The health of periodontium is important for the normal physiology of the tooth. Periodontium is anatomically interrelated with pulp by virtue of apical foramina and lateral canals which create pathways for the exchange of noxious agents between these two tissues.
Table of Contents
Not only the interaction between periodontium and pulp produces or aggravates the existing lesion, but it also presents challenges in deciding the direct cause of an inflammatory condition. So a correct diagnosis should be made after careful history-taking and clinical examination.
Read And Learn More: Endodontics Notes
Endodontic Periodontal Definition
An endo–period lesion is one where both pulp and periodontal tissues are affected by the disease’s progress.
Pathways of communication between pulp and periodontium
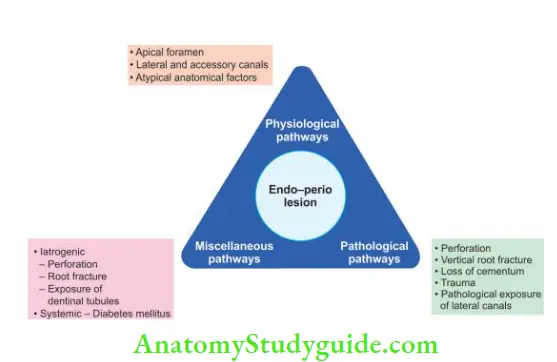
Pathways Of Communication Between Pulp And Periodontium
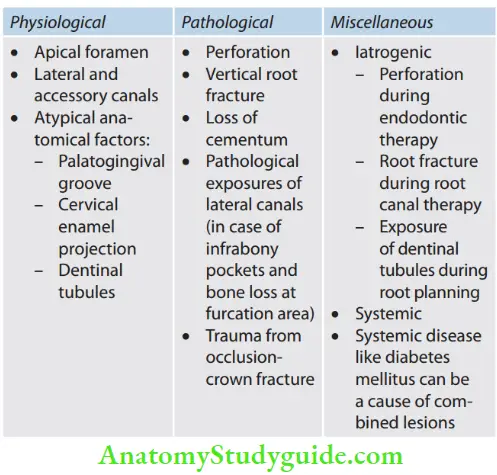
Physiological Pathways:
1. Apical Foramen
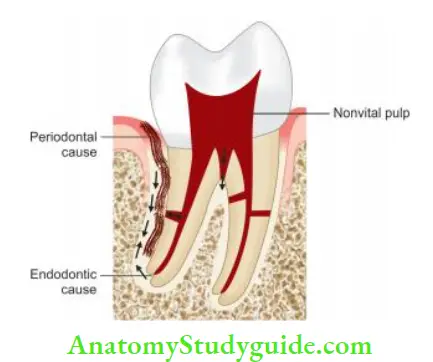
It is one of the major pathways of communication between dental pulp and periodontium. Inflammatory factors exit through the apical foramen and irritate the periodontium.
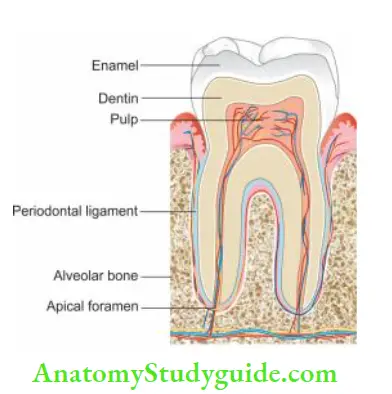
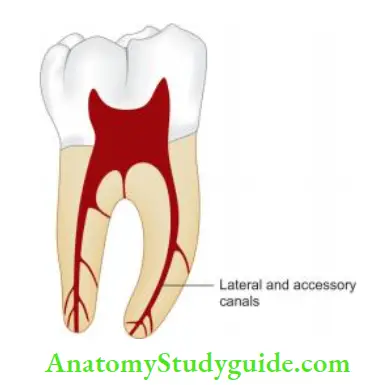
2. Lateral or Accessory Canals
The majority of lateral or accessory canals are found in the apical third and furcation area of the root. As periodontal disease progresses down the root surface, accessory, and lateral canals get exposed to the oral cavity. It is difficult to identify lateral canals on radiographs.
These can be identifid by isolated defects on the lateral surface of roots or by postobturation radiographs showing sealer puff.
Endo Perio Lesion Treatment
3. Palatogingival Groove
It is a developmental anomaly commonly seen in the maxillary lateral incisor. The groove begins in the central fossa, crosses the cingulum, and extends apically at varying distances.

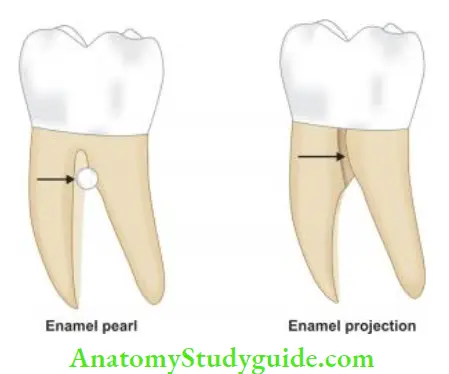
4. Cervical Enamel Projections
These are felt, ectopic extensions of enamel that extend beyond normal contours of cementoenamel junction (CEJ). They interfere with the attachment apparatus and are important in initiating periodontal lesions.
5. Dentinal Tubules
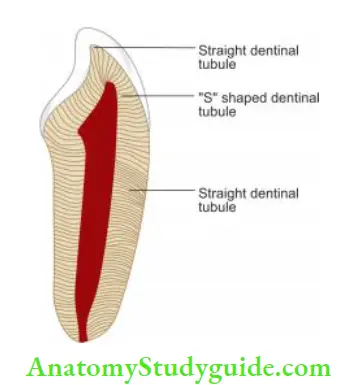
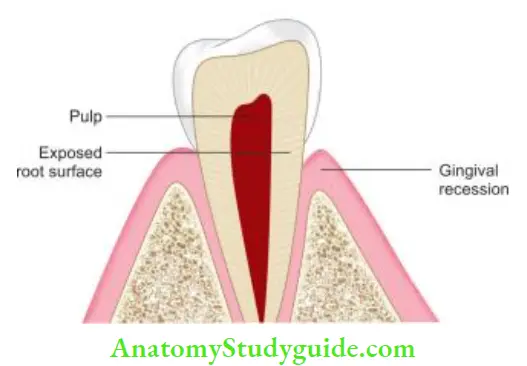
Dentinal tubules traverse from pulpodentinal junction to the cementodentinal or dentin enamel junction. Cementum acts as a protective barrier to the dentin but because of periodontal disease, periodontal therapy, etc., if the cementum is damaged, direct communication between dentinal tubules and the oral cavity may occur.
Pathological Pathways:
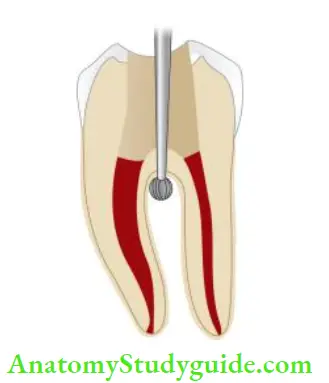
1. Perforation of the Root
Perforation creates an artificial communication between the root canal system and periodontium. The closer is the perforation to the gingival sulcus, the greater is the chances of apical migration of gingival epithelium in initiating a periodontal lesion.
Endo Perio Lesion Treatment
2. Vertical Root Fracture
Vertical root fracture forms a communication between the root canal system and the periodontium
3. Loss of Cementum
Loss of cementum can occur due to gingival recession, presence of inadequate attached gingiva, abrasion, periodontal surgery, overzealous tooth cleansing habits, etc.
4. Pathological Exposure Of Lateral Canals
Infrabony pocket or furcation bone loss can result in pulp exposure by exposing the lateral canals to the oral environment.
Miscellaneous Pathways
1. Latrogenic
Perforation during endodontic therapy: It produces mechanical or pathological communication between the root canal system and the external tooth surface.
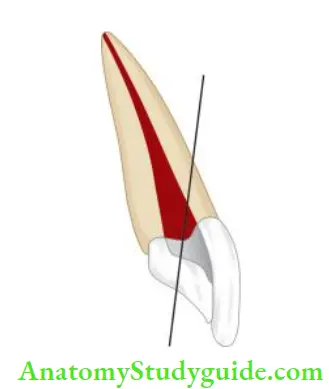
Root fracture during root canal therapy: Root fracture can occur due to excessive dentin removal during biomechanical preparation and weakening of the tooth during post-space preparation. The fracture site provides entry for bacteria and their toxic products from the root canal system to the surrounding periodontium.
Exposure of dentinal tubules during root planning: It can result in communication between pulpal and periodontal space.
Impact Of Pulpal Diseases On The Periodontium
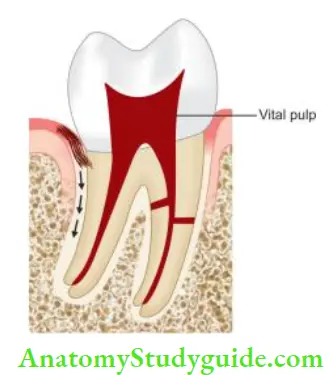
Pulpal infection may cause a tissue-destructive process that may progress from the apical region to the gingival margin, termed as retrograde periodontitis.
Restorative procedures and traumatic injuries cause inflammatory changes in the pulp, though it is still vital. Though a vital pulp does not affect the periodontium, the necrosed pulp is seen as associated with periodontal problems.
Inflammatory lesions may develop from a root canal infection through lateral and accessory canals.

Impact Of Periodontal Disease On Pulpal Tissue
Pathogenic bacteria and inflammatory products of periodontal diseases may enter the root canal system via accessory canals, lateral canals, apical foramen, and dentinal tubules resulting in retrograde pulpitis.
As periodontal disease extends from the gingival sulcus toward the apex, the auxiliary canals get affected which results in pulpal inflammation. It becomes more serious if these canals get exposed to the oral cavity because of the loss of periodontal tissues by extensive pocket depth.
Periodontal therapy using ultrasonic scalers, vibrators, curettes, and chemicals may harm the pulp especially if the remaining dentin thickness is <2 mm.
Etiology Of Endodontic–Periodontal Lesions
The primary etiologic agent in periodontitis is bacterial plaque. Besides this primary factor, there are secondary factors which contribute to the disease process either by increasing the chances of plaque accumulation or by altering the response of the host to the plaque.
Pulmonary diseases can result in periodontal problems and vice versa. It is the duration which is a key factor in evaluating the etiological effect of a particular factor.
1. Etiological Effects
Bacterial Plaque
Commonly associated microorganisms associated with endodontic–periodontal lesions are Actinomyces spp., F. nucleatum, P. intermedia, P. gingivalis, and Treponema spp. Sometimes C. albicans, viruses like herpes simplex, cytomegalovirus, and EBV have also been shown to play an important role in periapical lesions.
Foreign Bodies
Foreign bodies like amalgam filling, root canal filling material, dentin or cementum chips, and calculus deposits can irritate pulp and periodontium.
Contributing Factors Resulting in Combined Endodontic–Periodontal Lesions
- Malpositioned teeth causing trauma
- The presence of additional canals in teeth
- Cervical enamel projects into furcation of multirooted teeth
- A large number of accessory and lateral canals
- Trauma combined with gingival inflammation
- Vertical root fracture
- Crown fracture
- Root resorption
- Perforations
- Systemic factors such as diabetes
Classification Of Endodontic Periodontal Lesions
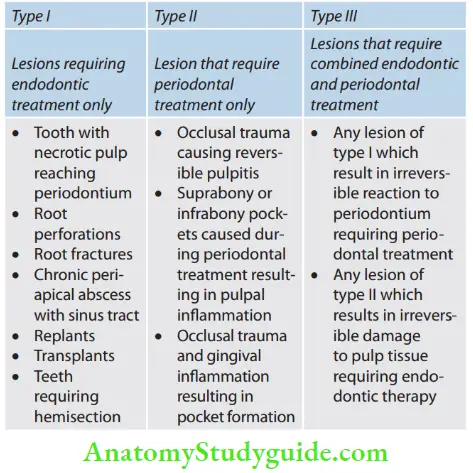
According to Weine: Based on etiology and treatment plan:
- Class 1: Tooth which clinically and radiographically simulates the periodontal involvement but it is due to pulpal inflammation or necrosis.
- Class 2: Tooth has both pulpal and periodontal disease occurring concomitantly.
- Class 3: The tooth has no pulpal problem but requires endodontic therapy plus root amputation for periodontal healing.
- Class 4: Tooth that clinically and radiographically simulates pulpal or periapical disease but has periodontal disease.
According to Simon et al.: Based on etiology, diagnosis, prognosis, and treatment.
- Type 1: Primary endodontic lesion.
- Type 2: Primary endodontic lesion with secondary periodontal involvement.
- Type 3: Primary periodontal lesions.
- Type 4: Primary periodontal lesion with secondary endodontic involvement.
- Type 5: Truly combined lesion.
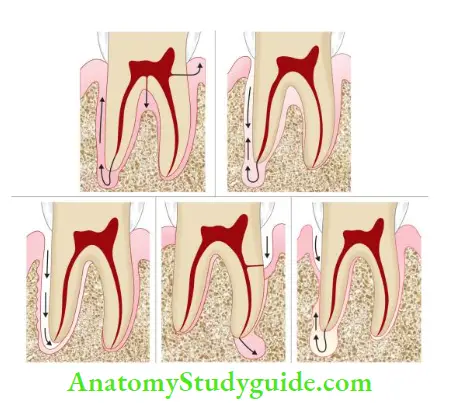
- (A) Primary endodontic lesion;
- (B) Primary endodontic lesion with secondary periodontal involvement;
- (C) Primary periodontal lesions;
- (D) Primary periodontal lesion with secondary endodontic involvement;
- (E) True combined lesion.
According to Grossman et al.: Oliet and Pollock’s classification based on the treatment protocol
Diagnosis Of Endodontic Periodontal Lesions
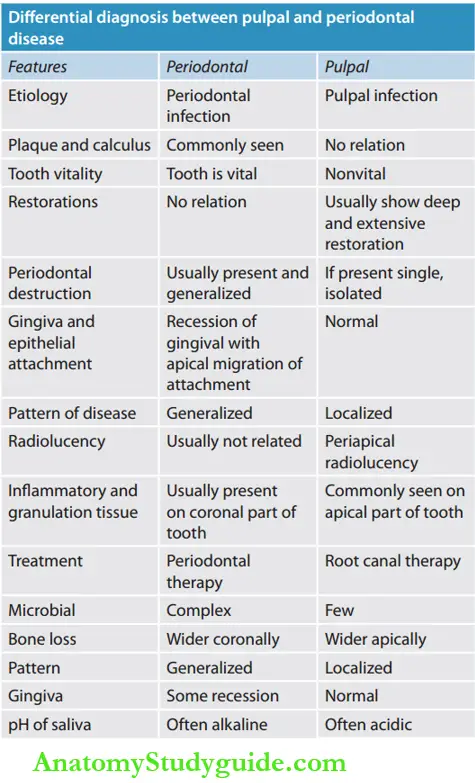
Diagnosis of a combined endodontic and periodontal lesion is often multifaceted and exasperating. A growing periapical lesion with secondary involvement of the periodontal tissue may have a similar radiographic appearance as a chronic periodontal lesion that has reached to the apex.
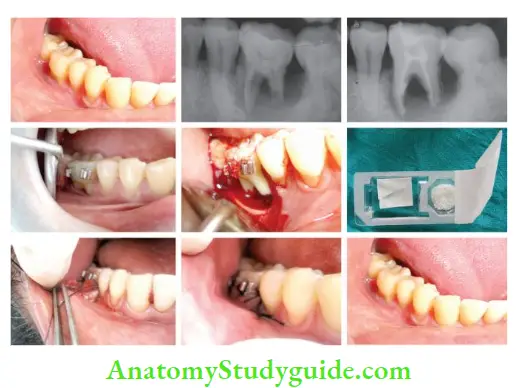
This, careful history taking, visual examination, diagnostic tests involving both pulpal and periodontal testing, and radiographic examination are needed to diagnose such lesions.
A tooth with a combined endodontic–periodontal lesion must fulfill the following criteria:
- The tooth involved should be nonvital
- There should be the destruction of the periodontal attachment which can be diagnosed by probing from the gingival sulcus to either the apex of the tooth or to the level of the involved lateral canal
- Both endodontic therapy and periodontal therapies are required to resolve the lesion completely
Endodontic Periodontal Lesions Chief Complaint of Patient
The patient may tell the pain indicates a pulpal or periodontal type. The history of the patient may reveal previous pulpal exposure or any periodontal treatment. Pulmonary condition is usually acute, whereas periodontal or secondary pulpal or combined lesions are usually chronic in nature.
Endodontic Periodontal Lesions Associated Etiology
For pulpal disease, caries, trauma, or pulp exposure is a common etiology, whereas for periodontal disease is associated with plaque/calculus, a history of bleeding gums, or bad odor.
Endodontic Periodontal Lesions Clinical Tests
Different signs and symptoms can be assessed by visual examination, palpation, and percussion. presence of carious tooth, recession, swelling of gingiva, plaque/calculus, or increased pocket depth may indicate endo–period lesion. Mobility tells the integrity of the attachment apparatus or the extent of inflmmation in the periodontal ligament.

Endodontic Periodontal Lesions Radiographs
Radiographs help in diagnosing caries, extensive restorations, previous root canal treatment, root form, root resorption, root fracture, root canal obliteration, thickened periodontal ligament space and any changes in the alveolar bone.

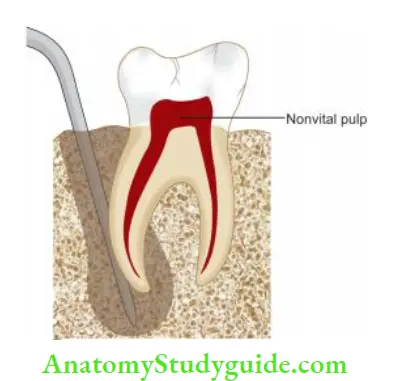
Endodontic Periodontal Lesions Pulp Vitality Tests
Any abnormal response of the pulp may indicate degenerative changes occurring in the pulp. Cases associated with nonvital pulp have pulpal pathology, whereas teeth associated with vital pulp usually have periodontal disease. Commonly used pulp vitality tests are cold test, electric tests, blood flow test, and cavity test.
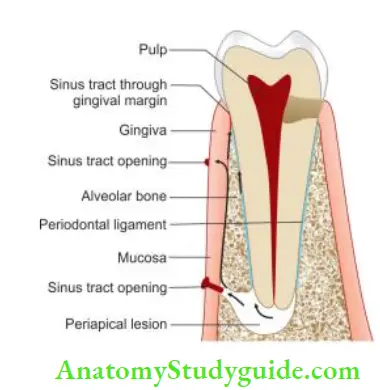
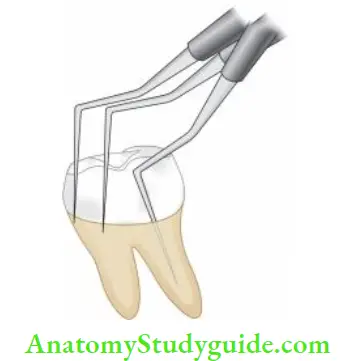
Endodontic Periodontal Lesions Tracking Sinus or Fistula
Gutta-percha is inserted slowly through the sinus and an X-ray is taken to track it. Being radiopaque, gutta-percha helps in determining and differentiating the source of infection.
![]()
Endodontic Periodontal Lesions Pocket Probing
Pocket probing helps to know the location and depth of the pocket and furcation involvement, if any.
Microbiological Examination
Microbiological analysis provides important information regarding the main source of the problem.
Distribution
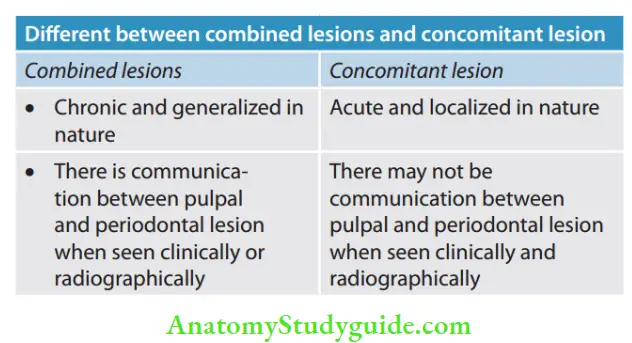
Pulmonary pathology is usually localized in nature, whereas periodontal condition is generalized.
Bone Loss
In pulpal disease, bone loss is generally localized and wider apically. It is not associated with vertical bone loss. In periodontal disease, bone loss is generalized which is wider coronally. It may be associated with vertical bone loss.
Pain
Pain in pulpal pathology is acute and sharp and the patient cannot identify the offending tooth. In periodontal pathology, pain is dull in nature and the patient can identify the offending tooth (because of the presence of proprioceptive nerve fiers in the periodontal ligament).
Swelling
If swelling is seen on the apical region, it is usually associated with pulpal disease. If it is seen around the margins or lateral surface of teeth, swelling is usually associated with periodontal disease.
Treatment and Prognosis
Treatment planning and prognosis depend mainly on the diagnosis of the specific endodontic and/or periodontal disease. In teeth with combined endodontic—periodontal lesions, the prognosis depends on the extent of destruction caused by periodontal disease.
If the lesion is of endodontic origin, an adequate endodontic treatment has a good prognosis. In combined disease, prognosis depends on the efficacy of periodontal therapy.
Primary Endodontic Lesions
Sometimes an acute exacerbation of a chronic apical lesion in a nonvital tooth may drain coronally through the periodontal ligament into the gingival sulcus, thus resembling a clinical picture of a periodontal abscess.
The lesion presents as an isolated pocket or swelling on the side of the tooth.
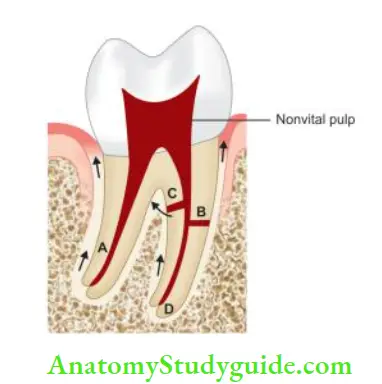
- A. from apical foramento gingival sulcus via periodontium,
- B. from lateral canal to pocket,
- C. from lateral canal to furcation;
- D. from apex to furcation.
Primary Endodontic Lesions Etiology
- Dental caries
- Deep restorations close to the pulp
- Traumatic injury
- Poor root canal treatment
Primary Endodontic Lesions Clinical Features
- The patient is usually asymptomatic, but a history of acute exacerbation may be present
- Since the tooth is associated with necrotic pulp, pulp does not show a response to vitality tests
- The sinus tract may be seen from the apical foramen, lateral canals, or the furcation area
- Probing shows true pockets. Pocket is associated with minimal plaque or calculus. A significant sign of this lesion is that the patient does not have periodontal disease in other areas of the oral cavity
Primary Endodontic Lesions Diagnosis
- Necrotic pulp draining through the periodontal ligament into the gingival sulcus
- Isolated pocket on the side of the tooth
- Pocket associated with a minimal amount of plaque or calculus
- The patient asymptomatic with a history of acute exacerbations
Primary Endodontic Lesions Treatment
- Root canal therapy
- Good prognosis
Primary Endodontic Lesions Prognosis
The prognosis after endodontic therapy is excellent. In fact, if periodontal therapy is performed without considering the pulpal problem, the prognosis becomes poor.
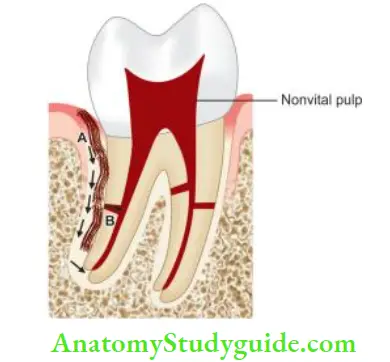
Primary Endodontic Lesion With Secondary Periodontal Involvement
This lesion appears if primary endodontic lesion is not treated. In such cases, the endodontic disease continues, resulting in the destruction of periapical alveolar bone, progression into the inter-radicular area, and finally causing the breakdown of surrounding hard and soft tissues.
As drainage persists through periodontal ligament space, accumulation of irritants results in periodontal disease and further apical migration of attachment.
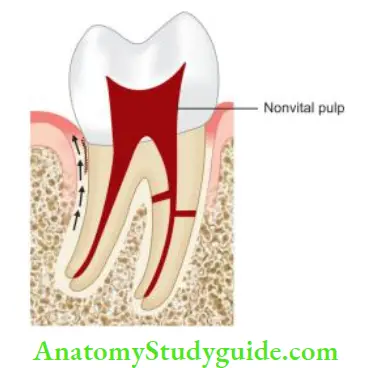
Primary Endodontic Lesion With Secondary Periodontal Involvement Clinical Features
- Isolated deep pockets are seen though there may be the presence of generalized periodontal disease
- In such cases, endodontic treatment will heal part of the lesion but complete repair will require periodontal therapy.
Primary Endodontic Lesion With Secondary Periodontal Involvement Diagnosis
- Continuous irritation of periodontium from necrotic pulp or from failed root canal treatment
- Isolated deep pockets
- Periodontal breakdown in the pocket.
Primary Endodontic Lesion With Secondary Periodontal Involvement Treatment
- Root canal treatment to remove irritants from pulp space
- Retreatment of failed root canal therapy
- Concomitant periodontal therapy
- Extraction of teeth with vertical root fracture if the prognosis is poor
- Good prognosis.
Primary Endodontic Lesion With Secondary Periodontal Involvement Prognosis
In case a vertical root fracture is causing the endo–period lesions, the tooth is extracted, otherwise, the prognosis is good.
Primary Periodontal Lesions
Primarily these lesions are caused by periodontal disease. In these lesions, periodontal breakdown slowly advances down to the root surface until the apex is reached. The pulp may be normal in most of the cases but as the disease progresses, the pulp may become affected.
Primary Periodontal Lesions Etiology
- Plaque
- Calculus
- Trauma.
Primary Periodontal Lesions Clinical Features
- Periodontal probing may show the presence of plaque and calculus within the periodontal pocket
- Due to attachment loss, the tooth may become mobile
- Usually, generalized periodontal involvement is present
Primary Periodontal Lesions Diagnosis
- Periodontal destruction associated with plaque or calculus
- A patient experiencing periodontal pain
- The pulp may be normal in most cases.
Primary Periodontal Lesions Treatment
- Oral prophylaxis and oral hygiene instructions
- Scaling and root planning
- Periodontal surgery and root amputation may be required in advanced cases.
Primary Periodontal Lesions Prognosis
The prognosis becomes poor as the disease advances.
Primary Periodontal Lesions With Secondary Endodontic Involvement
Periodontal disease affects pulp via lateral and accessory canals, apical foramen, dentinal tubules, or during iatrogenic errors. Once pulp gets secondarily affected, it can in turn affect the primary periodontal lesion.
Primary Periodontal Lesions With Secondary Endodontic Involvement Etiology
Periodontal procedures such as scaling, root planning, and curettage may open up lateral canals and dentinal tubules to the oral environment, resulting in pulpal inflmmation.
Here, the patient complains of sensitivity or inflammation after periodontal therapy.
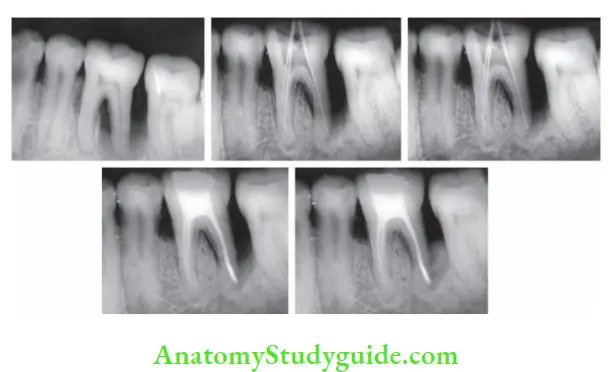
- (A) Preoperative radiograph;
- (B) Working length radiograph;
- (C) Master cone radiograph;
- (D) Radiograph after obturation;
- (E) Follow-up after 3 months.
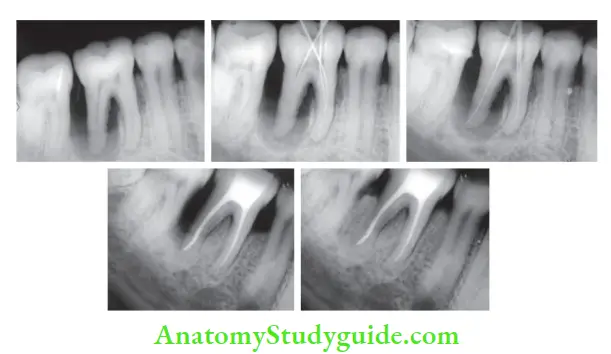
- (A) Preoperative radiograph;
- (B) working length radiograph;
- (C) master cone radiograph;
- (D) radiograph after obturation;
- (E) follow-up after 6 months.
Primary Periodontal Lesions With Secondary Endodontic Involvement Clinical Features
- Oral examination of the patient reveals the presence of generalized periodontal disease
- The tooth is usually mobile when palpated
- If severe periodontal destruction exposes the root surface, irreversible pulpal damage can result
- Radiographically, these lesions become indistinguishable from primary endodontic lesions with secondary periodontal involvement.
Primary Periodontal Lesions With Secondary Endodontic Involvement Diagnosis
- Periodontal destruction associated with nonvital tooth
- Generalized periodontal disease present
- Patients may complain of sensitivity after routine periodontal therapy
- Usually, the tooth is mobile
- The pocket may show discharge on palpation.
Primary Periodontal Lesions With Secondary Endodontic Involvement Treatment
- Root canal treatment
- Periodontal surgery in some cases
Primary Periodontal Lesions With Secondary Endodontic Involvement Prognosis
The prognosis depends on the periodontal problem.
Independent Endodontic And Periodontal Lesions Which Do Not Communicate
One may commonly see a tooth associated with pulpal and periodontal disease as separate and distinct entities. Both the disease states exist but with different etiological factors and with no evidence that either of disease has an impact on the other.
Periodontal Clinical Features
- Periodontal examination may show a periodontal pocket associated with plaque or calculus
- The tooth is usually nonvital
- Though both periodontal and endodontic lesions are present concomitantly, they cannot be designated as truly combined endo–period lesions because there is no demonstrable communication between these two lesions.
Periodontal Treatment
- Root canal treatment is needed for treating pulp space infection
- Periodontal therapy is required for periodontal problem
Periodontal Prognosis
The prognosis of the tooth depends on the periodontal prognosis
True Combined Endo–Perio Lesions
Truly combined lesions are produced when one of these lesions (pulpal or periodontal) which are present in and around the same tooth coalesce and become clinically indistinguishable. These are difficult to diagnose and treat.
True Combined Endo–Perio Lesions Clinical Features
- Periodontal probing reveals a conical periodontal type of probing and at the base of the periodontal lesion the probe abruptly drops farther down the root surface and may extend to the apex
- Radiograph may show bone loss from crestal bone extending down the lateral surface of the root
True Combined Endo–Perio Lesions Treatment
- First, see whether the periodontal condition is treatable if promising, and then go for endodontic therapy. Endodontic therapy is completed before initiation of definitive periodontal therapy
- After completion of endodontic treatment, periodontal therapy is started which may include scaling, root planning, and surgery along with oral hygiene instructions
True Combined Endo–Perio Lesions Prognosis
It depends upon the prognosis of the periodontal disease
Endodontic Periodontal Lesions Conclusion
Endodontic periodontal lesions present a diagnostic and treatment dilemma which can have diverse pathogenesis ranging from quite simple to complex. To reach at the correct diagnosis, the operator should have a thorough understanding and scientific knowledge of these lesions.
Treatment of combined endodontic and periodontal lesions does not differ from the treatment given when the two disorders occur separately. Even though dentistry is divided into multiple fields of specialization, to achieve the best outcome for endo–period lesions, a multi-disciplinary approach should be involved, though some cases may require only endodontic therapy or periodontal treatment and others may require the combined approach.
Leave a Reply