Periapical Granuloma
Periapical granuloma is one of the most common sequelae of pulpitis. It is usually described as a mass of chronically inflamed granulation tissue found at the apex of a nonvital tooth.
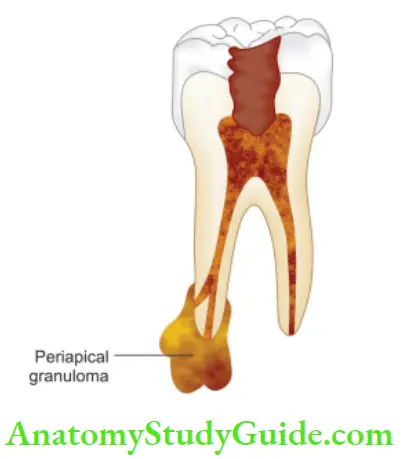
Table of Contents
Etiology of Periapical Granuloma:
Periapical granuloma is a cell-mediated response to pulpal bacterial products. Bacterial toxins cause mild irritation of periapical tissues. This leads to cellular proliferation and thus granuloma formation
Read And Learn More: Endodontics Notes
Periapical Granuloma Clinical Features:
- Most of the cases are asymptomatic but sometimes pain and sensitivity is seen when acute exacerbation occurs.
- The tooth is not sensitive to percussion
- No mobility
- Soft tissue overlying the area may/may not be tender
- No response to thermal or electric pulp test
- Mostly, lesions are discovered on routine radiographic examination
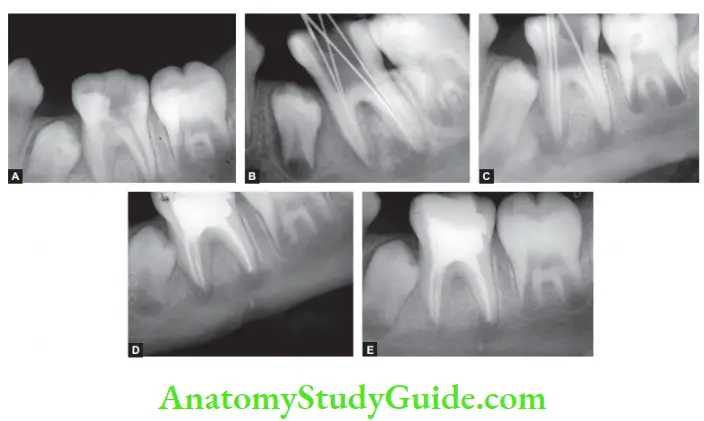
Periapical Granuloma Radiographic Features:
- Mostly discovered on routine radiographic examination.
- The earliest noticeable change seen is a thickening of the periodontal ligament at the root apex.
- The lesion may be well-circumscribed or poorly defied.
- Size may vary from small lesion to large radiolucency exceeding >2 cm in diameter.
- The presence of root resorption is also seen
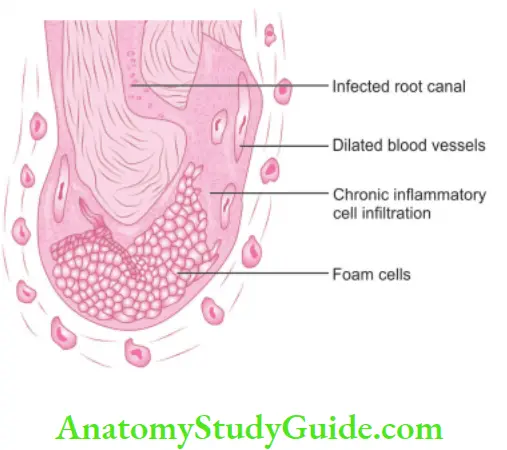
Periapical Granuloma Histopathologic Features.
- It consists of inflamed granulation tissue that is surrounded by a firous connective tissue wall.
- The granulation consists of dense lymphocytic infiltrate which further contains neutrophils, plasma cells, histiocytes, and eosinophils.
- Sometimes, Russell bodies may also be present
Periapical Granuloma Treatment and Prognosis.
- In restorable teeth, endodontic treatment is, and in case of the nonrestorable tooth, extraction followed by curettage of apical soft tissue is recommended.
Radicular Cyst Or Cystic Apical Periodontitis
The radicular cyst is an inflammatory cyst which results because of the extension of infection from the pulp into the surrounding periapical tissues.
Etiology:
- Caries, physical, chemical, or mechanical injury resulting in pulp necrosis.
- Irritating effects of restorative materials.
- Trauma.
- Pulpal death due to developmental defects.
Radicular Cyst Pathogenesis:
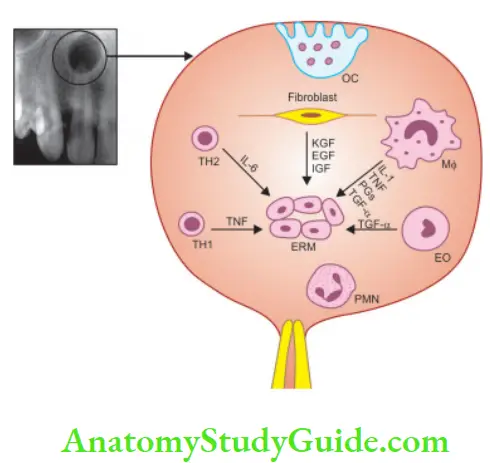
Periapical granulomas are initiated and maintained by the degradation products of necrotic pulp tissue. Stimulation of epithelial rests of Malassez occurs in response to inflammatory products.
According to Nair, cyst formation occurs as a result of epithelial proliferation, which helps to separate the inflammatory stimulus from the surrounding bone. By this mechanism, a cyst is formed and it is explained by the following two hypotheses:
Radicular Cyst Nutritional Defiient Theory:
It says that periapical inflammatory changes cause the epithelium to proliferate and make the center mass deprived of nutrition from peripheral tissues. It results in necrotic changes in the center lined by epithelial cells at the periphery.
Radicular Cyst Abscess Theory:
It says when an abscess is formed in connective tissue, epithelial cells proliferate and form a wall around the cavity because of their inherent tendency to cover the exposed connective tissue.
Valderhaug (1972) explained the following stages of cyst formation:
1. Initial stage:
Bacterial endotoxins cause inflammation in the apical region of a nonvital tooth which leads to the proliferation of epithelial cells of Malassez.
2. Cyst development stage:
Proliferative epithelial cells serve as building blocks for cyst wall development. This occurs due to simultaneous decomposition of epithelial and granulation tissue and convergence of multiple cavities, with subsequent epithelialization.
3. Cyst growth stage:
Due to the decomposition of epithelial cells, leukocytes, and accumulation of plasma exudates, the osmolality of the cyst fluid becomes higher than that of the serum. As a result, hydrostatic internal pressure becomes greater than capillary pressure. Tissue fluid, therefore, diffuses into the cyst, making it increase in size.
With osteoclastic bone resorption, the cyst expands. Other bone-resorbing factors, such as prostaglandins, interleukins, and proteinases, from inflammatory cells and cells in the peripheral portion of the lesion, permit additional cyst enlargement
Types of Radicular Cysts:
Nair gave the following two types of radicular cysts:
Periapical Pocket or Bay Cyst:
When proliferation occurs within the body of the granuloma, it plugs the apical foramen which limits the egress of bacteria. Sometimes, epithelial plugs protrude out from the apical foramen resulting in a pouch connected to the root and continuous with the root canal. This is termed as pocket or bay cyst.
Periapical True Cyst:
It is the cavity which is completely enclosed in epithelium lining and is independent of root canal of the offending tooth.
Radicular Cyst Clinical Features:
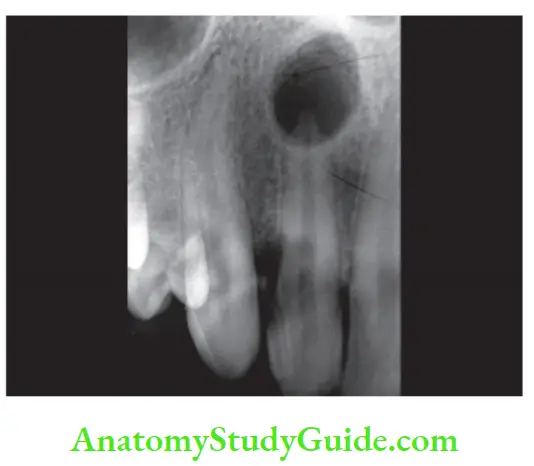
- Cyst is generally asymptomatic. It is discovered when periapical radiographs of a nonvital tooth is taken.
- Males are affected more than females.
- Peak incidence in the third or fourth decades.
- Commonly found in the anterior maxilla. In mandibular posterior teeth, separate small cysts may arise from each apex of multirooted teeth.
- The involved tooth is nonvital, discolored, fractured, or shows failed root canal.
- It grows as a slowly enlarging swelling. As the cyst increases in size, the covering bone becomes thin and exhibits springiness due to fluctuation.
- In the maxilla, palatal expansion is commonly seen with the maxillary lateral incisor.
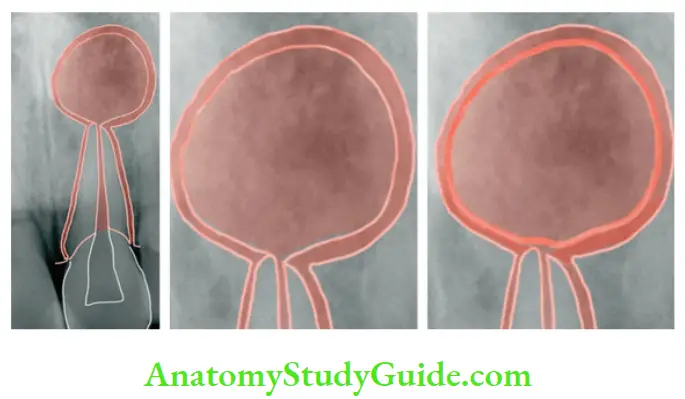
Radiographic Features:
Radiographically, the radicular cyst appears as round, pear, or ovoid-shaped radiolucency, outlined by a thin radiopaque margin.
Diffrential diagnosis:
1. Periapical granuloma:
Histological and radiological features differentiate these lesions. Moreover, the cyst is usually larger than a periapical granuloma.
2. Periapical cemento-osseous dysplasia:
It is seen associated with vital teeth or in regions of extractions. Lesion tends to become more opaque internally with time and does not exhibit extensions into adjacent bone.
3. Traumatic bone cyst:
Hollow cavity, not lined by epithelium but by fibrous tissue. Treated by aspiration of fluid from the cavity.
4. Globulomaxillary cyst:
A fissural cyst, a tooth may be vital and develops between the maxillary lateral incisor and canine
5. Lateral periodontal cyst:
It is associated with periodontal signs and symptoms.
6. Normal bony cavity:
It appears dissociated from the root apex whereas the residual cyst remains attached to the root apex.
7. Previously treated apical pathology/surgical defect or periapical scar.
8. Odontogenic tumors:
Ossifying fibroma is commonly seen in the posterior region of the mandible, adenomatoid odontogenic tumor in the anterior maxilla, and calcifying cystic odontogenic tumor is associated with unerupted teeth. In these lesions, the pulp is usually vital.
9. Giant cell lesion
10. Metastatic lesion
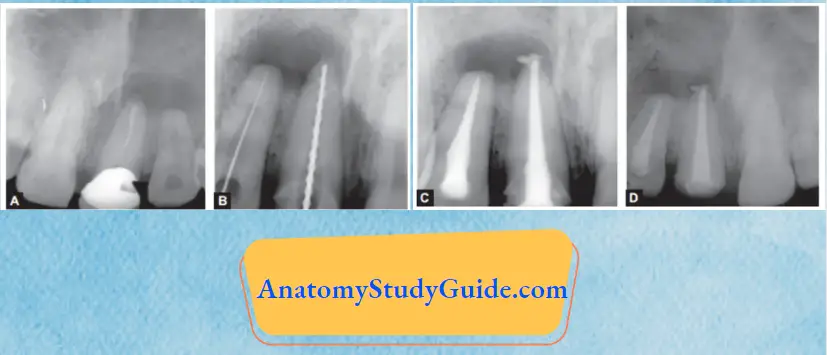
Radicular Cyst Treatment:
Different options for the management of residual cysts are
- Endodontic treatment
- Apicoectomy
- Extraction (severe bone loss)
- Enucleation with primary closure
- Marsupialization (in case of large cysts)
Condensing Osteitis
Condensing osteitis is a diffuse radiopaque lesion believed to form a localized bone reaction to a low-grade inflammatory stimulus, normally seen at an apex of a tooth in which there has been a long-standing pulp disease.
Condensing Osteitis Clinical Features:
- Usually asymptomatic, it is commonly seen around the apices of mandibular molars and premolars with chronic pulpitis.
- The pulp can be vital and chronically inflamed or necrotic.
- The tooth has a radiopaque area due to the overproduction of bone in the periapical area. Radiopacity may or may not disappear after endodontic treatment or tooth extraction.
Condensing Osteitis Diagnosis:
Usually discovered on routine radiographs, it appears as a localized area of radiopacity surrounding the offending tooth.
Condensing Osteitis Histopathology:
The dense bone around the root apex shows less trabecular pattern and borders lined with osteoblasts along with the presence of chronic inflammatory cells in bone marrow.
Condensing Osteitis Treatment:
- Endodontic treatment may result in complete resolution.
External Root Resorption
Resorption is associated with either a physiologic or a pathologic process that results in the loss of tissues like dentin, cementum, or alveolar bone.
In external root resorption, root resorption affects the cementum or dentin of the root. It can be
- Apical root resorption
- Lateral root resorption
- Cervical root resorption
Etiology:
Periradicular inflammation due to
- Infected necrotic pulp
- Over-instrumentation during root canal treatment
- Trauma
- Granuloma/cyst applying excessive pressure on the root
- Replantation of teeth
- Adjacent impacted tooth
External Root Resorption Symptoms:
- Asymptomatic during development
- When the root is completely resorbed, the tooth becomes mobile
- When external root resorption extends to the crown, it gives a “pink tooth” appearance.
- When replacement resorption results in ankylosis, the tooth becomes immobile with a characteristic high percussion sound.
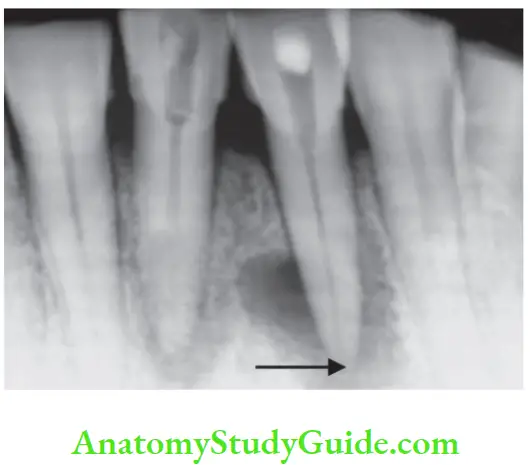
External Root Resorption Radiographic Features:
- Radiolucency at the root and adjacent bone
- Irregular shortening or thinning of the root tip
- Loss of lamina dura
External Root Resorption Diffrential Diagnosis:
It should be diffrentiated from internal resorption which shows ballooning of pulpal space.
External Root Resorption Treatment:
- Removal of the stimulus of underlying inflammation
- Nonsurgical endodontic treatment should be tried first before attempting surgical treatment.
Persistent Apical Periodontitis
It is post-treatment apical periodontitis in an endodontically treated tooth. Enterococcus faecalis is the most consistently reported organism in persistent apical periodontitis.
Etiology:
- It may result because of incomplete cleaning of complex pulp space which is inaccessible to instrumentation, irrigation, and thus obturation.
- Nair listed the following extraarticular factors which contribute to persistent apical periodontitis:
- Foreign body reaction to gutta-percha
- Periapical biofilms
- Cholesterol crystals
- Periapical scar tissue
- Actinomyces infection

Diseases Of Periradicular Tissue Of Nonendodontic Origin
Periradicular lesions may arise from the remnants of odontogenic epithelium.
Benign Lesions:
- Early stages of periradicular cemental dysplasia
- Early stages of monostotic fibrous dysplasia
- Ossifying fibroma
- Primordial cyst
- Lateral periodontal cyst
- Dentigerous cyst
- Traumatic bone cyst
- Central giant cell granuloma
- Central hemangioma
- Hyperparathyroidism
- Myxoma
- Ameloblastoma
Radiographic Features of Lesions of Nonodontogenic Origin:
- Presence of radiolucent areas
- Intact lamina dura
Diagnosis:
Teeth associated with nonodontogenic lesions are usually vital. The final diagnosis is based on a surgical biopsy and histopathological examination.
Malignant Lesions:
They simulate endodontic periradicular lesions and are often metastatic in nature:
- Squamous cell carcinoma
- Osteogenic sarcoma
- Chondrosarcoma
- Multiple myeloma
Diagnosis:
1. Vitality:
The involved tooth is vital but disruption of sensory nerves may show no response
2. Radiographic features:
Lesions are associated with rapid and extensive loss of hard tissue, that is, bone and tooth.
3. Biopsy:
Histological evaluation of diagnosis.
Conclusion:
One of the most important clinical factors for pulpal pain is caries which affects pulp by bacteria or their byproducts. Once the pulp gets affected by bacteria or their by-products, its inflammation starts, which if not timely treated, might develop into pulp necrosis.
Toxic byproducts formed as a result of pulp decomposition act as irritants on the periapical tissues and give rise to many forms of reactions and the latter involve periradicular tissues.
Some of these reactions occur for a short time accompanied by signs and symptoms, others develop slowly and are asymptomatic. To save a tooth from sacrificing, a proper diagnosis based on clinical, radiographically, and histological basis should be made so as to provide optimal treatment to the lesion.
In suspicious cases, a biopsy of the lesion, referral to the pathologist, and long-term follow-up is required.
Leave a Reply