Enamel Oral Histology Notes
Enamel
Enamel is the hardest calcified tissue in the body that forms a protective covering of the entire surface of the crown of the tooth. It is the one among the three calcified tissues of the tooth, which includes dentin and cementum.
Table of Contents
Salient Features Of Enamel
- Enamel is ectodermal in origin.
- It is laid down by ameloblasts, which are lost once the tooth erupts. Thus, enamel is not formed throughout life and cannot be regenerated.
- It is avascular and not innervated.
- As enamel is highly inorganic, the mineral content is lost after decalcification.
- The features of enamel can be appreciated in ground sections.
Read And Learn More: Oral Histology Notes
Physical Properties Of Enamel
- Colour:
- It ranges from yellowish white to greyish white.
- The crystals in enamel exhibit birefringence, thus refracting light differently in different directions.
- Young enamel – The light entering the enamel undergoes total internal reflection and no wavelength is absorbed, thus giving the low translucency and white appearance.
- Older enamel – The translucency of enamel decreases with age. The underlying dentin gives the enamel a yellowish appearance.
- Incisal areas – It appears more translucent due to the enamel thinning down to a knife edge.
- Hardness:
- Enamel is the hardest calcified biological tissue.
- It is harder, denser and more porous at the surface. Hardness and density decrease on approaching the interior or the cervical margin.
- It has high-abrasion resistance, thus making it suitable for mastication. This property compensates for the inability of enamel to regenerate or undergo repair.
- Enamel is brittle and prone to fracture. The underlying dentin provides the support to the enamel by acting as a shock absorber and distributing the forces.
- Thickness:
- It varies in different teeth and on different surfaces.
- Cusps of molars and premolars: 2–2.5 mm, knife edge at the cervical margin.
- In maxillary molars: thicker on the lingual surfaces; in mandibular
molars: thicker on the buccal surfaces. This could a functional adaptation for mastication.
- Permeability:
- Enamel acts as a semipermeable membrane allowing passage of certain molecules.
- Specific gravity:
- The specific gravity of enamel is 2.8.
Chemical Properties Of Enamel
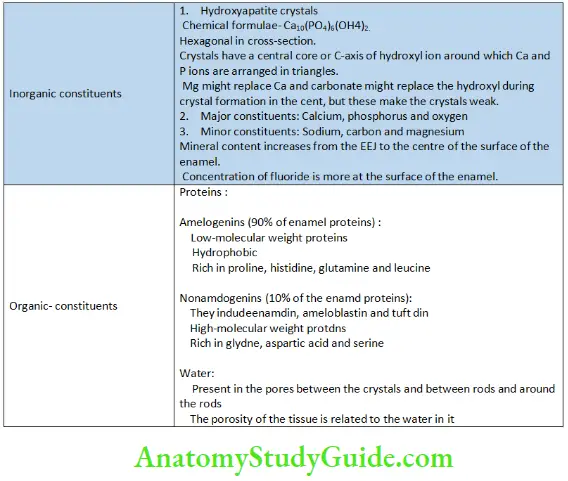
Organic and inorganic constituents of enamel:
Structure of enamel:
Enamel is a highly mineralized tissue. The minerals dissolve and the organic component of enamel is washed away when decalcified. The space occupied by mature enamel appears as an empty space when a decalcified section is observed under the microscope.
Chemical Content of Enamel by Volume and Weight
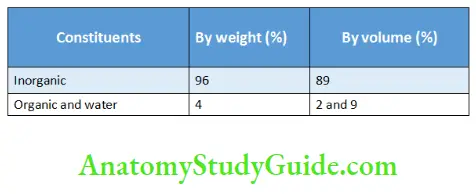
Enamel can be observed and studied using a ground section. A light microscope or a polarized microscope may be used and an electron microscope to study the ultrastructure. The organic and inorganic constituents are mentioned in Table
Organic and inorganic constituents of enamel
Enamel rods:
The fundamental unit of enamel is the enamel rods or enamel prisms. Enamel also comprises rod sheaths and inter-rod substance or interprismatic substance. Features of enamel rods
- Longitudinal sections: Enamel rods are cylindrical.
- Cross-section: There are three patterns of arrangements of the enamel prisms, which are described under the ultrastructure of enamel.
- Enamel rods are tortuous from the dentinoenamel junction (DEJ) to the surface.
- The length (2–2.5 mm) is greater than the thickness (5–6 microns) due to the wavy course and oblique arrangement.
- In the cusps: Rods are longer due to an increased thickness of enamel.
In the cervical areas: Rods are shorter. - Diameter of rods: It is more at the surface than at the DEJ in the ratio of 1:2.
- Rods have an arcade outline at the DEJ and a keyhole pattern at the surface (under the confocal laser scanning microscope).
- The rods are concave and the shallowest in the cervix and deepest at the incisal edge or the cusp tip.
- Rods allow light to pass through them.
- When the rods are cut transversely, they appear like fish scales
Note: Even though the enamel rods do have a regular geometry, the word enamel prism is accepted due to its popular use.
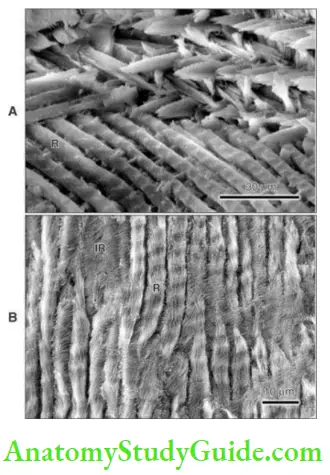
Ultrastructure of enamel:
Enamel rod or prism is the basic structural unit of enamel. One enamel rod is made up of several million crystallites that are packed into a thin, long rod of about 5– 6 µ in diameter and 2.5 mm in length. These rods run from the DEJ to the surface of the enamel.
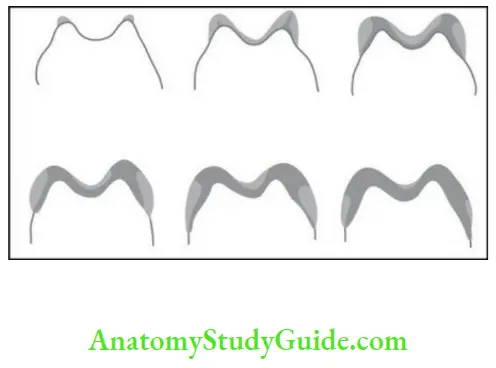
- The shape of the enamel prism in cross-section has three patterns.
- – Pattern I: Prisms are circular.
- – Pattern II: Prisms are arranged in parallel rows.
- – Pattern III: Prisms are aligned in staggered rows so that the tail of one prism is in between two heads in the next row leading to a key-hole appearance.
- The third pattern is the most common one.
- The enamel between the prisms is called the interprismatic enamel or the inter-rod enamel.
- In the type II pattern, the head and tail regions of the prism are clearly seen, as the crystals in the head of the prism are parallel to the long axis of the prism but deviate to about 65–70° in the tail. This change is gradual in a single prism and thus no clear divide is seen between the head and tail of the same prism; but the crystals in the tail of one prism show sudden divergence from the crystals of the
head of the adjacent prism. During histological sectioning of enamel, a variety of prism appearances are seen. Even though some of the areas are called interprismatic, they are actually the tail of prism from an adjacent row. The prismatic and the aprismatic enamels are actually continuous.
Cross-striations:
In longitudinal sections, the enamel rods are made up of segments that are separated by dark lines leading to a striated appearance. The lines are perpendicular to the long axis of the enamel rods.
Cross-striations Reason:
- The rods are segmented as the enamel is laid down in a rhythmic manner. The lines represent the diurnal pattern (every 24 hour) of formation of enamel.
- The segments are of 4 µ in length.
- Striations are more prominent in enamel. Which is not completely calcified.
- Recent studies suggest that variations in the organic matrix and the crystal orientation are the cause.
Direction of enamel rods:
The enamel rods are generally perpendicular to the dentin. The course of the rods varies in deciduous and permanent teeth.
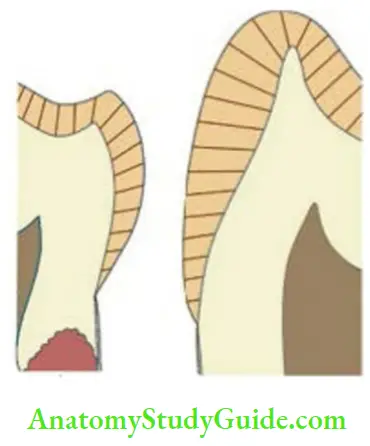
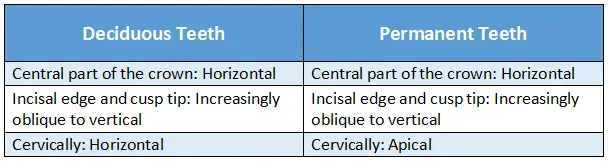
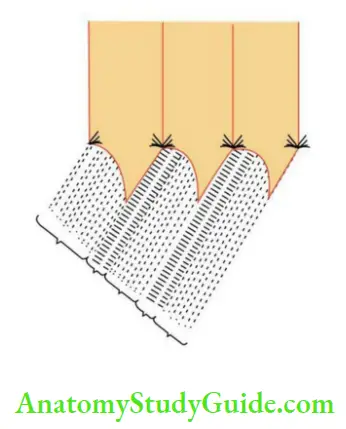
- The enamel rods converge in the developmental pits and fissures.
- The enamel rods show variations from the straight radial course:
- If the middle portion of the crown is sectioned as horizontal, the rods in adjacent sections bend in opposite directions. For example, rods in one disc starting from dentin in an oblique direction might bend to the left side but less sharply and in the adjacent disc might bend towards the right side.
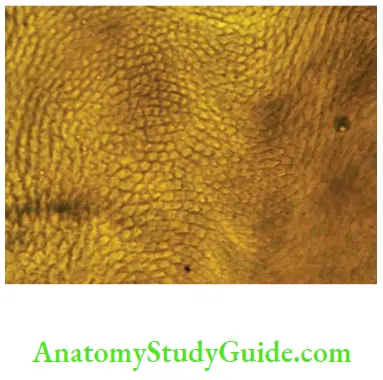
Gnarled Enamel
When a longitudinal section of a tooth is observed near the cusp tip and incisal edge, the bundles of enamel rods and adjacent enamel rods intertwine with each other irregularly. The arrangement of enamel rods appears more prominent and this optical phenomenon is called gnarled enamel
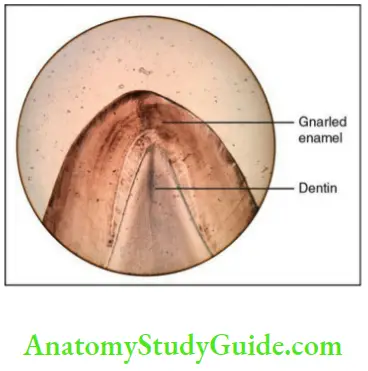
Gnarled Enamel Clinical significance:
It may be associated with greater strength of enamel and the ability to withstand masticatory forces.
Hunter–schreger bands:
Every 10–13 layers of enamel rods follow a particular direction, but blocks below and above follow paths in different directions. This change in the direction of enamel rods leads to a banding pattern called Hunter–Schreger bands.
Gnarled Enamel Reason
- Change in direction of the enamel rods
Extent
- They extend from the DEJ to a distance short of the outer surface of the enamel.
- Approximately, one-fourth of the outer surface of enamel is devoid of Hunter– Schreger band as all prisms run in the same direction.
Gnarled Enamel Appearance
- Alternate dark and white bands under oblique reflected light.
- Prisms that are cut longitudinally produce dark bands called diazones.
- Prisms that are cut transversely produce light bands called parazones.
- Angle between diazones and parazones is 40°.
Gnarled Enamel Clinical significance
- The change in the direction of enamel rods could be a functional adaptation making the enamel resistant to fracture under masticatory forces.
Incremental lines of retzius:
They are also called the striae ofRetzius.
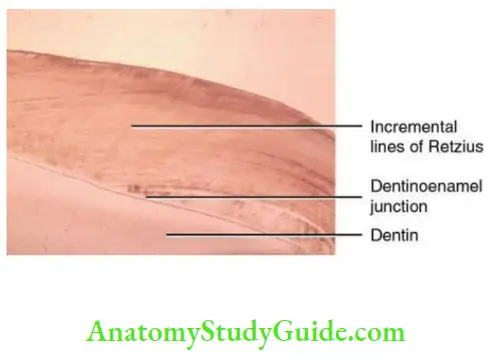
These are brownish bands seen in the ground sections representing the successive apposition of layers of enamel in the crown and reflecting the incremental pattern of
The lines could be due to
- Variation during the formation of enamel due to variations in mineralization such as hypomineralization and hypermineralization.
- Periodic bending of enamel rods.
- Variation in the inorganic or organic constituents in the region of the striae and thus can be considered as hypocalcified.
Gnarled Enamel Appearance
- In longitudinal sections: Appear as series of dark lines.
- In the cervical portion of the crown: Run obliquely.
- From the DEJ to the surface: Deviate occlusally.
- In transverse sections: Concentric.
- Middle part of the enamel: 7–10 cross-striations are seen between adjacent striae in an individual. The evenly spaced striae represent weekly deposition of enamel. The average distance between two cross-striations is 4 microns and thus the distance between enamel striae is 25–35 microns.
- Cervical enamel: The enamel is deposited slowly and the distance between the cross-striations is about 2 microns; the striae are thus 15–20 microns apart.
- Metabolic disturbance may cause accentuation of the striae.
- The striae that overlie the cusps and the incisal edges do not reach the surface unless there is a loss of enamel due to the way in which enamel is deposited.
Neonatal line (neonatal ring):
In the deciduous teeth and the permanent first molars, enamel is formed partly before and after birth. The line that separates the prenatal and postnatal enamel is the accentuated incremental line of Retzius, which is called the neonatal line.
- The line is due to the sudden change in the environment after birth.
- The prenatal enamel is better developed, as it develops with adequate supply of nutrients in an undisturbed environment in the fetus.
- Boys are considered to be dentally less matured than girls at the times of birth, as neonatal lines are absent in permanent first molars of boys.
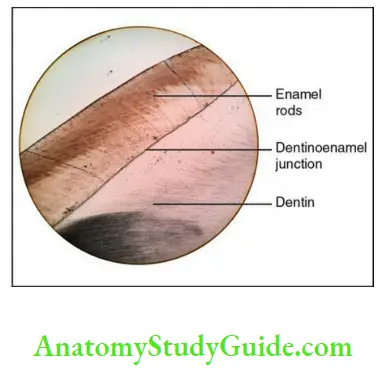
Dentinoenamel junction:
It is also called the enamel–dentin junction and amelodentinal junction.
The junction or the boundary between the enamel and dentin is called the
dentinoenamel junction (DEJ).
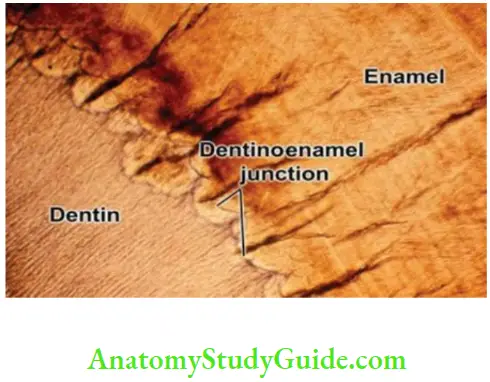
The junction assures the firm hold of the enamel onto dentin, which are two dissimilarly mineralized tissues. The DEJ must possess unique properties such as slowing down of crack propagation. It is less mineralized than enamel and dentin and formed before the development of the hard tissues. The crystals of enamel mix with that of the dentin at the DEJ. The DEJ is more prominent in the occlusal areas as the forces of mastication are greater in those areas.
Dentinoenamel Appearance: It is generally scalloped with the convexities towards the dentin.
Dentinoenamel Ultrastructure
- Three levels of features.
- Largest: Scalloping pattern, 25–100 microns, below the cusp tips and incisal edges.
- Second order: Smaller microscallops are 2–5 microns in size.
- Third nanostructural level: Yet to be fully determined; the initial crystals of enamel mingle with the fine ends of the collagen fibres of dentin.
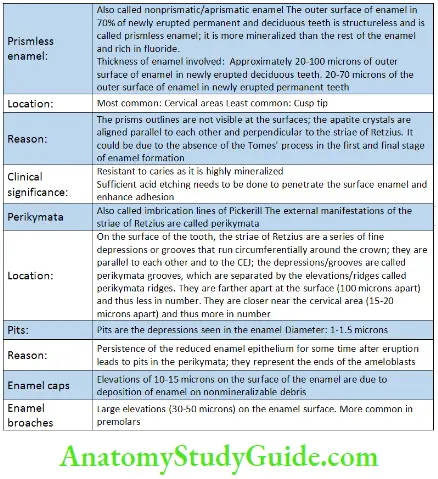
Surface Structures Of Enamel
- Prismless enamel
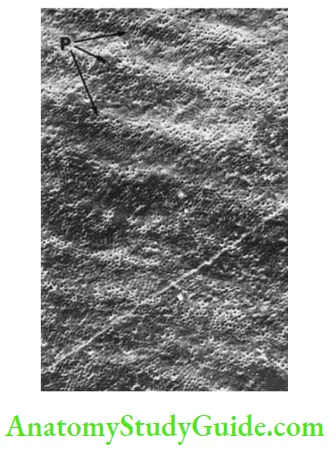
- Perikymata
- Pits
- Enamel caps
- Enamel broaches
- Enamel cracks
Surface Structures Of Enamel
Enamel Cuticle (Primary Enamel Cuticle/Nasmyth’s Membrane)
A delicate membrane that covers the crown of a newly erupted tooth is called the Nasmyth’s membrane. Once the crown is completely exposed in the mouth, the loosely attached reduced enamel epithelium covering is lost and the primary enamel cuticle is left behind.
Ultrastructural studies have revealed the presence of a basal lamina between the enamel surface and the reduced enamel epithelium. The basal lamina is secreted by the ameloblasts after the formation of enamel is complete. This basal lamina and the reduced enamel epithelium comprise the Nasmyth’s membrane.
Enamel Cuticle Function
- The enamel cuticle helps in protection of the enamel from resorption by the adjacent vascular tissue before the eruption of the tooth.
Pellicle/acquired pellicle:
Once the primary enamel cuticle is lost, an organic layer rich in salivary proteins is formed on the enamel surface immediately. This is called the acquired pellicle. When this pellicle becomes colonized by microorganisms, then it is bacterial plaque.
Enamel Tufts
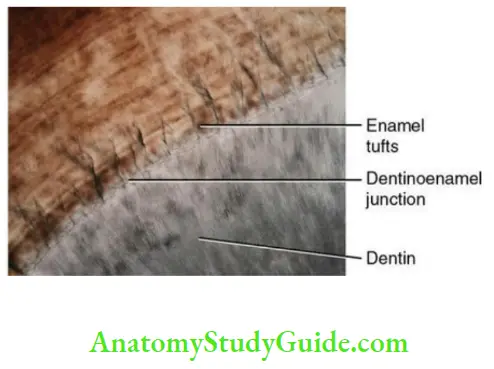
These are structures that resemble tufts of grass that arise from the DEJ and may extend for a short distance in the enamel. These tufts contain tuftelin, which is a nonamelogenin group protein.
Enamel Tufts Origin:
- Tufts comprise hypocalcified rods and interprismatic substance.
Enamel Tufts Appearance:
- The enamel tuft is a narrow, ribbon-like structure with its inner end arising at the DEJ and looking similar to a tuft of grass when viewed in thick ground sections under low magnification.
- Occur at every 100 microns along the DEJ.
- Abundant in transverse/horizontal sections.
- Rare in longitudinal sections.
Enamel Tufts Ultrastructure:
- SEM studies: Tufts are tubular structures with cross-striations.
- TEM studies: Tufts have plate-like structures in the centre originate from the superficial layer of dentin at the DEJ.
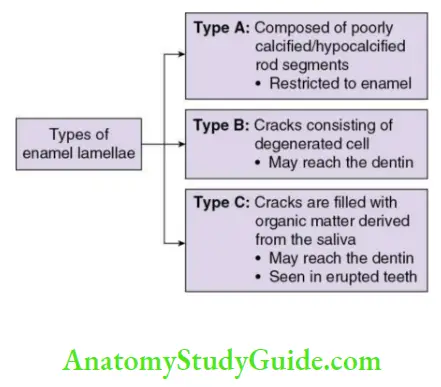
Enamel Lamellae
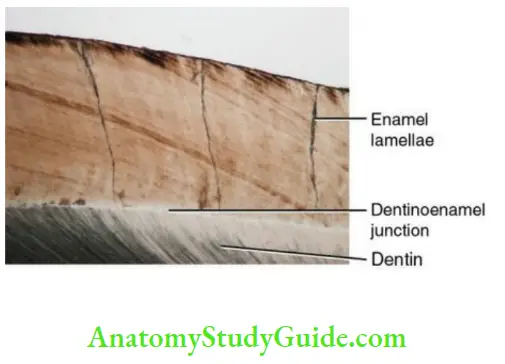
Enamel lamellae are thin, leaf-like or sheet-like structures that extend from the surface of the enamel to the DEJ.
Enamel Lamellae Origin:
- They are considered to be structural defects and may develop in areas of tension. The rods passing in these areas may not calcify completely. There are different types of enamel lamellae
- Severe disturbance may lead to the development of a crack, which may be filled with surrounding cells (if in an unerupted tooth) or by organic substances (if in a tooth after eruption).
Enamel Lamellae Appearance:
- Leaf-like structures in the enamel best seen in transverse sections.
Enamel LamellaeLocation:
- Tip of the crown to the cervical region.
Enamel Lamellae Clinical significance
- Enamel lamellae may be weak spots that act as a route of entry for bacteria that initiate caries.
- Enamel lamella may be mistakenly identified as cracks in ground sections. Decalcification of the ground section helps in distinguishing between cracks and lamellae. Cracks disappear after decalcification whereas lamellae persist.
Enamel Spindles And Odontoblastic Processes:
The odontoblastic processes cross the DEJ into the enamel and are referred to as enamel spindles. The spindles originate from the odontoblastic processes and extend into the enamel epithelium during the early stages of enamel development and lie between the ameloblasts. The spindles are almost perpendicular to the dentin.
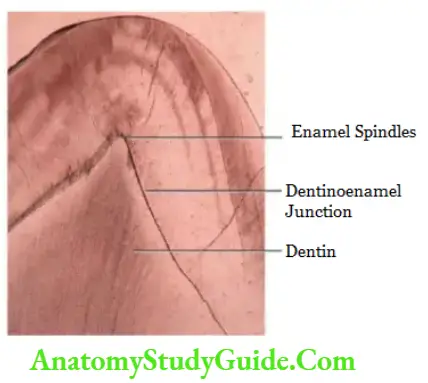
Studies have suggested that they might be dentinal collagen or the remnants of dead odontoblasts.
Enamel Appearance:
- Look like needle-like structures at the DEJ best seen in longitudinal sections.
Enamel Location:
- Beneath the cusp tips.
Enamel Ultrastructure:
TEM: Small needle-like structures 70 microns in length, 2 microns in diameter and
5 nm in width or granular and/or amorphous material.
Changes In And Around The Enamel Organ Before The Formation Of Enamel
Before the formation of enamel and dentin, the enamel organ comprises four layers:
Outer enamel epithelium (OEE)
Stellate reticulum
Stratum intermedium
Inner enamel epithelium (IEE)
The demarcation between the IEE and the dental papilla is the future DEJ, which determines the occlusal and the incisal part of the crown. The IEE and the OEE form the cervical loop at the border of the wide opening of the enamel organ. The IEE and OEE are separated from each other by the stratum intermedium and stratum reticulum.
Outer enamel epithelium:
The OEE consists of a single layer of cuboidal cells and is separated from the dental sac by a basement membrane. The regular arrangement of cells of the OEE is maintained only in the cervical parts of the enamel organ before the formation of the hard tissues. The cells of the OEE in the maximum convexity of the organ become irregular and appear similar to the cells of the stellate reticulum. The capillaries from the connective tissue protrude into the enamel organ and also indent the stellate reticulum before the formation of the enamel. The capillaries help in providing the nutrition to the cells of the IEE for the formation of enamel.
Stellate reticulum:
The cells of the stellate reticulum are star-shaped and have long processes. The cells are separated by intercellular spaces filled with intercellular substances. These cells are connected to adjacent cells and the cells of the OEE and stratum intermedium by
desmosomes. The stellate reticulum acts as a shock absorber against physical forces that might disturb the developing DEJ. This layer also allows a limited inflow of nutrition from the vessels to the formative cells and is thus reduced in thickness once the first layers of enamel and dentin are laid down.
Stratum intermedium:
These two to three layers of cells between the IEE and the stellate reticulum are flat to cuboidal in shape. This layer is known to have a role in the formation of enamel either by the control of diffusion of fluid in and out of the ameloblasts or by the formation of
the necessary components for enamel formation such as enzymes. The cells of this layer continue to divide by mitosis even after the cells of the IEE stop dividing.
Inner enamel epithelium:
The cells of the inner enamel epithelium that are derived from the basal layer of the oral epithelium become columnar before the formation of enamel and differentiate into ameloblasts that lay down the matrix of the enamel. The differentiation begins in the cusp tips and incisally and then proceeds to the area of the cervical loop. The changes that take place in the shape and structure of the cells are described under the life cycle of the ameloblasts.
Cervical loop:
The IEE and OEE are continuous at the free border of the enamel organ and form the cervical loop. The cuboidal cells in this zone increase in length. The cells in this area form the Hertwig’s epithelial root sheath once the crown is formed.
Amelogenesis
The process of formation of enamel is called amelogenesis. There are two steps in the formation of enamel:
- Organic matrix formation.
- Maturation and mineralization of the matrix.
Organic matrix formation:
- Once a small amount of dentin is deposited, the ameloblasts lose the projections and lay down islands of enamel matrix along the predentin.
- Amelogenin:
- It is a major component of proteins in the enamel matrix.
- Majority of it is removed during maturations. Amelogenin helps in maintaining the space between crystals.
- Ameloblastin and enamelin:
- They help in nucleation and crystal growth.
- Tuftelin:
- It is localized to the DEJ and Helps in cell signaling.
- Amelotin:
- Helps in enamel formation.
- Dentin sialoprotein and dentin phosphoproteins:
- Transiently expressed by the ameloblasts.
Tomes’ process:
- In the beginning of the secretory phase, the ameloblasts become long columnar cells with their nuclei away from the forming enamel. After the initial thin layer of aprismatic enamel is laid down, a cone-shaped process known as the Tomes’ process develops at the distal end of the ameloblast. This process is responsible for the prismatic structure of the enamel.
- The ameloblasts are attached to each other at the distal ends by a terminal bar apparatus, which separates the Tomes’ process from the cell proper.
- The Tomes’ process contains the secretory granules with the organic matrix of the enamel within it. The contents of the vesicle are released into the extracellular space at the distal end and between the ameloblasts. The ameloblasts move away from the dentinal surface after the secretion of the enamel matrix.
- Crystals of hydroxyapatite appear as soon as the organic matrix is deposited. The initial crystals are thin and smaller than in mature enamel. The crystallites are aligned at right angles to the distal surface of the ameloblasts and appear flat and hexagonal in cross-section. The crystals grow in length and remain at right angles to the ameloblasts and parallel to adjacent crystals. The crystals that
elongate around the tip of the Tomes’ process form the core of the prism and the ones where the ameloblasts are joined with each other form the boundary of the prism. A clear demarcation is seen between the core of the prism and the boundary. The crystals of the core of the prism are parallel to the long axis of the prism, and the crystals of the boundary of the prism deviate by 40–65°. Thus, four ameloblasts contribute to form one prism and each ameloblast is involved in the development of four prisms. Thus, the number of ameloblasts and the prisms are the same. One ameloblast contributes to the bulk of the head of each rod and three others form the tail of each rod. - The enamel prisms elongate in an incremental manner and each daily increment of enamel leads to a cross-striation. Every 7th day’s cross striation is the prominent striation that leads to enamel striae. When these striae end on the enamel surface, they are called perikymata.
Maturation And Mineralization
The change of enamel into its final form is called maturation. During this process, the crystals grow in width and thickness with concomitant decrease in the intercrystal space.
- Maturation starts from the tip of the crown and proceeds cervically and begins at the dentinal end of the enamel rods. Thus, the maturation of each rod is from the depth to the surface and from the cusp tip or incisal edge towards cervically. Maturation continues in the inner matrix as initial mineralization continues on the outer newly formed matrix.
- Water and degraded enamel proteins are removed and calcium, phosphate and carbonate ions are added by the ameloblasts.
- There is loss of the Tomes’ and decrease in the content of the organelle. The distal end of the ameloblast develops a ruffled end where the rest of the organelle congregate. This morphology is in alternation with the smooth-end ameloblast where the striated border is absent. This is called modulation, which occurs five to seven times. Modulation indicates alternate phases of resorption and secretion. These changes in the ameloblasts could be due to
- Movement of the calcium ions across the ruffled and smooth end.
- Local change in the pH alternating between physiologically normal and mildly acidic pH.
Mineralization
Multiple sources of calcium lead to the mineralization of the enamel matrix. The two sources of calcium are as follows:
1. Through the enamel organ by active transport thorough the plasma membrane of the ameloblast.
2. Passive flow of calcium ion from high concentration in the plasma to lower concentration in the enamel matrix.
- The first formed enamel at the DEJ is aprismatic and not well organized compared to the rest of the bulk of enamel in terms of the size of the crystals and morphology.
- The growth of crystals and the nucleation may be due to tuftelin and cross-over of the initial nucleation from the dentin across the DEJ.
- Amelogenins assemble between the first formed crystallites. The initial crystallites form as a precipitate from the matrix, which is supersaturated by hydroxyapatite. The crystallites continue to grow in length.
- Rate of enamel formation: 4 µ per day
- Enamel forms faster in permanent teeth. The size of the crystals increases after eruption due to the exchange of ions with saliva.
Uniqueness of amelogenesis:
- The secretory cell here is an epithelial cell. All other hard tissue–secretory cells are ectomesenchymal in origin.
- Mineralization of the matrix is by noncollagenous proteins, whereas collagen plays a major role in other hard tissues.
- Enamel matrix has no collagen, but collagen is a major component in the matrix of other hard tissues.
- The enamel matrix is partially mineralized, but the matrix of other hard tissues is not mineralized. Thus enamel does not contain a distinct organic phase such as predentin, cementoid or osteoid.
- As the ameloblasts undergo apoptosis after the formation of enamel, enamel is not formed throughout life, but other hard tissues are formed throughout life.
Enamel Clinical Considerations
- Enamel hypoplasia and hypocalcification:
- Enamel hypoplasia: It is characterized by pitting, furrowing and sometimes complete absence of enamel.
- Enamel hypocalcification: It manifests as chalky or opaque areas on the surface of the enamel.
Enamel Clinical Considerations Reason:
- Disturbance in matrix formation leads to defects in the enamel and thus enamel hypoplasia.
- Disturbance in maturation leads to deficiency of mineral content and thus enamel hypocalcification.
Enamel Clinical Considerations Cause:
- Systemic
- Local
- Hereditary
- Systemic
- Hypoplasia due to systemic causes is called chronologic hypoplasia. The hypoplasia occurs in areas where enamel was formed during the
systemic disturbance. The hypoplasia is restricted to a smaller area as
enamel is formed over a long period of time and the disturbance lasts for a shorter duration. - If the disturbance is of a short duration, then only those ameloblasts
forming the enamel at that time are affected and thus a narrow
hypoplastic zone is seen. - If the interruption in enamel formation occurs multiple times, then
multiple areas of hypoplasia are seen. - The incisors, canines and the first molars are most often affected if systemic causes of hypoplasia are active during the first year of life in most of the cases.
For example, mottled enamel
-
- Due to high fluoride concentration in water when drinking water contains more than 1 part of fluoride per 1 ppm of water.
- Local factors causing hypoplasia:
- Only one tooth may be affected.
- The cause could be infection of the pulp and periapical tissues of the deciduous tooth leading to disturbance in the enamel formation of the successor.
- Hereditary type of hypoplasia:
- Due to generalized disturbance of ameloblasts.
- Entire enamel of all the teeth in both the dentitions is affected.
- Enamel is thin and may not be seen on the radiograph.
- Crowns appear yellowish brown, smooth with the shape of a jacket crown.
- Hereditary type of hypocalcification:
- Enamel is formed in normal quantity but fails to mature.
- Enamel appears dull and opaque.
- The enamel might be peeled due to mastication leading to a rough irregular surface of enamel.
- Once the enamel is lost, the tooth becomes sensitive due to the exposure of dentin.
- Discolouration of teeth
- It is mainly due to the administration of tetracycline during childhood. The discolouration is due to its accumulation in dentin, but a little might be deposited in the enamel.
Enamel Synopsis
- Enamel is the hardest calcified tissue in the body that forms a protective covering of the entire surface of the crown of the tooth.
- Enamel is ectodermal in origin.
- Enamel is formed by ameloblasts, which are lost once the tooth erupts. Thus, enamel is not formed throughout life and cannot regenerate.
- Its colour ranges from yellowish white to greyish white.
- Enamel is the hardest calcified biological tissue.
- Its thickness varies in different teeth and on different surfaces.
- The fundamental unit of enamel is the enamel rod or enamel prism. Enamel also comprises rod sheaths and inter-rod substance or interprismatic substance.
- Enamel rod or prism is the basic structural unit of enamel. One enamel rod is made up of several million crystallites that are packed into a thin long rod of about 5–6 µ in diameter and 2.5 mm in length. These rods run from the DEJ to the surface of the enamel.
- In longitudinal sections, the enamel rods are made up of segments, which are separated by dark lines leading to a striated appearance. The lines are perpendicular to the long axis of the enamel rods.
- The enamel rods are generally perpendicular to the dentin. The course of the rods varies in deciduous and permanent teeth.
- When a longitudinal section of a tooth is observed near the cusp tip and incisal edge, the bundles of enamel rods and adjacent enamel rods intertwine with each other irregularly. The arrangement of enamel rods appears more prominent and this optical phenomenon is called gnarled enamel.
- Every 10–13 layers of enamel rods follow a particular direction but blocks below and above follow paths in different directions. This change in the direction of enamel rods leads to a banding pattern called Hunter–Schreger bands.
- Striae of Retzius are brownish bands seen in the ground sections representing the successive apposition of layers of enamel in the crown and reflecting the incremental pattern of enamel formation.
- The junction or the boundary between the enamel and dentin is called the DEJ. The junction assures the firm hold of enamel onto dentin, which are two dissimilarly mineralized tissues.
- A delicate membrane that covers the crown of a newly erupted tooth is called the Nasmyth’s membrane. Once the crown is completely exposed in the mouth, the loosely attached reduced enamel epithelium covering it is lost and the primary enamel cuticle is left behind.
- Enamel tufts are structures that resemble tufts of grass that arise from the DEJ and may extend for a short distance in the enamel. These tufts contain tuftelin, which is a nonamelogenin group protein.
- Enamel lamellae are thin, leaf-like or sheet-like structures that extend from the surface of the enamel to the DEJ. They are considered to be structural defects and may develop in areas of tension.
- Enamel spindles are odontoblastic processes cross the DEJ into the enamel and are referred to as enamel spindles.
- The life cycle of an ameloblast can be divided into the following six stages based on the function: Morphogenic, organizing, formative, maturative, protective and desmolytic.
- Amelogenesis occurs in two stages, which is organic matrix formation and maturation and mineralization of the matrix.
Leave a Reply