Leprosy Transmission Notes
Leprosy:
Leprosy or Hansen’s disease (after discovery of the causative organism by Hansen in 1874), was first described in ancient Indian text going back to 6th Century BC, is a chronic non-fatal infectious disease.
Read And Learn More Infammation And Repair Pathology
It affects mainly the cooler parts of the body such as the skin, mouth, respiratory tract, eyes, peripheral nerves, superficial lymph nodes and testis. In leprosy, the earliest and main involvement is of the skin and nerves.
- However, in bacteraemia from endothelial colonisation or by bacilli filtered from blood by the reticuloendothelial system, other organs such as the liver, spleen, bone marrow and regional lymph nodes are also involved.
- Advanced cases may develop secondary amyloidosis and renal disease, both of which are of immunologic origin.
Causative Organism:
The disease is caused by Mycobacterium leprae which closely resembles Mycobacterium tuberculosis but the organism is less acid-fast and has characteristic neurotropism.
- The organisms in tissues appear as compact rounded masses (globi) or are arranged in parallel fashion like cigarettes-in-pack.
- M. leprae can be demonstrated in tissue sections, in split skin smears by splitting the skin, scrapings from cut edges of the dermis, and in
Nasal smears by the following techniques:
- Acid-fast (Ziehl-Neelsen or ZN) staining The staining procedure is similar to the demonstration of M. tuberculosis but can be decolourised by a lower concentration (5%) of sulphuric acid (less acid-fast).
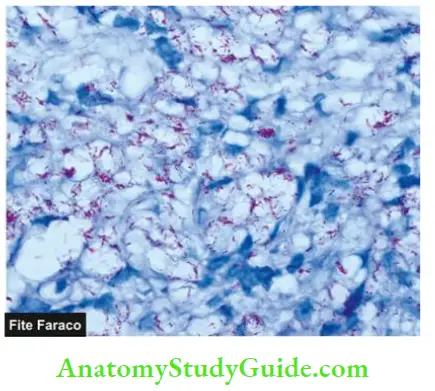
- Fite-Faraco staining This procedure is a modification of the ZN procedure and is considered better for more adequate staining of tissue sections.
- Gomori methenamine silver (GMS) staining can also be employed.
- Molecular methods, for example, PCR.
- IgM antibodies to PGL-1 antigen are seen in 95% of cases of lepromatous leprosy but only in 60% of cases of tuberculoid leprosy.
The slit smear technique gives a reasonable quantitative measure of M. leprae when stained with ZN method and examined under 100x oil objective for determining the density of bacteria in the lesion (bacterial index, BI).
- BI is scored from 1+ to 6+ (range from 1 to 10 bacilli per 100 fields to > 1000 per field) as multibacillary leprosy while BI of 0+ is termed paucibacillary.
- This forms the basis of the WHO classification of leprosy practised by field workers. Although lepra bacilli were the first bacterium identified for causing human disease, M. leprae remains one of the few bacterial species which is yet to be cultured on an artificial medium.
- The nine-banded armadillo, a rodent, acts as an experimental animal model as it develops leprosy which is histopathologically and immunologically similar to human leprosy.
Incidence:
The disease is endemic in areas with hot and moist climates and poor tropical countries. Leprosy is almost exclusively a disease in a few developing countries in Asia, Africa and Latin
- America. According to the WHO, India, Brazil and Indonesia continue to have new cases.
- India alone constitutes about 60% of new leprosy cases of all registered leprosy cases globally; the union territory of Dadra and Nagar Haveli has the highest prevalence while the state of Uttar
- Pradesh has a maximum number of cases. Very few cases are now seen in Europe and the United States.
- The WHO has launched a strategy against leprosy in 2016-2020 towards a leprosy-free world.
Mode Of Transmission:
Leprosy is a slow communicable disease and the incubation period between first exposure and appearance of signs of disease varies from 2 to 20 years (average about 3 years).
The infection may be transmitted by the following routes:
- Direct contact with untreated leprosy patients who shed numerous bacilli from damaged skin, nasal secretions, mucous membranes of mouth and hair follicles.
- Materno-foetal transmission across the placenta.
- Transmission from milk of leprosy affected mother to infant.
Leave a Reply