Pericardium and Heart
Pericardial Effusion
1. The accumulation of fluid in the pericardial sac is called pericardial effusion.
Table of Contents
2. Pericardial tamponade: Pericardial effusion compresses the heart and decreases the diastolic capacity of heart. It also reduces cardiac output. This results in diminished cardiac output but increased pulse rate and increased venous pressure.
3. Paracentesis: Aspiration of pericardial fluid is called paracentesis. It is done by
- Subcostal route: The needle is passed in the angle between the xiphoid process and left costal margin. The direction of needle is upwards, backwards and to the left.
- Parasternal route: It is drained by puncturing the left 5th or 6th intercostal space just lateral to the sternum.
Read And Learn More: Anatomy Important Question And Answers
Describe the Fibrous Pericardium under following heads
1. Fibrous Pericardium Gross anatomy,
2. Fibrous Pericardium Functions, and
3. Fibrous Pericardium Development.
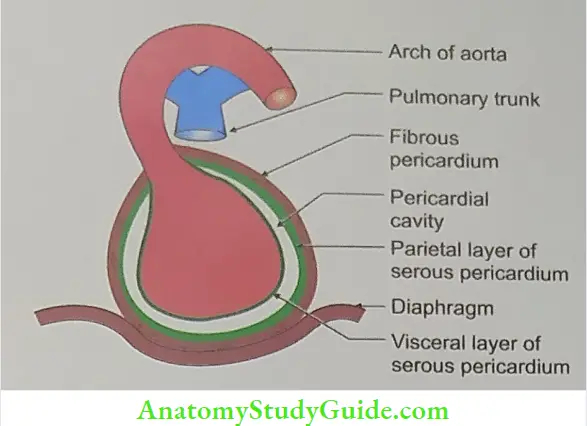
1. Fibrous Pericardium Gross anatomy
- Synonymous: Outer layer of pericardium.
- Introduction: It is a cone shaped open sac and has apex and base.
- Apex: It merges with the tunica adventitia of (pulmonary trunk and ascending aorta) and pretracheal layer of the deep cervical fascia.
- Base: It fuses with the upper surface of central tendon and musculature of the left part of the diaphragm.
- In front: It is attached to the upper and lower ends of the body of sternum by the superior and inferior sternopericardial ligaments, respectively.
- Structures piercing fibrous pericardium.
- Ascending aorta,
- Pulmonary trunk,
- Two venae cavae, and
- Four pulmonary veins.
- Fibrous Pericardium Relations
- Anteriorly: Thoracic wall is separated by lung, pleura and occasionally by thymus.
- Posteriorly
- Right and left bronchi,
- Oesophagus,
- Oesophageal plexus of nerves,
- Descending thoracic aorta,
- Thoracic duct,
- Azygos vein,
- Hemiazygos vein, and
- Posterior part of the mediastinal surface of both lungs.
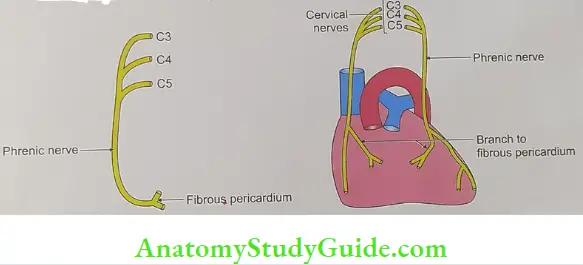
- On each side
- Cardiac impression of the corresponding lung,
- Phrenic nerves, and
- Pericardiacophrenic vessels.
- Below
- Left lobe of the liver, and
- Fundus of the stomach.
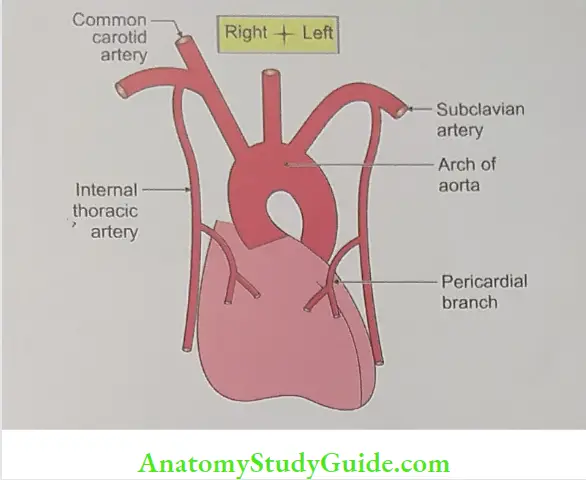
- Fibrous Pericardium Blood supply
- Arterial supply
- Pericardiacophrenic artery (branch of internal thoracic artery),
- Musculophrenic artery (terminal branch of internal thoracic artery), and
- Branches of descending thoracic aorta.
- Arterial supply
Venous drainage
- Azygos vein, and
- Internal thoracic vein.
Fibrous Pericardium Nerve supply: Fibrous pericardium is pain sensitive and is supplied by phrenic nerve.
2. Fibrous Pericardium Functions
- It keeps the heart in position, and
- It prevents over distension of the heart.
3. Development: It develops from septum transversum.
LAQ-6 Describe the Serous Pericardium under following heads
1. Serous Pericardium Gross anatomy,
2. Serous Pericardium Functions,
3. Serous Pericardium Development, and
4. Serous Pericardium Applied anatomy
1. Serous Pericardium Gross anatomy
- Synonymous: Inner layer of pericardium.
- Introduction: It is a closed sac and lines the inner wall of the fibrous pericardium. It consists of
- Visceral layer (epicardium), and
- Parietal layer. There is a potential sac present between fibrous and visceral layers. The maximum capacity of the sac is 300 ml.
- Blood supply
- Arterial supply: Coronary arteries, branches of ascending aorta.
- Venous drainage: Coronary sinus.
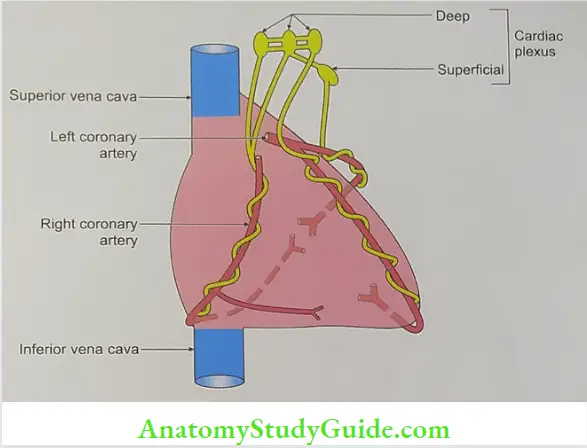
- Nerve supply: Cardiac plexus
Serous Pericardium Functions
- It allows the free movement of the heart within the fibrous pericardium.
- It keeps the surface moist and slippery.
Serous Pericardium Development
- Parietal layer of the serous pericardium develops from somatopleuric layer of pericardial sac.
- Visceral layer of serous pericardium develops from splanchnopleuric layer of pericardial sac.
Serous Pericardium Applied anatomy
- The accumulation of fluid in the pericardial sac is called pericardial effusion.
- Pericardial tamponade: Pericardial effusion compresses the heart and decreases the diastolic capacity of heart. This results in diminished cardiac output but increased pulse rate and increased venous pressure.
- Paracentesis: Aspiration of pericardial fluid is called pericardiocentesis. It is done under ultrasonography (USG) control by
- Subcostal route: The needle is passed in the angle between the xiphoid process and left costal margin. The direction of needle is upwards, backwards and to the left.
- Parasternal route: It is drained by puncturing the left 5th or 6th intercostal space just lateral to the sternum.
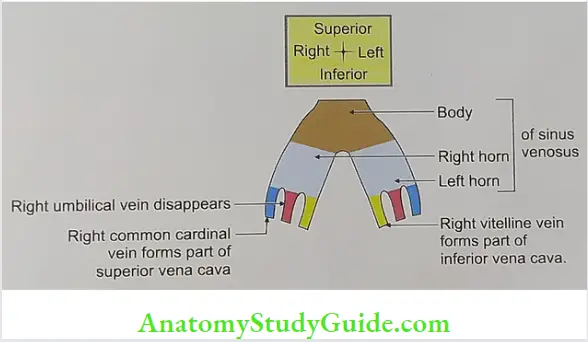
Name the derivatives of sinus venosus.
1. The sinus venosus lies at the venous end of the heart.
- Right and left horns.
- One vitelline vein (from the yolk sac),
- One umbilical vein (from the placenta), and
- One common cardinal vein (from the body wall) join each horn of the sinus venosus.
- Left horn of the sinus venosus remains very small. It becomes part of the coronary sinus.
- Right common cardinal vein becomes part of the superior vena cava.
- Right vitelline vein forms the terminal part of the inferior vena cava. After absorption of the sinus venosus into the right atrium, the coronary sinus and the venae cavae are seen opening into the atrium.
- The right margin of the original sinoatrial orifice (i.e. the right venous valve) expands very greatly and divides into three parts which form the
- Crista terminalis,
- Valve of the inferior vena cava, and the
- Valve of the coronary sinus.
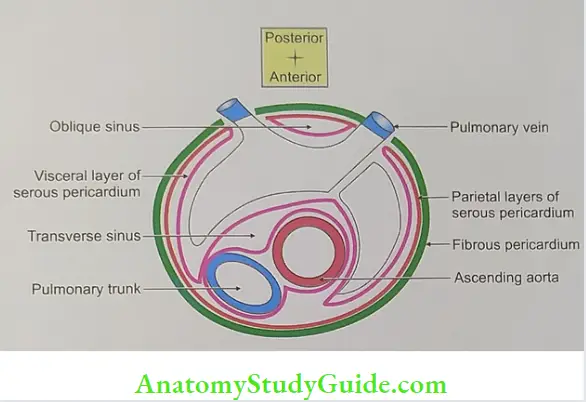
Transverse sinus (intervisceral space)
Transverse Sinus Synonymous: Intervisceral space.
Transverse Sinus Introduction: It is a horizontal gap present between arterial and venous ends of heart tube
- Arterial end
- Ascending aorta, and
- Pulmonary trunk.
- Venous end
- Superior vena cava,
- Inferior vena cava, and
- Pulmonary vein.
3. Transverse Sinus Location: It is present between two layers of visceral part of serous pericardium and situated on the upper part of the posterior surface of the heart.
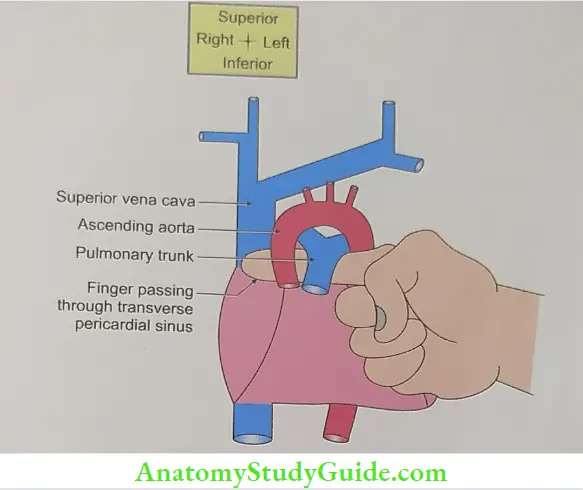
4. Boundaries
- Anteriorly
- Ascending aorta, and
- Pulmonary trunk.
- Posteriorly
- Intrapericardial part of superior vena cava,
- Upper margin of left atrium, and
- Four pulmonary veins.
- Superiorly: Bifurcation of pulmonary trunk.
- Inferiorly: Upper surface of left atrium.
- Each side: Pericardial cavity
Development: It develops from degeneration of the central cells of dorsal mesocardium.
Transverse Sinus Applied anatomy: During cardiac surgery, the ligature may be passed through the transverse sinus around the aorta and pulmonary trunk. The tubes of heart lung machine are inserted into the vessels and ligature is tightened.
Oblique Sinus
1. Oblique Sinus Synonymous: Parietovisceral space.
2. Oblique Sinus Introduction: It is a cul-de-sac (blind alley: 3) present behind left atrium or it is a space between four pulmonary veins. It is closed on all sides except inferiorly.
3. Oblique Sinus Location: It is located on the posterior surface of heart between parietal and visceral layers of pericardium.
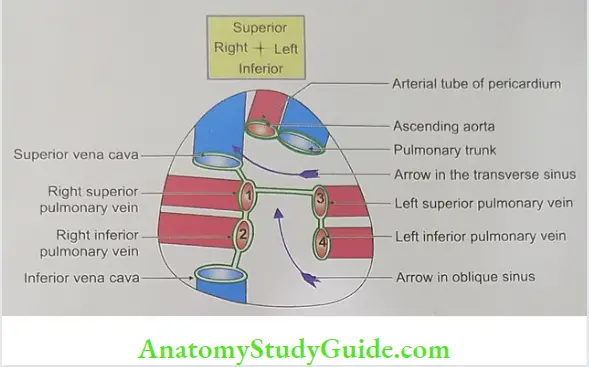
4. Oblique Sinus Formation: It is formed by a reflected part of parietal pericardium.
5. Oblique Sinus Boundaries
- Anteriorly: Posterior surface of left atrium.
- Posteriorly: Parietal pericardium.
- On right side: Right pair of pulmonary veins and inferior vena cava.
- On left side: Left pair of pulmonary veins.
- Above: Upper margin of left atrium.
6. Functions
- It suspends heart in pericardial cavity, and
- It permits free pulsations of left atrium.
7. Development: It is developed due to the rearrangement of the veins at venous end.
8. Applied anatomy: Oblique sinus permits the distension of left atrium during return of oxygenated blood from lung.
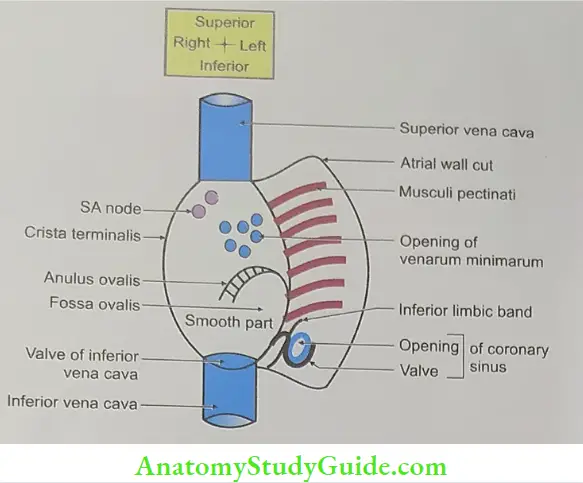
OLA-10 State the structures opening into right atrium.
1. Superior vena cava brings venous blood from upper half of the body.
2. Inferior vena cava brings venous blood from lower half of the body.
3. Coronary sinus brings venous blood from the substance of heart.
LAQ-7 Describe right atrium under following heads
1. Gross anatomy,
2. Development, and
3. Applied anatomy.
1. Gross anatomy
- Introduction: It is upper right chamber of heart, which receives venous blood from all parts of the body by following veins.
- Superior vena cava brings venous blood from upper half of the body,
- Inferior vena cava brings venous blood from lower half of the body, and
- Coronary sinus brings venous blood from the substance of heart.
- Right atrium forms
- Right and upper border of the heart, and
- Sternocostal surface and base of the heart.
- Extent: It extends from the opening of superior vena cava to the opening of inferior vena cava. It corresponds to right 3rd costal cartilage to right 6th costal cartilage.
- External features: It is elongated chamber and presents following features
- Right auricle
- It is an ear-like projection arising from right atrium. It covers
- Ascending aorta, and
- Infundibulum of right ventricle.
- Its margins are notched and interior surface is sponge-like.
- It prevents free flow of blood but favours thrombosis. It causes pulmonary embolism in auricular fibrillation.
- Sulcus terminalis: It extends
- From the angle made by superior vena cava and the right margin of right auricle, and
- To right border of inferior vena cava.
- Interior of the right atrium: It is divided into three parts (Fig. 17.11)
- Anterior part (It is also called pectinate part or rough part.): It shows following features
- Crista terminalis: It is produced by internal muscular ridge.
- Transverse muscular ridges: They are called musculi pectinati. They give the appearance of teeth of comb. They arise from crista terminalis and inserts on atrioventricular orifice. They are connected to each other and form reticular network.
- Posterior part: It is also called sinus venarum or smooth part. It demonstrates following features
- Intravenous tubercle of lower,
- Site: It is present between superior and inferior venae cavae.
- Function: In foetal life, it directs the flow of blood from superior vena cava to right ventricle.
- Anterior part (It is also called pectinate part or rough part.): It shows following features
-
-
- Opening of superior vena cava
- Opening of inferior vena cava: It is guarded by eustachian valve which is formed by duplication of the endocardium. It contains few muscle fibres. In foetal life, the valve regulates the flow of blood from the inferior vena cava to the left atrium through the foramen ovale.
- Coronary sinus: It is guarded by valve of coronary sinus.
- Openings of the venae cordis minimi (Thebesian vein).
-
- Septal wall (It is also called central part of posterior wall.)
- Fossa ovalis a shallow saucer primum shaped depression, derived from septum
- Limbus fossa ovalis: It is a prominent margin of fossa ovalis. Its anterior edge is continuous with left end of valve of inferior vena cava. It is developed from septum secundum.
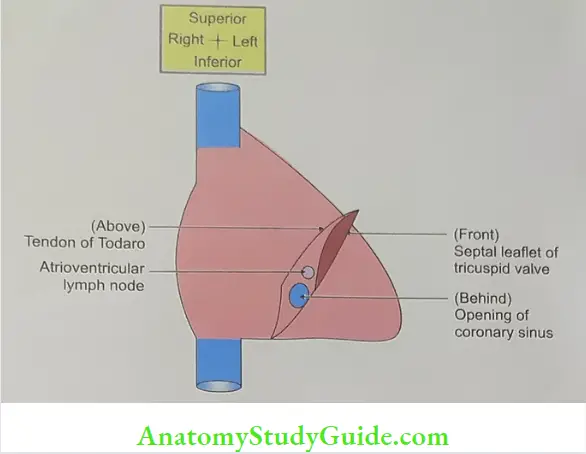
- ▲ of Koch:
- Boundaries
- Anteriorly: Septal leaflet of tricuspid valve
- Posteriorly: Opening of coronary sinus
- Superiorly: Tendon of Todaro
- Content: AV node
- Torus aorticus: It is elevation formed by non-coronary sinus (right posterior aortic sinus).
- Relations
- Anterior
- Pericardium,
- Pleura, and
- Anterior part of the mediastinal surface of lung.
- Posterior
- Right: Pair of pulmonary veins
- Left: Interatrial septum
- Right lateral border
- Right phrenic nerve and pericardiacophrenic vessels,
- Mediastinal pleura, and
- Cardiac impression of right lung.
- Medial border
- Root of ascending aorta, and
- Root of pulmonary trunk.
- Blood supply
- Arterial : Right coronary artery, branch of ascending aorta.
- Venous : Drains into coronary sinus.
- Development
- Chronological age: It develops at the end of 4th week of intrauterine life (IUL)
- Germ layer: Mesoderm
- The endocardium develops from angioblastic tissue.
- The myocardium develops from splanchnopleuric mesoderm.
- The pericardium develops from somatopleuric intraembryonic mesoderm.
- Anterior
- Site: Primitive atrial chamber.
- Sources: It is divided into
- Posterior smooth part (sinus venarum) develops from the absorption of the right horn of sinus venosus.
- Crista terminalis develops from
- Upper part of right venous valve, and
- Septum spurium (false).
- Valves of the inferior vena cava and coronary sinus develop from lower part of the right venous valve.
- Rough trabeculated part (atrium proper) and right auricle develops from right half of the primitive atrium.
- Most ventral smooth part is derived from right half of the atrioventricular canal.
- Upper part of interatrial septum develops from septum secundum and lower part from septum primum.
- Anomalies
- Atrial septal defect: It is due to the failure of fusion of the septum primum and the septum secundum. This results into admixture of arterial and venous blood.
- Patent foramen ovale.
- Persistence of foramen primum.
- Persistence of foramen secundum.
Applied anatomy
- Pressure in the right atrium can be measured by recording venous pressure in external jugular vein.
- For the repair of the atrial septal defect, the right atrium is incised along the right border avoiding the region of SA node.
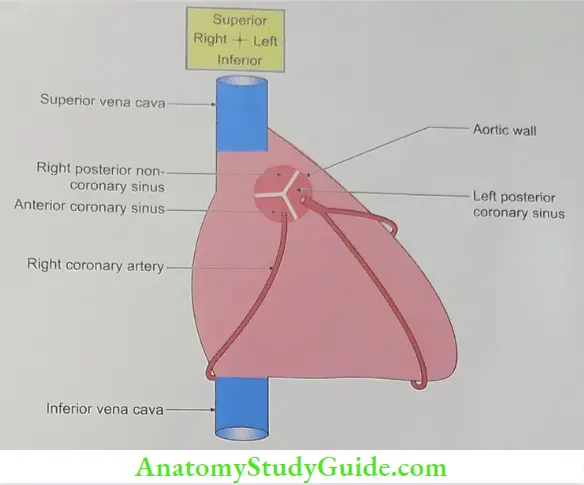
OLA-11 Name the aortic sinuses giving origin to coronary arteries.
Anterior coronary sinus gives origin to right coronary artery.
Left posterior coronary sinus gives origin to left coronary artery.
Peculiarities of coronary arteries
The following are the peculiarities of coronary arteries. They can be memorized by the ord
functional end arteries FEA
- Filled in diastole.
- Elastic lamina is absent.
- Artery of artery.
Functional end artery: The coronary arteries reveal communications, i.e. they do anastomose. Hence, structurally they are not end arteries. But in case of blockage of coronary artery, the blood received through anastomosing channel is so less that they do not meet the required demand. Therefore, they are called functional end arteries.
2. Filled in diastole: All the blood vessels in the body are filled in systole. However, coronary arteries are filled in diastole.
3. Elastic lamina is absent: Coronary arteries are highly muscular vessels and internal elastic lamina is discontinuous and poorly developed.
4. Coronary arteries demonstrate the longitudinal oriented muscles in the outer part of intima or inner part of media.
Applied anatomy of coronary arteries.
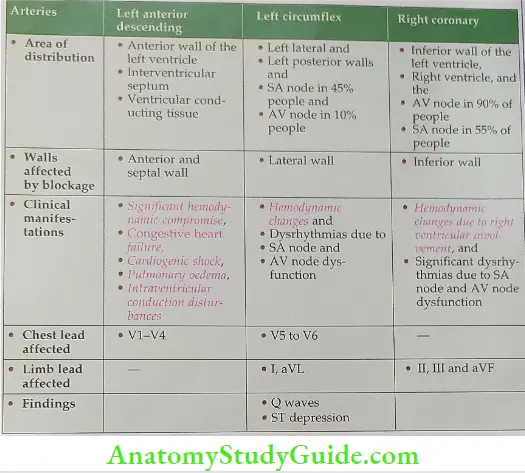
Applied anatomy of different coronary arteries
There are three main coronary arteries supplying the myocardium
1. Left anterior descending artery
2. Left circumflex artery
3. Right coronary artery
1. Left anterior descending artery (interventricular artery)
- Supplies blood to
- Anterior wall of the left ventricle,
- Interventricular septum, and
- Ventricular conducting tissue.
- If it is blocked by thrombus, it causes anteroseptal myocardial infarction.
- Clinical manifestations
- Significant hemodynamic compromise,
- Congestive heart failure,
- Cardiogenic shock,
- Pulmonary oedema,
- Intraventricular conduction disturbances.
This is the most severe form of myocardial infarction.
- ECG changes are seen in chest leads
- V1 to V4 in the form of Q waves, and
- ST segment elevations.
- Left circumflex artery
- Supplies blood to
- Left lateral and
- Left posterior walls
- SA node in 45% people, and
- AV node in 10% people.
- If it is blocked by thrombus, it causes lateral wall myocardial infarction.
- Clinical manifestations
- Hemodynamic changes and
- Dysrhythmias due to
- SA node and
- AV node dysfunction
- ECG changes are seen in
- Limb leads I, aVL and
- Chest leads V5 to V6 in the form of Q waves, and
- ST segment elevations.
- Right coronary artery
- Supplies blood to
- Inferior wall of the left ventricle,
- Right ventricle, and the
- AV node in 90% of people
- SA node in 55% of people.
- If it is blocked by thrombus, it causes-inferior wall myocardial infarction
- Clinically myocardial infarction can lead to some
- Hemodynamic changes due to right ventricular involvement, and
- Significant dysrhythmias due to SA node and AV node dysfunction.
- ECG changes are seen in
- Limb leads II, III and aVF in the form of
- Q waves, and
- ST segment elevations.
- Limb leads II, III and aVF in the form of
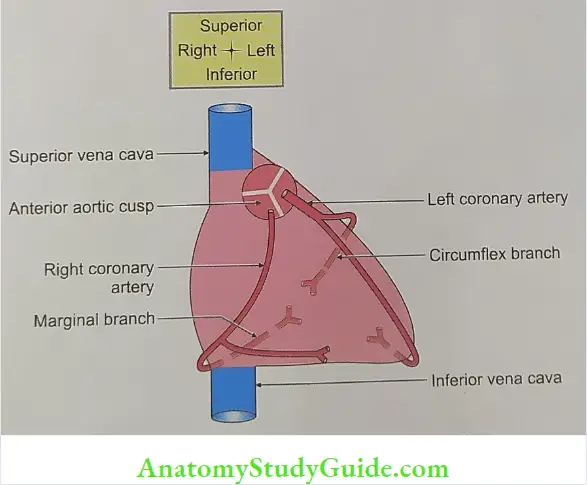
LAQ-8 Describe right coronary artery under following heads
1. Coronary Artery Origin,
2. Coronary Artery Course,
3. Coronary Artery Branches,
4. Coronary Artery Distribution, and
5. Coronary Artery Applied anatomy.
1. Coronary Artery Origin: It arises from anterior aortic sinus of ascending aorta.
2. Coronary Artery Course
- It passes between right auricular appendage and the infundibulum of the right ventricle.
- It passes vertically downwards in the atrioventricular groove (coronary sulcus).
- The artery turns backwards at the inferior border of the heart and runs posteriorly. The terminal part of the right coronary artery is small and anastomoses with the circumflex branch of left coronary artery.
- Peculiarity: Right coronary artery has a characteristic loop at the point where the posterior interventricular artery and AV nodal artery arises.
3. Coronary Artery Branches
Collateral branches
- Right conus artery
- The word ‘conus’ means cone. It is a 1st branch of right coronary artery.
- It is meant for the nutrition of the conus arteriosus.
- It may arise as the 3rd coronary artery.
- It anastomoses with the left conus artery, a branch of the anterior inter- ventricular branch of the left coronary artery to form an anastomotic necklace around the infundibulum or the commencement of the pulmonary trunk.
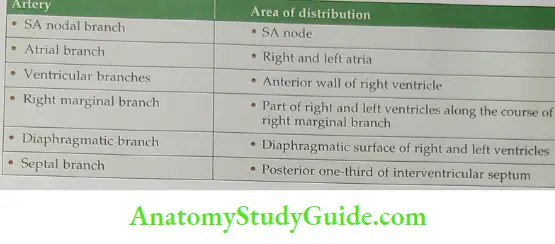
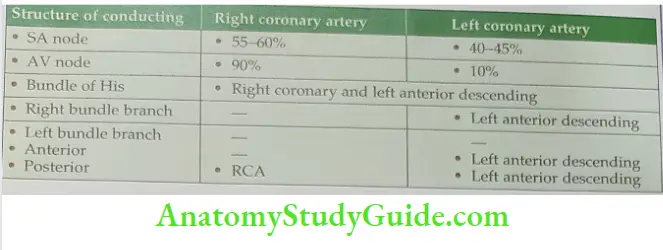
- SA nodal artery: It forms vascular ring around the termination of superior vena cava. It supplies SA node in 60% of the heart.
- Right anterior ventricular branches: They are 3 to 4 in number. They pass along the sternocostal surface and as the name suggests they supply anterior surface of right ventricle. One of the branches is the longest and is known as right marginal artery. It runs along the inferior border of the heart.
- AV nodal artery: This supplies AV node.
Coronary Artery Terminal branches
- Posterior interventricular branch: It passes along the interventricular groove towards the apex of the heart to supply the diaphragmatic surface of right ventricle.
- Transverse branch.
4. Coronary Artery Distribution
- Right atrium,
- SA node,
- Superior parts of the right ventricle,
- Posterior one-third of interventricular septum,
- AV node, and
- Right AV bundle.
Note: Right bundle branch is not supplied by right coronary artery.
5. Coronary Artery Applied anatomy
- Although the coronary arteries have numerous anastomoses at the arteriolar level, they are essentially ‘functional end arteries’, i.e. when a coronary artery is blocked demand in required time. the blood received by collateral channels is inadequate to meet the required the blood received by collateral channels is inadequate to meet the required demand in required time.
- The cardiac pain (due to angina pectoris or myocardial infarction) is usually referred to the left chest wall and inner aspects of left arm and forearm.
- The heart is supplied by upper four thoracic (i.e. T1-T4) spinal segments. The skin over precordium is supplied by T2, T3 and T4 spinal segments. The inner aspect of arm is innervated by T2 spinal segment. And the inner aspect of forearm and hand is innervated by T1 spinal segment.
- The cardiac pain is, therefore, referred to the precordium and inner aspects of the arm and forearm because of the same segmental innervation.
- The cardiac pain is usually referred to the left side because cardiac lesions mostly occur in the left half of the heart, but if the lesion is in right half of the heart, the pain will be referred on the right side. Hence it is wrong notion that cardiac pain is always referred to the left side ‘the left arm myth’.
- The coronary disease in old age is less fatal than in young age. The anastomoses and collateral channels increase as age advances.
- The slow gradual blocking coronary artery is less dangerous than sudden blockage because the arteries taking part in extra pericardiac anastomosis will dilate and provide blood supply to the heart.
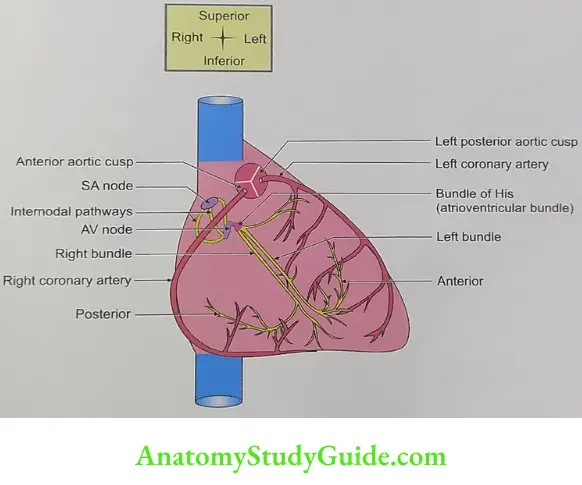
Blood supply of cardiac conduction system
OLA-12 Name any two branches of left coronary artery.
1. Anterior interventricular branch, and
2. Circumflex branch.
LAQ-9 Describe left coronary artery under following heads
1. Left Coronary Artery Origin,
2. Left Coronary Artery Course,
3. Left Coronary Artery Branches,
4. Left Coronary Artery Distribution, and
5. Left Coronary Artery Applied anatomy.
1. Left Coronary Artery Origin: It is shorter and wider than the right coronary artery and supplies the greater mass of myocardium. It arises from left posterior aortic sinus of ascending aorta.
2. Left Coronary Artery Course
- It passes between left auricle and the infundibulum of the right ventricle.
- After the short course, it divides into two terminal branches (circumflex and anterior interventricular).
- The circumflex branch is one of the two terminal branches of left coronary artery, runs from the left border of the heart to the back of the heart in the interventricular groove.
- It gives various branches to atrium and ventricle and anastomosis with the right coronary artery.
Branches
- Anterior interventricular artery (left anterior descending artery-LADy artery): It is downward continuation of the main trunk along the anterior interventricular It winds around the inferior border of the heart to anastomoses with the groove. posterior interventricular artery, i.e. junction of anterior one-third and posterior two-thirds of the posterior interventricular groove. It has following branches.
- Anterior ventricular branches for the sternocostal surfaces of both left and right ventricles.
- The large branch is called “left diagonal artery”.
- One of the right anterior ventricular branches gives the left conus artery. It supplies the conus arteriosus of the right ventricle and forms anastomotic necklace with the right conus artery, branch of right coronary artery.
- Septal branches supply anterior two-thirds of the interventricular septum.
3. Left Coronary Artery Circumflex artery: It passes along the left part of the posterior atrioventricular groove. The branches are as follows.
- Atrial branches: They are in three groups: Anterior, lateral and posterior for each corresponding three surfaces of the left atrium.
- Ventricular branches: They are 1 to 5 in number. One of these branches is larger and descends along the left border of the heart. It reaches the apex of the heart and is called left marginal artery.
- Nodal artery for the SA node in 35% of cases.
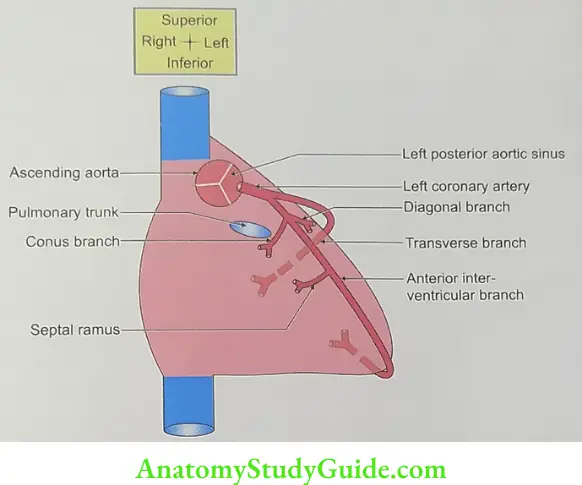
4. Left Coronary Artery Distribution
- Anterior aspects of both right and left ventricles,
- Anterior two-thirds of the ventricular septum,
- Left branch of the AV bundle,
- Left surface of the left ventricle, and
- Posterior aspect of the left atrium.
5. Left Coronary Artery Applied anatomy
- Anterior interventricular branch of left coronary artery (left anterior descending artery-LADy artery) is the most commonly occluded vessel in the myocardial infarction. The circumflex branch of left coronary artery is a 3rd commonly occluded vessel in myocardial infarction. This artery is also called widow maker artery. A widow maker heart attack is a type of heart attack that is caused by 100% blockage of the left anterior descending artery. It is also called “chronic total obstruction”.
- The left coronary artery in addition to the usual distribution, supplies blood to the entire interventricular septum and atrioventricular node. In such cases, it is called left dominant coronary artery.
- Although the coronary arteries have numerous anastomoses at the arteriolar level, they are essentially ‘functional end arteries’, i.e. when a coronary artery is blocked the blood received by collateral channels is inadequate to meet the required demand in required time.
- The cardiac pain (due to angina pectoris or myocardial infarction) is usually referred to the left precordium and inner aspects of left arm and forearm.
- The heart is supplied by upper four thoracic (i.e. T1-T4) spinal segments. The skin over precordium is supplied by T4, T3 and T2 spinal segments. The inner aspect of arm is innervated by T2 spinal segment. And the inner aspect of forearm and hand is innervated by T1 spinal segment.
- The cardiac pain is, therefore, referred to the precordium and inner aspects of the arm and forearm because of the same segmental innervation.
- The cardiac pain is usually referred to the left side because cardiac lesions mostly occur in the left half of the heart, but if the lesion is in right half of the heart, the pain will be referred on the right side. Hence, it is wrong notion that cardiac pain is always referred to the left side ‘the left arm myth’.
- The coronary disease in old age is less fatal than in young age because anastomoses increase and collateral channels develop with the advancement of age.
- The slow gradual blocking coronary artery is less dangerous than sudden blockage because the arteries taking part in extra pericardiac anastomosis will dilate and provide blood supply to the heart.
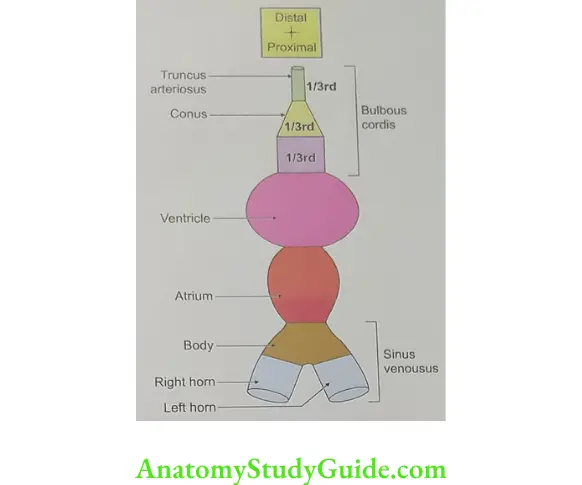
LAQ-13 Name the parts of heart tube.
Two endothelial heart tubes (right and left) appear and fuse to form one tube. This tube has a venous end and an arterial end.
- series of dilatations appear on this tube. These are Bulbus cordis,
- Proximal one-third (which is dilated),
- Middle one-third called the conus, and
- Distal one-third called the truncus arteriosus.
- Ventricle,
- Atrioventricular canal: Narrow part connecting atrium and ventricle is the
- Atrium,
- Sinus venosus, and
- Right and left horns.
OLA-14 Name the structures that fuse with each other at the level of atriovent- ricular canals so as to separate right and left side of the heart.
1. Septum primum, and
2. Two endocardial cushions.
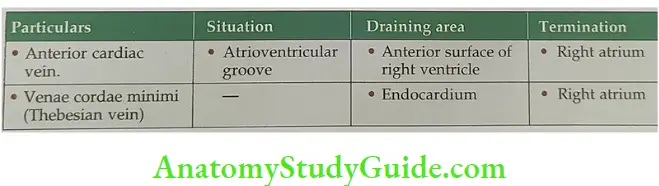
LAQ-10 Venous drainage of the heart
The veins draining the heart are divided in two groups.
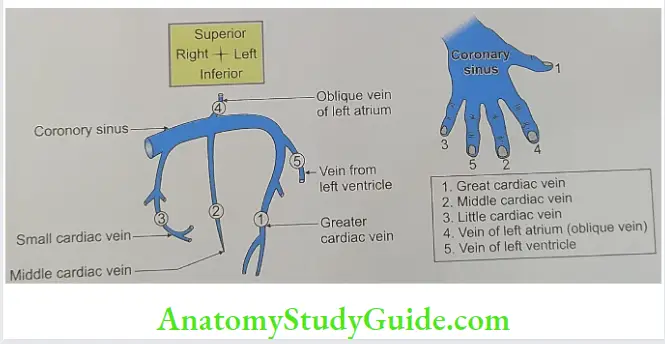
1. Veins draining into coronary sinus: This is a wide vessel that lies in the posterior part of atrioventricular groove. It is covered by a thin layer of myocardium. It opens in the posterior wall of right atrium. It is left to the opening of inferior vena cava. The tributaries of the coronary sinus are compared to fingers of hand to memorize
- Thumb represents great cardiac vein.
- Middle finger represents middle cardiac vein.
- Little finger represents small cardiac vein.
- Index finger indicates oblique vein of left atrium of Marshall.
- Ring finger represents posterior vein of left ventricle.
The tributaries of the coronary sinus and their details are described in
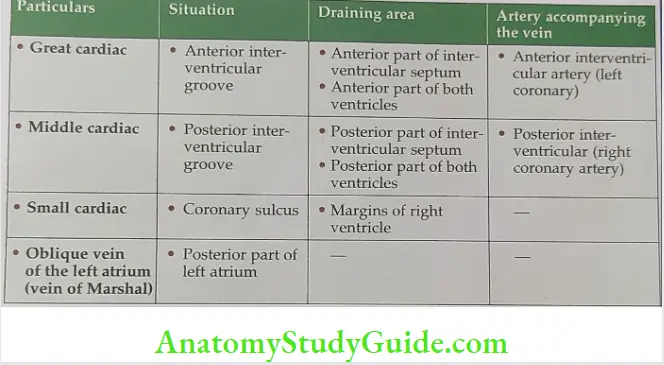
2. Veins directly opening into the right atrium are described in
Development of interatrial septum
1. Chronological age: It develops in the 4th week of intrauterine life (TUL).
2. Germ layer: Splanchnic layer of lateral plate mesoderm.
3. Site: From the roof of primitive atrial chamber.
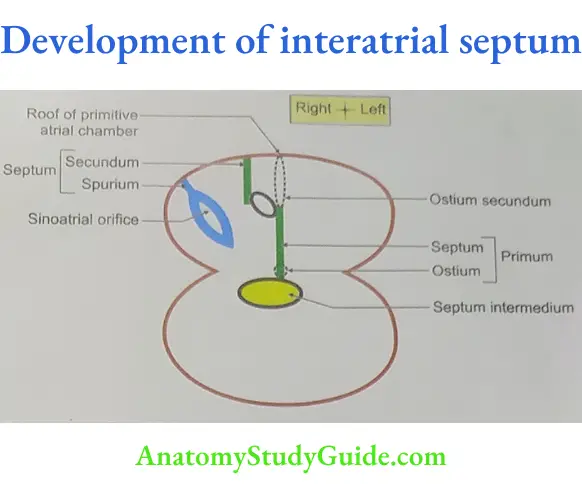
Source
- Septum primum: A thin crescent
shaped membrane grows from the roof of primitive common atrial chamber. It grows downward in the direction of septum intermedium (fused atrioventricular cushion). This septum is called septum primum. There is a gap between lower end of septum primum and septum intermedium called ostium primum. Before lower end of septum primum fuses with septum intermedium, upper part breaks open and the gap is formed which is called ostium secundum. - Septum secundum: Another crescentic membrane arises on right side of septum primum and on left side of valve of septum spurium (false). There is a noval gap between septum primum and septum secundum. It is called foramen ovale. The blood coming from right atrium passes to left atrium through foramen ovale.
- At birth, the left atrium receives blood from lungs by four pulmonary veins. Due to increase in the volume of blood, the pressure is increased in left atrium. The septum secundum and septum primum approximates and interatrial septum is developed.
Anomalies: Atrial septal defect is common anomaly.
- Incidence: 0.07%
- Gender variation: 2 to 1. Female: male ♂ infant.
- Types: It is of three types
- Cor triloculare biventricular: This is the most serious abnormality of atrial septal defect
- It is three-chambered heart with two ventricles.
- There is complete absence of the interatrial septum.
- It is always associated with serious defects elsewhere in the heart.
- Cor triloculare biventricular: This is the most serious abnormality of atrial septal defect
- Osteum primum defect is caused by
- Defective formation of atrioventricular (endocardial) cushion, or
- Failure of the septum primum to reach the atrioventricular cushion.
- Osteum secundum defect: It is a most significant defect. It is caused by
- Failure of development of septum secundum, and
Excessive resorption of septum primum.
- Failure of development of septum secundum, and
- Patent foramen ovale is caused by failure of approximation of septum primum and septum secundum after birth. It is clinically not significant as it does not allow shunting of blood.
Development of interventricular septum
1. Chronological age: It develops in the 7th week of intrauterine life (IUL).
2. Germ layer: Splanchnic layer of lateral plate mesoderm.
3. Site: From the floor of the common ventricular chamber (bulboventricular cavity).
4. Sources: It has two parts: Muscular and membranous parts
- Muscular part forms the major part of the interventricular septum. It arises as a muscular ridge or fold, the interventricular septum from the primitive ventricular chamber.
- Membranous part: It is also called interventricular foramen. It exists between the free age of interventricular septum and the fused endocardial cushion. It permits communication between right and left ventricles up to the end of 7th week. It has two parts
- Anterior membranous part develops from atrioventricular endocardial cushion. It is also called intermediate septum (septum between right atrium and left ventricle). The atrioventricular canal is formed between the primitive atrium and primitive ventricle. Initially the canal is round and changes to oval O. Two elevations develop on the anterior and posterior walls of this canal, which get fused and form septum intermedium. This communicates with right and left side of atrium to right and left side of ventricle.
- Posterior membranous part is formed by right and left bulbar septum.
5. Anomalies
- Ventricular septal defect (VSD): This is the most common congenital anomaly of the heart. It is because of failure of fusion of endocardial cushion or the atrioventricular canal.
- Pentalogy of Fallot
- Pulmonary stenosis
- Right ventricular hypertrophy
- Overriding of the aorta
- Ventricular septal defect
- Atrial septal defect
- Fallot’s tetralogy (tetralogy means four defects): It is most common congenital cyanotic heart disease. The main defect is an unequal division of the conus leading to narrow pulmonary and wide ascending aorta. It is characterized by
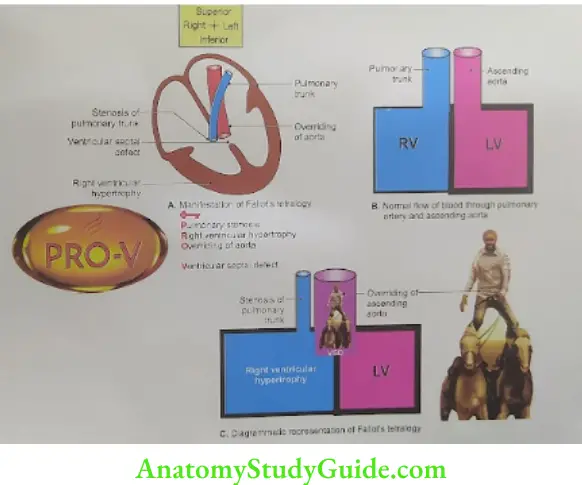
Pulmonary stenosis,
Right ventricular hypertrophy,
Overriding of the aorta, and
Ventricular septal defect.
The clinical manifestations are breathlessness on exertion. The child suddenly ceases his activity and lies in the knee chest position “squatting posture”, by doing so he gets relief probably because squatting reduces the venous return by compressing the abdominal veins and increases the systemic vascular resistance by kinking the femoral and popliteal arteries. Both these mechanisms tend to decrease the right to left shunt through ventricular septal defect and improve the pulmonary circulation.
Development of left atrium
1. Chronological age: It develops in the 5th to 7th week of intrauterine life (IUL).
2. Germ layer: Mesoderm.
B. Site: Primitive atrial chamber.
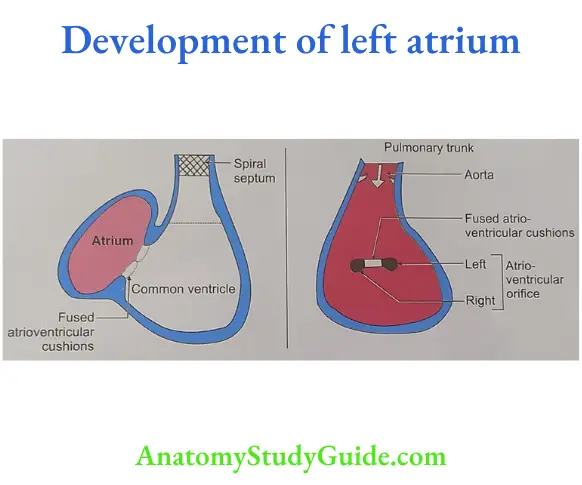
Sources
- The posterior smooth part (between the openings of the pulmonary veins) develops from the incorporation of the endocardial cushions of the four pulmonary veins.
- The anterior part (which is somewhat trabeculated including the left auricle) develops from the left half of the primitive atrium.
- The most ventral part develops from the left half of the atrioventricular canal.
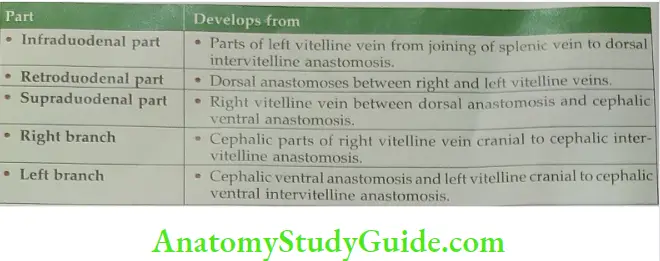
Development of portal vein
Chronological age: It develops in the 5th to 7th week of intrauterine life (IUL).
Germ layer: Mesoderm.
Site: Around the duodenum.
4. Sources
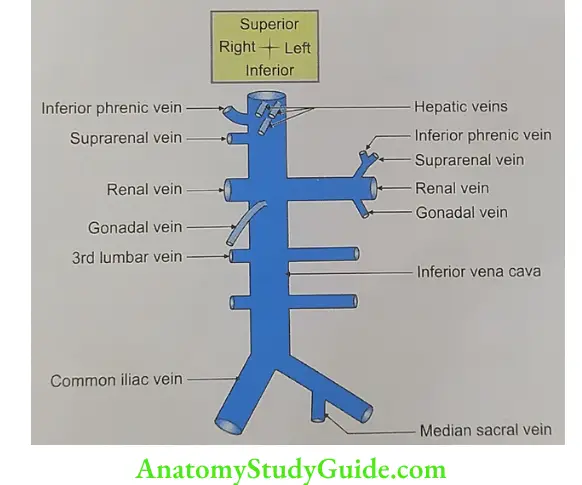
OLA-15 Tributaries of inferior vena cava
Tributaries: The tributaries of vena cava are not identical with the branches of the abdominal aorta. Especially, there are no corresponding veins to the three ventral branches to the gut. Following are the tributaries of the inferior vena cava.
1. Pair of common iliac veins.
2. Lumbar veins.
- 3rd and 4th pair of lumbar veins drain directly into the inferior vena cava.
- 1st and 2nd drain into ascending lumbar vein.
- A pair of renal veins,
- A pair of phrenic veins,
- Right gonadal vein, and
- Right suprarenal vein and hepatic veins.
Development of inferior vena cava
1. Chronological age: It develops in the 5th to 7th weeks of intrauterine life (IUL).
2. Germ layer: Splanchnic layer of lateral plate mesoderm.
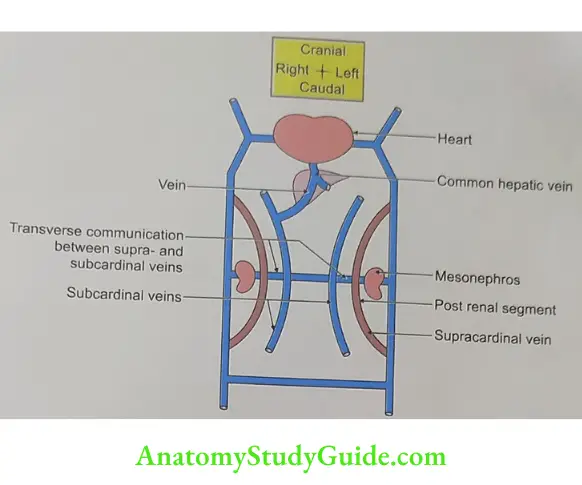
Site: Posterior abdominal wall.
Sources
- Right posterior cardinal vein caudal to joining of right supracardinal vein,
- Right supracardinal vein caudal to right supra-/subcardinal anastomosis,
- Right supracardinal-subcardinal anastomoses, anastomoses,
- Right subcardinal vein caudal to right subcardinohepatocardiac channel
- Right subcardinal hepatic cardiac channel anastomoses, and Hepatocardiac channel.
Anomalies
- Absence of inferior vena cava-results when the right subcardinal vein fails to establish connection with the liver.
- Double inferior vena cava (at lumbar level)-results from persistence of left supracardinal vein.
Leave a Reply