Concentration And dilution Of Urine
The kidney can produce a maximum urine concentration of 1400mosml/L and a minimum concentration of 30mosm/L according to body requirements. A normal human of 70 kg must excrete 600m Osmoles of solute per day. If the maximum concentrating capacity is l200mosm/l then the amount to urine that must be excreted to remove 600 mosmoles of solute is known as obligatory urine volume.
Table of Contents
Principle factors for the concentration of urine
- High antidiuretic hormones.
- Hyperosmolarity of deep medulla, which is generated and maintained by the counter-current system. It has two components.
- Countercurrent multiplier.
- Counter current exchanger.
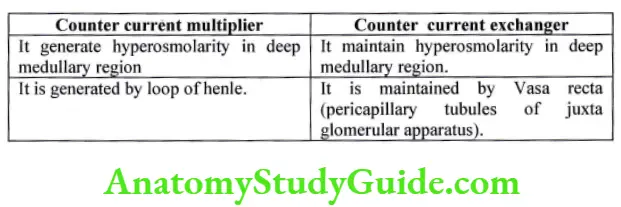
Countercurrent multiplier
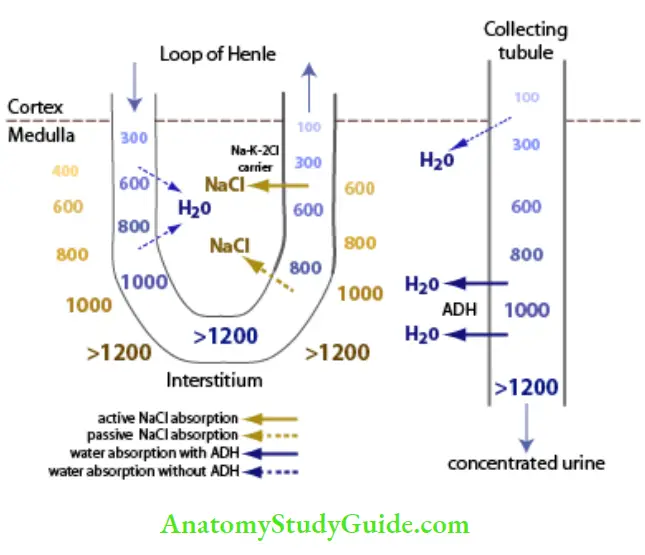
The osmolarity of interstitial fluid is 300 mOsm/l. corrected Os molar activity after considering intermolecular attraction and repulsion is 282mOsm/l. renal medullary interstitial has an osmolarity of 1200-1400 mOsm/1. it implies renal interstitial has accumulated solute above solvent (water). It is done by Countercurrent multiplier, which can be explained under two steps.
- Origin of single-effect
- Multiplication of single effect
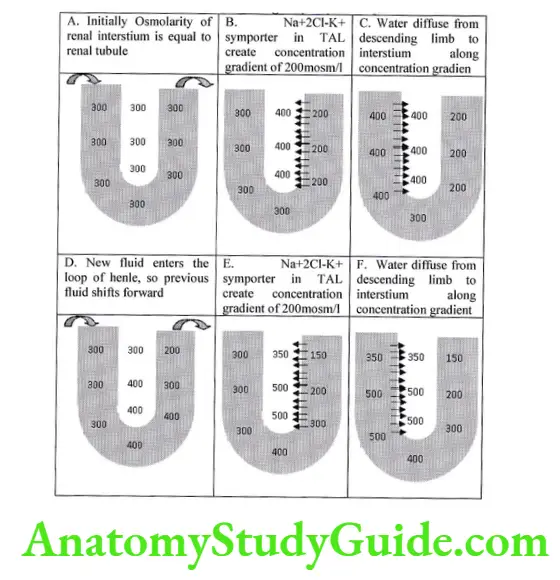
Origin of single-effect
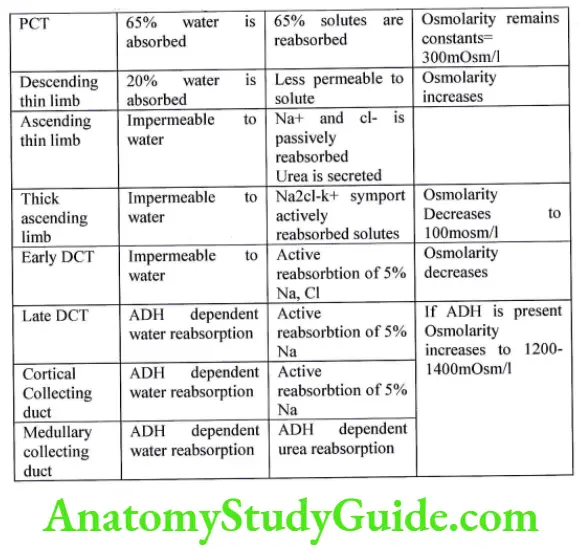
The main factor is the selective permeability of different segments of the nephron to solute and solvent.
- Active transport of solutes from thick ascending limb (TAL) of loop of henle via Na+ 2Cl-K+ Symporter. It is capable of establishing a gradient of 200mosm/l between lumen and tubule. Beyond 200mosmi Ki and Cl- diffuse back via the paracellular pathway. Due to this active transport of solute, Osmolarity of interstitium increases.
- High permeability of descending limb of loop of henle to water. Due to high inertial osmolarity water diffuses from descending limb of the loop of the henle into the interstitium, thus increasing the fluid osmolarity in the tubule which equals to medullary interstitial.
- Facilitated diffusion of urea from the inner medullary collecting duct into the deep medullary interstitial. It is stimulated by ADH which inserts urea transporter UT- Al.
Imaginary steps of origin of effect:-
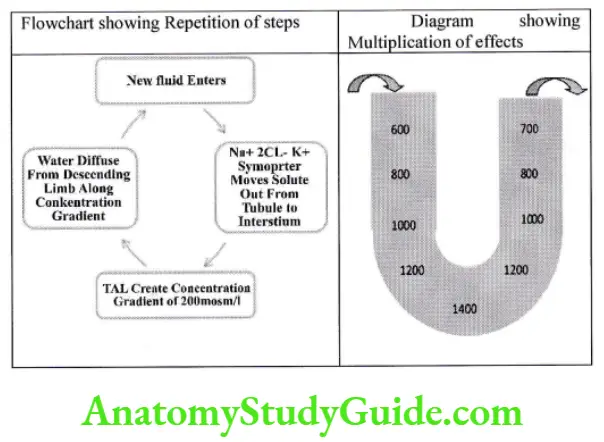
Multiplication of single effect
The steps repeat again and again. With sufficient time, the interstitial traps the solute, increasing the medullary concentration to 1200-1400mOsm/l.
Role of Urea
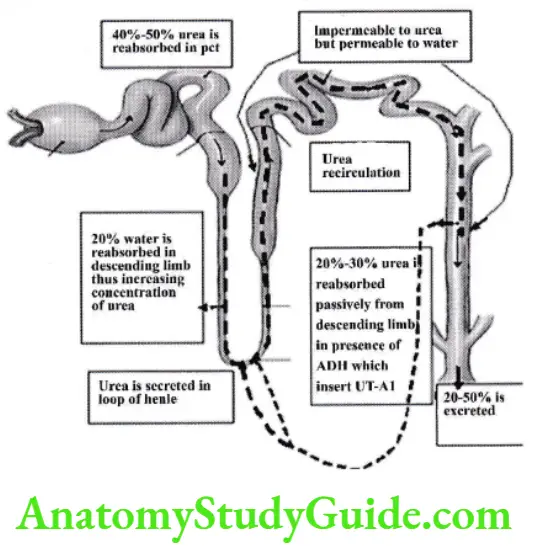
- Urea contributes to 40-50%o of renal medullary Osmolarity which is 500-600 mOsm/l.
- 40-50% urea is reabsorbed in pct.
- In descending loop offense 20% water is absorbed increasing the concentration of urea.
- The ascending limb and part of the cortical collecting duct is impermeable to urea.
- In medullary collecting duct permeability of urea depends on ADH, which inserts UT-A1 and helps in the passive absorption of urea in interstitium.
- From the interstitium some amount of urea is secreted in the descending limb of loop of henle, help to prevent the washout of urea from interstitium.
- Some amount of urea recirculating in tubule and interstitium.
Applied:-
- People who ingest high proteins diet have higher urea concentration and can concentrate better.
- Malnourished have low urea, thus have low urine concentrating capacity.
Role of ADH
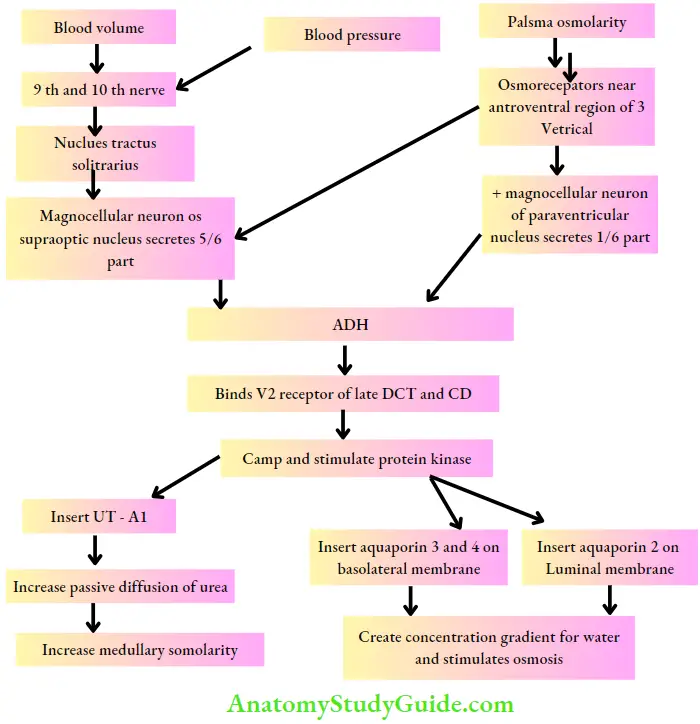
Summary
Counter current Exchanger
It maintains medullary hyperosmolarity. This function is severed by vasa recta which are peribulbar capillaries of the juxta glomerular apparatus. Blood flow through the vasa recta is slow and low (57o of renal blood flow). It may be due to the high resistance offered by.
- Long length of vasa recta
- Increased viscosity of blood
- Decreased hydrostatic pressure
vasa recta is highly permeable to water and solutes, except for plasma proteins. It act as a counter-current exchanger as it runs parallel to, but in opposite direction to loop of Henle. The “U” shape of the vasa recta prevents the washout of medullary hyperosmolarity.
When the vasa recta descends down in the deep medulla, solute diffuses in from the interstitial, and Osmolarity equilibrates with renal medullary interstitium: 140OmOsm/I.
When it ascends up in cortex all solutes are passively diffused out in the interstitium thus Osmolarity falls to 300 mosm/l.
Although a large amount of exchange occurs across the vasa recta, the Osmolarity of the interstitium remains constant.
Applied:- The ability to maintain Osmolarity is flow-dependent. If blood flow increases, vasa recta will dissipate the medullary gradient and will decrease urinary concentrating ability.
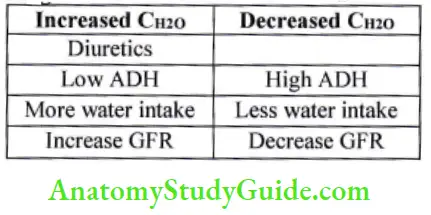
Assessment of renal concentration and diluting ability – free water clearance
For assessing urinary dilution or concentration, urinary Osmolarity, and volume must be measured. Urinary Osmolarity ranges from 5OmOsm/l to 1200mOsm/kg H2O, which corresponds to urinary volume of 18 1 to 0.51.
The critical basic process of dilution or concentration of urine is the separation of solute from water. If more solute is separated then urine becomes dilute, and if solute is not separated then urine becomes concentrated. The kidney produces a quantity of water “free of all solutes”. When it is excreted from the body urine becomes dilute, when it is not excreted from body urine becomes concentrated. Free water clearance quantifies the kidneys’ capability to generate solute-free water.
The kidney produces urine composed of solute and solute-free water. The amount of solute cleared from plasma is “Os molar clearance”. The amount of solute-free water cleared from plasma is “Free water clearance”. “Free water clearance” represents the volume of clean water that must be added to or removed from urine to make it iso-osmotic with plasma.
Urine flow = Osmolar clearance + Free water clearances
V = Cosm + C H2O
H2O = V – Cosm U = urinary concentration of substance
We know Cosm = U X V/P V = urinary flow rate
CH2O = V – {(U X V)/P} P = plasma concentration of substance
Interpretation
Curol 0, urine is iso-osmolar with plasma
Cnzo> 0 urine is dilute than Plasma
Cazo <0 urine is concentrated than plasma
Crzo dePends on
- ADH
- Water intake
Applied:
Leave a Reply