Intracellular Accumulations
Intracellular accumulation of substances in abnormal amounts can occur within the cytoplasm (especially lysosomes) or nucleus of the cell. This phenomenon was previously referred to as infiltration, meaning thereby that something unusual has infiltrated the cell from outside which is not always the case.
Read And Learn More: General Pathology Notes
Intracellular accumulation of the substance in mild degree causes reversible cell injury while more severe damage results in irreversible cell injury.
Abnormal intracellular accumulations can be divided into 3 groups:
- Accumulation of constituents of normal cell metabolism produced in excess, for example, Accumulations of lipids (fatty change, cholesterol deposits), proteins and carbohydrates.
- Accumulation of abnormal substances produced as a result of abnormal metabolism due to lack of some enzymes, for example, Storage diseases or inborn errors of metabolism.
- Accumulation of pigments for example, Nendogenous pigments under special circumstances, and exogenous pigments due to lack of enzymatic mechanisms to degrade the substances or transport them to other sites.
Excessive Intracellular Accumulation Of Normal Constituents:
These substances accumulate inside the cell when they are produced in excess e.g. fats, proteins and carbohydrates.
Fatty Change (Steatosis):
Fatty change, steatosis or fatty metamorphosis is the intracellular accumulation of neutral fat within parenchymal cells. The deposit is in the cytosol and represents an absolute increase in the intracellular lipids.
Fatty change is particularly common in the liver but may occur in other nonfatty tissues as well e.g. in the heart, skeletal muscle, kidneys (lipoid nephrosis or minimum change disease) and other organs.
Fatty Liver:
The liver is the most common site for the accumulation of fat because it plays a central role in fat metabolism. Depending upon the cause and amount of accumulation, fatty change may be mild and reversible, or severe producing irreversible cell injury and cell death.
Aetiology of Normal Constituents:
Fatty change in the liver may result from one of the two types of causes:
- Conditions with excess fat: These are conditions in which the capacity of the liver to metabolise fat is exceeded for example,
- Obesity
- Diabetes mellitus
- Congenital hyperlipidaemia
- Liver cell damage: These are conditions in which fat cannot be metabolised due to liver cell injury for example,
- Alcoholic liver disease (most common)
- Starvation
- Protein calorie malnutrition
- Chronic illnesses (for example, Tuberculosis)
- Acute fatty liver in late pregnancy
- Hypoxia (for example, Anaemia, cardiac failure)
- Hepatotoxins (for example, Carbon tetrachloride, chloroform, ether, aflatoxins and other poisons)
- Drug-induced liver cell injury (for example, Administration of methotrexate, steroids, CCl4, halothane anaesthetic, tetracycline etc)
- Reye’s syndrome
Pathogenesis of Normal Constituents:
The mechanism of a fatty liver depends upon the stage at which the etiologic agent acts in normal fat transport and metabolism. Hence, the pathogenesis of fatty liver is best understood in the light of normal fat metabolism in the liver
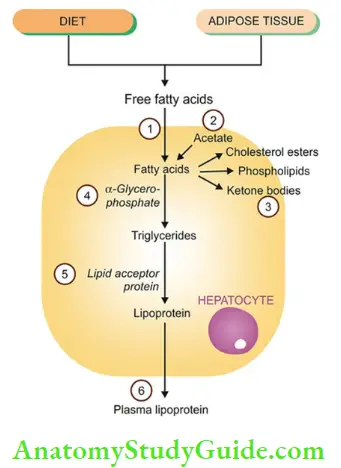
Lipids as free fatty acids enter the liver cell from either of the following 2 sources:
- From diet as chylomicrons (containing triglycerides and phospholipids) and as free fatty acids.
- From adipose tissue as free fatty acids.
- Normally: Besides the above two sources, a small part of fatty acids is also synthesised from acetate in the liver cells.
- Most free fatty acid is esterified to triglycerides by the action of α- glycerophosphate and only a small part is changed into cholesterol, phospholipids and ketone bodies.
- While cholesterol, phospholipids and ketones are used in the body, intracellular triglycerides are converted into lipoproteins, which require ‘lipid acceptor protein’.
- Lipoproteins are released from the liver cells into circulation as plasma lipoproteins (LDL, VLDL).
- In fatty liver: Intracellular accumulation of triglycerides occurs due to defect at one or more of the following 6 steps in the normal fat metabolism shown given in below
- Increased entry of free fatty acids into the liver.
- Increased synthesis of fatty acids by the liver.
- Decreased conversion of fatty acids into ketone bodies resulting in increased esterification of fatty acids to triglycerides.
- Increased α-glycerophosphate causes increased esterification of fatty acids to triglycerides.
- Decreased synthesis of ‘lipid acceptor protein’ resulting in decreased formation of lipoprotein from triglycerides.
- Block in the excretion of lipoprotein from the liver into plasma.
- In most cases of fatty liver, one of the above mechanisms is operating.
- But liver cell injury from chronic alcoholism is multifactorial and involves the following metabolic abnormalities:
- Increased lipolysis
- Increased free fatty acid synthesis
- Decreased triglyceride utilisation
- Decreased fatty acid oxidation to ketone bodies
- Block in lipoprotein excretion from the liver
Even a severe form of fatty liver may be reversible if the liver is given time to regenerate and progressive fibrosis has not developed. For example, intermittent drinking is less harmful because the liver cells, which have tremendous regenerative capacity, get time to recover.
Similarly, in a chronic alcoholic who becomes a teetotaller, the enlarged fatty liver may return to normal if fibrosis has not developed.
Morphologic Features of Normal Constituents:
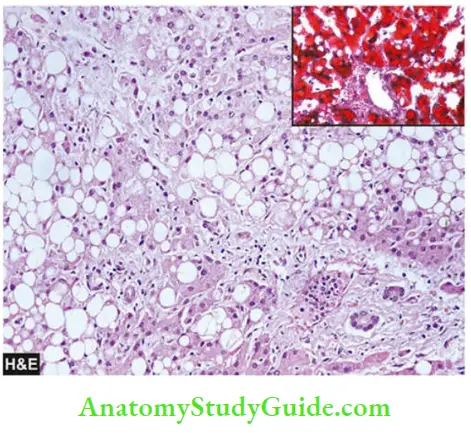
- Grossly: The liver in fatty change is enlarged with a tense, glistening capsule and rounded margins. The cut surface bulges slightly and is pale yellow to yellow and is greasy to the touch.
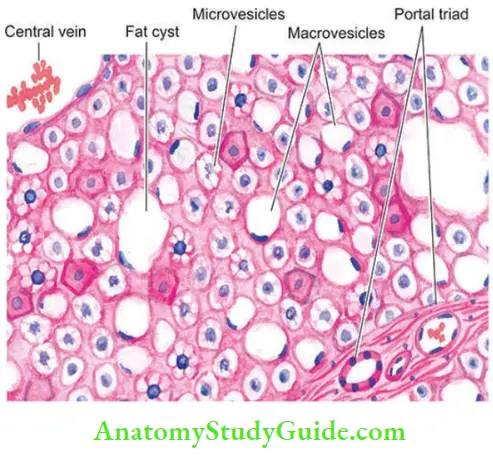
- Microscopically: A characteristic feature is the presence of numerous lipid vacuoles in the cytoplasm of hepatocytes. This is because the fat in the H and E stained section prepared by the paraffin embedding technique is dissolved in organic solvents used and appears as non-staining vacuoles.
- The vacuoles are initially small and are present around the nucleus (microvesicular).
- With the progression of the process, the vacuoles become larger pushing the nucleus to the periphery of the cells (macrovesicular).
- At times, the hepatocytes laden with large lipid vacuoles may rupture and lipid vacuoles coalesce to form fatty cysts.
- Infrequently, lipo granulomas may appear as a reaction to extravasated fat and consist of collections of lymphocytes, macrophages, and some multinucleated giant cells.
- Fat can be demonstrated in fresh unfixed tissue by frozen sections with fat stains for example,
- Sudan dyes (Sudan III, IV, Sudan Black) and Oil Red O. Alternatively, osmic acid which is a fixative as well as a stain can be used to demonstrate fat in the tissue.
Cholesterol Deposits:
Intracellular deposits of cholesterol and its esters in macrophages may occur when there is hypercholesterolaemia. This turns macrophages into foam cells.
The examples are as follows:
- Fibrofatty plaques of atherosclerosis
- Clusters of foam cells in tumour-like masses called xanthomas and xanthelasma.
- Cholesterolosis is the focal presence of cholesterol-laden macrophages in the lamina propria of the gallbladder in cholelithiasis.
Stromal Fatty Infiltration:
This form of lipid accumulation is quite different from the parenchymal fatty change just described. Stromal fatty infiltration is the deposition of mature adipose cells in the stromal connective tissue in contrast to intracellular deposition of fat in the parenchymal cells in fatty change.
The condition occurs most often in patients with obesity. Two commonly affected organs are the heart and the pancreas. Thus, the heart can be the site for intramyocardial fatty change as well as epicardial (stromal) fatty infiltration.
The presence of mature adipose cells in the stroma generally does not produce any dysfunction.

Intracellular Accumulation Of Proteins:
Pathologic accumulation of proteins in the cytoplasm of cells may occur in the following conditions:
- In proteinuria, there is excessive renal tubular reabsorption of proteins by the proximal tubular epithelial cells which show pink hyaline droplets in their cytoplasm in H and E-stained sections.
- The change is reversible; with control of proteinuria, the protein droplets disappear.
- The cytoplasm of actively functioning plasma cells shows pink hyaline inclusions called Russell’s bodies representing synthesised immunoglobulins.
- In α1-antitrypsin deficiency, the cytoplasm of hepatocytes shows eosinophilic globular deposits of a mutant protein.
- Mallory’s body or alcoholic hyaline in the hepatocytes is an intracellular accumulation of intermediate filaments of cytokeratin and appears as amorphous pink masses.
- It may be stated here that amyloid is primarily an extracellular deposition of abnormal proteinaceous substance but in advanced diseases, it may be deposited in intracellular locations too.
Intracellular Accumulation Of Glycogen:
Conditions associated with excessive accumulation of intracellular glycogen are as under:
1. In diabetes mellitus, there is intracellular accumulation of glycogen in different tissues because normal cellular uptake of glucose is impaired. Glycogen deposits in diabetes mellitus are seen in the epithelium of the distal portion of the proximal convoluted tubule and descending loop of Henle, in the hepatocytes, in beta cells of pancreatic islets, and in cardiac muscle cells.
In routine H and E-stained sections, deposits of glycogen produce clear vacuoles in the cytoplasm of the affected cells. Best’s carmine and periodic acid-Schiff (PAS) staining may be employed to confirm the
presence of glycogen in the cells.
2. In glycogen storage diseases or glycogenosis, there is a defective metabolism of glycogen due to genetic disorders.
Excessive Intracellular Accumulations of Normal Constituents:
- Intracellular accumulations may occur from normal constituents of cell metabolism (for example, fats, proteins, carbohydrates), or accumulation of abnormal substances due to either absence of some metabolic enzymes, or due to pigments.
- Fatty change is a deposition of fat in the parenchymal cells of organs such as the liver, kidneys, muscle, pancreas etc.
- Fatty liver is more common and occurs from various etiologic factors, most often from alcoholic liver disease; others are obesity, diabetes, starvation, pregnancy, drugs etc.
- The mechanism for fatty liver is due to excess of free fatty acids, derived either from diet or from adipose tissues, resulting in intracellular accumulation of triglycerides in the hepatocytes.
- Fatty liver is characterised by an enlarged pale-yellow liver, having cytoplasmic vacuoles (microvesicles or macrovesicles) in the hepatocytes.
- Fat in the sections can be stained by fat stains, for example, Sudan Black, Sudan II, IV, Oil Red O and osmic acid.
- Stromal fatty infiltration is an extracellular accumulation of adipocytes.
- Intracellular accumulation of proteins may occur in tubular epithelial cells in diabetes, alcoholic hyaline in liver cells, and Russell bodies in the plasma cells.
- Intracellular glycogen accumulates in tubular cells in diabetes and in parenchymal cells in glycogen storage diseases.
Leave a Reply