usually non-vital.
Question 85. Can digital pressure on a tooth reveal any diagnostic clue?
Answer. Gentle pressure on the tooth often helps to diagnose fracture or cracked tooth syndrome.
It can also give indication regarding the presence of periapical inflmmation.
Question 86. What is electric pulp testing?
Answer. The electric pulp testing is a diagnostic examination, which helps to reveal the vitality of a tooth.
Question 87. How electric pulp vitality testing is done?
Answer. In this test electrical impulses are sent across the pulp and as the pulpal nerves are sensitised, varying degrees of sensory reply from the pulp can be recorded, which alters in different inflmmatory states.
Question 88. Describe the results of electric pulp testing in different pathophysiologic states of pulp.
Answer.
- In reversible pulpitis—The pulp gets stimulated at a lower level of current as compared to that of a normal pulp (because of lower pain threshold)
- In irreversible pulpitis—The threshold level is further lowered and the pulp responds to an even lower level of current
- In chronic pulpitis—The pulp responds to a higher level of current (as compared to normal pulp) and it happens due to the decreased number of sensory nerve fiers in the pulp as a result of necrosis.
Question 89. What is the use of laser Doppler flwmetry in evaluating tooth vitality?
Answer. Laser Doppler flwmetry can be used as an advanced diagnostic aid for accurate diagnosis of pulpal pathology.
Question 90. Which one is the most reliable pulp vitality test?
Answer. Cold test is by far the most reliable method of pulp vitality testing.
Question 91. Name the common gram-negative anaerobic bacilli found in an infected pulp.
Answer.
- Bacteriodes buccae
- Bacteriodes denticola
- Bacteriodes endodontalis
- Bacteriodes gingivalis
- Fusobacterium nucleatum
- Wolinela recta
- Selenomonous sputigena.
Question 92. Name the common Gram-negative anaerobic cocci found in an infected pulp.
Answer. Veillonella parvula.
Question 93. Name the common Gram-positive anaerobic rods found in an infected pulp.
Answer.
- Actinomyces israelii
- Actinomyces odontolyticus
- Eubacterium alactolyticum
- Eubacterium brachy
- Eubacterium lentum
- Eubacterium nodatum
- Lactobacillus catenaforme
- Lactobaiilus minutes.
Question 94. Name the gram-positive anaerobic cocci present in infected pulp.
Answer.
- Streptococcus constellatus
- Streptococcus intermedius
- Streptococcus morbillorum
- Peptostreptococcus anaerobius
- Peptostreptococcus magnus
- Peptostreptococcus prevotii.
Question 95. Name the aerobic or facultative anaerobic organisms in inflmed pulp.
Answer.
- Gram-negative rods
- Capnocytophaga ochracea
- Eikenella corrodens
- Campylobactorsputorum
- Gram-positive rods
- Actinomyces naeslundii
- Actinomyces viscosus
- Gram-positive cocci
- Streptococcus mutans
- Streptococcus milleri
- Streptococcus mitior
- Streptococcus sanguis.
Question 96. What are periapical lesions?
Answer. When the inflammatory process spreads beyond the root apex of a tooth from the pulp and produce pathological conditions there, the lesions are called periapical lesions.
Question 97. Mention the sources from where inflmmations can come to produce lesions in periapical region.
Answer.
- Inflammation from dental pulp (most common source)
- Inflammation from periodontium
- Inflammation from blood (anachoretic infection)
- Inflammation from adjacent inflmed teeth
- Periapical inflammation following trauma
- Spread of inflammation from fractured jaw.
Question 98. Name the common periapical lesions in the mouth.
Answer.
- Primary acute apical periodontitis
- Periapical granuloma
- Phoenix abscess
- Periapical abscess
- Periapical cyst.
Question 99. How primary acute apical periodontitis occurs?
Answer. It occurs mostly as a result of extension of the pulpal inflmmation into the periapical tissues.
Question 100.Can primary acute apical periodontitis occur in a vital tooth?
Answer. If the lesion occurs as a result of occlusal trauma, the involved tooth in that case is usually vital.
Question 101. Name the common clinical fidings in primary acute apical periodontitis.
Answer.
Moderate pain and sensitivity in the tooth
- Slight extrusion of the tooth due to accumulation of inflmmatory exudates in the apical periodontal ligament
- The most important and determining feature is the severe pain on slight pressure during mastication
- Thermal changes (hot and cold) do not aggravate the pain.
Question 102.What are the possible complications in primary acute apical periodontitis?
Answer.
- Periapical abscess formation
- Regional lymphadenopathy
- Cellulitis
- Development of periapical granuloma.
Question 103. What is the treatment in primary acute apical periodontitis?
Answer.Extraction or endodontic treatment of the diseased tooth.
Question 104. What is chronic apical periodontitis?
Answer. It is a localized mass of granulation tissue around the root apex of a non-vital tooth, which develops in response to a low grade infection or inflmmation.
Question 105. What is the other name of chronic apical periodontitis?
Answer. Periapical granuloma.
Question 106. Name the etiological factors of periapical granuloma.
Answer.
- Extension of the pulpal inflmmation beyond the root apex
- Occlusal trauma
- Orthodontic tooth movements with excessive uncontrolled force.
- Acute trauma due to blows on the tooth
- Perforation to the root apex during endodontic therapy
- Spread of periodontal infection into the root apex
- Chemical irritation.
Question 107. How periapical granuloma develops?
Answer. Inflmmation extending from the dental pulp of a tooth into the periapical region causes destruction of the apical periodontal ligaments, adjoining alveolar bone and cementum, etc. As a result, these tissues are replaced by a mass of granulation tissue and thus periapical granuloma develops.
Question 107a. After the formation, how does periapical granuloma further increases in size?
Answer. It occurs due to gradual resorption of bone surrounding the root apex by chemical mediators like osteoclast activating factor (OAF) and collagenase, etc. These mediators are released by chronic inflmmatory cells present in the area.
Question 108. Describe the clinical features of periapical granuloma in a tooth.
Answer.
- The offending tooth produces sensitivity to percussion
- There can be mild pain and discomfort in the tooth during chewing solid foods
- Patient may give a previous history of pain in the same tooth (when pulpitis was present)
- The involved tooth is always non-vital
- Tooth does not responds to thermal or electric pulp testers.
Question 109. Why the offending tooth is often sensitive to percussion in periapical granuloma?
Answer. It occurs due to edema, hyperemia and inflmmation of the apical periodontal ligaments.
Question 110. What is the early radiographic change in periapical granuloma?
Answer. In early stages, periapical granuloma radiographically shows widening of the periodontal ligament space of the affected tooth.
Question 111. What is the radiographic feature of a fully developed periapical granuloma?
Answer. Fully developed lesions usually produce a well-defied, radiolucent area of varying size, which appears to be in continuity with the root apex.
Question 111a. As similar type of apical radiolucency is seen in both cases, so how can the periapical granuloma be differentiated from cementoma?
Answer. Through vitality test (in cementoma the tooth is vital and it is non-vital in periapical granuloma).
Question 112. Can periapical granuloma cause root resorptions in the affected tooth?
Answer. Long-standing periapical granuloma may cause varying degrees of root resorption and loss of apical lamina dura.
Question 113. Describe the histopathology of periapical granuloma.
Answer.
- Periapical granuloma appears as a granulation tissue mass consisting of proliferating firoblasts, endothelial cells and numerous immature blood capillaries.
- Chronic inflmmatory cells, e.g. macrophages, lymphocytes and plasma cells, etc.are often present in the lesion.
- Some lesions show the presence of epithelial islands, cell rest of Malassez, cholesterol clefts and few giant cells.
Question 114. Why periapical granuloma is called a sterile lesion?
Answer. In case of periapical granuloma a balance between the pathogenicity of bacteria within the root canal of tooth and the defense capacity of periapical tissue is established.
Because of this no bacteria could be found within the periapical granuloma and hence it is called a sterile lesion.
Question 115. What are the consequences of periapical granuloma?
Answer.
- Root resorption of the affected tooth
- Development of periapical abscess
- Development of periapical cyst
- Development of hypercementosis.
Question 116. What is the treatment of periapical granuloma?
Answer. The lesion is treated either by extracting the tooth or by performing root canal treatment in the tooth with apicoectomy or apical curettage.
Question 117. What is a phoenix abscess?
Answer. It is an explosive type of acute exacerbation in a pre-existing periapical granuloma.
Question 118. What are the clinical manifestations of phoenix abscess?
Answer. Clinically phoenix abscess presents severe pain, local swelling and extreme tenderness in the tooth upon pressure and sometimes facial cellulitis.
Question 119. What is a periapical abscess?
Answer. Periapical abscess can be defied as a localized, acute or chronic suppurative infection in the periapical region of a non-vital tooth.
Question 120. Name the etiological factors of periapical abscess.
Answer.
- Extension of pulpal infection
- Fractured tooth
- Perforation of apical foramen during root canal treatment
- Extension of periodontal infection
- Secondary infection in pre-existing periapical granuloma or cyst or scar.
- Anachoretic infection.
Question 121. Name the common microorganisms involved in the causation of periapical granuloma.
Answer.
- Prevotella
- Porphyromonas
- Anaerobic streptococci
- Anaerobic staphylococci.
Question 121a. Name one microorganism which cannot survive in the periapical abscess.
Answer. Pseudomonas group of organisms.
Question 122. Describe the clinical features of acute periapical abscess.
Answer.
- Severe pain in the affected tooth
- Localized swelling and erythematous change in the overlying mucosa
- Extrusion of the tooth from its socket
- Aggravated pain during percussion
- The associated tooth is non-vital.
Question 123. In acute periapical abscess, how the tooth reacts to thermal changes?
Answer. Reaction of tooth to thermal changes is important in acute periapical abscess. Application of heat intensifis pain, whereas application cold relieves the pain temporarily.
Question 124. What are the possible outcomes in an acute periapical abscess if no treatment is done?
Answer. If prompt treatment is not given in an acute periapical abscess, the following things can happen:
- Acute abscess may turn into a chronic one
- Development of pus discharging sinus (intraoral or extra-oral)
- Development of cellulitis
- Development of space infections
- Development of Ludwig’s angina
- Development of septicaemia and cavernous sinus thrombosis
- Development of osteomyelitis.
Question 125. Generally under what circumstances an acute periapical abscess may turn into a chronic one?
Answer. If the host resistance is high or the virulence of the causative organisms is low.
Question 126. What is the radiographic appearance of an acute periapical abscess?
Answer. Radiographic changes in acute abscess are little and are limited to only slight thickening of the periodontal ligament space in apex region of the involved tooth.
Question 126a. How many days after its formation, an acute periapical abscess can be visible radiographically?
Answer. After 7 to 10 days.
Question 127. Why an acute periapical abscess does not exhibit much radiographic change?
Answer. As the acute periapical abscess develops quite rapidly, there is little time for the lesion to
cause any signifiant amount of bone resorption that could be detected radiographically.
Question 128. What is the radiographic feature of chronic periapical abscess?
Answer. In chronic periapical abscess, radiographs often reveal small radiolucent areas at the root apex with poorly defied margins.
Question 128a. How periapical abscess, periapical granuloma and periapical cyst can be compared radiographically?
Answer. Although not always confirmatory, radiographs can help in distinguishing between these three lesions. Periapical abscess will have small radiolucent area at the root apex with poorly defied margins.
Periapical granuloma will produce a well defied radiolucent area at the root apex. Periapical cyst produces a well defied radiolucent area at the root apex, surrounded by a well-corticated margin.
Question 129. Describe the histological features of acute periapical abscess.
Answer. The abscess exhibits a zone of liquefaction necrosis containing proteinaceous exudates, necrotic tissue and a large number of viable or dead neutrophils (pus).
There is presence of many dilated blood capillaries with infitration of neutrophils. Bony trabeculae in the periapical region may show empty lacunae, which results from the death of the osteocytes.
Question 130. Describe the histological features of chronic periapical abscess.
Answer. In chronic periapical abscess the inflammatory cell pattern is different and these lesions often exhibit infitration by lymphocytes, plasma cells and macrophages, etc. Areas of bone destruction are also accompanied by areas of firosis as well as bone regeneration in chronic lesions.
Question 131. What are the treatment modalities of acute periapical abscess?
Answer.
- Drainage of pus
- Administration of antibiotics
- Root canal therapy or extraction of the affected tooth.
Question 132. What is osteomyelitis?
Answer. Osteomyelitis is defied as the inflmmation of bone and bone marrow along with the surrounding periosteum.
Question 133. Name the structures affected in osteomyelitis.
Answer. This inflmmatory condition involves all the structures of bone, e.g. the bone marrow, Haversian systems, periosteum, blood vessels, nerves and epiphyses, etc.
Question 134. Name the different types of osteomyelitis in the jaw bones.
Answer. Jaw bone osteomyelitis can be broadly divided into the following groups:
- Acute osteomyelitis
- Chronic specific osteomyelitis
- Chronic non-specific osteomyelitis
- Radiation-induced osteomyelitis
- Idiopathic osteomyelitis.
Question 135. On what basis the specifi and non-specific type of osteomyelitis in the jaw are determined?
Answer. Determination of these two types are made on the basis of specifiity of their causative microorganisms. On this basis osteomyelitis may be of two types—specific osteomyelitis and non-specifi osteomyelitis.
Question 136. What are the different types of chronic specifi osteomyelitis of the jaw?
Answer.
- Tuberculous osteomyelitis
- Syphilitic osteomyelitis
- Actinomycotic osteomyelitis.
Question 137. What are the different types of chronic non-specifi osteomyelitis of the jaw?
Answer.
- Chronic intramedullary osteomyelitis
- Chronic focal sclerosing osteomyelitis
- Chronic diffuse sclerosing osteomyelitis
- Chronic osteomyelitis with proliferative periosteitis
- Chronic subperiosteal osteomyelitis
- Chronic periosteitis.
Question 138. What are the etiological factors of jaw bone osteomyelitis?
Answer.
- Direct spread of infection from dental pulp into the jawbone
- Spread of infection from pre-existing suppurative odontogenic lesions e.g. periapical abscess, granuloma or cyst; periodontal abscess and pericoronitis etc.
- Infection following removal of tooth without proper asepsis and antibiotic coverage
- Compound fracture of the jaw bone with exposure of bone outside the skin or mucosa
- Gunshot injuries in the jaw with soft tissue laceration and exposure of bone
- Spread of microorganisms from overlying soft tissue (skin or mucosa) infections
- Post-radiation secondary infection
- Infection to the pre-existing bony diseases, e.g. Paget’s disease of bone, firous
- dysplasia and osteopetrosis, etc
- Phosphorus poisoning
- Anachoretic infections
- Idiopathic factors.
Question 138a. What is the most common cause of acute osteomyelitis of the jaw?
Answer. Odontogenic infections.
Question 139. Name the local factors, which can favor the development of osteomyelitis of jaw.
Answer.
- Anatomical site of the jaw bone
- Pre-existing bone diseases
- Radiation injury in the bone.
Question 140. How the anatomy of jaw inflences the development of osteomyelitis?
Answer. Local anatomy of the bone is important in the development of osteomyelitis, for example the mandibular bone has poor blood supply in comparison to that of the maxilla and it also has a more compact bony pattern; for these reasons osteomyelitis occurs far more commonly in mandible as compared to maxilla.
Question 141. Name the common pre-existing bone diseases, from which osteomyelitis maydevelop.
Answer. Paget’s disease of bone, firous dysplasia, jaw cysts, osteopetrosis, etc.
Question 142. Why osteomyelitis of the jaw bone may occur following radiotherapy to the head and neck area?
Answer. Radiotherapy to the head and neck area often produces obliterative endarteritis to the blood vessels inside jaw bone; which results in an impaired blood supply to the jaw bone itself and thereby increases the possibility of osteomyelitis, whenever there is any infection.
Question 143. Name the systemic factors which might predispose to the development of osteomyelitis.
Answer.
- Malnutrition and chronic alcoholism
- Drug addiction
- Anemia, especially sickle cell anemia
- Diabetes (poorly controlled)
- Acute leukemia
- Agranulocytosis
- Syphilis
- Measles and typhoid fever
- HIV infection and AIDS
- Extremes of age
- Urinary tract infections.
Question 144. Name the aerobic organisms, which might cause osteomyelitis.
Answer.
- Staphylococcus aureus
- Haemolytic streptococcus
Question 145. Name the anaerobic organisms which might cause osteomyelitis.
Answer.
- Bacteroides
- Anaerobic streptococcus.
Question 145a. Among all types, the commonest bacteria responsible for acute osteomyelitis of jaw is?
Answer. Staphylococcus aureus.
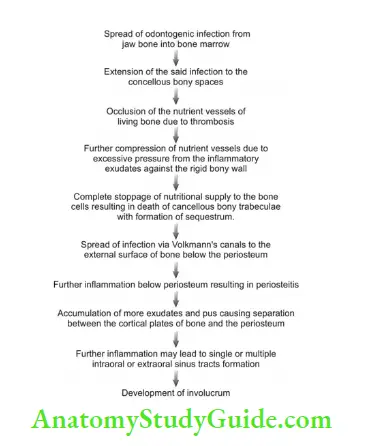
Question 146. Describe the basic steps in the pathogenesis of osteomyelitis.
Answer.
- Spread of Infection from the periapical lesions or infected pulp or other foci enters into bone marrow and the concellous bony spaces
- Occlusion of nutrient vessels of the living bone by the formation of thrombus (the thrombus consists of dead or viable neutrophils, microorganisms and necrotic tissue debris, etc.
- Formation of thrombus and excessive pressure from the inflmmatory exudates against the rigid bony wall cause total disruption of nutrition supply to the bone cells
- This causes death of cancellous bony trabeculae with formation of sequestrum
- The infection then spreads via the Volkmann’s canals in the cortical plates and reaches to the external surface of bone below the periosteum and cause periosteitis
- Further extension of the inflmmation may lead to single or multiple sinus tracts formation
- Repair of bone begins after the acute phase is over
- If a small piece of sequestrum gets surrounded by new bone and entrapped within the bone mass, it is called the ‘involucrum’.
Question 146a.How a bone reacts to osteomyelitis?
Answer.
- The bone may be completely necrosed or dead (formation of sequestrum)
- Bone may be severely inflmed but not dead
- Bone may cause synthesis of new, highly mineralized bone in the medullary area in response to inflmmation (focal and diffuse sclerosing osteomyelitis)
- There may be new bone formation of the outer cortex (Garre’s osteomyelitis).
Question 147. What is sequestrum?
Answer. Sequestrum is a dead or necrotic bony fragment, which forms due to severe inflmmation and thrombosis of the nutrient vessels, resulting in complete stoppage of nutritional supply to the bone cells during osteomyelitis.
Question 147a. What happens to the sequestrum in course of the disease?
Answer. Necrotic bone fragment or sequestrum often exfoliates spontaneously from the bony wound.
Question 148. What is an involucrum?
Answer. Although sequestrum is a dead piece of bone, few osteoblasts still survive inside it and when the acute phase of osteomyelitis is over, a new layer of bone may form over the sequestrum, which completely surrounds it; this enclosed sequestrum within normal bone is called ‘involucrum’.
Question 149.Under what circumstances necrosis of cortical plate of bone occurs in osteomyelitis?
Answer. In severe osteomyelitis huge accumulation of inflmmatory exudates causes elevation of periosteum from the cortical surface of bone; the separation between cortical plate and periosteum may result in necrosis of the cortical bone as it gets its main blood supply from the periosteum itself.
Question 150. What is acute suppurative osteomyelitis?
Answer. Acute suppurative osteomyelitis is a serious type of diffusely spreading acute inflmmation of the bone characterized by extensive tissue necrosis.
Question 151. Under what circumstances acute suppurative osteomyelitis occur?
Answer. Acute suppurative osteomyelitis is characterized by unilateral destruction or necrosis of bone with no scope for bone regeneration; it is possible only when virulence of the causative microorganisms overpowers the host’s local and systemic defence mechanism.
Question 152. Under what circumstances non-suppurative osteomyelitis can develop?
Answer. During osteomyelitis when a balance exists between the virulence of the pathogenic organism and the host’s local and systemic defense mechanism; then non-suppurative types of lesion generally develop.
Question 153. What is the common age of occurrence of acute osteomyelitis and why?
Answer. Acute osteomyelitis usually occurs after 30 years of age; as there is more probability for development of systemic diseases from this age onwards and moreover there is also decreased bony resistance to infection (due to reduced vascularity).
Question 154. Name the microorganisms often responsible for acute osteomyelitis.
Answer. Staphylococci and Streptococci are the predominant organisms for acute suppurative osteomyelitis of the jaw. However, Actinomyces israelii, Pneumococci, Prevotella, Porphyromonous and Bacteroides can also cause the disease.
Question 155. In acute osteomyelitis, which jaw is more often affected and why?
Answer. The mandible is involved more often than the maxilla as it has a limited blood supply and it is a dense bone with thicker cortical plates.
Question 156. In acute osteomyelitis, how size of the lesions vary in maxilla and mandible?
Answer. Mandibular lesions are usually diffuse in nature and are large; while the maxillary lesions are mostly well-localized and small in size.
Question 157. From which pre-existing diseases, acute osteomyelitis of maxilla develops among infants?
Answer. Maxillary lesions of acute osteomyelitis are rare and are seen in infants or neonates following birth injuries or severe otitis media, etc
Question 158. Describe the clinical features of acute suppurative osteomyelitis.
Answer. Acute suppurative osteomyelitis often clinically presents the following features:
Severe throbbing, deep seated pain and diffuse large swelling of the jaw and related soft tissues
- Loosening and soreness of the regional teeth with diffiulty in taking food Pain, swelling and erythema in the overlying gingiva; occasional discharge of pus from gingival crevice
- Excessive salivation and bad breath
- Enlarged and tendered lymph nodes
- Anesthesia and paresthesia of the jaw
- Patients are slightly febrile and often have fever, malaise, anorexia and vomiting, etc.
Question 159. Why patients feel diffiulty in mouth opening in acute suppurative osteomyelitis?
Answer. There is often excessive muscle edema in the jaws, which may cause diffiulty in mouth opening and swallowing.
Question 160. What is pathologic fracture of bone? Does it occur in osteomyelitis?
Answer. When a bone is weakened by an underlying pathology it may get fractured even under normal functional pressure; this type of fracture is called pathological fracture.
Pathological fracture of bone is very common in case of osteomyelitis.
Question 161.What are the initial radiographic changes in the bone in acute suppurative osteomyelitis?
Answer. In the initial stages of the disease when bone destruction is yet to occur, no noticeable radiographic changes can be observed in the jaw.
Question161a.Can radiographic evidence of bone destruction be seen in acute osteomyelitis?
Answer. No.
Question 162.In acute suppurative osteomyelitis, from when the radiographic bony changes are detectable?
Answer. Radiographic changes become more apparent in about ten days time since the onset of the disease.
Question 163.Describe the radiographic features of acute suppurative osteomyelitis.
Answer. Radiographic features of acute suppurative osteomyelitis include large areas of radiolucencies in the jaw bone, with ill-defied, moth-eaten margins.
Question 164. How the sequestrum appears radiographically in acute suppurative osteomyelitis?
Answer. Sequestra are frequently seen as multiple radiopaque foci of diminished radiodensity within the lesion.
Question 165. How the involucrum appears radiographically in acute suppurative osteomyelitis?
Answer. The involucrum radiographically appears as a gray shadow on the outer surface of the cortical plate.
Question 166.What is a Brodie’s abscess?
Answer. When a suppurative infection in the bone becomes walled off or surrounded from all sides by healthy tissue; it may lead to a localized intra-bony abscess formation; which is called Brodie’s abscess. The abscess may remain within the bone as a sterile lesion or it may act as persistent source of infection.
Question 167. Name the lesions, which look similar to primary acute suppurative osteomyelitis.
Answer.
- Metastatic tumor in the bone with secondary infection
- Primary intra-alveolar carcinoma
- Primary mesenchymal malignant neoplasm
- Primary lymphoma of bone.
Question 168. Name the different treatment modalities of acute suppurative osteomyelitis.
Answer. Incision and drainage, antibiotic therapy, removal of the sequestrum and elimination of the primary source of infection, e.g. offending tooth.
Question 169. What are the clinical features of chronic suppurative osteomyelitis?
Answer. Patients with this condition often complains of mild, dull pain in the jaw for several weeks, which had started following an acute tooth abscess, tooth fracture or extraction.
Jaw swelling and sequestrum formation are also common.
Question 170.Describe the different types of radiographic images produced by chronic osteomyelitis.
Answer. Chronic osteomyelitis may present at least four different types of images:
- An ill-defied radiolucency in the bone with ragged borders
- A radiolucency with multiple radiopaque foci within it; the later structures represent sequestra
- A dense zone of radiopacity with faint radiolucency at the margin
- A “salt and pepper” radiographic effect in the bone.
Question 171. What is chronic focal sclerosing osteomyelitis?
Answer. Chronic focal sclerosing osteomyelitis is a rare non-suppurative inflmmatory condition of bone characterized by sclerotic bone formation around the root apex of a non-vital tooth.
Question 172. What is the other name of chronic focal sclerosing osteomyelitis?
Answer.Condensing osteitis.
Question 173.Chronic focal sclerosing osteomyelitis may occur under what circumstances?
Answer. This is the type of osteomyelitis, which develops if the following conditions prevail:
- The inflmmation in the bone must be chronic in nature
- Tissue resistance against infection must be very high
- Virulence of the infective organisms causing osteomyelitis should be low.
Question 174. What is osteosclerosis?
Answer. In chronic focal sclerosing osteomyelitis a low-grade inflmmation in the jaw bone causes stimulation of the osteoblast cells, which results in the formation of dense trabecular bone in the area and this process is known as osteosclerosis.
Question 174a. Name the disease which has features similar to focal sclerosing osteomyelitis.
Answer. Focal periapical osteopetrosis.
Question 175. Name the common causes of chronic focal sclerosing osteomyelitis.
Answer.
- Chronic pulpitis
- Traumatic malocclusion.
Question 176. Name the tooth, which is most frequently involved in chronic focal sclerosing osteomyelitis.
Answer. Mandibular fist molar.
Question 177. What is the common age of occurrence of chronic focal sclerosing osteomyelitis?
Answer. The disease frequently develops in children or young adults before the age of 20 years.
Question 178. What is the clinical feature of chronic focal sclerosing osteomyelitis?
Answer. The condition is mostly asymptomatic and there is no expansion of bone, the only presenting sign is a large carious tooth in the jaw with occasional mild pain.
Question 179.Describe the radiographic feature of chronic focal sclerosing osteomyelitis.
Answer. It presents a well-circumscribed radiopaque mass around the root apex of a nonvital tooth with no radiolucent border around the lesion.
Question 180.What is a bone scar?
Answer. A residual area of chronic focal sclerosing osteomyelitis in the jaw that is seen after resolution of the inflmmatory focus is known as bone scar.
Question 181.How can the chronic focal sclerosing osteomyelitis can be distinguished from benign cementoblastoma radiographically?
Answer. In case of chronic focal sclerosing osteomyelitis root tips of the involved tooth are usually visible within the radiopaque lesion but it is not so in case of benign cementoblastoma.
Question 181a.How focal periapical osteopetrosis can be distinguished radiographically from periapical cyst?
Answer. Focal periapical osteopetrosis produces a radiopacity at the root apex of tooth while periapical cyst produces a small area of radiolucency at the root apex.
Question 181b.A painless tooth with large caries, having a radiopaque lesion at the root apex; the condition is likely to be?
Answer. Chronic focal sclerosing osteomyelitis.
Question 182.Describe the histological features of chronic focal sclerosing osteomyelitis.
Answer. There is usually presence of a dense mass of sclerotic bone in the lesion with little or no interstitial marrow tissue.
Question 182a.In focal sclerosing osteomyelitis, the sclerotic bone is attached to the root apex or not?
Answer. The bone is not attached to the root apex.
Question 183.Name the lesions, which are often confused with chronic focal sclerosing osteomyelitis.
Answer. Mature cementoma, peripheral osteoma, complex odontoma and cementoblastoma.
Question 184.Why biopsy is mandatory in case of chronic focal sclerosing osteomyelitis?
Answer. Biopsy may be necessary to rule out metastatic tumor of the jaw.
Question 185. What is the treatment of chronic focal sclerosing osteomyelitis.
Answer. The affected tooth should be treated endodontically or it should be removed.
Question 186.In chronic focal sclerosing osteomyelitis, is it necessary to remove the sclerotic bone at the root apex?
Answer. No treatment is required for the apical sclerotic bone.
Question 187. What is diffuse sclerosing osteomyelitis?
Answer. Diffuse sclerosing osteomyelitis is a proliferative reaction of bone in response to lowgrade inflmmation and it typically involves a wide area.
Question 188.Which jaw bone is frequently affected in case of diffuse sclerosing osteomyelitis?
Answer. It is mainly involves the mandible especially in edentulous areas.
Question 189. Diffuse sclerosing osteomyelitis of the jaw often develops in response to which lesions?
Answer. It mainly occurs in response to wide spread periodontal or periapical inflmmations.
Question 190.Name the bacterias responsible for the development of diffuse sclerosing osteomyelitis.
Answer. Propionibacterium acnes and Peptostreptococcus intermedium.
Question 191. Diffuse sclerosing osteomyelitis generally occurs in which age group?
Answer. It usually occurs in elderly people.
Question 192. What is the usual clinical appearance of diffuse sclerosing osteomyelitis?
Answer. The disease is usually asymptomatic but sometimes patients may complain of a vague pain in the jaw (predominantly mandible) affecting a wide area with foul taste in the mouth.
Question 193. What is SAPHO syndrome?
Answer. SAPHO syndrome is a special pathologic entity characterized by the following-
- Chronic multifocal osteomyelitis of bone
- Hyperostosis and osteitis of the bone
- Negative bacterial culture
- No response with antibiotic therapy.
Question 194. What is radiographic appearance of diffuse sclerosing osteomyelitis?
Answer. The disease produces the typical ‘cotton–wool’ radiopacities in the jaw with well demarcated border.
Question 195. Diffuse sclerosing osteomyelitis microscopically presents what type of features?
Answer. Microscopically the disease shows formation of dense irregular bone within a hypocellular firous stroma. Bony trabeculae often reveal multiple reversal lines and resting lines.
Question 196. Name the lesions included in the differential diagnosis of diffuse sclerosing osteomyelitis.
Answer. Paget’s disease of bone:
- Osteopetrosis
- Cementomas
- Gardner’s syndrome
- Late stage of firous dysplasia.
Question 197. What is the treatment of diffuse sclerosing osteomyelitis?
Answer. No treatment is required as the disease is often asymptomatic.
Question 198. What is Garre’s osteomyelitis?
Answer. Garre’s osteomyelitis represents a reactive periosteal osteogenesis in response to lowgrade infection or trauma.
Question 199. How the term Garre’s osteomyelitis is coined?
Answer. The condition is named after German physician C. Garre, who fist authentically reported about the diseses in 1893.
Question 200. What is the special characteristic of Garre’s osteomyelitis?
Answer. The most important characteristic of the disease is focal gross thickening of the involved bone due to sub-periosteal new bone deposition (duplication of the cortex).
Question 201. Name the conditions which predispose the development of Garre’s osteomyelitis
Answer.
- Chronic periapical abscess, infected granuloma or cyst
- Perifollicular infection in an erupting tooth or impacted tooth
- Chronic periodontal infection
- Chronic trauma in the jaw bone.
Question 202. How Garre’s osteomyelitis occurs?
Answer. Generally in Garre’s osteomyelitis, a low-grade chronic inflmmation spreads through the cortical bone of the jaw and then it initiates a proliferative reaction in the periosteum, leading to sub-periosteal new bone formations.
Question 203. Why Garre’s osteomyelitis type sub-periosteal osteogenesis does not occur in acute suppurative osteomyelitis?
Answer. Because acute infection in suppurative osteomyelitis does not permit suffiient time for the bone cells to undergo any sub-periosteal osteogenesis as may be seen in Garre’s osteomyelitis.
Question 204. What is the mean age of occurrence of Garre’s osteomyelitis?
Answer. About 13 years.
Question 205. In Garre’s osteomyelitis, which jaw is more often affected?
Answer. Mandible is commonly involved in Garre’s osteomyelitis in its posterior part.
Question 206. Describe the clinical features of Garre’s osteomyelitis.
Answer.
Presence of a grossly carious, non-vital tooth in the jaw (mostly lower fist permanent molar) with low grade periapical inflmmation
- There is a very characteristic thickening and swelling of the affected bone with little or no pain
- Occasionally slight tenderness or a vague pain may be felt in the affected area of bone
- The overlying skin and oral mucosa appears normal.
Question 207. Describe the radiographic appearance of Garre’s osteomyelitis.
Answer. Garre’s osteomyelitis radiographically presents the following features:
- A central radiolucent jaw lesion with few radiopaque foci within it.
- Several concentric layers of reactive bone formation below the periosteum over the cortex producing the typical onion skin appearance.
Question 208. Name the common diseases associated with periosteal new bone formations in the jaw.
Answer.
- Osteomyelitis
- Trauma
- Cyst
- Malignancy
- Fracture of bone.
Question 209. What is ‘duplication’ of the cortex in Garre’s osteomyelitis?
Answer. The standard occlusal radiograph in this disease reveals a smooth, convex, bony overgrowth on the outer cortex of the jaw; which is often called ‘duplication’ of the cortex.
Question 210. Name the lesions which look similar to Garre’s osteomyelitis.
Answer.
- Ossifying firoma
- Immature firous dysplasia
- Ewing’s sarcoma
- Osteoblastic osteosarcoma
- Fracture callus
- Metastatic tumor of the jaw bone
- Pulse granuloma.
Question 211. What is pulse granuloma of the jaw?
Answer. It is a granulomatous reaction produced by foreign materials introduced into the living body tissue and is characterized by chronic inflmmation and subsequent formation of hyaline eosinophilic structure in the tissue with few giant cells.
Question 212. Why the condition is called pulse granuloma?
Answer. The term pulse granuloma has been coined since vegetable materials especially pulses are believed to cause this disease more often than others.
Question 213.In case of pulse granuloma, how the foreign materials get inside the living tissue?
Answer. The foreign materials may enter into the oral tissue via the following routes:
- Extraction sockets
- Surgical flps
- Open root canals
- Ulcerations in the oral mucosa.
Question 214. What are endodontic-periodontic lesions?
Answer. Sometimes infection from dental pulp may spread into the periodontal tissues and likewise infection in the periodontal tissue may spread to involve the dental pulp secondarily. Therefore co-existence of these dual infections are called endodonticperiodontic lesions.
Question 215. Name the factors which may facilitate the development of endodontic periodontic lesions.
Answer.
- Dynamic nature of both pulpal and periodontal diseases
- Communication between pulp and periodontium via accessory canals or the apical foramen.
Question 216. Classify endodontic-periodontic lesions.
Answer. According to Simon, the endodontic–periodontic lesions are classifid into four types:
- Primary endodontic lesions
- Primary endodontic lesions with secondary periodontal involvement
- Primary periodontal lesion with secondary endodontic involvement
- True combined lesion.
Question 217. What are primary endodontic lesions?
Answer. Here the infection originates in the pulp, which later on extends via the accessory canals or apical canals into the periodontium and produces a resultant inflmmation there.
Question 218. What is the treatment of primary endodontic lesions?
Answer. Endodontic treatment alone usually solves the problem.
Question 219. What are primary endodontic lesions with secondary periodontal involvement?
Answer. These lesions occur if prompt endodontic therapy is not done in a situation, where the pulpal infection has already spread into the periodontium; as a result periodontal tissue breakdown occurs.
Question 220. What is the treatment of primary endodontic lesions with secondary periodontal involvement?
Answer. Treatment in such cases will involve both endodontic as well as the periodontal therapy.
Question 221. What is primary periodontal lesion with secondary endodontic involvement?
Answer. These lesions occur if microorganisms causing periodontal disease enter into the dental pulp via accessory root canal or via apical foramen and produce pulpal infections through these retrograde pathways.
Question 222. What is the treatment of primary periodontal lesion with secondary endodontic involvement?
Answer. Treatment will be both periodontal and endodontic in such cases.
Question 223. What are true combined endodontic-periodontic diseases?
Answer. Periodontal and endodontic lesions may arise independently in a tooth and at some stage both these lesions may coalesce together to establish a true combined endodonticperiodontic disease.
Question 224. What is treatment of true combined endodontic-periodontic diseases?
Answer. Dual therapy for both lesions reQuestionuired but prognosis is mostly poor.
Leave a Reply