Pelvic Viscera
Question 1. Define the pelvis and enumerate its contents.
Answer:
The pelvis is a large, basin–shaped region of the body at the junction of the trunk and lower limbs.
It contains the following organs:
- Urinary bladder
- Prostate (in male only)
Read And Learn More: Anatomy Question And Answers
- Uterus (in female only)
- Rectum
These organs are called pelvic viscera, and the pelvis protects them.
Urinary bladder and urethra:
Question 8. Write a short note on the Female Urethra.
Answer:
The female urethra is 4 cm long and 6 mm in diameter. It begins at the internal urethral meatus of the bladder, opposite the middle of the pubic symphysis. It passes anteroinferiorly behind the pubic symphysis, embedded in the anterior wall of the vagina to open into the vestibule of the vagina above the vaginal orifice.
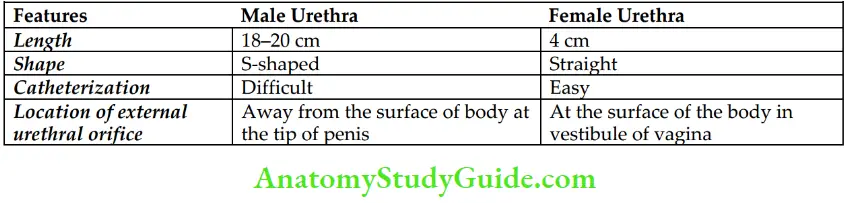
Question 9. Give differences between the male and female urethra.
Answer:
Question10. Discuss the Histological Features of the Male Urethra
Answer:
Male urethra Histological features: In a histological section the wall of the urethra presents 3 coats.
From the outside inward, these are:
- Muscular coat
- Submucous coat
- and Mucosa.
These are:
- Muscular coat: It consists of an inner longitudinal and outer circular layer of smooth muscle fibers.
- Submucous coat: It consists of erectile vascular tissue.
- Mucosa: It presents regional variations:
- Above the colliculus seminalis, it is lined by transitional epithelium.
- Between colliculus seminalis and navicular fossa, it is lined by stratified columnar epithelium.
- Distal to the navicular fossa, it is lined by stratified squamous nonkeratinized epithelium.
Prostate
Question 12. Enumerate the structures present within the parotid gland.
Answer:
Parotid gland These are:
- Prostatic urethra
- Prostatic utricle
- Ejaculatory ducts
Question 13. Give the Histological features of the Prostate Gland.
Answer:
Prostate gland:
The prostate is a compound tubuloalveolar/tubuloacinar gland. A histological section through it presents two components: stroma and parenchyma.
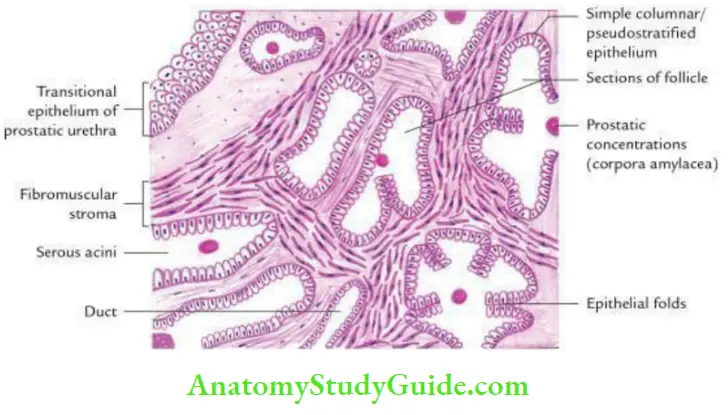
Prostate gland Stroma:
- It is fibromuscular and made up of collagen fibers and smooth muscle fibers. It forms:
- Discrete bundles of muscle fibers surround serous alveoli and run in many directions.
- The thin capsule of collagen and smooth muscle fibers.
Prostate gland Parenchyma:
It consists of serous acini and ducts.
- Serous acini:
- Are large, irregular, and of different shapes.
- Have wide lumen, in old age some of them may contain small colloidal mass (amorphous eosinophilic mass) called prostatic concretions/corpora amylacea (amyloid bodies).
- Are lined by secretory tall columnar cells. The lining epithelium shows aggressive infolding.
- Ducts:
- They may be seen between the acini.
- They are lined by bilaminar epithelium, an inner layer of columnar cells, and outer layer of cuboidal cells.
Question 14. Briefly describe Age-Related changes in the Prostate.
Answer:
These are as under:
- At birth: The prostate is very small and consists mainly of stroma with rudiments of the duct system.
- At 9–14 years: The duct system becomes more elaborate.
- At puberty: Rapid growth of follicles with condensation and reduction of stroma under the influence of testosterone.
- From 20–30 years: Marked proliferation of glandular tissue and infolding of follicular walls.
- From 30–45 years: Involution starts and there is an increase in the number of prostatic concretions (amyloid bodies).
- From 40–50 years: Either enlargement (BHP) or senile atrophy of the gland.
Question 15. Write a short note on the mesonephric duct.
Answer:
Mesonephric Duct:
The mesonephric duct (or Wolffian duct) is a male genital duct that develops from mesonephros and opens into the cloaca.
Mesonephric Duct Derivatives:
- Duct of epididymis
- Vas deferens
- Seminal vesicle
- Ejaculatory duct
Question 17. Write a short note on the broad ligament of the uterus.
Answer:
Ligament of the uterus:
It is a fold of peritoneum passing from the side of the uterus to the lateral wall of the pelvis.
Ligament of the Uterus Contents: These are
- Uterine tube
- Round ligament of uterus
- Uterine vessels
- Ovarian vessels
- Ligament of ovary
- Some lymph vessels
- Uterovaginal and ovarian nerve plexuses
- Vestigial remnants of the mesonephric duct and its tubules, viz.
- Epoophoron, a remnant of proximal mesonephric tubules.
- Duct of Gartner, a remnant of the cephalic part of the mesonephric duct.
- Paroophoron, a remnant of distal mesonephric tubules.
- Extraperitoneal tissue

Note: The ureter as a rule is not a content of broad ligament.
Ligament of the uterus Applied anatomy:
The ureteric stone can be palpated on vaginal examination at the site, where the ureter is in close relationship to the lateral fornix of the vagina.
Question 18. Give a brief account of the development of the uterus and associated common congenital anomalies.
Answer:
Uterus Development:
The uterus develops from the following sources:
- Most of uterus develops from the cephalic part of the uterovaginal canal formed by the fusion of the caudal parts of the paramesonephric ducts.
- Funds of the uterus is formed by the incorporation of segments of horizontal parts of the paramesonephric ducts.
- The myometrium is derived from the surrounding mesoderm.

Congenital anomalies:
These are as follows :

- Double uterus (uterus didelphys) and double vagina: It occurs due to a lack of fusion of the paramesonephric duct and sinovaginal bulbs.
- Double uterus with single vagina: It occurs when paramesonephric ducts fail to fuse.
- Bicornuate uterus: In this case, the vagina and cervix are single, but the body of the uterus is duplicated.
- Unicornuate: In this case, half of the uterus is missing due to degeneration of one of the paramesonephric ducts.
- Infantile uterus: In this condition, the uterus remains rudimentary.
- Agenesis of the uterus (complete absence of the uterus): It occurs when paramesonephric ducts fail to develop.
Question 19. Describe the histological features of the uterus.
Answer:
Histological features of the uterus:
In a histological section, the wall of the uterus presents 3 layers:
From inside outward, these are:
- Endometrium
- Myometrium (thickest coat), and
- Perimetrium.

1. Endometrium/mucosa:
Epithelium: Uterine mucosa is lined by simple columnar epithelium.
- Lamina propria: It is thick and contains simple tubular glands lined by a layer of columnar cells with abundant interglandular stroma.
Note: Functionally endometrium is made up of two layers
- Thick superficial functional layer.
- Thin deep basal layer.
The functional layer of endometrium undergoes changes in different phases of menstrual cycle:
- Proliferative phase:
- Glands are straight tubular and have a narrow lumen
- Stroma is highly cellular and non-oedematous with coiled arteries in deeper parts
- Secretory phase:
- Glands become highly tortuous and dilated exhibiting a saw-tooth appearance/step ladder appearance
- Stroma becomes oedematous
- The Lumen of glands becomes filled with secretions
- Menstrual phase:
- Loss of epithelium
- Necrosis of walls of vessels
- Necrotic stroma, spiral arteries, and glands are sloughed off
- Presence of blood cells
- Presence of blood in the uterine lumen
Note: Menstrual flow: It consists of blood, uterine fluid, and necrotic endometrial tissue of the functional layer of the endometrium.
2. Myometrium/muscular layer (thickest layer):
- Consists of an interlacing bundle of long smooth muscle fibers, which are arranged in 3 ill-defined layers separated by connective tissue.
- The inner and outer layers are longitudinal, and the middle layer is circular.
- The presence of large blood vessels in the middle layer gives it a spongy appearance.
3. Perimetrium/serosa: Consists of a single layer of a mesothelial lining and a connective tissue layer.
Question 20. Describe the histological features of the cervix of the uterus.
Answer:
Histological features of the cervix of the uterus:
- The section through the cervix presents the following histological features:
- It is lined by tall columnar mucous-secreting epithelium.
- The lamina propria contains branched tubular mucous-secreting glands (cervical glands).
- The vaginal portion of the cervix is lined by stratified squamous epithelium.
Question 21. Write a short note on the uterine/fallopian tube.
Answer:
Uterine/FallopianTube:
The uterine tubes are a pair of ducts that convey the ova from the ovary to the uterus. Each tube is about 10 cm (4 inches) long and lies in the upper border of the broad ligament. It is the site of fertilization of the ovum.
Uterine/FallopianTube Parts:
From lateral to medial, each tube is divided into 4 parts :
- Infundibulum, 1 cm long
- Ampulla, 5 cm long
- Isthmus, 2.5 to 3 cm long
- Interstitial/intramural part, 1 cm long

- Infundibulum:
- It is a funnel-shaped lateral end of the uterine tube, which projects beyond the broad ligament. It bears finger-like processes called fimbriae.
- One of the fimbriae which is longer than the others and remains in contact with the tubal pole of the ovary is called as ovarian fimbria.
- At the lateral end, the uterine tube opens into the peritoneal cavity through its abdominal ostium. It is about 3 mm in diameter.
- Ampulla:
- It is thin-walled, dilated, and tortuous, forming approximately lateral 2/3rd of the tube.
- It is about 4 mm in diameter. It is the commonest site of fertilization.
- Isthmus: It is thick, narrow, rounded, and cord-like. It is the narrowest part of the tube.
- Interstitial part (intramural part): It lies within the wall of the uterus.
Uterine/FallopianTube Arterial supply:
- Medial 2/3rd by uterine artery
- Lateral 1/3rd by ovarian artery
Uterine/FallopianTube Applied anatomy:
- Salpingitis: It is inflammation of the uterine tube. Chronic salpingitis can lead to tubal blockage.
- Sterility: The most common cause of secondary sterility is tubal blockage, which is usually caused by infection, but may be congenital.
- The patency of the tube can be tested by:
- Insufflation test (Rubin’s test): If the tube is patent when the air is pushed into the uterus, it passes through the uterine tube and leaks into the peritoneal cavity.
- Hysterosalpingography: It is a radiological technique, in which the cavities of the uterus and fallopian tubes are visualized by injecting a radiopaque substance into the uterine cavity.
Question 22. Describe the histological features of the fallopian tube.
Answer:
The wall of the fallopian tube consists of 3 coats.
From the inside outward, these are the:
- Mucosa
- Muscular coat and
- Serous coat.

- Mucosa:
- Is lined by both ciliated and nonciliated columnar cells.
- Lamina propria consists of loose connective tissue (highly vascular). It is thrown into numerous longitudinal folds, which branch but do not anastomose.
- However, they form a labyrinth. Because of these folds, the lumen is highly irregular.
- Muscular coat: It is made up of inner circular and outer longitudinal layers of smooth muscle fibers.
- Serous coat: It is the outermost layer lined by mesothelial cells.
Question 23. Write a short note on the vagina.
Answer:
Vagina:
- It is a fibromuscular canal extending from the cervix of the uterus to the vestibule of the vagina.
- It is situated behind the urinary bladder and urethra and in front of the rectum and anal canal.
- Its diameter gradually increases from below upward.
- Its lumen is circular at the upper end, has a transverse slit in the middle, and is Hshaped in the lower part.
- Its anterior wall is 7.5 cm long, while its posterior wall is 9 cm long.
Its lower end is closed by a thin annular fold of mucous membrane, the hymen, in married women it ruptures and is represented by rounded tags around the vagina orifice called carunculae hymenales. Its upper end forms a circular recess around the cervix called the fornix.
Vagina Functions:
- Acts as an organ of copulation in female
- Forms the longest part of the birth canal during childbirth
Vagina Arterial supply:
- Vaginal artery, a branch of the internal iliac artery
- Branches of uterine and internal pudendal arteries
Question 24. Give the histological features of the vagina.
Answer:
The wall of the vagina from inside outward consists of 3 coats:
- Mucosa
- Muscular coat and
- Adventitia.
These are:
1. Mucosa:
- It is lined by stratified squamous nonkeratinized epithelium consisting of 16–18 layers of cells
- Lamina propria It is made up of dense connective tissue with many elastic fibers (highly vascular).
Note: Lamina propria does not contain glands; the vaginal epithelium is kept moist by glands of the cervix.
2. Muscular coat: It consists of ill-defined inner circular and outer longitudinal layers of smooth muscle fibers intermingled with elastic fibers.
3. Adventitia: It is made up of fibrous tissue containing numerous thick elastic fibers.
Question 25. Write a short note on paramesonephric ducts.
Answer:
- The paramesonephric ducts (or Mullerian ducts) are female genital ducts that develop by vertical evagination of coelomic epithelium.
- They run downwards and unite with each other to form a uterovaginal canal which terminates at the sinus tubercle in the primitive urogenital sinus.
Derivatives of paramesonephric ducts:
- Fallopian tubes
- Uterus
- Uterine cervix
- The upper part of the vagina
Ovary
Question 28. Write a short note on the ovarian fossa.
Answer:
The ovarian fossa is a peritoneal depression in the lateral pelvic wall where the ovary lies.
Ovarian Fossa Boundaries:
- Anterior: Obliterated umbilical artery.
- Posterior: Ureter, internal iliac artery.
- Superior: External iliac vein.
- Floor: Peritoneal depression beneath which passes obturator nerve and vessels.

Ovarian Fossa Applied Anatomy:
- In case of ovarian cyst rupture, the fluid may be collected in this fossa.
- Oophoritis (inflammation of the ovary) may cause localized peritonitis of the ovarian fossa and eventually irritate the obturator nerve. This manifests as pain on the medial aspect of the thigh.
Rectum
Question 29. Describe the rectum under the following headings:
- Introduction
- Curvatures
- Relations
- Arterial supply
- Venous drainage
- Lymphatic drainage and
- Applied anatomy.
Answer:
1. Rectum Introduction:
- It is a distal part of the large intestine between the sigmoid colon and anal canal.
- It joins the anal canal at an angle of 90° angle forming an anorectal flexure.
- It is 12 cm long and lies in the lesser pelvis in front of the last 3 pieces of sacrum and coccyx.
- Its lower dilated part is called the ampulla, which initiates an urge to defecate when feces enter into it.
2. Rectum Curvatures:
The rectum lies in the median plane at the beginning as well as at the end, but it shows two types of curvature in its course.
- Two anteroposterior curvatures:
- Sacral flexure: It follows the concavity of the sacrum and coccyx.
- Perineal flexure: It is the backward bend at the anorectal junction.
- Three lateral curvatures:
- Upper lateral curvature is convex to the right.
- Middle lateral curvature is convex to the left.
- Lower lateral curvature is convex to the right.

3. Rectum Relations:
Peritoneal relations:
- The upper 1/3rd of the rectum is covered by the peritoneum anteriorly and at the sides.
- The middle 1/3rd of the rectum is covered by the peritoneum only anteriorly.
- The lower 1/3rd of the rectum is not covered by the peritoneum.

Visceral relations:
- In male:
- Upper 2/3rd
- Recto-vesical pouch
- Coils of ileum and sigmoid colon
- Lower 1/3rd
- The base of the urinary bladder
- Terminal parts of ureters
- Seminal vesicles
- Ampullae of ductus deferens
- Prostate
- In female:
- Upper 2/3rd: Rectouterine pouch containing coils of ileum.
- Lower 1/3rd: Lower part of the vagina.
Posterior relations:
They are the same in males and females as follows:
- Lower 3 pieces of the sacrum, coccyx, and anococcygeal body.
- Piriformis, coccygeus, and levator ani muscles.
- Median sacral, superior rectal, and lateral sacral arteries.
- Sympathetic trunks with the ganglion impar, anterior primary rami of sacral and coccygeal nerves, and pelvic splanchnic nerves.
4. Rectum Arterial supply:
- The rectum is supplied by 4 arteries: One superior rectal, two middle rectal, and one median sacral.
- The superior rectal artery provides the main supply. It is the continuation of the inferior mesenteric artery.
- Middle rectal arteries are the branches of the anterior divisions of the internal iliac arteries.
- The median sacral artery is a direct continuation of the aorta.
Note: The two inferior rectal arteries, the branches of the internal pudendal arteries (from the anterior division of internal iliac arteries), are said to supply the rectum, but strictly speaking, they supply the anal canal.
5. Rectum Venous drainage:
- Superior rectal veins continue upward as inferior mesenteric veins and drain into the portal system.
- Middle rectal veins drain into internal iliac veins.
- Inferior rectal veins drain into internal pudendal veins.
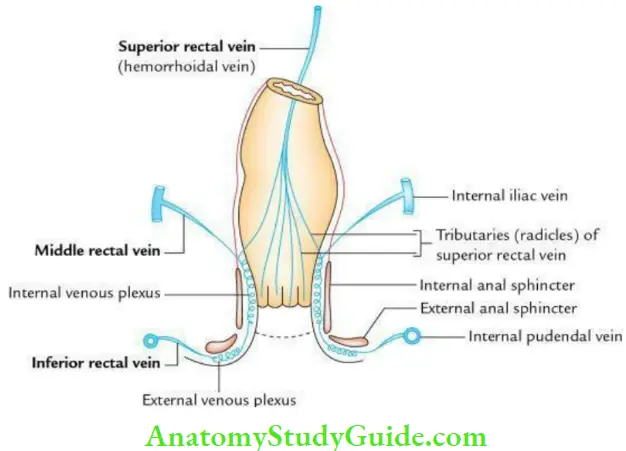
Note:
There are free anastomoses between the tributaries of these veins in the rectal wall.
6. Rectum Lymphatic drainage:
- Lymphatics from the upper halfaccompany the superior rectal vessels and drain into the inferior mesenteric nodes. A few of these vessels are intercepted by the pararectal lymph nodes situated on each side of the rectosigmoid junction.
- Lymphatics from the lower halfaccompany of the middle rectal vessels drain into the internal iliac nodes.

7. Rectum Applied anatomy:
Per-rectal examination: It is commonly done in clinical practice to palpate the following structures
- In male:
- The posterior surface of prostate
- Seminal vesicles
- Vasa deferentia
- In female:
- Perineal body
- Cervix
Prolapse of the rectum (procidentia):
- It is the protrusion of the rectum through the anus. It can be incomplete or complete.
- In incomplete prolapse, there is a protrusion of only mucosa while in complete prolapse, the whole thickness of the rectal wall protrudes through the anus.
Question 30. Give the anatomical basis of internal hemorrhoids.
Answer:
- The hemorrhoids are folds of submucosa containing varicose superior rectal vessels.
- They produce soft swellings called hemorrhoids and they are not seen until they prolapse through the anus.
- They are caused by increased pressure in the lower rectum following chronic constipation, pregnancy straining when passing stool, etc.
- The blood vessels (radicals of the superior rectal vein and branches of the superior rectal artery) stretch under pressure and may bulge to form hemorrhoids.
- Clinically they present as
- Painless bleeding during bowel movement.
- Itchy or painful lump in and around the anus.
Question 31. Describe the interior of the rectum and Houston’s valves
Answer:
The interior of the rectum presents two types of mucous folds:
- Longitudinal folds: They are present in the lower part. They are temporary and disappear when the rectum distends
- Transverse folds: They are semilunar transverse folds and permanent. They do not disappear when the rectum distends.
They consist of mucous folds containing submucous tissue and smooth muscle of the rectal wall. They are called as Valves of Houston

Question 32. Write a short note on the valves of Houston.
Answer:
Valves of Houston:
They are semilunar transverse folds of the rectal wall which protrude into the rectum.
They are 4 in number as follows:
- 1st, and IIIrd project from the right rectal wall while IInd and IVth project from the left rectal wall.
- 3rd valve of Houston is the largest and projects from the right rectal wall at the upper end of the ampulla hence cannula for rectal wash should be passed with the patient in the left lateral position to avoid obstruction
Leave a Reply