Obstructive Jaundice (Surgical Jaundice)
Obstructive Jaundice (Surgical Jaundice) Definition: Jaundice that occurs due to obstruction to the outflow of bile is called obstructive jaundice.
Table of Contents
- Since these cases have to be managed by surgical intervention, it is also called surgical jaundice.
- However, haemolytic jaundice cases are not obstructive but a few are managed by splenectomy hence it is called as surgical jaundice.
- Before we start a detailed discussion of obstructive jaundice, we will study anatomy of the pancreas. This is an important long case in the university examina¬tion. For a better understanding of obstructive jaundice, students are requested to understand various causes of obstructive jaundice which are given in the subsequent pages.
Case Of Obstructive Jaundice
Choledocholithiasis and carcinoma head of pancreas/ periampullary region are two important causes of obstructive jaundice. They constitute more than 90% of cases of obstructive jaundice treated surgically.
- Presence of jaundice, high-coloured urine, clay-coloured stools and itching gives the clue to the diagnosis. Palpable liver, palpable mass (cholangiocarcinoma, carcinoma head of pancreas) and palpable gallbladder (periampullary carcinoma) supports the diagnosis. Early diagnosis by imaging, endoscopy, ERCP, MRCP is possible.
- Since causes are many, they are treated accordingly. Relief of pain, relief of jaundice with or without resection (in malignancies) should be done early to prevent complications such as cholangitis, liver abscesses, septicaemia, renal failure and even death.
Case Of Obstructive Jaundice Aetiology
- Causes in the Lumen
- Stones in the common bile duct
- Ova, cysts, ascaris worms
- Hydatid cyst of the biliary tree
- Stone in the pancreatic duct/CBD junction
- Causes in the Wall
- Periampullary carcinoma
- Bile duct stricture
- Stenosis of sphincter of Oddi (papillary stenosis)
- Klatskin’s tumour—carcinoma of the bile duct where right and left ducts join
- Choledochal cyst
- Post-laparoscopic cholecystectomy
- Causes from Outside (due to Pressure)
- Carcinoma head of pancreas
- Chronic pancreatitis
- Lymph nodes at the porta hepatis obstructing the biliary tree.

Case Of Obstructive Jaundice Clinical Features
First study to differentiate choledocholithiasis from carcinoma periampullary/head of pancreas.

Investigations In Obstructive Jaundice
1. Hb% is low in malignancy.
2. TC and DC are increased in case of infections. High white cell counts suggest cholangitis and it becomes an indication for preoperative stenting in cases of carcinoma head/periampullary carcinoma. If cholangitis is due to CBD stones (more common), ERP followed by extraction of the stones with a stent is the initial definite treatment.
3. BT, CT and PT are altered in case of obstructive jaundice
4. Urine for urobilinogen is negative in obstructive jaundice.
5. Serum alkaline phosphatase: Normal value 60– 300 units/L. More than 500 units is suggestive of obstructive jaundice.
- These are the enzymes which bring hydrolysis of phosphate esters in alkaline medium.
- Sources of alkaline phosphatase include liver, biliary tree, bone, intestine, kidney.
- Excretion is mainly through biliary tree
- Segmental obstruction—bilirubin is LP.
6. GGT: Gamma-glutamyl transpeptidase.
7. Abdominal ultrasound: It is the most useful, noninvasive, reliable and quick investigation for obstructive jaundice. Dilated biliary radicles, both intrahepatic and extrahepatic, can be demonstrated (first clue in obstructive jaundice).
- Gallstones can be diagnosed with their posterior acoustic shadow.
- Mass lesion in the head region can be seen in cases of chronic pancreatitis or carcinoma head of the pancreas causing obstructive jaundice.
- Ultrasound can detect multiple secondaries in the liver, thus, favouring the diagnosis of malignancy. However, it is not an ideal investigation for CBD stones.
8. CECT (contrast-enhanced CT) scan: A head mass of even 2–3 cm in size and portal vein infiltration can be demonstrated by CT scan. Obliteration of fat plane between the mass and superior mesenteric vessels can be demonstrated by CT scan which decides the operability of periampullary carcinoma or carcinoma head of the pancreas relative contraindication.
- CT scan cannot differentiate head mass of carcinoma from chronic pancreatitis. (PET scan may differentiate.)
- CT scan can also detect coeliac nodes, presence of which is a contraindication for radical resections.
- Take precautions against contrast-induced nephropathy.




9. Endoscopy is useful to diagnose a periampullary carcinoma which may be seen as an ulcerative lesion in the second part of the duodenum. Biopsy can also be taken which shows adenocarcinoma. Please note if a lesion is detected such as growth, no stenting/or intervention (ERCP) is done. However, when bilirubin levels are very high and to improve general condition of the patient, as in cholangitis, temporary stenting can be done. In case of obstructive jaundice due to stones, smooth bulge can be seen in the second part of the duodenum. In carcinoma, ulcerated lesion can be seen.

10. MRI: When CBD stones are suspected MRI is done. It is easy and no contrast is used. If stones are detected one can proceed with ERCP and basketting of stones.


11. ERCP (endoscopic retrograde cholangiopancreatography).: With the help of a side-viewing endoscope, ampulla of Vater is cannulated and a radioopaque dye is injected. It fills up the biliary and pancreatic system.
- ERCP Interpretation
- Stones appear as filling defects in the CBD or in the common hepatic duct (CHD), which may be mobile (change position, if patient is moved).
- A periampullary carcinoma gives rise to an irregular filling defect or there may be total cut off in the flow of dye. (Done for cholangitis due
to carcinoma cases.) - Chronic pancreatitis may show the dilated duct and stones in the pancreatic duct—‘chain of lakes’ appearance.
- ERCP Uses: If stones in the CBD are diagnosed, they can be treated in the following ways:
- Extraction by using a basket.
- Large stone can be crushed by using a lithotripter
and can be extracted. - Sphincterotomy (incision of sphincter of Oddi) can be done to facilitate extrusion of small stones.
- In patients with cholangitis with obstructive jaundice, stenting of common bile duct can be done to relieve obstruction. Stent removal is necessary at a later date.
- In selected patients with biliary strictures, stent is placed after ERCP to relieve obstructive jaun¬dice (sometimes permanent in malignancies).
- In selected patients with chronic pancreatitis, pancreatic duct can be stented to relieve pain.



12. Endosonogram: Endoscopy-aided ultrasound can detect missed stones in the CBD. It can also detect pancreatic head mass, lymph nodes. Endosono-guided FNAC can also be done.

13. Percutaneous transhepatic cholangiography (PTC): Using an ultrasound image-intensifier, a dilated biliary radicle is identified within the liver and a fine needle (Chiba needle1) is introduced into it. The stylet is then removed and a radio¬opaque dye injected. Chiba needle is 15 cm long and 0.7 mm in diameter.
- Percutaneous transhepatic cholangiography Precautions
- BT, CT, PT should be normal. Otherwise, vitamin K injection 10 mg is given 4 or SC for 3 days.
- If there is a bleeding tendency, this procedure should not be done.
- Broad-spectrum antibiotics are given before the procedure.
- Percutaneous transhepatic cholangiography Complications
- Infection, cholangitis, septicaemia
- Biliary leak can be significant producing abdo-minal pain and guarding. Hence, PTC should be done just prior to the surgery.
- Haemorrhage


14. Diagnostic laparoscopy
- It is used in many GI malignancies.
- It can be aided by laparoscopic ultrasound.
- It can complement the staging by CT, MRI, etc. It can improve prediction of resectability to about 98% accuracy.
- It is a simple but invasive investigation, requires 3 ports.
- Specially excellent to detect peritoneal meta-stasis (which cannot be picked by other tests) which is the sign of inoperability.
15. CA 19-9: Often head mass can be due to carcinoma/chronic pancreatitis. Biopsy is not mandatory. Clinical suspicion of a head mass may be treated with Whipple’s pancreaticoduodenectomy. However, gross elevation of CA 19-9 (carbohydrate antigen) will suggest carcinoma.
Summary of the Investigations in Cases of Obstructive Jaundice
- CBP, LFT is done first to know the type of jaundice and to know the general condition of the patient.
- If ultrasound detects IHBR and CBD stones, no other investigations are necessary. ERCP and basketting of the stones is done.
- If ultrasound shows doubtful stones, CECT is done.
- If periampullary carcinoma is suspected, side viewing endoscopy and biopsy is done followed by CECT to detect signs of operability.
- In high (at the porta hepatis or at confluence of left and right hepatic ducts) obstructions—MRI and CECT are done.

Treatment Of Obstructive Jaundice
Preoperative Preparation; In all malignancies, Kernofsky criteria or ECOG criteria of performance status is calculated and discussion is done with patient and relatives regarding the plan of treatment—surgery, complications, chemotherapy, etc. Discussion of the disease and the performance status should be discussed in tumour board once staging is done and appropriate treatment is done.
- Correction of fluid and electrolyte status and adequate hydration before surgery for 2-3 days is essential, especially when patients have vomiting or have developed sepsis. Adequate hydration is done to improve the urinary output.
- Injection vitamin K, 10 mg, subcutaneously or intra-venously for 3 days is given to correct the prothrombin time. If prothrombin time is not corrected with this treatment, fresh frozen plasma should be given.
- Broad-spectrum antibiotics are given before, during and after surgery.
- Adequate blood transfusion to correct anaemia.
Treatment of CBD Stones: Once the diagnosis of CBD stones are confirmed by imaging, a few options are available depending upon expertise, facilities. They are given below.
1. Preoperative ERCP, sphincterotomy + extraction of stones followed by laparoscopic cholecystectomy: This method has become the choice today. Expertise and sophisticated equipment are necessary for this.

2. Cholecystectomy is done first. This is followed by introduction of a cannula into the cystic duct and a radio-opaque dye is injected. This is called OTC (On Table Cholangiography). If the dye goes freely into the duodenum without filling defect, it is a normal OTC. If there are filling defects in the CBD, it is explored.
- Precautions while doing OTC
- There should not be any air bubble in the syringe.
- 5-10 ml of dye has to be injected.
- Leakage of the dye should not occur.
- OTC and CBD exploration can be done by laparoscopy only.
3. Supraduodenal choledocholithotomy: Some patients come after Lap. cholecystotomy and failed ERCP and basketting. They are managed by open method. Supraduodenal CBD is explored through an incision over the anterior wall and the stones are removed.
- Operating choledochoscope is passed into the common hepatic duct and its branches and the stones, if present, are removed. Closure of the CBD is done after inserting ‘T-tube’.
- After 8-10 days, a T-tube cholangiography is done and if the dye goes freely into duodenum and no filling defect is seen in the CBD, the T-tube is removed by gentle traction. By 10-12 days, the track is well formed. Hence, even if minor leak occurs, bile flows outside without causing peritonitis.


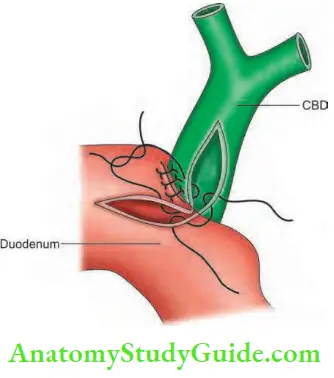
4. Cholecystectomy + choledocholithotomy + choledo-choduodenostomy: It can be done when CBD is dilated more than 1.5 cm in diameter and stoma should be at least 2-3 cm in size. Indications are:
- Recurrent stones in the CBD
- Multiple intrahepatic stones (Caroli’s disease)
- Stricture of the lower CBD Advantages of choledochoduodenostomy
- Biliary leak is negligible
- There is no worry, even if there are retained stones in the CBD.
- It is a permanent solution for stenosis, stricture or multiple intrahepatic stones.
Leave a Reply