Drugs Acting On The Kidney
Diuretics
Question 1. Classify diuretics. Discuss the pharmacology of loop diuretics. Describe the mechanism of action, therapeutic uses, and adverse effects of loop diuretics/furosemide.
Answer:
A Diuretic is an agent which increases the excretion of solute and water.
Classification of Diuretics:
- High efficacy diuretics: Furosemide, bumetanide, piretanide, ethacrynic acid, torsemide.
- Moderate efficacy diuretics:
- Thiazides (benzothiadiazines): Chlorothiazide, hydrochlorothiazide, polythiazide,cyclopenthiazide.
- Thiazide-related agents: Chlorthalidone, clopamide, indapamide, metolazone, xipamide.
- Low efficacy diuretics:
- Potassium-sparing diuretics: Triamterene, amiloride, spironolactone, eplerenone.
- Carbonic anhydrase inhibitors: Acetazolamide.
- Osmotic diuretics: Mannitol, urea, glycerol.
- Newer agents:
- Vasopressin antagonists: Conivaptan, tolvaptan, lixivaptan.
- SGLT2 inhibitors: Dapagliflozin, canagliflozin.
Read And Learn More: Pharmacology Question And Answers
Loop diuretics/furosemide:
Loop diuretics are highly efficacious diuretics and furosemide, a sulfonamide is the most popular and powerful loop diuretic.
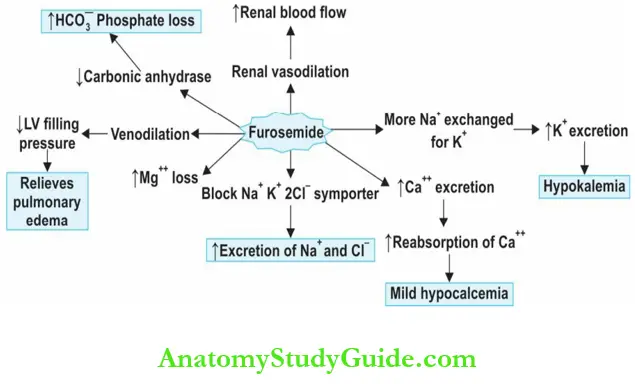
Mechanism of action of loop diuretics:
Frusemide inhibits NaCl– reabsorption in the thick ascending limb of the loop of Henle (LH) by blocking the Na+ K+ 2Cl– symporter.
It increases the excretion of Na+ and Cl– in the urine. Because a large amount of NaCl– is reabsorbed in this segment, loop diuretics excrete a large amount of Na+ → highly efficacious diuretics. Diuretic response increases with dose → high ceiling of effect.

Other Actions of Diuretics:
- Loop diuretics ↑ ↑ excretion of K+, Ca++, and Mg++ (but no hypocalcemia because Ca++ gets reabsorbed in the distal tubule).
- ↑ ↑ uric acid reabsorption in the proximal tubule.
- Cause vasodilation in renal vasculature → increase renal blood flow and renin release.
- Induce that the synthesis of PGE2 (through COX-2) → inhibit sodium reabsorption in the loop diuresis.
- Weak carbonic anhydrase inhibitor, → ↑ excretion of HCO3 and phosphate.
- IV frusemide causes vasodilatation → reduces left ventricular filling pressure → thus relieves pulmonary congestion in acute CHF and in pulmonary edema even before the onset of diuresis
Pharmacokinetics:
Loop diuretics are rapidly and almost completely absorbed orally. IV furosemide acts in 2–5 minutes and on oral use, it takes 20–40 minutes. Duration of action is 2–4 hours. Loop diuretics are extensively and firmly bound to plasma proteins furosemide.
Dose: 20–80 mg OD in the morning
Bumetanide is 40 times more potent and is better tolerated because the adverse effects like hypokalemia, ototoxicity, hyperglycemia and hyperuricemia are milder but may cause myopathy.
Torsemide is more potent, longer acting, given once a day and dose reduced in liver failure.
Adverse Effects of Diuretics:
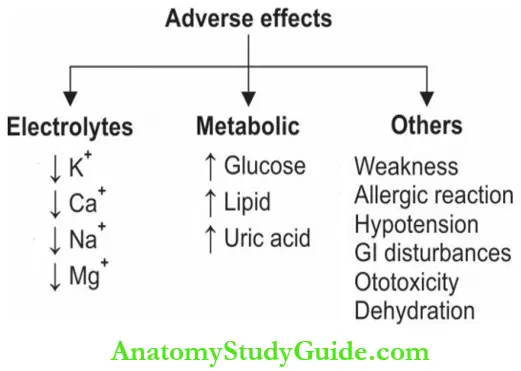
- Hypokalemia and metabolic alkalosis: Hypokalemia is dose-dependent and causes irritability, drowsiness, confusion, dizziness, muscle weakness and cardiac arrhythmias. This can be prevented and corrected by:
- High dietary intake of K+,
- Oral KCl supplements or
- By adding a K+ sparing diuretic.
- Hyponatremia, dehydration, hypovolemia and hypotension: Due to salt and water loss.
- Hypocalcemia and hypomagnesemia: Seen after prolonged use.
- Hyperuricemia: Increased uric acid absorption → may precipitate acute gout on long-term use. Allopurinol may be needed.
- Ototoxicity: Loop diuretics cause hearing loss by a toxic effect on the hair cells in the internal ear (more with ethacrynic acid) and is dose-related. Tinnitus and vertigo may occur.
- Hyperglycemia and hyperlipidemia are mild.
- GIT disturbances like nausea, vomiting and diarrhea → common with ethacrynic acid.
- Allergic reactions like skin rashes (most are sulfonamide derivatives).
- Weakness, fatigue, dizziness and muscle cramps are mostly due to hypokalaemia.

Uses of Diuretics:
- Edema is Highly effective in edema of all origins like cardiac, hepatic and renal edema.
- Chronic CCF Loop diuretics reduce venous and pulmonary congestion.
- Acute renal failure: ↑ Urine output and K+ excretion. In chronic renal failure, large doses are needed.
- Cerebral edema Frusemide is an alternative to
- Acute pulmonary edema and acute LVF are Quickly relieved by IV frusemide due to its immediate vasodilator effect and then by diuretic action.
- Forced diuresis In the treatment of poisoning
- Poisoning due to drugs like barbiturates and salicylates → frusemide + IV fluids.
- Anion overdosage (fluoride, iodide, and bromide)—respond to furosemide along with saline infusion (to avoid hyponatremia and dehydration).
- Hypertension with renal impairment may be treated with loop diuretics for short periods.
- Acute hypercalcemia and hyperkalemia—IV frusemide to increase excretion of Ca++ and K+ but Na+ and Cl– should be replaced to avoid hyponatremia and hypochloremia.
- Blood transfusion to avoid volume overload, when a large volume of blood is transfused.

Thiazide Diuretics
Question 2. Discuss briefly the pharmacology of thiazide diuretics. Why thiazides are contraindicated in diabetes mellitus. The rationale for the use of thiazides in diabetes insipidus/rationale for the use of thiazides in lithium-induced nephrogenic diabetes insipidus.
Answser:
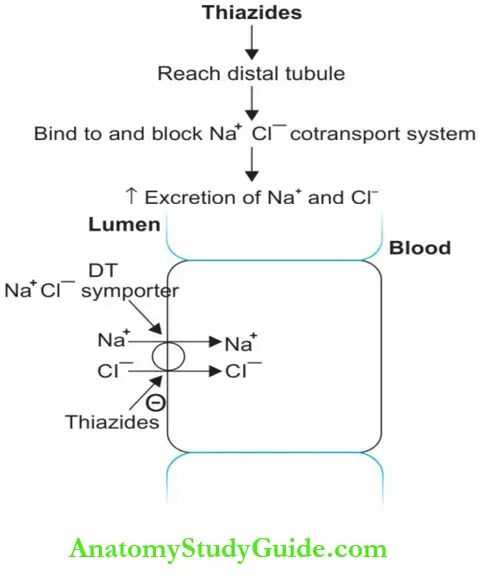
All thiazides have a sulfonamide group.
Actions and mechanism of action: Thiazides have moderate efficacy as diuretics because 90% of the filtered sodium is already reabsorbed before reaching the distal tubule. They block the Na+ Cl– symporter in the early DT and thus increase the excretion of Na+ and Cl–
Other Actions of Thiazide Diuretics:
- Also inhibit carbonic anhydrase activity and ↑ HCO–3 loss.
- ↑ ↑ excretion of Mg+ and K+.
- ↓ ↓ excretion of Ca++ and uric acid (resulting in hypercalcemia)
Paradoxical action of thiazides: Paradoxical action of thiazides in diabetes insipidus → ↓ glomerular filtration → ↓ urine output.
Pharmacokinetics: Thiazides are well-absorbed orally, rapid acting (~act within 60 minutes) duration varies from 6–48 hours. They are excreted by the kidney.
Adverse Effects of Thiazide Diuretics:
- Hypokalemia.
- Metabolic alkalosis, hyperuricemia, hypovolemia, hypotension, dehydration, hyponatremia, hypomagnesemia, hypochloremia, hypercalcemia, and hyperlipidemia are similar to that seen with loop diuretics.
- Hyperglycemia induced by thiazides may precipitate diabetes mellitus on long-term use.
- Thiazides ↑ k+ loss → hypokalemia → ↓ insulin release → hyperglycemia
- Correction of hypokalemia reduces hyperglycemia.
- Impotence in men.
- Weakness, fatigue, anorexia, gastrointestinal disturbances and allergic reactions like rashes and photosensitivity.
Uses of Thiazide Diuretics:
- Hypertension: Thiazides are the first-line drugs.
- Congestive heart failure: Useful in mild to moderate CHF.
- Edema: Metolazone may be combined with loop diuretics in severe refractory edema. Other
thiazides are not very effective - Renal stones and hypercalciuria: Thiazides reduce calcium excretion.
- Diabetes insipidus: Thiazides benefit such patients by reducing plasma volume, GFR and thereby reducing urine output by a paradoxical effect.
Thiazide diuretics can reduce polyuria and polydipsia in both central and nephrogenic diabetes insipidus (NDI). Thiazides (specifically hydrochlorothiazide) are effective in lithium-induced nephrogenic diabetes insipidus (DI).

In NDI, hydrochlorothiazide causes:
- Increased osmolality in the medulla
- Partial correction of lithium-induced reduction in aquaporin expression
- Increased expression of sodium transporters in distal and collecting tubules.
- Thus dilute urine production can be reduced in NDI. Dietary sodium restriction will potentiate the effects.
Potassium Sparing Diuretics
Question 3. Write short note on K+ sparing diuretics.
Answer:
May act in two ways:
- Aldosterone antagonist—spironolactone
- Directly acting—triamterene, amiloride.
Spironolactone of K+ sparing diuretics:
- Aldosterone activates the mineralocorticoid receptor and regulates sodium absorption and potassium secretion in the collecting tubule and ducts.
- It increases Na+ reabsorption.
- Spironolactone an aldosterone antagonist is structurally similar to aldosterone → binds to the mineralocorticoid receptors on DT and CD and competitively inhibits the action of aldosterone.
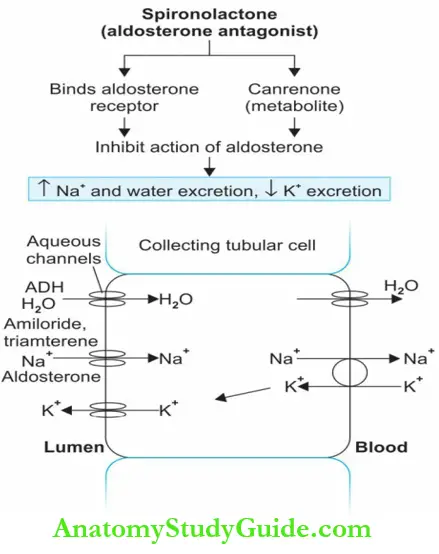
Because a major amount of Na+ is already reabsorbed in the proximal parts, spironolactone has low efficacy:
- It also reduces K+ loss due to other diuretics.
- It increases the excretion of Ca++ by a direct action on renal tubules.
- Spironolactone is given as a microfine powder to increase bioavailability (75%). It has a slow onset of action.
- A metabolite canrenone has a long t½ (18 hours) hence, long-acting.
Eplerenone of K+ sparing diuretics:
Eplerenone an analog of spironolactone has greater selectivity for mineralocorticoid receptors and the hormonal adverse effects are milder. It is used in the treatment of hypertension and in heart failure in place of spironolactone but is expensive.
Amiloride and triamterene of K+ sparing diuretics:
- Amiloride and triamterene are directly acting agents—they block the Na+ transport through the sodium channels in the luminal membrane of DCT and CD.
- Since K+ secretion is dependent on Na+ entry, these drugs reduce K+ excretion.
- Drug Interactions
- ACE inhibitors + K+ sparing diuretics → hyperkalemia.
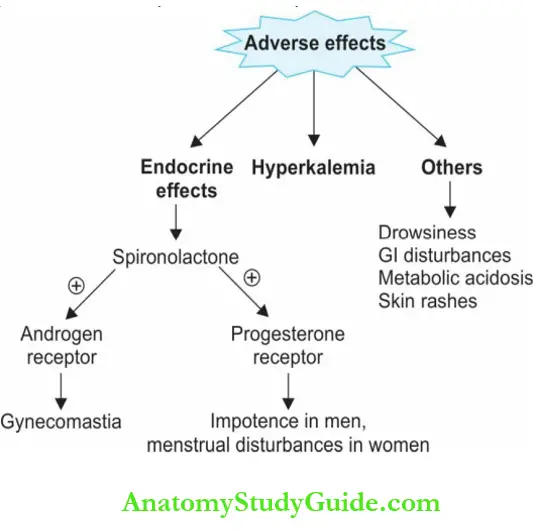
Adverse Effects of K+ sparing diuretics:
- Endocrine side effects: Gynecomastia, impotence in men, hirsutism and menstrual irregularities in women with large doses of spironolactone. It binds to the androgen and progesterone receptors and also interferes with steroidogenesis.
- Hyperkalemia: Seen particularly in patients with renal insufficiency or on other hyperkalemia drugs.
- Drowsiness, metabolic acidosis, GI disturbances, and skin rashes can occur.
Uses of K+ sparing diuretics:
- With thiazides or loop diuretics to prevent potassium loss.
- Edema: In cirrhosis, and renal edema whereb aldosterone levels may be high.
- Hypertension: Along with thiazides to avoid hypokalemia and for additive effect.
- CCF: Moderate to severe heart failure along with frusemide
- Spironolactone for primary or secondary aldosteronism.
Carbonic Anhydrase Inhibitors
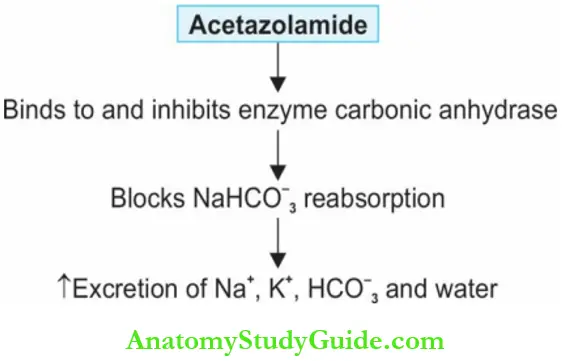
Carbonic anhydrase catalyzes the formation of carbonic acid from H2O and CO2 which spontaneously ionizes to H+ and HCO–3 This HCO–3 combines with Na+ and is reabsorbed.
Acetazolamide:
- Acetazolamide is a carbonic anhydrase inhibitor → blocks sodium bicarbonate reabsorption and causes HCO–3 diuresis
![]()
![]()
- Carbonic anhydrase is present in the nephron, ciliary body of the eyes, gastric mucosa, pancreas, and other sites.
- Acetazolamide increases the excretion of sodium, potassium, bicarbonate, and water. The loss of bicarbonate leads to metabolic acidosis
Other actions of Carbonic Anhydrase Inhibitors:
- Eye: Acetazolamide → ↓ formation of aqueous humor → ↓ IOP.
- Brain: Bicarbonate is secreted into CSF and carbonic anhydrase inhibition reduces the formation of CSF.
Adverse Effects of Carbonic Anhydrase Inhibitors:
- Metabolic Acidosis due to HCO3 loss.
- Renal stones Ca++ is lost with HCO3 → hypercalciuria → form renal stones.
- Hypokalemia, drowsiness, and allergic reactions can occur.
Uses of Carbonic Anhydrase Inhibitors:
- Glaucoma: ↓ IOP acetazolamide, methazolamide—given orally. Brinzolamide and dorzolamide are available as eye drops and are better tolerated.
- For alkalinization of urine in over dosage of acidic drugs. Also, HCO–3
- increases uric acid and cysteine excretion → these are soluble in alkaline urine.
- Metabolic alkalosis: Responds as acetazolamide increases HCO–3 excretion.
- Hyperphosphatemia: Increases urinary phosphate excretion.
- Mountain sickness: In mountain climbers who rapidly climb great heights, severe pulmonary edema and cerebral edema may occur particularly in unacclimatized persons.
Initial symptoms of mountain sickness include headache, dizziness, nausea, and weakness. Acetazolamide may relieve symptoms by reducing the formation as well as the pH of CSF it can also be used for prophylaxis.

Osmotic Diuretics
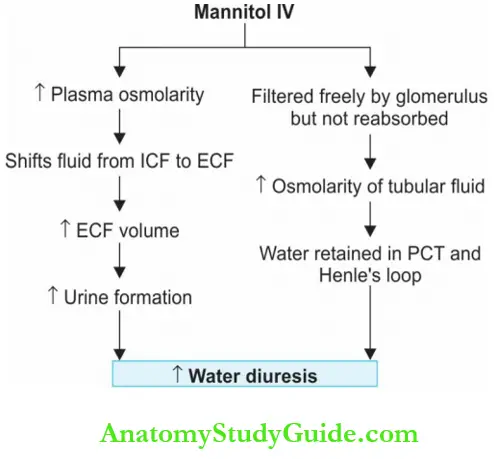
Mannitol is a pharmacologically inert substance not absorbed orally → causes osmotic diarrhea. When given IV, mannitol gets filtered by the glomerulus but is not reabsorbed.
- Water is retained in the proximal tubule and descending limb of Henle’s loop by osmotic effect resulting in water diuresis (aquaretic). Mannitol also opposes the action of ADH in the collecting tubule.
- There is increased urinary excretion of Na+, K+, Ca++, Mg+, HCO–3, and PO4.
Adverse effects of Osmotic Diuretics:
Dehydration, ECF volume expansion (water is extracted from cells due to osmotic effect), hyponatremia (due to volume expansion), headache, nausea, vomiting, and allergic reactions.
Contraindication: Osmotic diuretics → expand plasma volume → worsen pulmonary edema
Uses of Osmotic Diuretics:
- To maintain urine volume and prevent renal shutdown in conditions like massive hemolysis, rhabdomyolysis, shock and severe trauma → IV mannitol prevents renal failure.
- However, in patients who have already gone into renal failure, mannitol can be dangerous since it can cause pulmonary edema and may precipitate heart failure due to volume expansion.
- Glaucoma → ↓ intraocular pressure in acute glaucoma.
- Head injury → ↓ intracranial pressure due to osmotic activity.
- Dose: 1–2 g/kg IV infusion.
Glycerol (glycerine) is effective orally—reduces intraocular and intracranial pressure. It can be used topically to relieve edema including corneal edema.
Vasopressin Antagonists
- A new class of drugs, vasopressin receptor antagonists viz conivaptan, tolvaptan and lixivaptan (the vaptans) induce diuresis.
- They are vasopressin receptor (V2), antagonists, inhibit the effects of ADH in the collecting tubule, and cause free water diuresis.
- Conivaptan is given parenterally while tolvaptan and lixivaptan are effective orally.
Uses of Vasopressin Antagonists:
- Vaptans enhance water excretion and correct hyponatremia in the syndrome of inappropriate Adh Secretion (SIADH).
Diuretic Resistance
- The inability to reduce plasma sodium levels even after using a full therapeutic dose of diuretics is diuretic resistance.
- Causes Higher sodium intake, reduced absorption of the diuretic, and inadequate renal blood flow as in CCF leading to lower amounts of it reaching the kidney.
Chronic renal failure and nephrotic syndrome patients may also be refractory to diuretics. Diuretic resistance may be managed with:
- Upgradation from a lower to a higher efficacy diuretic.
- Using a suitable combination.
- Reduced salt intake helps.
- Timing the diuretic intake 30–60 minutes before food also works because renal diuretic levels would be high enough to avoid salt retention.
- NSAIDs cause water retention leading to diuretic resistance hence they should be avoided.
Drug Interactions with Diuretics:
Question 4. What drug interactions are expected with diuretics?
Answer:
1. Frusemide + warfarin/highly protein-bound drugs → compete for protein binding
2. Avoid ototoxic drugs like aminoglycosides with loop diuretics.
- Aminoglycosides + loop diuretics → ↑ ototoxicity.
3. Diuretics → ↓ K+ → digoxin toxicity
4. NSAIDs + diuretics:
- NSAIDs → salt and water retention → ↓ diuretic effect
- Could be because of inhibition of PG synthesis in the kidneys.
5. Diuretics + Lithium
- Diuretics ↓ Li excretion → Toxicity
6. Avoid oral K+ supplements with K+ sparing diuretics because together they can cause → severe hyperkalemia.
- ACEI + K+ sparing diuretics → Hyperkalemia
Contraindications for Diuretics:
- Toxemia of pregnancy: Diuresis induced in pregnancy results in reduced fetal circulation which may result in fetal death. Hence diuretics contraindicated.
- Hepatic cirrhosis: Diuretics can cause mental disturbances and hepatic coma in cirrhosis patients. The combined effect of raised NH3 levels, alkalosis and hypokalemia may be responsible for this. Hence diuretics should be used carefully in them.
Combination of Diuretics:
- Diuretics combined in refractory edema
- Diuretics acting at different sites may be combined
- Thiazide + loop diuretic → Synergistic effect
- However, they could result in severe dehydration and electrolyte disturbances → should be used for short periods only.
- A potassium sparing diuretic + thiazide/loop diuretic → Better diuresis (additive
effect)Counter hypokalemia.
Antidiuretics
Question 5. Write short note on vasopressin/ADH/antidiuretics.
Answer:
Antidiuretics are drugs that reduce urine volume.
These include:
- Antidiuretic hormone (vasopressin)
- Vasopressin analogs
- Desmopressin
- Terlipressin
- Lypressin
- Felypressin
- Thiazide diuretics
Antidiuretic hormone (ADH):
It is synthesized in the supraoptic and paraventricular nuclei of the hypothalamus, transported along the hypothalami-hypophyseal tract to the posterior pituitary, and is stored there. ADH is released in response to two stimuli—dehydration and a rise in plasma osmolarity.
Vasopressin receptors of antidiuretics:
V1 and V2 are both GPCRs. V1 receptors mediate vasoconstriction, while V2 receptors mediate water retention in the collecting duct. V1 receptors are of two subtypes

Actions of antidiuretics:
- ADH increases water reabsorption by acting on the collecting duct. It activates the V2 receptors present in the collecting duct and increases the water permeability of these cells.
- ADH causes vasoconstriction and raises BP-mediated V1 receptors.
- All vasculature including cutaneous, mesenteric, celiac, and coronary are constricted.
- It also acts on other smooth muscles to increase constriction and peristalsis in the gut (can cause cramps). Vasopressin contracts the uterus. It is given parenterally.
Adverse effects of antidiuretics:
Intranasally ADH can cause nasal irritation, allergy, rhinitis, and atrophy of the nasal mucosa. Other effects include nausea, abdominal cramps (due to contractions of the uterus), and backache.
Vasopressin Analogs:
- Desmopressin: Desmopressin is selective for V2 receptors and is longer-acting and more potent than vasopressin. Given orally, bioavailability is 1–2% and intranasally bioavailability is 10–20%. Desmopressin is used for conditions where V2 agonist is required.
- Terlipressin: Terlipressin is a prodrug of vasopressin and is longer-acting—used for bleeding esophageal varices. Felypressin is used with local anesthetics to prolong the duration of action because of its vasoconstrictor properties. Lypressin is another analog used in place of ADH.
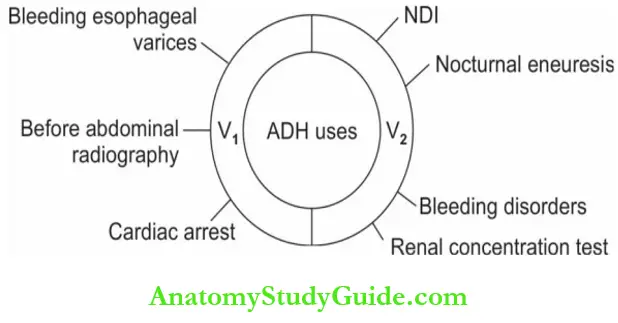
Uses of vasopressin and its analogs: Mediated through V1 receptors
- Bleeding esophageal varices ADH constricts mesenteric blood vessels and may help.
- Analogs like desmopressin, terlipressin, and lypressin can be used.
- Before abdominal radiography, ADH promotes the expulsion of gases from the bowel.
- Cardiac arrest IV vasopressin has been useful in reverting asystolic cardiac arrest. Mediated through V2 receptors
- Nephrogenic diabetes insipidus (NDI) is treated with desmopressin—may require lifelong treatment.
- Nocturnal enuresis Desmopressin given along with restriction of fluid intake at bedtime controls bed-wetting.
- It should be given only for short periods. Blood pressure should be monitored.
- Bleeding disorders Hemophilia and von Willebrand’s disease ADH may release factor 8 and prevent bleeding.
- Renal concentration tests A small dose of desmopressin (2 µg) can increase the urine
concentration to a great extent if the kidneys are normal.
Leave a Reply