Pathogenesis Of Autoimmunity
Autoimmunity occurs when mechanisms of immune tolerance of the body are broken. In general, abnormal immune response in autoimmunity is explained by a combination of three factors that may be interacting:
Table of Contents
Read And Learn More Amyloidosis
- Endogenous abnormalities in the immune system
- In a genetically susceptible host
- With trigger from exogenous agents
These factors are considered below:
1. Endogenous Abnormalities In The Immune System:
Following abnormalities in the cells of the immune system cause the failure of immune tolerance:
- Altered antigen presentation: Alteration in the availability and presentation of self-antigens is an important part of autoimmunity:
- Presentation of newer or cryptic epitopes by altered processing of self-antigen (epitope is an antigenic determinant component of an antigen which is recognized by body’s immune system while cryptic epitope is a new peptide determinant on antigen).
- Presentation of self-antigen (along with cryptic epitope) by B cells instead of its presentation by dendritic cells activates autoreactive T cells.
- Enhanced function of antigenic presenting cells by either costimulatory molecular expression or by cytokine production.
- Increased T and B cell stimulation: Enhanced help from T cells and increased B cell function from the following mechanisms produces autoantibodies and autoimmunity:
- Excessive stimulation of T cells produces nonspecific signals which bypass the need for antigen-specific helper T cells. This results in polyclonal activation of B cells with the formation of multiple autoantibodies.
- Increased production of B cell activating factor may cause T cell-independent B cell activation and formation of excess of autoantibodies.
- The absence of autoimmune regulatory (AIRE) gene expression in the thymus fails to delete central autoreactive cells from the body and initiate autoantibody production and inflammatory destruction.
- Altered production of cytokines due to deranged activity of B and T cells may contribute to autoimmunity, for example, Reduced production of TNF and IL-10.
- Defective clearance of apoptotic material: If apoptotic material is not cleared efficiently by body’s immune system, the apoptotic debris becomes immunogenic. This activates dendritic cells and stimulates B cells forming autoantibodies against apoptotic material.
- Release of sequestered self-antigens: Self-antigens that are completely sequestered may act as foreign-antigen if introduced into circulation later. This may occur when there is damage or inflammation at these sites, and that causes significant immunologic attack by activated T cells.
For example, In multiple sclerosis, immune attack against autoantigens (myelin, non-myelin) expressed in the brain.
- In sympathetic ophthalmia, immune damage against autoantigens is expressed in the eye.
- In trauma to the testis, there is the formation of anti-sperm antibodies against spermatozoa.
2. Genetic Susceptibility:
Evidence has been accumulating that genetic susceptibility genes have an important role in autoimmunity:
- HLA gene association:
- It has been seen that particular MHC alleles (mainly class II HLA alleles) have a fairly consistent association for susceptibility to a particular autoimmune disease.
- This may be owing to differences in the ability of varying alleles of MHC molecules to present autoantigenic peptides to autoreactive T cells. Alternatively, cross-reactivity between MHC gene products and microbial protein products may incite autoimmunity by molecular mimicry.
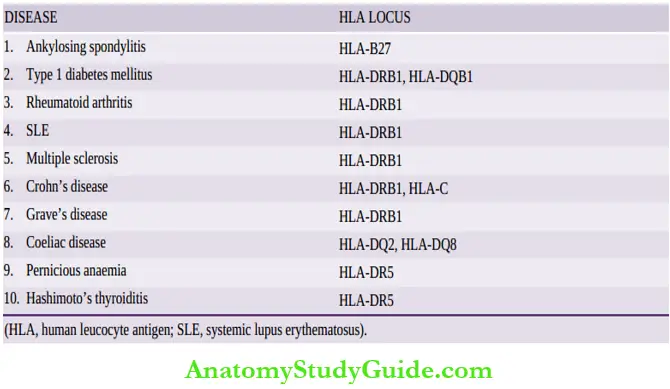
- A few common examples of HLA loci predisposing to autoimmune diseases is given in the table.
- Other evidences: Besides HLA association, a few other factors supporting genetic predisposition to autoimmune diseases are as under:
- Identical twins have a far higher occurrence of the same autoimmune disease than non-identical twins, favoring genetic basis.
- Inherited deficiency of early proteins in the complement pathway (C1q, C2, C4) is associated with the development of SLE.
3. Exogenous Agents:
Certain environmental agents, in particular microbial infections, act as a trigger for autoimmunity.
HLA loci predisposing to autoimmune diseases:
Microbial Infections
Infection with viruses ( for example, EBV infection), bacteria ( for example, Streptococci, Klebsiella), and mycoplasma, has been implicated in triggering autoimmunity.
The mechanism for this can be explained in one of two ways:
- Molecular mimicry by which the protein products of microbe express the same antigen as self-antigen (i.e. pathogen-associated molecular pattern PAMP) and thus activate autoreactive lymphocytes.
- For example, in rheumatic heart disease, there is a formation of autoantibodies against the M protein of Streptococcal antigens which cross-react with self-proteins of the myocardium, joints, and brain and produce lesions there.
- Upregulation of costimulatory signals on antigen-presenting cells results in clonal energy which activates T cells specific for auto-antigens.
Other factors:
Besides infections, the role of other environmental agents such as cigarette smoking, tissue damage, and inflammation in triggering autoimmunity has been found.
Immune Tolerance And Pathogenesis Of Autoimmunity
Immune tolerance is defined as the ability of an individual to recognize autoantigens and show selective unresponsiveness to autoantigens.
Normally, immune tolerance is maintained by three general processes: sequestration of self-antigens, generation, and maintenance of self-tolerance, and altered immunomodulatory controls.
A state of self-tolerance is generated and maintained by either central deletion of autoreactive lymphocytes, or peripheral silencing of autoreactive lymphocytes (or clonal energy).
Autoimmunity occurs when mechanisms of immune tolerance of the body are broken.
Abnormal immune response in autoimmunity is explained by a combination of three factors that may be interacting:
- Endogenous abnormalities in the immune system
- In a genetically susceptible host
- With trigger from exogenous agents.
1. Endogenous abnormalities in the immune system: May be altered antigen presentation, increased B and T cell stimulation, defect in clearance of apoptotic debris, and release of sequestered auto-antigens.
2. Genetic susceptibility: To autoimmune diseases is generally due to specific HLA class II alleles, most often B27 and DRB1.
3. Exogenous agents: W hich may trigger the onset of autoimmunity most often are viral or bacterial infections which may be due to molecular mimicry or up regulation of costimulatory signals.
Leave a Reply