Endodontic Failures And Retreatment Notes
Many studies have been conducted to determine the success and failures of endodontic treatments. Properly executed root canal treatment has shown success in > 95% of the cases.
Table of Contents
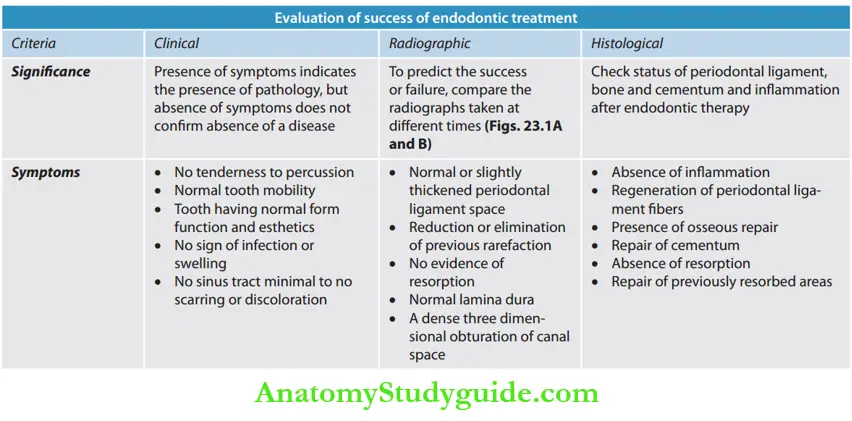
Endodontic failure cannot be subscribed to any particular criteria of evaluation; instead success or failure following endodontic therapy could be evaluated from a combination of various criteria like clinical, histopathological, and radiographical criteria.
Read And Learn More: Endodontics Notes
Definitions related to endodontic treatment outcome
- Healed: Both clinical and radiographic presentations are normal.
- Healing: It is a dynamic process, reduced radiolucency combined with normal clinical presentation.
- Disease: No change or increase in radiolucency, clinical signs may or may not be present or vice versa.
Evaluation Of Success Of Endodontic Treatment
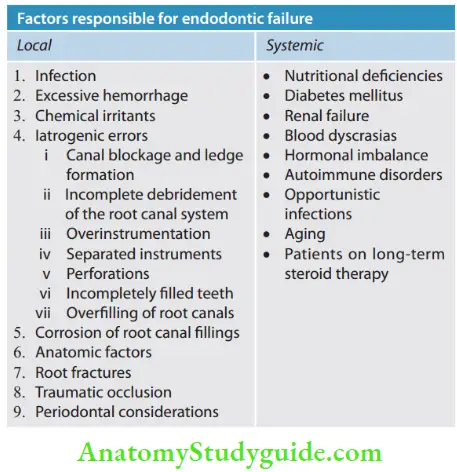

Local Factors Causing Endodontic Failures
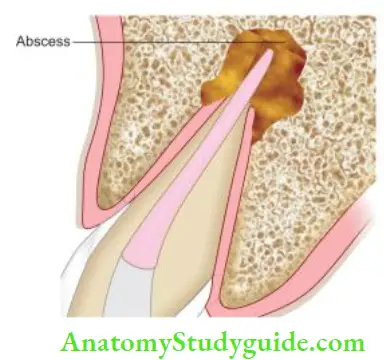
- Infection
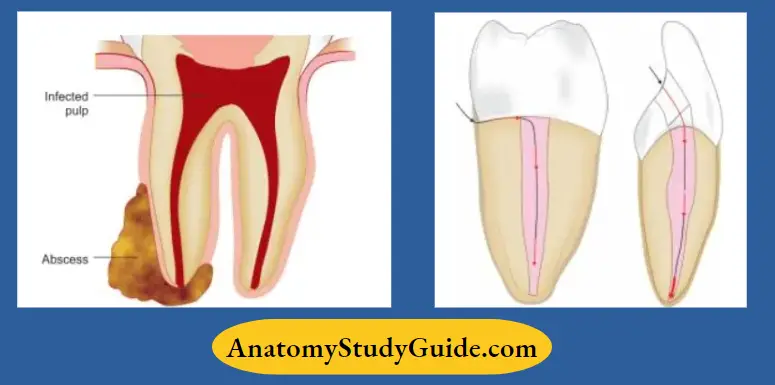
- If the infected tissue is present, then the host-parasite relationship, the virulence of microorganisms, and the ability of infected tissues to heal in the presence of microorganisms are the main factors which influence the repair of periapical tissues following endodontic therapy
- If an apical seal or coronal restorations are not optimal, reinfection of a root canal can occur.
Excessive Hemorrhage
Extirpation of pulp and instrumentation beyond periapical tissues lead to excessive hemorrhage. A clump of extravasated blood cells and fluid must be resorbed, otherwise, it acts as a foreign body and nidus for bacterial growth, especially in the presence of infection.
Chemical Irritants
Chemical irritants in the form of intracanal medicaments and irrigating solutions decrease the prognosis of endodontic therapy if they get extruded in the periapical tissues.
iatrogenic Errors
- Canal blockage and ledge formation
- In cases with canal blockage and ledge formation, complete cleaning and shaping of the root canal system cannot be accomplished
- Because of working short of the canal terminus, bacteria, and tissue debris may remain in non-instrumented areas contributing to endodontic failure.
- Incomplete debridement of the root canal system
- The presence of infected and necrotic pulp tissue in the root canal acts as the main irritant to the periapical tissues
- Poor debridement can cause residual microorganisms, their by-products, and tissue debris to recolonize and contribute to endodontic failure.
- Over instrumentationOverinstrumentation results in trauma to the periodontal ligament and the alveolar bone, thus affecting the success rate.
- Instrument separation
- Seltzer et al reported that the prognosis of endodontic therapy was not significantly affected in teeth in which vital pulp was present before treatment, but if instrument separation occurred in teeth with pulpal necrosis, the prognosis was found to be poor after treatment
- Separated instruments impair the mechanical instrumentation of infected root canals apical to the instrument, which contribute to endodontic failure.

- Perforation
- Perforation is the mechanical communication between the root canal system and the periodontium
- The prognosis of endodontically treated teeth with perforations depends on many factors such as location (its closeness to gingival sulcus), the time elapsed before the defect is repaired, adequacy of perforation seal, and size of the perforation.
- Incompletely filed teeth
- Incompletely filed teeth are teeth filed >2 mm short of the apex
- Underfiling can occur due to incomplete instrumentation or ledge formation, blockage of the canal, and improper measurements of working length
- Remaining infected necrotic tissue, microorganism, and their by-products in inadequately instrumented and filed teeth cause continuous irritation to the periradicular tissues and thus endodontic failure.

- Overfilling of root canals
- Overfilling of root canals, that is, obturation of the canal extending >2 mm beyond the radiographic apex. Filling material acts as a foreign body which may generate an immunological response and cause continuous irritation of the periapical tissues
- Biofilms present on extruded material contain treatment-resistant bacteria resulting in endodontic failure.
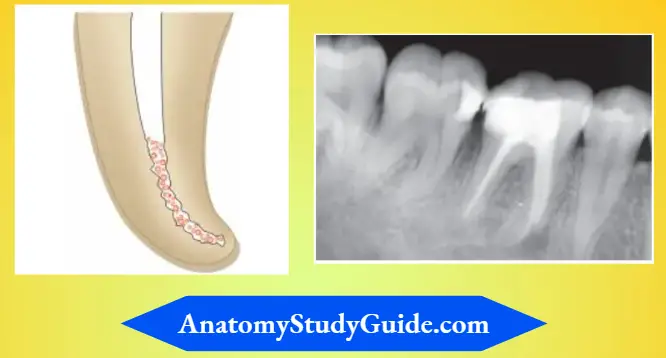
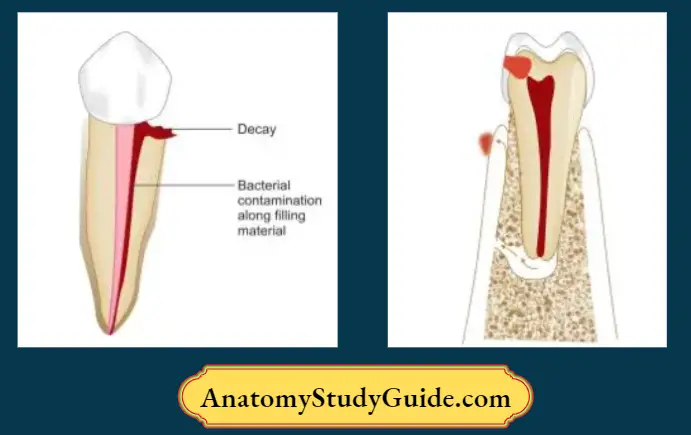
- Corrosion of Root Canal Fillings
Silver cones show corrosion which is commonly seen in coronal and apical areas due to contact of tissue fluids either periapical exudation or saliva. Corrosion products are cytotoxic and act as tissue irritants causing persistent periapical inflammation.
Anatomic Factors
The presence of curved canals, calcifications, lateral, and accessory canals, bifurcations, and aberrant canal anatomy like C- or S-shaped canals may cause inadequate cleaning and shaping and thereby incomplete obturation, resulting in endodontic failure.
Root Fractures
Partial or complete fractures of the roots can cause endodontic failure.
Traumatic Occlusion
Traumatic occlusion causes endodontic failures because of its effect on the periodontium.
Periodontal Considerations
The recession of the attachment apparatus may expose lateral canals to the oral fluids which can lead to reinfection of the root canal system because of the percolation of fluids.
Systemic Factors
The presence of systemic disease (nutritional deficiencies, diabetes mellitus, renal failure, blood dyscrasias, hormonal imbalance, autoimmune disorders, opportunistic infections, aging, and patients on long-term steroid therapy) can intensify the response of periapical tissues to the irritants during endodontic therapy and also impair healing.
Case Selection For Endodontic Retreatment
Retreatment is usually indicated in symptomatic endodontically treated teeth or in asymptomatic teeth with improperly done endodontic therapy to prevent the future emergence of the disease.
Before initiating endodontic retreatment, the following factors should be considered:
- When should the treatment be considered, that is, if the patient is asymptomatic even if treatment is not proper, the retreatment should be postponed
- Patient’s needs and expectations
- The strategic importance of the tooth
- Periodontal evaluation of the tooth
- Other interdisciplinary evaluation
- Chair time and cost.
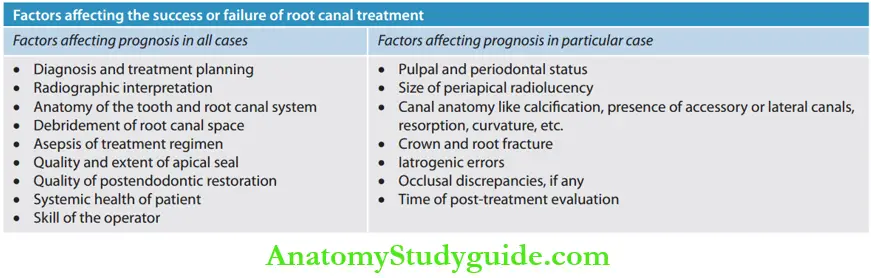
Factors affecting the prognosis of endodontic treatment
- Presence of any periapical radiolucency
- Quality of the obturation
- Apical extension of the obturation material
- Bacterial status of the canal
- Observation period
- Postendodontic coronal restoration
- Iatrogenic complication.
Contraindications of endodontic retreatment
- Unfavorable root anatomy (shape, taper, remaining dentin thickness)
- Presence of untreatable root resorptions or perforations
- Presence of root or bifurcation caries
- Insufficient crown/root ratio
Steps Of Retreatment
Steps of retreatment
- Coronal disassembly
- Establish access to the root canal system
- Remove canal obstructions and establish patency
- Through cleaning, shaping, and obturation of the canal.


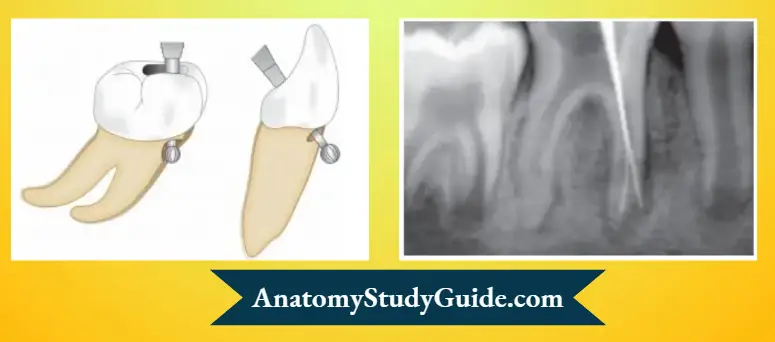
Coronal Disassembly
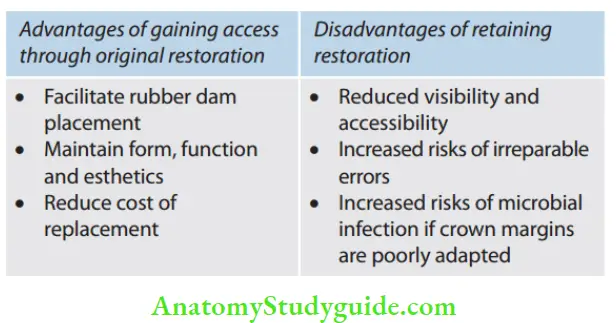
Endodontic retreatment procedures require the removal of existing coronal restoration. Though access can be made through the existing restoration, it is removed if it has poor marginal adaptation or secondary caries.
Establish Access to Root Canal System
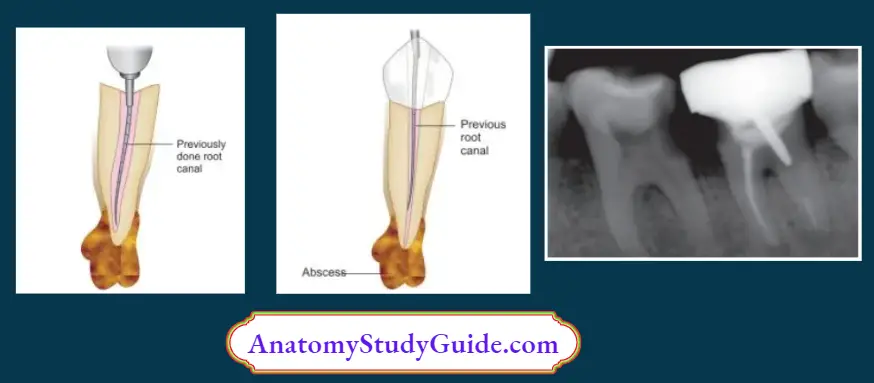
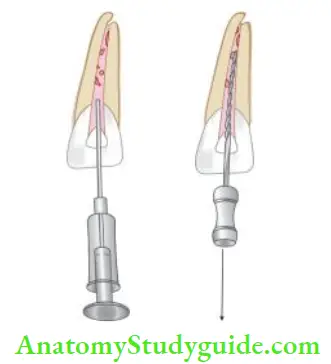
In teeth with post and core, the post has to be removed for gaining access to the root canal system. endodontic retreatment of mandibular second molar with defective obturation, fractured instrument in mesiobuccal canal associated with periapical radiolucency.
A patient complained of occasional pain along with the sinus tract, which was confirmed by taking a radiograph with gutta-percha placed in the sinus tract.
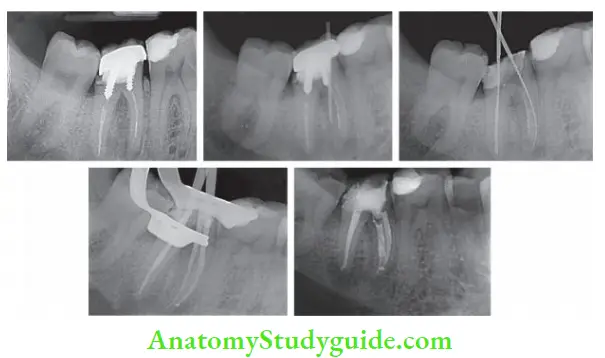
- (A) Preoperative radiograph showing defective root canal, improper post placement, and separated instrument in the mesiolingual canal;
- (B) Sinus tracking radiograph confirmed the offending tooth;
- (C) Removal of the post and establishing access to the distal and mesiobuccal canals. Separated instrument present in the mesiolingual canal;
- (D) After removal of the instrument, cleaning, and shaping, the master cone radiograph;
- (E) Post obturation radiograph.
Posts can be removed by the following method:
- Weakening the retention of posts by using ultrasonic vibration
- Pulling of posts but it increases the risk of root fracture
- With the help of special pliers using post-removal systems (PRSs)
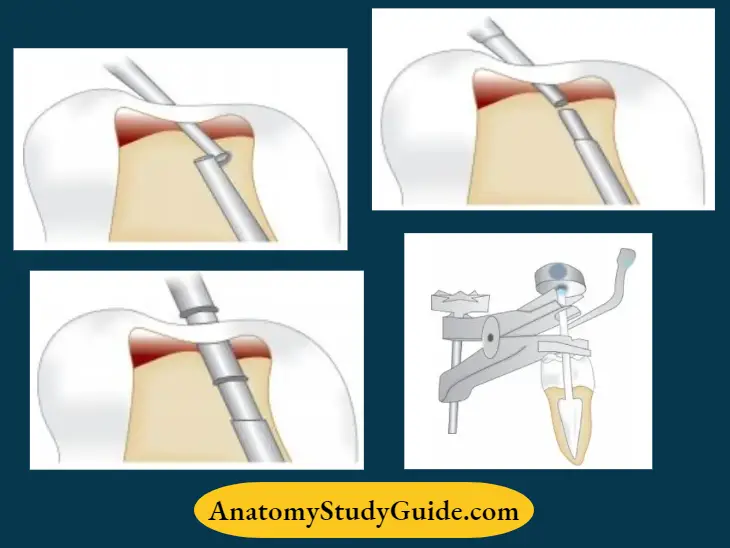
PRS kit consists of file differently designed trephines and corresponding taps, a torque bar, a Transmetal bur, rubber bumpers, and extracting pliers.
- Initially, a Transmetal bur is used for efficiently dooming of the pothead
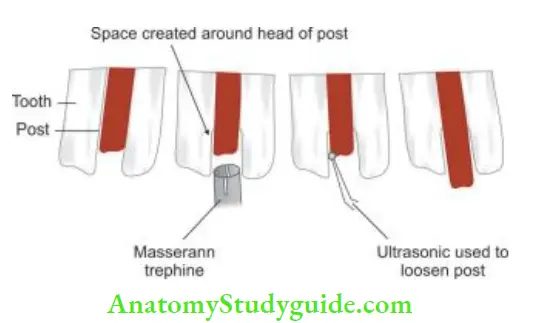
- Then a drop of a lubricant like RC Prep is placed on the post head to further facilitate the machining process
- After this, the trephine is selected to engage and machine down the coronal 2–3 mm of post
- Subsequently, a microtubular tap is inserted against the post head and screwed it into a post with a counterclockwise direction. Before doing this, a rubber bumper is inserted on the tap to act as a cushion against forces
- When the tubular tap tightly engages the post, the rubber bumper is pushed down to the occlusal surface
- Mount the post-removal plier on the tubular tap by holding it firmly with one hand and engaging it with the other hand by turning the screw knob clockwise if the post is strongly bonded in the canal, then an ultrasonic instrument is vibrated on the tap or a torque bar is inserted onto the handle to increase the leverage, thereby facilitating its removal
- After that, select an ultrasonic tip and vibrate it on the tubular tap, which causes the screwed knob to turn further and thus help in post-removal.
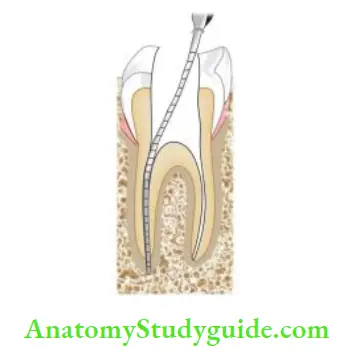
Removing Canal Obstructions And Establishing Patency
The patency of the canal is regained by removing canal obstructions like silver points, gutta-percha, pastes, sealers, separated instruments, posts, etc.
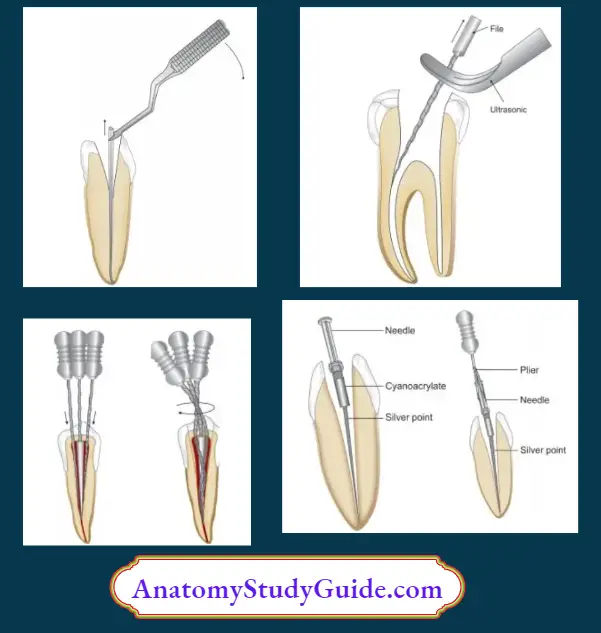
Silver Point Removal
Silver points can be bypassed or removed depending on the accessibility and canal anatomy. These can be retrieved from the canal by:
- Using microsurgical force; especially when the cone head is sticking up in the chamber
- Working ultrasonic fie around the periphery of the instrument to loosen it
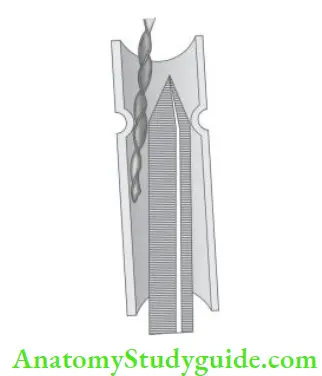
- Placing H-fies in the canal and working down alongside the silver point. These files are twisted around each other by making a clockwise rotation. This rotation will grasp around the silver point which then can be removed
- Using a hypodermic needle which is made to fit tightly over the silver point on which cyanoacrylate is placed as an adhesive. When it sets, the needle is grabbed with pliers
- By tap and thread option using microtubular taps from the PRS kit
- Using instrument removal system.
Gutta-Percha Removal
Relative difficulty in removing gutta-percha is influenced by length, diameter, curvature, and internal configuration of the canal system.
The following factors affect gutta-percha removal:
- Density of filing
- Curvature of canal
- Length of the canal.
Gutta-percha can be removed by
- Use of solvents: Gutta-percha is soluble in chloroform, methyl chloroform, benzene, xylene, eucalyptol oil, halothane, and rectified white turpentine; it can be removed from the canal by dissolving it in these solvents
- Being highly volatile, chloroform is the most effctive and commonly used. However, it has been shown to be carcinogenic in high concentrations, so excessive filing in pulp chambers should be avoided.
- Use of hand instruments: Hand instruments are mainly used in the apical part of the canal. H-fies are used to engage the cones so that they can be pulled out in a single piece. Hot fie or reamer can also be used to remove the gutta-percha points.
With overextended cones, fies sometimes have to be extended periodically to avoid separation of the cone at the apical foramen.
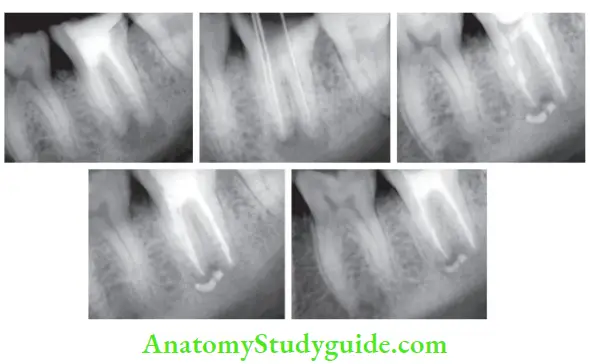
- (A) Preoperative radiograph showing defective root canal and periapical radiolucency with respect to mandibular second molar;
- (B) Gutta-percha removed using D-fies and working length taken;
- (C) Metapex placed for periapical healing;
- (D) After 25 days, obturation done using MTA;
- (E) Radiograph was taken after 3 months, showing healing of the periapical area.

- (A) Preoperative radiograph showing defective RCT in 35;
- (B) Radiograph was taken after removal of old gutta-percha using D-fies;
- (C) Postobturation radiograph.
The coronal portion of gutta-percha should be explored by Gates-Gliddens to:
- Remove gutta-percha quickly
- Provide space for solvents
- Improve convenience form
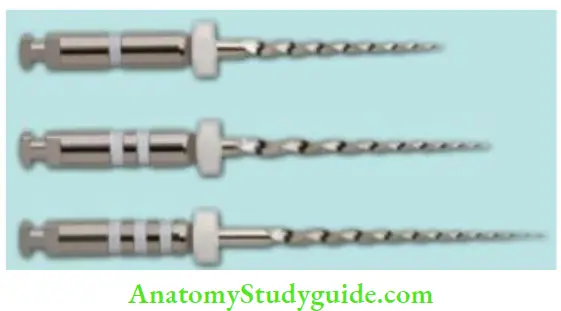
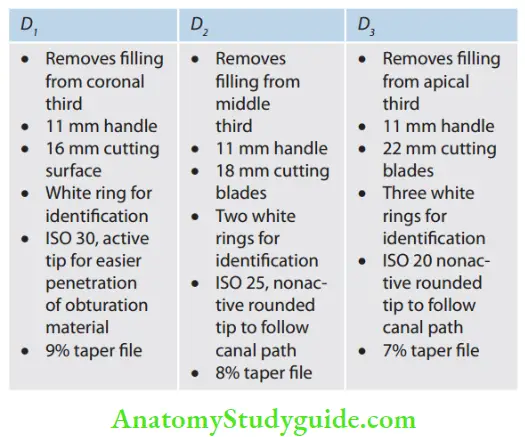
- Use of rotary instrumentation: Rotary instruments are safe to be used in straight canals. ProTaper universal system was introduced in 2006, it consists of D1, D2, and D3 to be used at 500–700 rpm
- Using microdebriders: These are small files constructed with 90° bends and are used to remove any remaining gutta-percha on the sides of canal walls or isthmuses after repreparation.
Removal of Resilon
Resilon can be removed using a combination of hand and rotary instruments similar to gutta-percha. For effctive removal of resin, a combination of chloroform dissolution and rotary instrumentation is recommended. For the removal of resin sealer, the use of Gates-Glidden drills and H-files is recommended.
Carrier-Based Gutta-Percha Removal
- Grasp the carrier with pliers and try to remove it using the fulcrum mechanism rather than straight pulling it from the tooth
- Use ultrasonics along the side of the carrier and thermos often the gutta-percha. The move ultrasonics apically and displace the carrier coronally
- Use solvents to chemically soften the gutta-percha and then use hand fies to loosen the carrier
- Use rotary instruments to remove the plastic carrier from the canal
- Use an instrument removal system to remove the carrier especially if it is a metal carrier.
Removal of Paste
Soft-setting pastes can be removed using the normal endodontic instruments preferably using a crown-down technique
Hard-setting cements like resin cements can be first softened using solvents like xylene, eucalyptol, etc., and then removed using endodontic files. Ultrasonic endodontic devices can also be used to break down the pastes by vibrations and facilitate their removal.
The following methods can be employed to remove pastes for retreatment cases:
- Heat is employed for some resin pastes for softening them
- Ultrasonic energy is employed to remove brick hard resin type pastes
- Chemicals like Endosolve “R” and Endosolve “E” are employed for softening hard paste (R denotes resin-based and E denotes eugenol-based pastes)
- Microdebriders are used to remove remnants of paste material. These are available in 16 mm length with Hedstroem-type cutting blades and tip diameters of 0.2 and 0.3 mm in 2% taper
- End-cutting NiTi rotary instruments are used to penetrate paste. But to avoid iatrogenic errors, they should be used with caution.
Separated Instruments and Foreign Objects
- The primary requirement for the removal of broken instruments or foreign objects is their accessibility and visibility
- if the root canal is obstructed by a foreign object in coronal third, then attempt retrieval, in the middle-third, attempt retrieval or bypass and if it is in the apical third leave it or treat surgically
- If overpreparation of the canal compromises the dentin thickness, leave the instrument in place rather than compromising the coronal dentin
- If the instrument is readily accessible, remove it by holding it with instruments like Stieglitz pliers and Massermann extractor. Massermann extractor comprises a tube with a constriction into which a stylet is introduced to grasp the fractured instrument
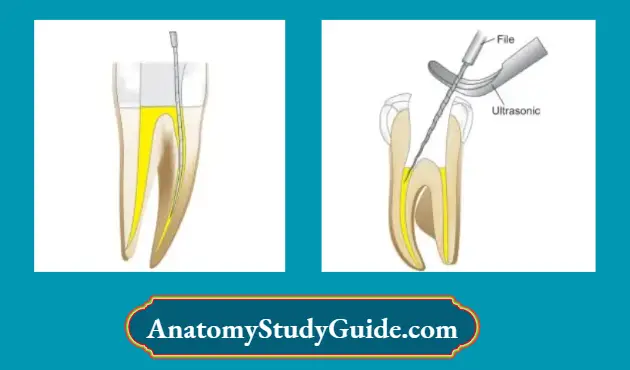
- Ultrasonics can also be used to remove the instrument by vibration effect
- Modified Gates-Glidden but can also be used. It creates a staging platform before using an ultrasonic tip to rotate around the fire in a counterclockwise direction so to remove it
- When it is not possible to remove the foreign objects, attempts should be made to bypass it and complete the biomechanical preparation of the canal system
- Bypassing of instruments can be done by using hand instruments like reamers and fees. These instruments are inserted alongside the broken instrument to soften its cementation and thus facilitate its removal.
- While making efforts to bypass the instrument, copious irrigation is needed. Irrigation with sodium hypochlorite, hydrogen peroxide, and RC Prep may flat the object coronally through the effervescence they create
- Use of ultrasonic K-file no. 15 or 20 with vibration and copious irrigation may also pull the instrument coronally.
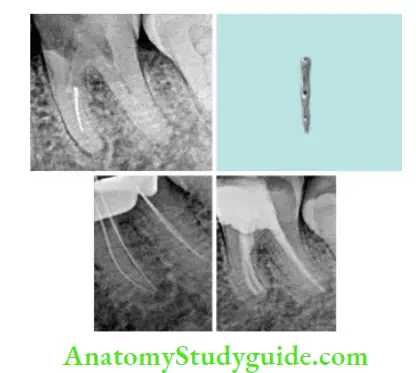
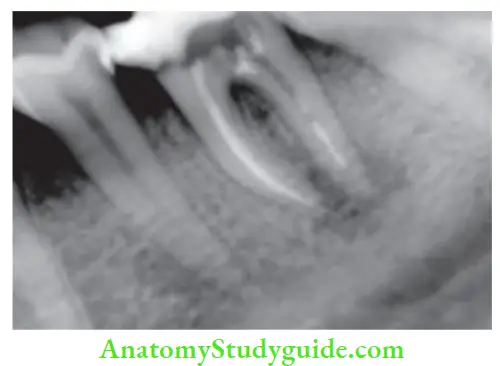
- (A) Preoperative radiograph showing separated instrument present in mesiolingual canal of mandibular first molar;
- (B) Separated instrument;
- (C) Working length radiograph after removal of the instrument;
- (D) Post obturation radiograph.
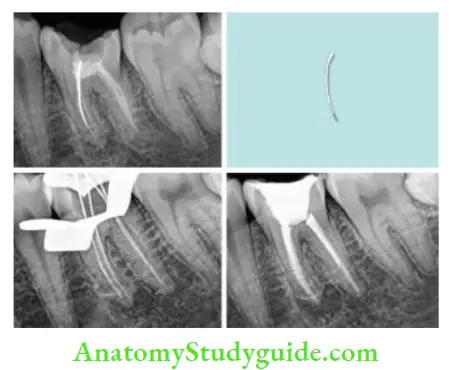
- (A) Preoperative radiograph showing separated instrument present in a mesiobuccal canal of Mandibular fist molar;
- (B) Separated instrument removed;
- (C) Working length radiograph after removal of the instrument;
- (D) Post obturation radiograph.
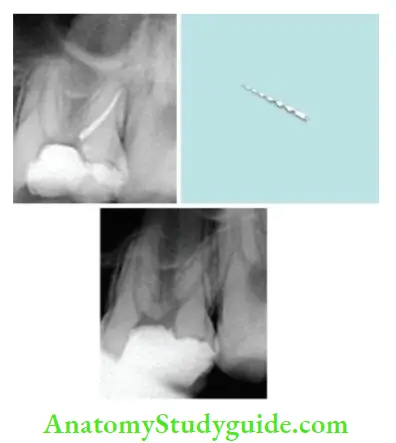
- (A) Preoperative radiograph showing separated instrument present in the distobuccal canal of maxillary first molar;
- (B) Separated instrument removed using ultrasonic vibration;
- (C) Radiograph after removal of the instrument.
Completion of the Retreatment
After gaining access to the root canal system, with its thorough cleaning and shaping and managing other complications, the treatment is completed using routine procedures. It is difficult to retreat a case nonsurgically especially if:
- Access is to be made through previously placed restoration
- Post removal is impossible
- Gutta-percha is extended periodically
- There is the presence of foreign objects, or hard-setting pastes which are amenable to remove nonsurgically.


Outcome of Retreatment
The outcome of retreatment can be short-term and long-term. Short-term outcome is associated with postoperative discomfort including pain and swelling.
The long-term outcome of retreatment depends on regaining the canal patency and obturation of the root canal system.
Endodontic Failures And Retreatment Conclusion
One should attempt primary endodontic treatment if the tooth can be saved successfully with endodontic therapy, but due to some factors, if it fails, nonsurgical endodontic retreatment should be considered before going for surgical intervention or extraction of the tooth.
Nonsurgical endodontic retreatment is a predictable procedure that allows patients to maintain their teeth. But, as with any procedure, the correct diagnosis to understand indications and limitations helps in proper treatment planning.
Leave a Reply