Gastrointestinal Tract
Drugs Used In Peptic Ulcer
Overview: Acid peptic disease is common in the present day as stress is part of everyday life in majority of the population
Read And Learn More: Pharmacology Question And Answers
Peptic Ulcer Classification:
1. Drugs that neutralize gastric acid:
- Antacids magnesium hydroxide, aluminum hydroxide, calcium carbonate, sodium bicarbonate
2. Drugs that reduce gastric acid secretion:
- H2 receptor blockers
- Cimetidine, ranitidine, famotidine, roxatidine, nizatidine
- Proton pump inhibitors
- Omeprazole, esomeprazole, lansoprazole, dexlansoprazole,pantoprazole, rabeprazole
- Muscarinic antagonists
- Pirenzepine, telenzepine, propantheline
3. Ulcer protective:
- Drugs that enhance mucosal defense
- Sucralfate, bismuth salts, rebamipide, carbenoxolone, misoprostol
- Others
- Vonoprazan
4. Anti-H. pylori drugs:
- Amoxicillin, clarithromycin, metronidazole
Drugs That Neutralize Gastric Acids
Question 1. Classify drugs used in peptic ulcer. Write the pharmacology of any 2 of them.
Or
Write short note on:
- Antacids
- Ranitidine.
Answer:
1. Antacids: Antacids are basic substances.
- Given orally they neutralize the gastric acid in the stomach and raise the pH of gastric contents.
- Peptic activity is also reduced, as pepsin is active only below pH
- Thus antacids provide rapid relief of symptoms in hyperacidity. Since the pH rises >5 there could be rebound hyperacidity due to raised gastrin levels.
- The duration of action of antacids is generally 30–60 minutes when taken on an empty stomach.
Antacids Types:
- Systemic antacids
- Sodium bicarbonate, sodium citrate
- Nonsystemic antacids
- Aluminum hydroxide
- Magnesium hydroxide, magnesium trisilicate, magnesium carbonate
- Calcium carbonate.
Systemic Antacids:
- Sodium bicarbonate is rapid but short-acting.
NaHCO3+ HCl → NaCl + H2O + CO2
Systemic Antacids Disadvantages:
- Sodium bicarbonate gets absorbed from the intestines leading to systemic alkalosis.
- There is a ‘rebound’ hyperacidity as gastrin levels increase due to raised gastric pH.
- Sodium load may increase and is troublesome in cardiovascular diseases.
- CO2 released in the stomach can cause bloating and escapes as eructation.
- When higher doses of sodium bicarbonate or calcium carbonate are given with calcium-rich dairy products, a syndrome known as milk–alkali syndrome can result—characterized by hypercalcemia, metabolic alkalosis, and renal dysfunction.
- Sodium bicarbonate is not preferred for long-term use because of the above disadvantages.
Systemic Antacids Uses:
- Peptic ulcer and hyperacidity for short periods.
- To alkalinize the urine in the treatment of poisoning due to acidic drugs.
- To treat metabolic acidosis.
Sodium citrate:
Sodium citrate is absorbed systemically and can be used as an alternative.
Nonsystemic antacids:
- Nonsystemic antacids are not absorbed.
- They are insoluble compounds that react in the stomach with HCl to form chloride salt and water.
For example:
- Mg (OH)2 + 2HCl → MgCl2 + 2H2O
- CaCO3+ 2HCl → CaCl2 + H2O + CO2
Aluminum hydroxide:
- Aluminum hydroxide is slow acting. It is also an astringent and demulcent forming a protective coating over the ulcers.
- The aluminum ions relax the smooth muscles resulting in delayed gastric emptying and constipation.
Magnesium salts:
- Their action is quick and prolonged. Rebound acidity is mild. Magnesium chloride formed in the stomach is an osmotic purgative and the dose used as an antacid may cause mild diarrhea.
- Prolonged use may cause hypermagnesemia in the presence of renal dysfunction.
- An aqueous suspension of magnesium hydroxide is called milk of magnesia.
Calcium carbonate:
- Calcium carbonate acts quickly and has prolonged action but liberates CO2 which may cause discomfort. Calcium salts also have a chalky taste.
- They may cause constipation and hypercalcemia. Long-term use may also result in renal calcium stones and milk–alkali syndrome.
Question 2. Give reason: Aluminium- and magnesium salts are given in combination as antacids.
Answer:
Antacid combinations are given to produce maximum benefits with the least adverse effects:
Magnesium + Aluminium salts:
- Quick and prolonged effect: Fast-acting [Mg(OH)2] and long-acting [Al(OH)3] compounds.
- Neutralizing side effects: Magnesium salts have a laxative effect, while aluminum salts are constipating—combination neutralizes each other’s side effects.
- Gastric emptying: Magnesium salts increase while aluminum salts delay gastric emptying.
Magnesium + Aluminium saltsAdditive effect:
The combination has an additive effect and a lower dose of each compound is adequate.
Magnesium + Aluminium salts Use:
- Antacids are used as adjuvants in hyperacidity, peptic ulcer, and reflux esophagitis.
- Antacid tablets should be chewed and swallowed as they do not disintegrate well in the stomach.
- Gels are more effective than tablets.
- One dose given 1 hour after food neutralizes the acid for 2 hours.
Magnesium + Aluminium salts Drug interactions:
Antacids form complexes with iron, tetracyclines, digoxin, ranitidine, fluoroquinolones, sulfonamides, and antimuscarinic drugs. To avoid the above DI, antacids should be given 2 hours before or 2 hours after other drugs.

Antifoaming Agents
Simethicone:
- Simethicone or dimethylpolysiloxane is a silicone polymer. It is pharmacologically inert, repels water, and helps in the proper dispersion of antacids in the gastric contents.
- It is also an antifoaming agent as it reduces surface tension and thereby decreases gastric flatulence. Simethicone may be used in combination with antacids.
Oxethazaine:
- Oxethazaine is a local anesthetic that anesthetises the sensory nerve endings in the stomach and esophagus → inhibits gastrin release and also relieves pain.
- Oxethazaine is available in combination with antacids. It can cause drowsiness and dizziness.
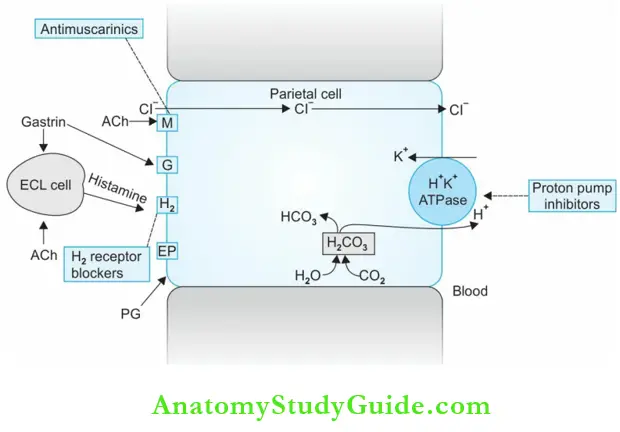
Drugs that reduce gastric acid secretion. H2-Receptor Blockers:
Question 3. Write a short note: H2-blockers/ranitidine/cimetidine.
Or
Mention the uses of H2-blockers/ranitidine.
Or
List the advantages of ranitidine over cimetidine.
Answer:
- Cimetidine, ranitidine, famotidine, roxatidine, and nizatidine are H2-receptor blockers.
- Ranitidine → Blocks H2 – receptors on parietal cells → ↓ ↓ Gastric acid secretion
These drugs bind to the histamine H2 -receptors on the parietal cells and competitively inhibit the action of histamine on these receptors and thereby reduce gastric secretion.
- Both volume and acidity of basal, nocturnal, and food-induced secretion are reduced.
- Inhibition is dose-dependent—a single dose causes 60–70% gastric acid reduction.
- Secretion of intrinsic factor and pepsin are also reduced.
- Help faster healing of peptic ulcers.
H2-Receptor Blockers Pharmacokinetics:
- H2 -blockers are rapidly and well-absorbed but undergo first-pass metabolism (~50% bioavailability).
- Food does not interfere with their absorption. They are partly metabolized in the liver and excreted by the kidneys.
- In renal impairment, a dose of H2 blockers should be reduced.
H2-Receptor Blockers Adverse effects:
- H2 -blockers (except cimetidine) are fairly safe and well-tolerated with minor side effects like diarrhea, dizziness, muscle pain, and headache.
- They cross the placenta and are also secreted in the milk hence avoid in pregnancy and lactation. Rarely cause blood dyscrasias.
Cimetidine:
- Cimetidine can cause antiandrogenic effects because it inhibits the binding of testosterone to androgen receptors, displaces testosterone from its binding sites on the androgen receptors; increases plasma prolactin levels, and inhibits estrogen metabolism in the liver.
- Prolonged use may result in gynecomastia, decreased sperm count, impotence, and loss of libido in men and galactorrhea in women.
- CNS effects include confusion, restlessness, delirium, and hallucinations in the elderly.
- Headache, dizziness, rashes, and diarrhea.
- Cardiovascular effects like bradycardia, AV block, cardiac arrest, atrial fibrillation, ventricular extrasystoles, and ventricular tachycardia have been reported.
- Cimetidine inhibits microsomal enzymes (cytochrome P450) and interferes with the metabolism of many drugs resulting in several drug interactions.
- Cimetidine and other H2 -blockers should be given IV only as a slow infusion because the rapid injection can cause bradycardia, hypotension, and cardiac arrest.
- Cimetidine is not preferred because of adverse effects, drug interactions, and also the availability of safer drugs.
2. Ranitidine:
- Ranitidine is the preferred H2 -blocker as it has several advantages over cimetidine:
- Ranitidine is more potent and longer-acting than cimetidine.
- Has no antiandrogenic effects, does not increase prolactin levels, and does not influence estrogen metabolism—hence no antiandrogenic side effects.
- No CNS effects as it does not cross BBB (IV ranitidine can rarely cause CNS effects).
- Does not inhibit microsomal enzymes significantly → any related drug interactions.
- The only common adverse effects are headache and dizziness.
- Dose: Ranitidine 150 mg BD or 300 mg HS
Famotidine, Roxatidine, and Nizatidine are similar to but more potent and longer-acting than ranitidine.
- Dose: Famotidine 20 mg BD/40 mg at bedtime.
- Roxatidine 75 mg BD/150 mg at bedtime.
H-Blockers Uses:
- Peptic ulcer: They provide rapid relief from pain and the ulcers heal with 6–8 weeks of treatment but to be continued for long periods to prevent recurrence.
- Gastritis: First-line drugs for non-ulcer dyspepsia.
- Prevention of stress-induced ulcers: Given for short periods as in critically ill patients.
- Zollinger-Ellison syndrome: High gastrin levels due to gastrin-secreting tumor is known to cause peptic ulcers. High doses of H2-blockers are alternatives to PP inhibitors till surgical resection of the tumor is done.
- Preanesthetic medication: H2-blockers reduce gastric acid secretion and prevent damage to the respiratory mucosa if aspiration occurs during surgery.
- GERD: H2-blockers are alternatives to PPIs in mild GERD
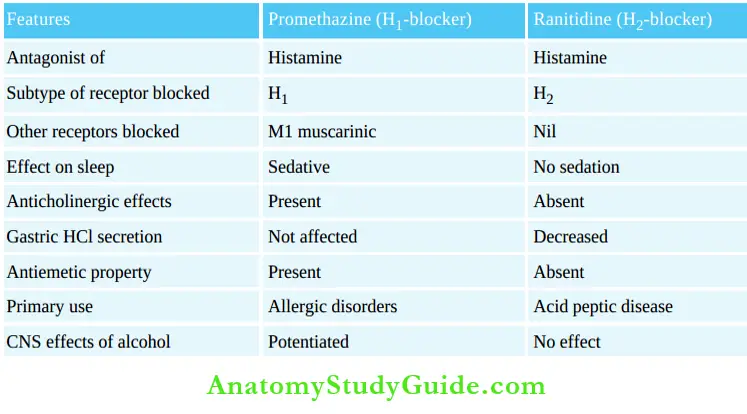
Promethazine and ranitidine:
Proton Pump Inhibitors
Question 3. Write the mechanism of action of PPIs/short note on omeprazole/PPI.
Answer:
Dr George Sachs put forward the idea that drugs that inhibit the proton pump could control acid secretion. Proton pump inhibitors (PPIs) are the most efficacious inhibitors of the gastric acid secretion. Omeprazole, pantoprazole, lansoprazole, dexlansoprazole, rabeprazole and esomeprazole are PPIs with minor pharmacokinetic variations.
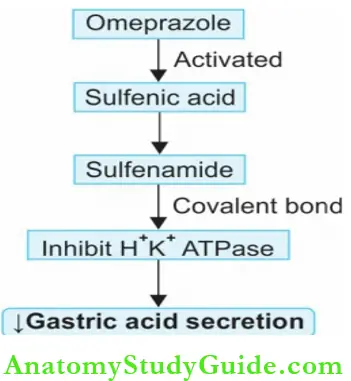
PPIs Mechanism of action:
- Parietal cells of the stomach secrete H+ with the help of the enzyme H+K+
- ATPase (proton pump) is present in its plasma membrane. This is the final step in gastric acid secretion due to all stimuli.
- PPIs are prodrugs, they accumulate in the parietal cells where they get activated to sulfenamide in an acidic environment. The active form firmly binds H+ K+
- ATPase by covalent bonds and irreversibly inhibits H+K+ ATPase. It thereby inhibits gastric secretion. The binding is irreversible and a single dose can almost totally (90–95%) inhibit gastric secretion.
- However, it requires 3 – 4 days of PPI therapy for maximum efficacy to develop.
- In the same way, the acid secretion resumes completely only after 3 – 4 days after stopping the PPI, after the new H+K+ ATPase enzyme is synthesized.
- Ulcer heals rapidly even in resistant cases.
PPIs Pharmacokinetics:
- All PPIs are effective orally; some of them like pantoprazole and rabeprazole can also be given IV.
- PPIs are weak bases and get rapidly absorbed from the intestines, and reach the parietal cell canaliculi because of their acidic nature. The concentration in parietal cell canaliculi is 1,000 times more as it gets trapped.
- Though the t½ of PPIs is short (1–2 hours), the effect of a single dose remains for 2–3 days because of its accumulation in the parietal cell canaliculi (hit and run drugs).
- Because the maximum number of proton pumps are active by about 1 hour after food, PPIs should be taken 1 hour before food so that their peak levels are reached when the highest number of proton pumps are active.
Some Ulcerogenic Drugs:
- NSAIDs
- Theophylline
- Glucocorticoids
- Caffeine
- Iron
- Tetracyclines
- Alendronate
PPIs Adverse effects:
- PPIs are well-tolerated and are largely safe.
- Prolonged acid suppression → bacterial overgrowth in stomach → ↑ GI infections.
- Dizziness, headache, diarrhea, abdominal pain, nausea, arthralgia, and rashes are rare.
Long-term use may result in:
- Vitamin B deficiency due to its reduced absorption—because acid is necessary for vitamin B12 to be released from the food.
- Acid is needed for the absorption of magnesium, calcium, and iron.
- In elderly patients, ↑ risk of osteoporosis—check calcium levels and bone density.
- ↑ Gastrin levels due to reduced gastric acidity → Could result in rebound acidity.
- Atrophic changes in the stomach are noticed after 3 – 4 years of use.
PPIs Drug Interactions
- Itraconazole requires acidity for absorption → ↓ absorption
- Inhibit microsomal enzymes → ↓ metabolism of diazepam, → toxicity (omeprazole, esomeprazole) phenytoin, warfarin
- Clopidogrel, being a prodrug, needs CYP2 C19 for its activation. PPIs like omeprazole should be avoided with clopidogrel. If required pantoprazole or rabeprazole may be given.
Lansoprazole:
- Lansoprazole and dexlansoprazole have higher oral bioavailability, faster onset of action and longer acting.
- Dose: 15–30 mg OD.
Pantoprazole:
- Pantoprazole is more acid stable and has higher oral bioavailability.
- Microsomal enzyme inhibition is milder compared to omeprazole and lansoprazole and therefore, the drug interactions are fewer.
- Dose: 40 mg OD.
Rabeprazole:
- Rabeprazole has the fastest onset of action; efficacy is similar to omeprazole with milder inhibition of microsomal enzymes like pantoprazole.
- Dose: 20 mg OD.
Esomeprazole:
- Esomeprazole the S-enantiomer of omeprazole, has a better bioavailability.
- Dose: 20–40 mg.
PPIs Uses :
- Peptic ulcer: In patients not responding to H2-blockers, PPIs are used for faster and better ulcer healing and pain relief. Most duodenal ulcers heal in 4–6 weeks while gastric ulcers may require 6–8 weeks.
- GERD: Severe GERD needs long-term acid suppression with PPIs.
- Dyspepsia: H2-blockers are preferred for non-ulcer dyspepsia, but PPIs may also be used.
- Drug-induced ulcers: PPI is given for 4–6 weeks and withdrawn after the ulcer heals.
- H. pylori regimen: PPIs also form a component in the H2. pylori treatment regimen.
- Zollinger-Ellison syndrome: PPIs are useful when ZE syndrome is associated with gastrin-secreting tumors.
- Gastrinomas: Could cause peptic ulceration—when surgery is not possible PPIs are useful

Ulcer Protectives
Question 4. Write a short note on ulcer protectives/sucralfate.
Answer:
1. Sucralfate:
Sucralfate: is a salt of sucrose and sulfated aluminum hydroxide. In an acidic medium (pH <4) or water, sucralfate polymerizes to form a sticky, viscid gel that firmly adheres to the base of the ulcers. It remains there for over 6 hours acting as a physical barrier and preventing contact with acid and pepsin. Sucralfate is not absorbed, is excreted in the feces, and is well tolerated.
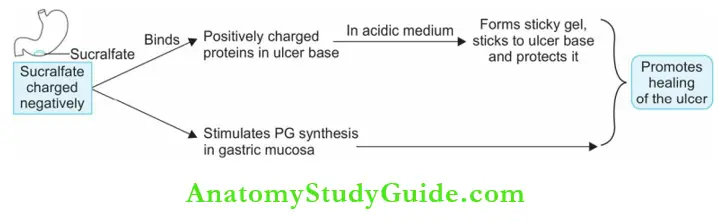
Sucralfate Use:
- For peptic ulcer one tablet (1 g) is given 1 hour before each meal and one at bedtime for 4–8 weeks and then 1 g BD for 6 months to prevent a recurrence.
- Prevention of stress-induced ulcers.
- Topical with lignocaine—for anal fissures and hemorrhoids.
- Side effects are rare constipation (due to aluminum), abdominal discomfort, and dryness of the mouth. Long-term use may cause toxicity due to aluminum absorption.
- Dose: 1 g 1 hour before each meal and at bedtime for 4–8 weeks.
Sucralfate Drug Interactions:
- Sucralfate needs acidic pH for activation. Hence antacids should not be given with it.
- Sucralfate adsorbs and interferes with the absorption of tetracyclines, digoxin, phenytoin, and ranitidine.
Rebamipide: Rebamipide increases mucosal defense by temporarily activating genes coding for cyclooxygenase 2 and also acting as a free radical scavenger—it protects the gastroduodenal mucosa and promotes the healing of gastroduodenal ulcers.
2. Bismuth salts:
Colloidal bismuth subnitrate and bismuth subsalicylate—on oral administration chelate proteins in the ulcer base. Bismuth salts may cause constipation, black stools, darkening of the tongue, and dizziness.
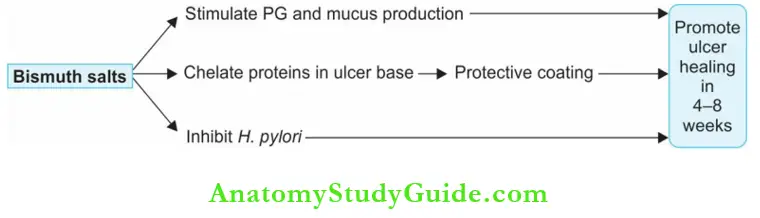
- Used occasionally in combination regimens for H. pylori infections and also for prevention of traveler’s diarrhea.
- Bismuth compounds should be used only for short periods.
- Dose: 120 mg 1 hour before meals and at bedtime.
3. Carbenoxolone:
- Carbenoxolone is a steroid-like compound obtained from the root of licorice. On ingestion, it alters the composition of mucus so that it is more viscid and adheres to gastric mucosa to protect the ulcer base.
- It also inhibits pepsin activity and prolongs the life of PGs.
- Because of its steroid-like effects, it causes salt- and water retention leading to edema and weight gain. It is, therefore, not preferred.
Other Drugs:
Prostaglandins: PGE1, PGE2, and PGI2 synthesized by the gastric mucosa inhibit gastric secretion, increase mucus production, and mucosal blood flow, and exert a cytoprotective effect.
- They bind to the PG receptor (EP3) present in the parietal cells and inhibit cAMP production.
- Synthetic PGE1 analog misoprostol and PGE2 analogs like enprostil, arbeprostil, and misoprostol are used in acid-peptic disease.
- They are of special value in preventing NSAID-induced gastric ulceration because NSAIDs are PG synthesis inhibitors—but are expensive.
- Diarrhea, muscle cramps, and oxytocic effects are common—they should be avoided in pregnancy because they are ecbolics.
Treatment Of H. Pylori Infection
- The gram-negative bacterium H. pylori is adapted to living in the stomach. Infection with H. pylori is associated with gastritis and peptic ulcer.
- It could also be responsible for the recurrence of peptic ulcer disease and is considered as a major risk factor for stomach cancer. Eradication of
- H. pylori various combination regimens of 2–4 drugs are tried with efficacy up to 95%.
- The use of a PP inhibitor in the regimen improves the efficacy of the antibiotics in eradicating H. pylori by raising gastric pH and enhancing antibiotic stability activity of amoxicillin and clarithromycin are pH dependent.
Some regimens are:
1. One-Week Regimen:
- Clarithromycin 250 mg BD + Metronidazole 400 mg BD + Omeprazole 20 mg BD.
- Amoxicillin 1,000 mg BD + Tinidazole 500 mg BD + Lansoprazole 30 mg BD.
2. Two Weeks Regimen:
- Clarithromycin 500 mg TDS/Amoxicillin 750 mg TDS + Omeprazole 20 mg BD.
- Amoxicillin 750 mg + Tinidazole 500 mg + Omeprazole 20 mg—all twice daily.
- Clarithromycin 500 mg + Amoxicillin 750 mg + Omeprazole 20 mg + Lansoprazole 30 mg— all twice daily.
- Amoxicillin 1,000 mg + lansoprazole 30 mg + Clarithromycin 500 mg—all twice daily.
Emetics
- Emetics are drugs that produce vomiting. When a poisonous substance is ingested, vomiting has to be induced. The stimuli, pathways, centers, and receptors involved in the emetic reflex are depicted in below.
- Emetics may act directly by stimulating the CTZ or reflexly by irritating the stomach mucosa. Mustard powder (1 teaspoon) with water or hypertonic salt solution can evoke vomiting reflexly.
Apomorphine:
- It is a derivative of morphine. Given SC/IM, it produces vomiting in 5–10 minutes. It acts by stimulating the dopaminergic receptors in the CTZ.
- Apomorphine can depress respiration and should, therefore, be avoided in the presence of respiratory depression.
Ipecacuanha:
- Obtained from the dried root of Cephalis ipecacuanha contains an alkaloid emetine. Given as a syrup (Dose: 15–20 mL), it produces vomiting in 15 minutes.
- It acts both directly on the CTZ and reflexly by irritating the gastric mucosa. It is safe even in children.

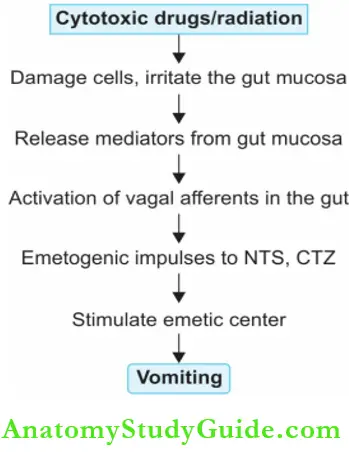
Pathophysiology of drug-induced vomiting:
Some Emetic Drugs:
- Most anticancer drugs cisplatin, methotrexate
- Levodopa, bromocriptine, and other dopamine agonists
- Morphine and other opioids
- Cholinomimetic drugs
- Metronidazole
- Ergot alkaloids
- Chloroquine, emetine
Antiemetics
Antiemetics are drugs used in the prevention and treatment of vomiting.
- Vomiting is a protective mechanism aimed at eliminating unwanted harmful material from the stomach.
- But in some situations, vomiting may not serve any useful purpose and may only be troublesome.
- It can cause dehydration, weakness, and electrolyte imbalance. In such circumstances, vomiting needs to be suppressed with drugs.
Antiemetics Classification:
- Dopamine D2 antagonists (prokinetics): Metoclopramide, domperidone
- 5-HT3 antagonists: Ondansetron, granisetron, dolasetron, tropisetron, palanosetron 3.
- Antimuscarinics: Hyoscine, promethazine, cyclizine, diphenhydramine
- Neuroleptics: Chlorpromazine, prochlorperazine, haloperidol
- Neurokinin receptor antagonists: Aprepitant, fosaprepitant
- Others: Glucocorticoids—Cannabinoids—dronabinol, nabilone
Dopamine D2 Antagonists:
- Metoclopramide and domperidone act centrally by blocking dopamine D2 receptors in the CTZ and thereby preventing vomiting.
- They enhance the tone of the lower esophageal sphincter and increase gastric peristalsis they are prokinetics.
5-HT3 Antagonists:
Ondansetron:
- 5-hydroxytryptamine released in the gut is an important inducer of emesis and the nerve endings including vagal afferents in the gut are rich in 5-HT3 receptors.
- Anticancer drugs, radiation therapy, and infection of the GI mucosa induce the release of 5-HT in the gut which initiates emetic reflex through 5-HT3 receptors present in the gut, nucleus tractus solitaries (NTS), and area postrema in the brain.
- Ondansetron blocks 5-HT3 receptors in the GI tract, CTZ and
- NTS and prevents vomiting. It is a powerful antiemetic and can be given orally or IV (4–8 mg).
- Oral bioavailability is 60–70%, t½ 3–5 hours, and duration of action 4–12 hours.
5-HT3 Antagonists Pharmacokinetics:
- 5-HT3 antagonists are well absorbed from the gut, metabolized in the liver by microsomal enzymes, and excreted by the kidneys. They can be given orally, IM, and IV.
- Dose reduction may be required in liver dysfunction.
- Dose: Ondansetron 4–24 mg in one or 2 divided doses.
5-HT3 Antagonists Adverse effects:
- All 5-HT3 antagonists are well-tolerated with minor adverse effects like headache, constipation, abdominal discomfort, and rashes.
- Dolasetron may prolong QT interval and should be avoided in patients with prolonged QT interval.
- Granisetron, dolasetron, palanosetron, and tropisetron are all given once daily.
- Dose: Granisetron 1–2 mg OD: 10 µg/ kg IV.
5-HT3 Antagonists Uses:
- To control vomiting induced by anticancer drugs or radiotherapy—given IV 30 minutes before or orally 1 hour before starting chemotherapy.
- From day 2 may be given orally (ondansetron 8 mg BD for 3–7 days).
- To prevent postoperative vomiting, a 5-HT3 blocker is given IV (4 – 8 mg ondansetron) before induction and the dose is repeated after 8 hours if required.
- Drug-induced vomiting (not effective in motion sickness).
Antimuscarinics
Hyoscine is a labyrinthine sedative very effective in motion sickness. Hyoscine also relaxes the gastrointestinal smooth muscle.
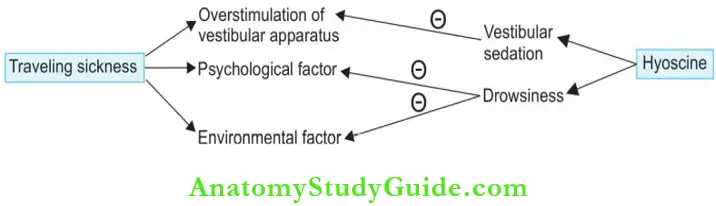
- Taken 30 minutes before the journey, hyoscine (0.4–0.6 mg oral) acts for 6 hours and the dose should be repeated if the journey is longer than that.
- A transdermal patch applied behind the ear delivers hyoscine constantly over 3 days. Sedation and dry mouth are common side effects.
Dicyclomine:
Dicyclomine is used to control vomiting (10–20 mg oral) in morning sickness and motion sickness.
H1 antihistamines:
- H1 antihistamines like promethazine, diphenhydramine, doxylamine, cyclizine, and cinnarizine have anticholinergic properties.
- They block H-receptors in the area postrema as well as muscarinic receptors in the CNS. They may also act on the GI tract. Some of them are useful in motion sickness and postoperative vomiting.
- Doxylamine is available in combination with pyridoxine for ‘morning sickness’ in some countries. Though some studies have shown it to be free of teratogenic potential, its safety is not proved and therefore, not used for the purpose in some countries.
- Dose: Doxylamine 10 mg + Pyridoxine 10 mg tab.
Neuroleptics:
- Neuroleptics like prochlorperazine block D2-receptors in the CTZ and are useful in vomiting due to other causes except motion sickness.
- Sedation and extrapyramidal symptoms are the common side effects. Prochlorperazine (5–25 mg) is used as an antiemetic and is also effective in vertigo associated with vomiting.
Neurokinin Receptor Antagonists:
- Aprepitant and fosaprepitant block the neurokinin (NK1) receptor in the area postrema and act as antiemetics.
- Aprepitant is available for oral use, while fosaprepitant is given IV and gets converted to aprepitant in the body.
- Aprepitant has a t½ of 12 hours.
- It is metabolized in the liver by microsomal enzymes CYP3A4 and may compete with other drugs metabolized by the same pathway.
- NK1 antagonists may cause dizziness, weakness, and diarrhea.
Neurokinin Receptor Uses:
- Prevention of chemotherapy-induced vomiting in combination with a 5-HT3 antagonist and a glucocorticoid.
- The efficacy of the combined regimen is more than the individual drugs.
- Dose: Aprepitant 125 mg 1 hour before chemotherapy followed by 80 mg daily for the next two days.
Other Antiemetics:
1. Glucocorticoids:
- Used in combination with other antiemetics like ondansetron or metoclopramide to control. Control delayed vomiting following anticancer drug therapy.
- Their mode of action is not clear but may activate the glucocorticoid receptors in the NTS.
2. Pyridoxine (vitamin B6):
- It is used in the prevention of vomiting in pregnancy without any known pharmacological basis.
- The proposed rationale is that pyridoxine serves as a cofactor in GABA synthesis and GABA acting as the inhibitory neurotransmitter at CTZ may suppress vomiting. Dose: 20–60 mg.
3. Cannabinoids:
- Dronabinol, a cannabinoid is ∆9 tetrahydrocannabinol. It stimulates the cannabinoid receptors (CB1) in the vomiting center. It also increases appetite. Dronabinol is orally effective and almost completely absorbed in oral administration.
- Dronabinol can cause hallucinations, euphoria, dysphoria, behavioral abnormalities, dependence, increased appetite, dryness of mouth, and hypotension.
4. Nabilone: Nabilone is similar to dronabinol.
5. Sedative hypnotics:
- Benzodiazepines raise the threshold for vomiting by depressing the CNS.
- Their anxiolytic and sedative properties also help.
- Sedative hypnotics are used as adjuvants in treating anticancer drug-induced vomiting.
6. Propofol: The general anesthetic propofol has useful antiemetic properties.
Propofol Uses:
- Prevention of anticancer drugs-induced vomiting in combination with other antiemetics when other drugs are ineffective.
- To enhance appetite as an appetite stimulant.
Antiemetic Combinations:
Severe retching and vomiting like that induced by anticancer drugs are treated with a combination of antiemetics including ondansetron, metoclopramide, glucocorticoids, and sedative-hypnotics.
Preferred drugs for vomiting due to various causes:
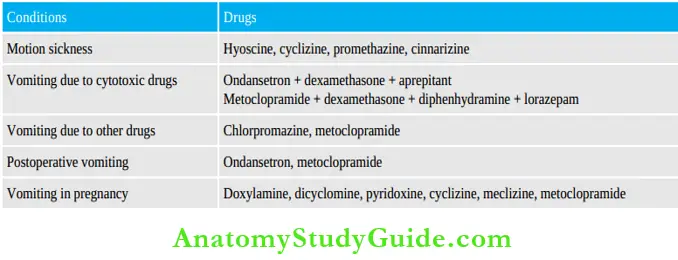
Anticancer drug regimens particularly later cycles can cause ‘anticipatory’ vomiting, i.e. vomiting at the sight or even the thought of receiving anticancer drugs. This can be avoided by using appropriate antiemetics in the earlier cycles of anticancer therapy and the use of sedatives.
Prokinetic Agents
Drugs that enhance gastroduodenal motility and hasten gastric emptying are called prokinetic agents.
They are:
- Prokinetics:
- D2 antagonists
- Metoclopramide, domperidone
- Others:
- Cisapride, mosapride, itopride
- Cholinomimetics—bethanechol
- Anticholinesterases—neostigmine
- Motilin receptor agonists—erythromycin
Metoclopramide Actions:
GIT:
- Metoclopramide promotes forward movement of contents of the upper GI tract— increases esophageal and gastric peristalsis.
- It raises lower esophageal sphincter pressure, speeds up gastric emptying, and prevents the reflux of stomach contents into the esophagus. It thus prevents reflux esophagitis. Prokinetics have no significant effects on the motility of the small intestine and the colon.
CNS:
- Metoclopramide acts as an antiemetic by blocking the dopamine D2 receptors on the CTZ.
- The effect on the gut, i.e. speeding up gastric emptying also contributes.
Metoclopramide Mechanism of Action:
Metoclopramide acts through both dopaminergic and serotonergic receptors.
1. D2 blockade:
- Stimulation of dopamine receptors in the gut particularly upper GIT, inhibits cholinergic stimulation of the gastrointestinal smooth muscle relaxes the stomach, lower esophageal sphincter (LES), and delays gastric emptying.
- Metoclopramide blocks the D2 receptors causing a reversal of these effects, i.e. it increases gastric peristalsis, and LES tone with faster gastric emptying.
- Blocking the D2 receptors in the CTZ is responsible for antiemetic actions.
2. Serotonergic receptors:
- 5-HT4 agonist—metoclopramide stimulates the 5-HT4 receptors on the gut which increases the release of acetylcholine from myenteric motor neurons.
- 5-HT3 antagonist—in high doses, metoclopramide blocks 5-HT3 receptors on inhibitory myenteric interneurons which can increase ACh release in the gut.
- Blockade of 5-HT3 receptors in the NTS and CTZ adds to the antiemetic effects.

Metoclopramide Pharmacokinetics:
- Metoclopramide is rapidly absorbed on oral administration crosses the blood–brain barrier, and placenta, and is also secreted in the milk.
- The onset of action is almost immediate (1–2 minutes) after IV injection while it takes 30–60 minutes after oral intake. Dose: 10 mg TDS.
Metoclopramide Adverse effects:
- Sedation, restlessness, anxiety, and diarrhea are seen.
- Dopamine receptor blockade results in gynecomastia, galactorrhea, and extrapyramidal symptoms with dystonia, tardive dyskinesia, and on long-term use, symptoms of parkinsonism can occur.
Metoclopramide Drug Interactions:
- Metoclopramide → blocks the D2 receptors hence → blocks the effects of levodopa.
- Gastric emptying is faster and thereby absorption of drugs like diazepam is also faster.
Metoclopramide Uses:
- Gastro-oesophageal reflux disease (GERD)—‘heartburn’ due to reflux of acid into the esophagus is benefited by prokinetic agents; used as adjuvants. Prokinetics also help some patients with non-ulcer dyspepsia.
- As antiemetics in the postoperative period, vomiting due to anticancer drugs and radiotherapy, in vomiting due to gastrointestinal disorders and migraine—metoclopramide is an effective antiemetic.
- As pre-anesthetic medication to promote gastric emptying and thereby prevent aspiration before emergency induction of general anesthesia.
- In endoscopy to assist the passage of tubes into the duodenum.
- Delayed gastric emptying: In patients undergoing surgeries like vagotomy and antrectomy and in diabetic gastroparesis, gastric emptying may be delayed—prokinetics are useful.
Domperidone:
- Domperidone is a dopamine D2 receptor blocker like metoclopramide. It blocks the dopamine receptors in the CTZ and thereby acts as an antiemetic.
- Advantages over metoclopramide are— domperidone does not cross BBB and hence extrapyramidal and neuropsychiatric side effects are rare.
- Because CTZ is outside the BBB, domperidone can act as an antiemetic.
- Dose: 10–40 mg TDS.
- Side effects are rare and include headache, dryness of mouth, diarrhea, and rashes— domperidone is well-tolerated.
Domperidone Uses: Domperidone can be used in place of metoclopramide and is often preferred over it.
- Cisapride: Cisapride enhances gastric motility by promoting the release of acetylcholine in the gut wall. However, it is now banned because it can cause cardiac arrhythmias.
- Mosapride and renzapride: Mosapride and renzapride do not produce cardiac arrhythmias and do not prolong QT interval—hence can be used.
- Itopride: Itopride blocks dopamine D2 receptors like metoclopramide and also enhances ACh levels in the gut (cholinesterase inhibitor). It promotes gastric motility and also has antiemetic effects. It is given in the dose of 50 mg TDS.
Domperidone Adverse effects:
Include headache, dizziness, and gastrointestinal disturbances. Itopride can be used in the treatment of gastroparesis, GERD, and dyspepsia.
Cholinomimetic drugs:
- Like bethanechol, enhance GI motility by activating M3 muscarinic receptors in the gut. They were earlier used in gastroparesis but are not preferred due to cholinergic side effects.
- Anticholinesterase drug neostigmine also enhances gastrointestinal motility and promotes colonic evacuation.
- It is used in the dose of 2 mg IV in acute colonic pseudo-obstruction (Ogilvie’s syndrome) to empty the colon.
Motilin receptor agonists:
- Motilin is a peptide hormone that promotes motility in the upper gastrointestinal tract. Erythromycin is a motilin receptor agonist and promotes gastric and intestinal motility.
- It has been tried in diabetic gastroparesis and in decreased small bowel motility.
Drugs Used For Constipation
Overview:
- Purgatives are drugs that promote defecation. They are also called laxatives or cathartics.
- Laxatives or aperients have milder action, while cathartics or purgatives are more powerful evacuants. Carminatives are drugs that promote expulsion of gases from the gut.
Constipation Classification:
- Bulk laxatives: Bran, plantago seeds, agar, methylcellulose, ispaghula husk
- Fecal softeners: Docusate sodium (DOSS), liquid paraffin (emollients)
- Osmotic purgatives:
- Nonabsorbable salts: Magnesium sulfate, magnesium hydroxide, sodium phosphate, sodium sulfate, magnesium citrate, sodium potassium tartrate
- Nonabsorbable sugars: Lactulose, sorbitol, polyethylene glycol.
- Stimulant purgatives: Phenolphthalein, bisacodyl, castor oil, anthraquinones
- Cascara sagrada, senna
- Others:
- 5-HT4 agonists—prucalopride, cisapride
- Opioid antagonists—methylnaltrexone, alvimopan
- Chloride channel activator—lubiprostone
Bulk Laxatives
Bulk laxatives include indigestible vegetable fiber and hydrophilic colloids that increase the volume forming a large, soft, solid stool. Dietary fiber consists of cell walls and other parts that are unabsorbable and add to the bulk of the intestinal contents, forming semisolid to solid stools.
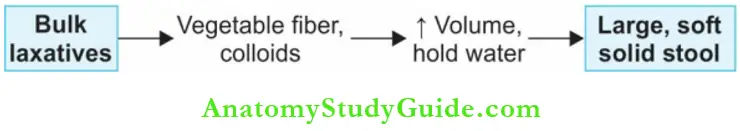
- Adding fiber to the diet is a safe and natural way of treating constipation and symptoms of IBS, viz. constipation and diarrhea.
- Adequate water intake should be stressed with all bulk laxatives.
- All of them need 1–3 days to act and all can cause allergy.
- Bulk laxatives may interfere with the absorption of other drugs.
Bran:
Bran is the residue left when flour is made from cereals and contains 40% fiber—but is unpalatable. Large quantities need to be consumed and can cause flatulence.
Ispaghula and plantago:
- Ispaghula and plantago seeds contain natural mucilage which absorbs water to form a gelatinous mass and are more palatable than bran.
- Ispaghula husk is available as a powder but should not be swallowed as dry powder to avoid esophageal impaction—may be mixed with water or milk.
- Dose: 3–12 g/day.
Methylcellulose: Methylcellulose a derivative of cellulose (4–6 g/day) holds water as it is hydrophilic.
Agar:
- Agar obtained from marine algae is a mucilaginous substance and contains indigestible hemicellulose.
- Dose: 4–5 g mixed with water.
- Bulk laxatives should be avoided in patients with stenosis or adhesions in the gut.
Bulk Laxatives Uses:
Bulk laxatives are used in
- Functional constipation—adequate intake of dietary fiber is the best measure to prevent functional constipation.
- When straining at stools is to be avoided as in hemorrhoids, fissures, and MI.
- Irritable bowel syndrome—in diarrhea they help form solid stools.
Fecal Softeners
Docusate sodium:
- Docusate sodium [dioctyl sodium sulfosuccinate, (DOSS)] is an anion detergent, that softens feces by lowering the surface tension of the intestinal contents which allows more water to be retained in the feces.
- It requires 1–3 days for action; enhances the absorption of many drugs due to its detergent action. It is unpalatable (bitter) and can cause nausea and abdominal pain.
- Dose: 100–400 mg/day.
Liquid paraffin:
- Liquid paraffin is a chemically inert mineral oil. It is not digested but lubricates and softens feces. It is unpalatable; aspiration may cause lipoid pneumonia; small amounts absorbed in the intestines may cause paraffinomas; it may leak out of the anus causing discomfort.
- Long-term use can result in a deficiency of fat-soluble vitamins due to impaired absorption—hence not preferred.
Osmotic Purgatives
Osmotic purgatives include
- Nonabsorbable salts—salts of magnesium and sodium.
- Nonabsorbable sugars—lactulose, sorbitol, lactitol, glycerine, polyethylene glycol.
Osmotic purgatives are solutes that are not absorbed in the intestine, osmotically retain water and increase the bulk of intestinal contents. They increase peristalsis to evacuate a fluid stool in m1–3 hours.
Osmotic purgatives include:

Nonabsorbable salts:
Nonabsorbable salts are osmotic or saline purgatives and are used to prepare the bowel before surgery and for food poisoning.
Nonabsorbable sugars:
- Lactulose is a synthetic disaccharide that is not absorbed, holds water, and acts as an osmotic purgative.
- Flatulence and cramps may be accompanied. In the colon, lactulose is fermented to lactic and acetic acids which inhibit the growth of colonic ammonia producing bacteria.
- It also inhibits the absorption of ammonia by lowering pH and lowers blood ammonia levels.
It is used in hepatic coma for this effect (hepatic coma is worsened by ammonia).
- Sorbitol: Sorbitol is similar to lactulose. Lactilol is another synthetic sugar more palatable than lactulose.
- Glycerine: Glycerine is used as a rectal suppository or as an enema (with an oil).
- Polyethylene glycol: Polyethylene glycol (PEG) isotonic solution containing PEG with sodium sulfate, sodium
- Chronic constipation Bulk laxatives chloride, sodium bicarbonate, and potassium chloride is given orally.
- The solution is balanced in such a way that it avoids electrolyte imbalance or fluid shift into the gut.
- Large volumes are rapidly ingested—3–4 liters over 2 hours—for cleansing the bowel before endoscopic examination of the bowel.
- PEG powder may be taken with water for chronic constipation.
- It has the advantage that there is no associated flatulence or abdominal cramps.
Stimulant Purgatives:
- Stimulant purgatives increase intestinal motility and increase the secretion of water and electrolytes by the mucosa.
- They may cause abdominal cramps.
Bisacodyl:
- Bisacodyl related to phenolphthalein is converted to an active metabolite in the intestines which stimulates the colon.
- It can be given orally (5–10 mg enteric coated tab—takes 8–12 hours for stools to be passed) but usually is used as rectal suppositories (10 mg) which results in defecation in 15–40 minutes.
- There is wide variation in the dose needed. It is a popular laxative and is safe except that prolonged use may cause mild proctitis and a burning sensation in the rectum since it is an irritant. Hence bisacodyl should not be used for more than 10 days at a time.
Leakage of the suppository can sometimes result in anal soreness.
- Dulcolax 5 mg tab, 10 mg suppository.
- Sodium picosulfate is similar to bisacodyl.

Phenolphthalein:
- Phenolphthalein indicator acts on the colon after 6–8 hours to produce soft, semiliquidstools with some griping.
- It undergoes enterohepatic circulation which prolongs its actions.
- Allergic reactions including pink-colored skin eruptions, other severe forms of allergy, and risk of cardiac toxicity and colic limit its use.
- Anthraquinones like cascara sagrada and senna (source: Plants) are given orally, active anthraquinones are liberated in the intestines and stimulate the myenteric plexus in the colon.
- Evacuation takes 6–8 hours.
- Long-term use causes melanotic pigmentation of the colon.
Castor oil:
- Castor oil is hydrolyzed in the upper small intestine to ricinoleic acid, a local irritant that increases intestinal motility.
- It is a powerful and one of the oldest purgatives.
- The stool is semiliquid and is accompanied by griping. It is not preferred.
Choice of purgatives:

Other Laxatives
- Chloride channel activators: Lubiprostone is a derivative of prostanoic acid. It stimulates the opening of the chloride channels in the small intestine leading to the secretion of a fluid rich in chloride. This in turn stimulates intestinal motility and promotes evacuation within 24 hours. It is indicated in chronic constipation and irritable bowel syndrome.
- Opioid antagonists: Opioid-induced constipation can be troublesome in cancer patients and terminally ill patients receiving opioids for pain relief over long periods. Methylnaltrexone and alvimopan are opioid antagonists which block the opioid receptors in the gut. They do not cross the BBB and therefore, do not antagonize the analgesic effects of opioids.
- Enema: Enema produces defecation by softening stools and distending the bowel. Evacuant enema is used to prepare the gut for surgery, endoscopy, and radiological examination
Drug-Induced Constipation
Drugs like anticholinergics, NSAIDs, opioids, clonidine, iron, calcium channel blockers; antihistamines and tricyclic antidepressants (due to anticholinergic effect) can cause constipation. When withdrawal of the causative agent is not possible, a laxative may be used.
Laxative abuse:
- Habitual use of laxatives especially stimulant laxatives may lead to various gastrointestinal disturbances like irritable bowel syndrome, loss of electrolytes, loss of calcium in the stool, and malabsorption.
- Misconceptions regarding bowel habits should be cleared.
- The patient should be convinced that normal bowel habits may vary between 3 stools daily and 2 stools per week.
Contraindications: Laxatives are contraindicated in:
- Intestinal obstruction
- Patients with undiagnosed acute abdomen.
Drugs Used In The Treatment Of Diarrhea
Question 5. Write a short note:
Answer:
- ORS
- Antidiarrheal drugs.
Answer:
Diarrhea is the frequent passage of liquid stools. It can be due to a variety of causes like infection, toxins, anxiety, and drugs. In diarrhea, there is an increase in motility and secretions in the gut with reduced absorption of water and electrolytes.
Hence the approaches in the treatment of diarrhea include:
- Replacement of fluid and electrolytes
- Treatment of the cause
- Antidiarrheal agents.
1. Replacement of fluid and electrolytes:
Correction of fluid and electrolyte disturbances can be life-saving in most cases, especially for infants. Oral rehydration with sodium chloride, glucose, and water is useful. In the ileum, glucose, and sodium citrate enhance sodium absorption and water follows.
- Oral rehydration powders are mixed with water to make an oral rehydration solution (ORS).
- ORS with sodium bicarbonate or trisodium citrate are available used in place of bicarbonate because the use of citrate makes ORS more stable, absorption of glucose is better and stool output is lower. If the
- ORS readymade powder is not available, a mixture of 5 g table salt (a pinch) with 20 g sugar dissolved in one liter of boiled and cooled water may be used till regular ORS is available. In severe degrees of dehydration, IV fluids should be started.
Composition of oral rehydration salt/solution (ORS):

Dose and Frequency of Administration:
- Mild dehydration: 50 mL/kg over 4–6 hours in multiple small divided doses.
- Moderate dehydration: 100 mL/kg over 4–6 hours in multiple small divided doses.
The adequate maintenance dose should be given based on the severity:
New formula (WHO):
- NaCl – 2.6 g
- KCl – 1.5 g
- Trisodium citrate – 2.9 g
- Glucose – 13.5 g
- Water – 1 L
- Total osmolarity – 245 mOsm/liter
WHO-ORS modified formula:
- ORS with lower osmolality has improved efficacy with reduced incidence of vomiting and stool volume.
- WHO and UNICEF have, therefore, recommended a modified ORS solution with 245 mOsm/L osmolarity in place of the standard preparation (310 m Osm/L) with a decreased concentration of sodium and glucose.
WHO-ORS Disadvantages:
It can cause hyponatremia in adults suffering from cholera.
Super ORS:
- Amino acids are added which could promote sodium absorption but is expensive and the benefit provided is marginal.
- Boiled rice powder 40–50 g/liter is a good and simple glucose supplement. Since rice also has some proteins (7%), it is a source of amino acids which stimulates the absorption of salt and water.
- The starch content adds to the calories. Rice is easily available, is relatively inexpensive, and has good efficacy rice-based ORS may be preferred particularly in developing countries. Wheat, maize, or potato may be used instead of rice.
Some Drugs that Produce Diarrhoea:
- Ampicillin
- Erythromycin
- Colchicine
- Prostaglandins and their analogs
- Emetine
- Anticholinesterases like physostigmine
- Mosapride
- Some anticancer drugs
- Digitalis
- Lithium
- Magnesium sulfate (oral)
ORS Uses:
- Diarrhea
- For rehydration needed in heatstroke
- Burns
- Following surgery or trauma
2. Treatment of the cause:
- Acute diarrhea could often be due to viral, bacterial, or protozoal infection.
- The pathogen should be identified whenever possible and treated accordingly.
- Gastroenteritis is often due to viruses and does not require antibiotics.
- Mild bacterial gastroenteritis is also self-limiting but some infections like typhoid, cholera, and amoebic dysentery need suitable antibiotics.
3. Antidiarrheal Drugs:
Antidiarrheal drugs provide only symptomatic relief.
They are:
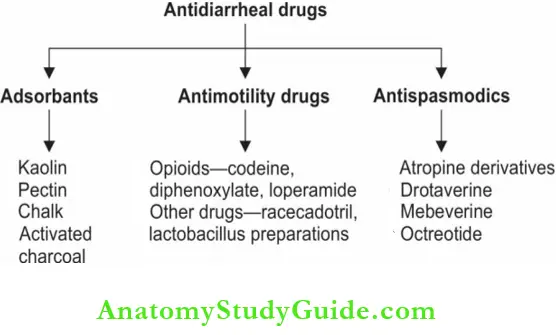
Classification adsorbents:
- Kaolin, is a natural compound containing hydrated magnesium and aluminum silicate, while pectin is the sugar obtained from apples.
- These adsorb intestinal toxins and microorganisms by coating them.
- They are not absorbed and have no prominent side effects but they interfere with the absorption of other drugs → hence a2 hour gap is required after administration of other drugs.
Antimotility Drugs
Opioid agonists:
Codeine an opium alkaloid, stimulates the opioid receptors on the gastrointestinal smooth muscles to reduce peristalsis. This delays the passage of intestinal contents and facilitates the absorption of food.
Diphenoxylate and loperamide:
Diphenoxylate and loperamide are opioids— µ agonists with selective action on the gut. They are given a small dose of atropine in order to discourage abuse if taken repeatedly at short intervals, side effects of atropine would appear. In therapeutic doses, CNS effects are not prominent.
- They are less sedating, less addicting, and are the most commonly used antimotility drugs.
- Loperamide is longer-acting than diphenoxylate; it also has weak anticholinergic properties.
- Its low solubility in water discourages abuse by injection. The onset of action is in 1–2 hours and the duration of action is almost 12–18 hours.
- Both loperamide and diphenoxylate may cause nausea, vomiting, and abdominal cramps.
- They can cause paralytic ileus, abdominal distension, and toxic megacolon, and several fatalities are reported in children. Hence loperamide and diphenoxylate are contraindicated in children below 4 years of age.
Dose: 4 mg followed by 2 mg after each stool up to a maximum of 10 mg/day.
Question 6. Explain why loperamide should be avoided in infective diarrheas.
Answer:
Diarrhea Uses: Antimotility drugs are used for symptomatic treatment of noninfective diarrheas (as adjuvants).
Antimotility drugs should be avoided in infective diarrheas due to invasive pathogens for the following reasons:
- They increase the risk of systemic invasion by the pathogen.
- Risk of intestinal perforation.
- Delayed clearance of the infecting organisms.
- Risk of megacolon.
Other Drugs:
Racecadotril:
- Enkephalins are opioids produced in the body and are degraded by enkephalinases. Racecadotril, a new antidiarrheal is a prodrug converted to thiorphan which is a selective inhibitor of enkephalinase in the gut and peripheral tissues and thereby increases enkephalin labels.
- Enkephalins are neurotransmitters in the gut—they have antisecretory activity on the intestines (act on opioid receptors)—thus correcting the hypersecretion of water and
electrolytes seen in diarrhea without reducing intestinal motility.
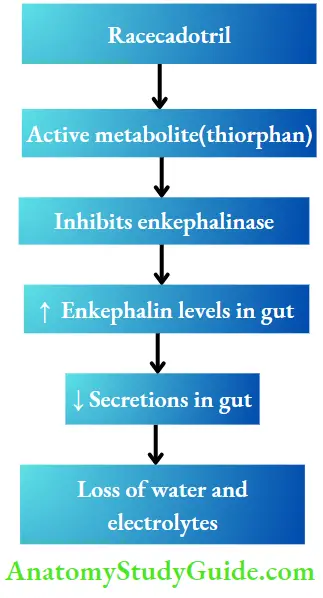
- The onset of action is quick, and pain and distension subsides. It is not contraindicated in children. (but loperamide is contraindicated in children).
- Racecadotril is well-tolerated with minor adverse effects like drowsiness, skin rashes, nausea, and flatulence. Should be used for short-term—not >7 days. Dose: 100 mg TDS. It is now commonly used as antidiarrheal.
Lactobacillus preparations:
- Lactobacillus acidophilus and Lactobacillus sporogenes colonize the intestines and promote the growth of saccharolytic flora and alter the gut pH so that the growth of pathogenic organisms is inhibited.
- They are probiotics and reduce the incidence of antibiotic-induced diarrhea.
- Curd and buttermilk are cheaper alternatives to lactobacilluspreparations.
Antispasmodics:
- Diarrhea is often associated with abdominal colic and pain. Antispasmodics may be required to relieve the pain. Atropine derivatives like propantheline and dicyclomine, relax gastrointestinal smooth muscles and relieve abdominal colics.
- Drotaverine related to papaverine is a directly acting smooth muscle relaxant and also has analgesic properties. It acts by inhibiting the enzyme
- PDE and thereby increasing cAMP/cGMP levels which cause smooth muscle relaxation. It is used as an antispasmodic in renal, biliary, and intestinal colic and also in IBS and dysmenorrhea. Adverse effects are headache, dizziness, flushing, and constipation.
- Dose: 40–80 mg TDS.
Mebeverine:
- Mebeverine a reserpine derivative, is an antispasmodic acting both directly on the gut smooth muscle and indirectly to reduce colonic hypermotility.
- It reduces the permeability of smooth muscles for sodium ions and also decreases the efflux of potassium ions.
- Given orally it is rapidly and completely absorbed. Adverse effects include dizziness, headache, constipation, and some gastritis but is devoid of anticholinergic side effects. ‘
- Dose: 135 mg TDS.
Octreotide: Octreotide is a long-acting, synthetic analog of somatostatin. Its actions on the gut are:
- Reduces GI motility and fluid secretion.
- Inhibits the secretion of various hormones like gastrin, secretin, cholecystokinin, growth hormone, insulin, glucagon, 5-HT, pancreatic polypeptide, and vasoactive intestinal peptide.
- Octreotide is used subcutaneously in gastrointestinal secretory tumors causing diarrhea and in diarrhea due to vagotomy, dumping syndrome, and AIDS.
Traveler’s Diarrhea:
Infection is the most common cause of traveler’s diarrhea and should be treated with suitable antimicrobials like doxycycline or ciprofloxacin. Oral rehydration salts may also be used.
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is characterized by abnormal bowel functions with no specific organic cause.
- Diarrhea or constipation with abdominal pain may be present. Causes could be stress, lack of dietary fiber, food allergy, or emotional disturbances.
- When constipation is prominent, soluble dietary fiber like is paghula is recommended, while loperamide is preferred for diarrhea.
- Benzodiazepines relieve anxiety and other measures are taken depending on the symptoms and probable cause. Newer antidepressants have shown good responses in several studies.
Alosetron:
- Blocks the 5-HT3 receptors in the gut and inhibits reflex activation of the GI smooth muscle and thus reduces colonic motility.
- It is longer acting than other 5-HT3 antagonists like ondansetron used in vomiting.
- Alosetron may be used in women having IBS with prominent diarrhea—not responding to other drugs.
- Adverse effects include constipation and colitis.
Linaclotide:
- Linaclotide reduces the activation of colonic sensory neurons thereby reducing pain. It also activates motor neurons in the intestines resulting in chloride-rich intestinal secretions.
- It is a second-line drug in constipation associated with IBS.
Antispasmodics:
For relief of pain associated with food intake, antispasmodics, like dicyclomine (inhibit gastrocolic reflex) and mebeverine may help.
Inflammatory Bowel Diseases
Inflammatory bowel diseases (IBD) like ulcerative colitis and Crohn’s disease are treated with glucocorticoids, sulfasalazine, and immunosuppressants.
- Glucocorticoids: For IBD involving the rectum or sigmoid colon, prednisolone retention enema or other rectal preparations may be used. Budesonide controlled-release oral formulations which release the drug in the distal bowel (distal ileum and colon) are tried.
- Sulfasalazine: Sulfasalazine is split by flora in the colon to 5-aminosalicylate (5-ASA) and sulfapyridine. Adverse effects are common and are mostly due to sulfapyridine. Nausea, vomiting, fever, headache, diarrhea, megaloblastic anemia, and various allergic manifestations ranging from skin rashes to Stevens-Johnson syndrome can occur.
- Mesalamine: Mesalamine is 5-ASA which is better tolerated with minor side effects. Mesalamine retention
enema and suppositories are used. - Immunosuppressants: Immunosuppressants like azathioprine, 6-mercaptopurine and methotrexate are used for induction and maintenance of remission in patients with active IBD.
- Antitumor necrosis factor (anti-TNF) therapy: In IBD, TNF is an important proinflammatory cytokine. Infliximab, adalimumab, and certolizumab are monoclonal antibodies to TNF indicated in moderate to severe Crohn’s disease and ulcerative colitis.
Leave a Reply