Obesity, Bariatric And Metabolic Surgery
Obesity, Bariatric And Metabolic Surgery Introduction: Obesity is a chronic, complex disease that negatively affects one’s health. It is characterized by excess fat in the body, which occurs when calorie consumption is significantly higher than calorie expenditure. Body mass index (BMI), which is measured in kg/m2, is used to classify patient’s weight.
Table of Contents
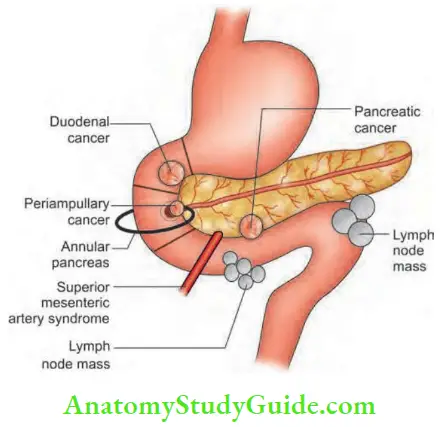
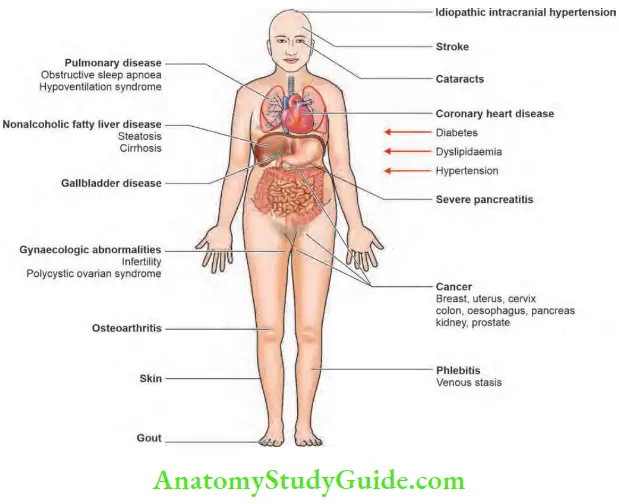
Morbid obesity (BMI >35 kg/m2) may be associated with comorbidities, such as diabetes mellitus, hypertension, coronary artery disease, osteo¬arthritis, sleep apnoea, etc., which reduce life expectancy. Bariatric surgery is often performed to reduce excess body weight and is known as metabolic surgery when primarily carried out to manage associated comorbidities.
Obesity, Bariatric And Metabolic Surgery Aetiology and Pathophysiology
The aetiology of obesity is multifactorial and occurs due to causes like a sedentary lifestyle, a familial tendency, environmental factors, psychosocial behaviour, a few medical conditions (for example, Cushing’s syndrome, hypothyroidism), and congenital diseases (example, Prader-Willi syndrome).
An elevated BMI is associated with increased leptin levels. Obesity can affect any age and is becoming increasingly prevalent among children and adolescents. India has emerged as the third most obese nation after USA and China due to its socioeconomic changes. Obesity affects almost every organ of the body and causes many diseases that result in significant morbidity and mortality.
Obesity, Bariatric And Metabolic Surgery Management of Obesity
Medically treatable causes for obesity should be evaluated by appropriate tests. If no cause is established, a trial of diet and exercise with behavioural changes should be prescribed. If this also fails, bariatric surgery should be considered after proper counselling. Patients with a BMI >35 kg/m2 with comorbidities should be considered for surgery. Laparoscopic surgery is currently the standard of care, and robotic bariatric surgery is also sometimes adopted.
Types of Bariatric Surgery
- Restrictive procedure, example, laparoscopic adjustable gastric banding (LAGB) and laparoscopic sleeve gastrectomy (LSG)—this largely restricts food intake.
- Restrictive procedures with some malabsorption: Roux-en-Y gastric bypass (RYGB), one anastomosis gastric bypass or mini gastric bypass (OAGB or MGB)—this restricts food intake and causes some malabsorption.
- Malabsorptive procedures with some restriction: Biliopancreatic diversion (BPD), duodenal switch (DS)—this causes severe malabsorption with less food restriction and is rarely performed in India.
Indications for Bariatric Surgery
- BMI >40 kg/m2 or BMI >35 kg/m2 with associated medical comorbidity.
- Failed dietary therapy with above BMI levels.
- Psychiatrically stable without substance abuse.
- Knowledgeable about the operation to be performed and its sequelae.
- Motivated individual.
- Age >18 years and <70 years.
Contraindications for Bariatric Surgery
- Medical: Cirrhosis with portal hypertension, auto-immune connective tissue disorders, inflammatory bowel disease (IBD), chronic administration of steroids, poor fitness for general anaesthesia.
- Surgical: Inability to ambulate, Prader-Willi syndrome (congenital obesity syndrome with severe hyperphagia, growth-hormone deficiency, hypogonadism, dysmorphic features, and cognitive impairment).
Details of Surgery Laparoscopic RYGB
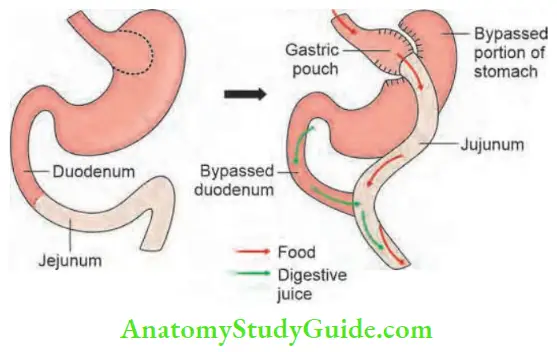
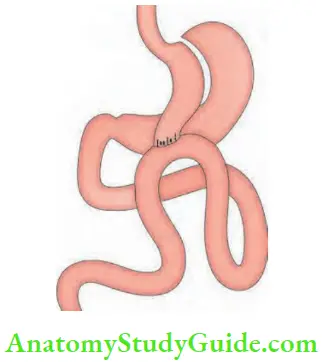
- Laparoscopic RYGB: Gastric bypass, which was first described by Mason and Ito in 1969, incorporates a loop of jejunum anastomosed to a proximal gastric pouch. However, loop gastric bypass may result in bile reflux. To overcome this dis¬advantage, RYGB was developed, and it has now become one of the most commonly performed bariatric surgeries.
- The roux limb should be at least 75 cm, and the biliopancreatic limb should be 100-150 cm.
- Enteroenterostomy (jejunum) is performed to prevent stenosis or obstruction.
- All potential spaces for internal hernias should be closed using nonabsorbable sutures.
- A small proximal gastric pouch (15-20 ml) should be constructed from the cardia of the stomach to prevent dilation and to minimize acid production.
- The gastric pouch should be divided from the distal part of the stomach.
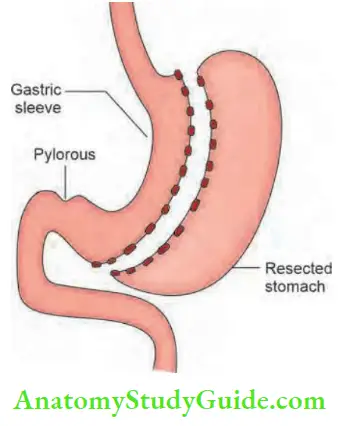
- Laparoscopic sleeve gastrectomy: It is widely practiced worldwide due to its simplicity. A narrow gastric sleeve is fashioned over a gastric calibration tube by stapling the stomach vertically, and the resected stomach is removed.
- One anastomosis gastric bypass or mini gastric bypass (OAGB or MGB): This is a type of gastric bypass in which 150-200 cm of the jejunum is bypassed by anastomosing it to a long, narrow gastric pouch.
Complications of Bariatric Surgery
- Staple line/anastomotic leaks: These may be lethal, if not recognized early. The leak rate is high in the initial period. More recent studies report anastomotic leak rates of 0.35-0.5%.
- DVT (deep vein thrombosis) and pulmonary embolism: Obese individuals are prone to DVT. However, this has become uncommon with chemoprophylaxis and early mobilization.
- Nutritional deficiency: Various nutritional defi-ciencies may occur due to severe food restriction and malabsorption, if the patient is not taking the required daily dose of additional nutritional supplements and adequate proteins.
- Bowel obstruction after Roux-en-Y bypass: It occurs due to the potential for internal hernias, which commonly occurs after laparoscopic RYGB and is estimated to be between 3 and 4.5%. Two potential locations:
- Petersen’s space: It is the space caused by the herniation of intestinal loops through the defect between the small bowel limbs, the transverse mesocolon, and the retroperitoneum after RYGB. Jejunojejunostomy mesenteric defect.
- Marginal ulcer: It occurs in 2-10% of cases who undergo gastric bypass surgery. It may lead to perforation, stricture formation, or gastric pouch outlet obstruction, which will require endoscopic dilation, if it not treated promptly.
Bariatric Surgery Recent Advances
Certain endoscopic procedures, such as gastric balloon and endoscopic sleeve gastroplasty, are being tried to limit food intake. The use of appetite suppressants or drugs that limit food absorption cannot be taken for long time without adverse effects. Research is now directed towards the role of altering gut microbiota to manage obesity.
Leave a Reply