Perineum Structures Perineal Membrane In Male Female General Histology
Perineum
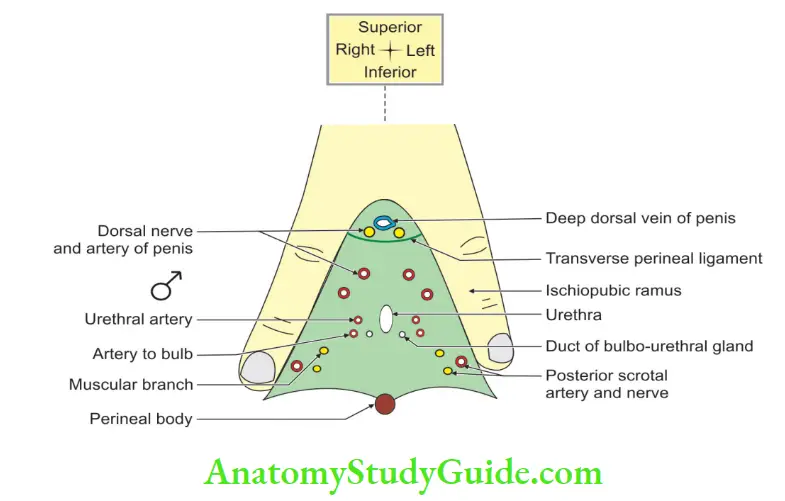
Question – 1: Enumerate the structures piercing the perineal membrane in male ♂
Table of Contents
Answer:
1. Urethra: Urethra in the midline.
2. Ducts: Ducts of the bulbourethral gland.
3. Arteries:
- Artery to the bulb
- Urethral artery, a branch of artery of penis
- Deep artery of the penis (a branch of perineal artery), and
- Dorsal artery of penis.
- Posterior scrotal artery, a branch of perineal artery (a branch of internal pudendal artery).
Read And Learn More: General Histology Question And Answers
4. Nerves:
- Nerve to the bulb, a branch of nerve to bulbospongiosus (a branch of perineal nerve).
- The posterior scrotal nerve.
- Branches of perineal nerve to the superficial perineal muscle.
Perineal Body (central perineal tendon)
Perineal Body Introduction: It is a pyramidal fibromuscular mass situated in the midline of perineum.
1. Perineal Body Location:
Male ♂: It is located close to the bulb of penis.
Female ♀: It is present between anal canal and pudendal cleft.
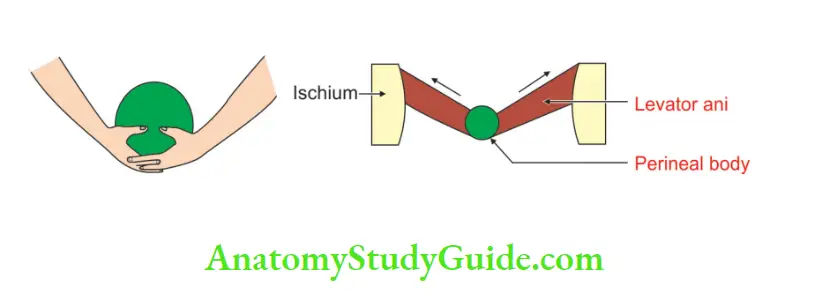
2. Perineal Body Formation:
It is formed by 10 muscles—4 paired and 2 unpaired.
1. Paired (BSNL):
- Bulbospongiosus (B).
- Superficial transverse perinei (S).
- Deep transverse perinei (N).
- Levator ani (L).
2. Unpaired:
1. Perineal body is also called “obstetrical perineum”
2. It is a musculofascial structure.
3. Fascia
- Two layers of superficial perineal fascia:
- Superficial fatty layer
- Deep membranous layer
- Two layers of urogenital diaphragm:
- The superior layer of the urogenital diaphragm
- The inferior layer of the urogenital diaphragm
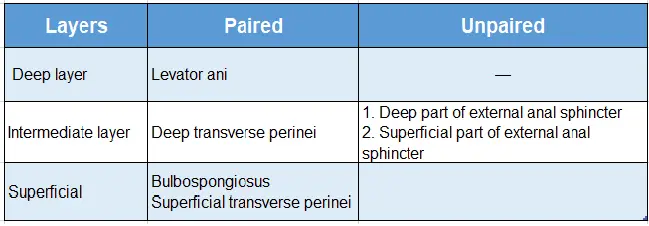
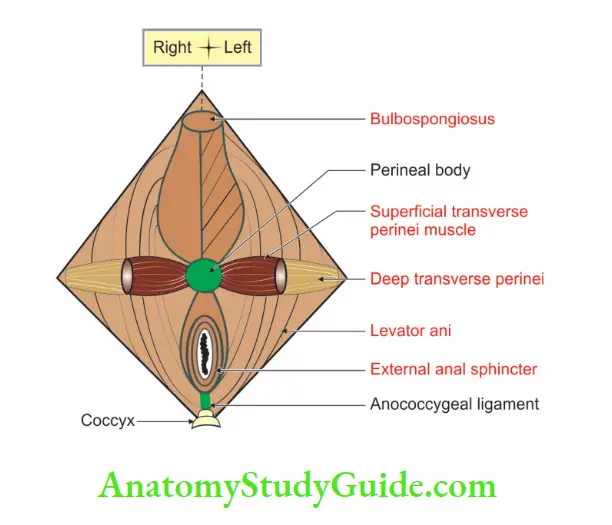
4. Muscles: They are arranged in three layers.
- Deep layer: Paired levator ani
- Intermediate layer
3. Perineal Body Development
It develops from the tip of the urorectal septum.
4. Perineal Body Applied anatomy:
1. In female ♀ it acts as a very important support for the pelvic organs.
2. Injury to the perineal body may weaken the pelvic floor and leads to prolapse of the vagina and uterus.
3. Episiotomy (incision of vulva) is given to facilitate the labour. It prevents the rupture of the perineal body.
4. The torn perineal body during parturition, if not properly repaired, leads to wider hiatus urogenitalis.
Question – 2: Attachments and nerve supply of external anal sphincter
Answer:
1. External anal sphincter: Is divided into three parts.
- Subcutaneous part: It is situated deep to the skin and is separated by perianal fascia.
- Intermediate or superficial part: It extends from perineal body to the tip of the coccyx.
- Deep part: It encircles the upper part of the anal canal.
2. Nervese supply: It is supplied by pudendal nerve (Somatic nerve).
External Anal Sphincter
1. External Anal Sphincter Formation:
It is formed by the skeletal muscles.
- Control: It is under voluntary control.
- Extent: It surrounds the whole anal canal.
- Function: It keeps the anus and anal canal closed.
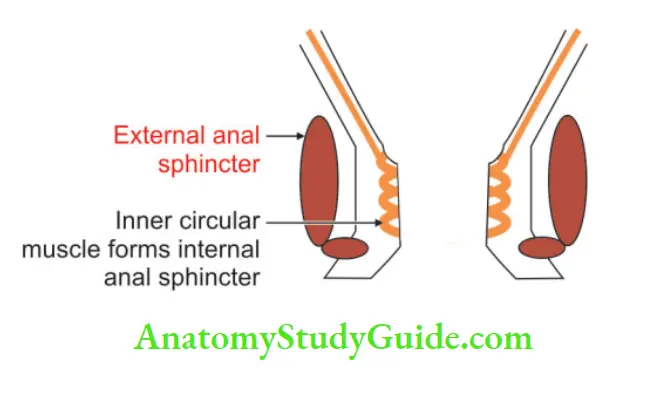
2. External Anal Sphincter History:
Old view: It has three anatomical (structural) and physiological (functional) components
- Subcutaneous
- Intermediate, and
- Deep.
Recent view: It is a single anatomical and physiological unit
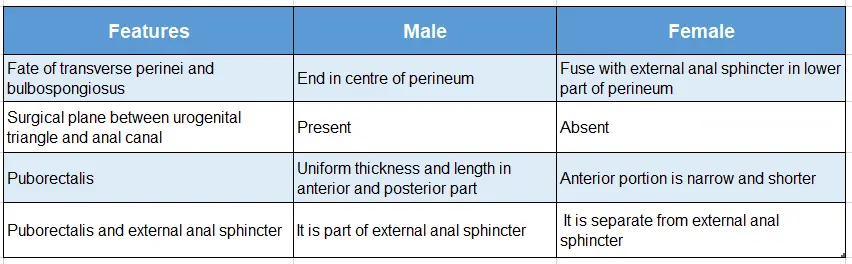
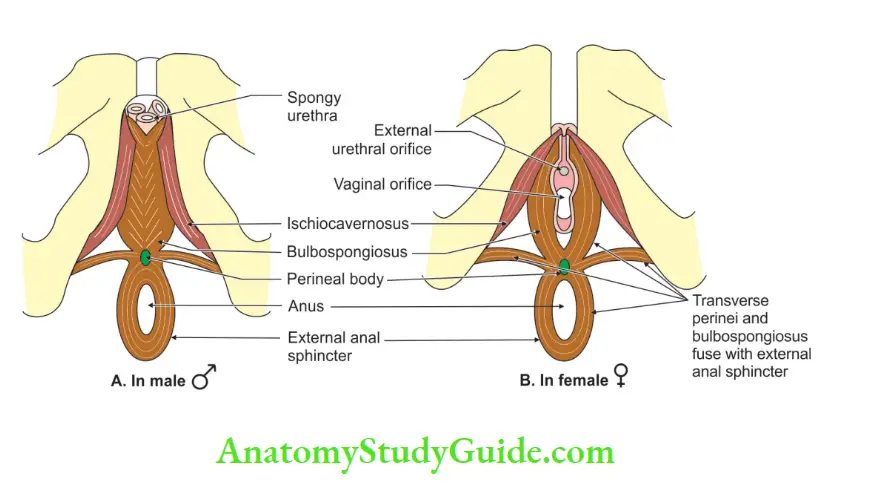
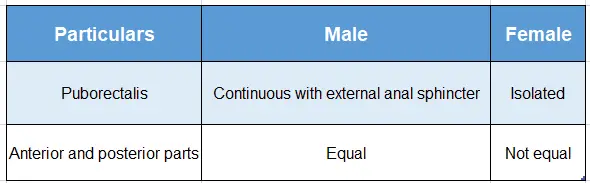
3. External Anal SphincterGender variations:
Features of the external anal sphincter of male and female:
Cat of nine tails:
The perineal body is formed by 9 muscles
1. Four paired:
- Bulbospongiosus
- Superficial transverse perineal
- Levator ani
- Deep transverse perinei
2. Unpaired—1
External anal sphincter
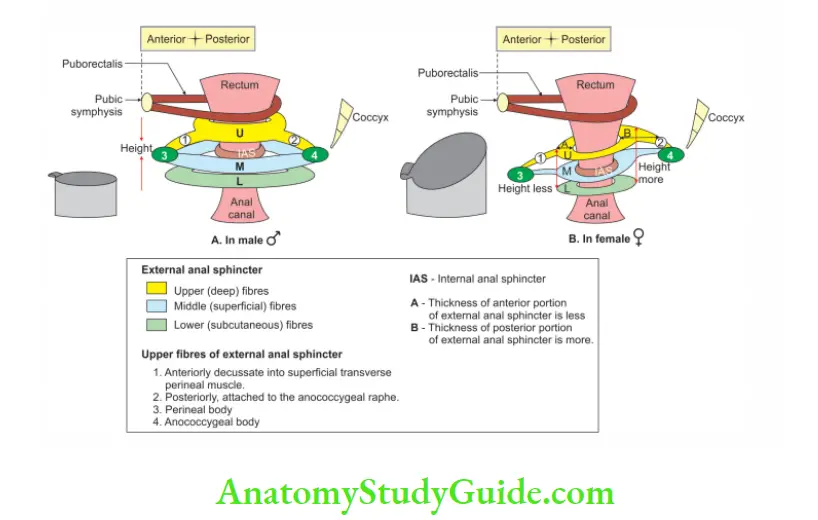
External anal sphincter in males and females:
4. Parts
It is divided into three parts
Subcutaneous part:
- It is below the level of the internal anal sphincter.
- It is separated from anal epithelium by submucosa.
- It is formed by flat bands.
- It is 15 mm in breadth.
- It surrounds the lower part of the anal canal.
- It is situated deep into the skin and is separated by perianal fascia.
Intermediate or superficial part:
- It extends from the perineal body to the tip of the coccyx.
- It is separated from the subcutaneous part by perianal fascia.
- It is separated from the internal anal sphincter by conjoint fibres of the levator ani and longitudinal muscle of the rectum and anal canal.
Deep part: It encircles the upper part of the anal canal.
5. Nerve supply: It is supplied by the pudendal nerve (somatic nerve.
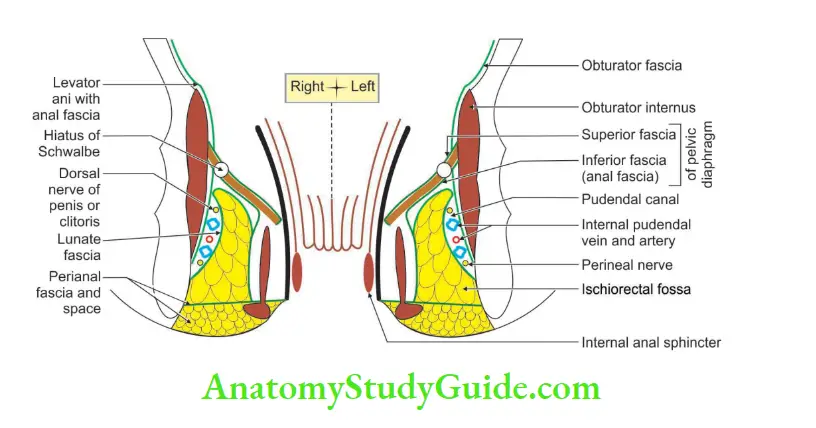
Boundaries Of Ischiorectal Fossa
Boundaries
1. Apex: It is formed by the junction of the obturator and anal fascia (inferior fascia of the pelvic diaphragm).
2. Base: It is formed by the skin.
3. Anterior: Posterior border of the perineal membrane.
4. Posterior:
- Lower border of the gluteus maximus.
- Sacrotuberous ligament.
5. Lateral wall:
- Obturator internus.
- Obturator fascia.
- Medial surface of ischial tuberosity.
6. Medial wall:
- In the lower part: External anal sphincter.
- In the upper part: Levator ani.
Contents Of Ischiorectal Fossa
1. Pudendal canal with its content.
- Pudendal nerve (ventral division of ventral ramus of S2, S3 and S4).
- Internal pudendal vessels (anterior division of internal iliac artery).
2. Posterior scrotal nerve and vessels.
3. Perforating cutaneous branch of S2, and S3.
4. Inferior rectal nerve and vessels (S2, S3, S4).
5. Pad of fat.
6. Perineal branch of S4 nerve. It supplies the anterior part of the external anal sphincter.
Question – 3: Describe the ischiorectal fossa under the following heads
1. Gross anatomy
2. Boundaries
3. Contents
4. Recesses
5. Spaces
6. Canals, and
7. Applied anatomy.
Answer:
Ischiorectal Fossa Introduction:
It is also called ischioanal fossa. It is the wedge  shaped space present in the lateral part of anal
shaped space present in the lateral part of anal 
1. Gross Anatomy:
- Location: It is present 1 on either side of the anal canal and below the pelvic diaphragm.
- Dimension: Length x width x depth 2″ x 1″ x 2″
2. Boundaries:
Apex: It is formed by the junction of the obturator and anal fascia (inferior fascia of the pelvic diaphragm).
Base: It is formed by the skin.
Anterior: Posterior border of the perineal membrane.
Posterior:
- Lower border of the gluteus maximus
- Sacrotuberous ligament.
Lateral wall:
- Obturator internus.
- Obturator fascia.
- Medial surface of ischial tuberosity.
Medial wall:
- In the lower part: External anal sphincter
- In the upper part: Levator ani.
3. Contents:
1. Pudendal canal with its content
- Pudendal nerve (ventral division of ventral rami of S2, S3 and S4).
- Internal pudendal vessels (anterior division of internal iliac artery).
2. Posterior scrotal nerve and vessels:
3. Perforating cutaneous branch of S2, S3.
4. Inferior rectal nerve and vessels.
5 . Pad of fat.
6. Perineal branch of S4 nerve. It supplies the anterior part of the external anal sphincter.
4. Recesses:
These are narrow extensions of ischiorectal fossae.
1. Anterior recess: It extends from the urogenital diaphragm. It reaches up to the posterior surface of the body of the pubis.
2. Posterior recess: It is smaller than the anterior. It is present deep in the sacrotuberous ligament.
3. Horseshoe recess: It connects two ischiorectal fossae behind the anal canal.
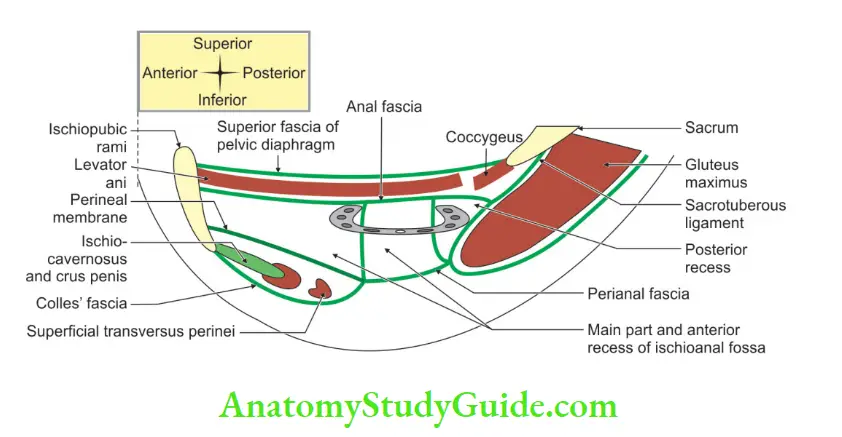
5. Spaces:
- Perianal space:
- Perianal fascia is a septum which separates the perianal space from the ischiorectal space.
- It extends from the white line of Hilton medially to the pudendal canal laterally.
- The fat is arranged tightly in the small loculi.
- The infections in this space are, therefore, very painful. It is due to the tension caused by swelling.
- Ischiorectal space:
- .It is deep into the perianal space.
- The fat is arranged loosely due to incomplete septa.
- The infections in this space are less painful since there is no tension in the swelling.
- Lunate fascia arches over ischiorectal fat and divides it into
-
- Suprategmental space.
- Tegmental space
6. Canals (fascial canal, Alcock’s canal):
It is the connective tissue sheath in the lower lateral wall of the ischiorectal fossa.
7. Applied anatomy:
1. It allows distension of the anal canal during the passage of faeces.
2. It also allows dilatation of the vagina during parturition.
3. The loss of fat results in prolapse of the rectum.
4. The perineal and ischiorectal spaces are common sites for abscesses.
5. Through the horseshoe recess, a unilateral abscess may become bilateral.
6. Presence of hiatus of Schwalbe: It is a gap at the apex of the fossa.
7. It is due to the defective origin of the levator ani from the obturator fascia.
8. It is occasionally present.
9. Very rarely pelvic organs may herniate through it into the ischiorectal fossa.
10. Psoas abscess may enter the iliac fossa.
11. It may travel the ischiorectal fossa along the pudendal vessels.
12. An abscess in the ischiorectal space may burst in the anal canal and produces a fistula in ano.
Pudendal Canal (fascial canal, Alcock’s canal)
Introduction: It is the connective tissue sheath in the lower lateral wall of the ischiorectal fossa.
1. Pudendal Canal Location:
- 2.5 cm above the ischial tuberosity.
2. Pudendal Canal Formation:
- Laterally: Obturator fascia
- Above: Lunate fascia
- Below: Falciform process of the sacrotuberous ligament
- Medially: Perianal fascia
- Extent: From lesser sciatic foramen to deep perineal pouch.
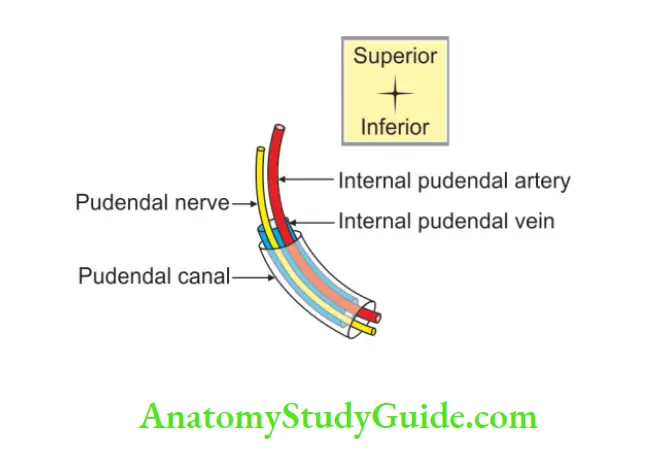
3. Pudendal Canal Contents:
1. Pudendal nerve (S2-S4 ventral division of ventral rami), and
2. Internal pudendal vessels.
3. The arrangement of the structures within the canal is as follows from above downwards.
- Dorsal nerve of penis or clitoris.
- Internal pudendal vein.
- Internal pudendal artery.
- Perineal nerve.
4. Pudendal Canal Applied Anatomy:
1. The pudendal nerve is blocked to anaesthetise the perineum. This is called pudendal block. It is given by the following methods.
2. Transvaginal procedure: A long needle is passed, through the vaginal wall and guided by a finger to the ischial spine. It can be palpated per vaginal.
3. Perineal procedure: The ischial tuberosity is palpated subcutaneously through the buttock.
4. The needle is inserted into the pudendal canal along the medial side of the tuberosity.
5. The canal lies about 1″ (2.5 cm) deep to ischial tuberosity.
Question 4: Describe the internal pudendal artery under
l. Origin
2. Termination
3. Gender variation
4. Extent
5. Course
6. Relations
7. Branches and distribution, and
8. Applied anatomy.
Answer:
1. Origin: It is one of the smaller terminal branches of the anterior division of the internal iliac artery. It arises in the pelvis just below the origin of the obturator artery.
2. Termination: It continues as the artery of the penis/clitoris distal to the perineal branch of the internal pudendal artery.
3. Gender variation: It is larger in males ♂ than in females ♀
4. Gender Extent: It extends from the origin to the initial part of the deep perineal pouch.
5. Course:
It is divided in three parts by sacrospinous ligament
- The first part is proximal to the sacrospinous ligament. It is also called the pelvic part.
- The second part is deep to the sacrospinous ligament. It is present in the gluteal region.
- The third part is distal to the sacrospinous ligament. It is also called part of an internal pudendal artery in the pudendal canal.
6. Relations:
1. The first part (intrapelvic part):
1. The artery runs downwards in the pelvis.
2. It runs in front of the
- Piriformis
- Sacral plexus, and
- Inferior gluteal artery.
3. It leaves the pelvis by piercing the parietal pelvic fascia.
4. It passes through the greater sciatic foramen, below the piriformis.
5. It thus enters the gluteal region.
2. The second part (part present in the gluteal region):
1. The artery crosses the tip of the ischial spine.
2. It is under cover of the gluteus maximus.
3. Here it lies between the
- Pudendal nerve medially, and
- Nerve to the obturator internus laterally.
4. It leaves the gluteal region by passing through the lesser sciatic foramen.
5. It enters the pudendal canal.
3. The third part (part of an internal pudendal artery in the pudendal canal):
1. The artery runs downwards and forwards in the lateral wall of the ischioanal fossa.
2. It is about 4 cm above the lower margin of the ischial tuberosity.
3. It is related to the
- Dorsal nerve above, and
- Perineal nerve below.
4. In deep perineal space, it is called artery of the penis/clitoris:
The artery of the penis or clitoris is a continuation of the internal pudendal artery.
- It runs forwards close to the side of the pubic arch.
- It lies medial to the dorsal nerve of the penis or of the clitoris.
- The artery ends a little behind the arcuate pubic ligament.
- It divides into the deep and dorsal arteries of the penis and clitoris.
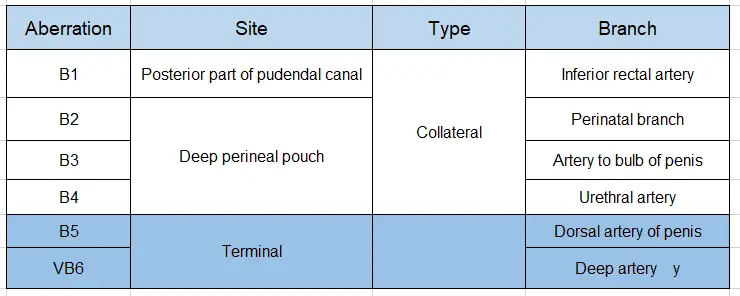
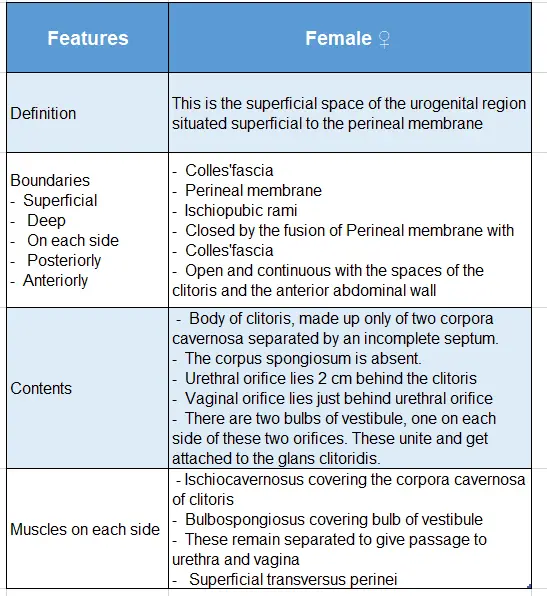
7. Branches and distribution:
Branches are grouped for the purpose of convenience. They are branches given in relation to
- Pudendal canal
- Deep perineal pouch, and
- Terminal branches.
To be precise, the branches arising in the pudendal canal are branches of the internal pudendal artery. The arteries arising distal to the pudendal canal are branches of the artery of the penis/clitoris.
MCQ:
Note: Please note that, all the branches of the internal pudendal artery except the inferior rectal artery pierce the perineal membrane.
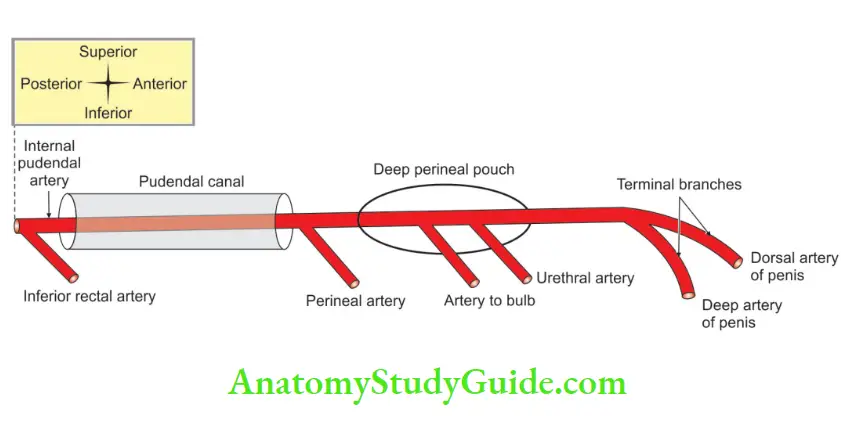
1. Pudendal canal:
Branches are given at two ends of the pudendal canal. They are
- The inferior rectal artery at the posterior end.
- The perineal artery is at the anterior end of the pudendal canal.
1. Inferior rectal artery: Accompanies the nerve of the same name. It supplies the
- Perianal skin
- Sphincters of the anus, and the
- The anal canal below the pectinate line. Here it anastomoses with the branches of the superior rectal artery.
2. Perineal branch: Pierces the urogenital diaphragm.
- Distribution: It supplies the
- Bulbospongiosus and
- Ischiocavernous muscles.
- Course: It runs forwards into the superficial perineal space, superficial to the perineal membrane. It divides into
- Posterior scrotal or labial branches, and
- Transverse perineal branch.
-
- Posterior scrotal artery: Posterior scrotal artery or labial branch supplies tissues between the anus and the bulb.
- Transverse perineal branch: The transverse perineal branch runs medially along the superficial transverse perineal muscle.
2. Deep perineal pouch:
Branches given from the internal pudendal artery in the deep perineal pouch are branches of arteries of the penis/clitoris.
- The artery to the bulb of the penis, and
- Urethral artery.
Artery: The artery of the bulb passes medially through the deep transverse perineal muscle. It reaches the bulb of the penis after piercing the perineal membrane. It supplies the
- The posterior part of the corpus spongiosum
- Bulbourethral gland, and
- Proximal half of the corpus spongiosum.
Urethral artery: The urethral artery arises just below the perineal membrane. It passes through the fascia of the urogenital diaphragm. It enters the corpus spongiosum and reaches the glans penis. It is distributed to the urethra and the erectile tissue around it.
3. Terminal branches:
Terminal branches are two
- Deep arteries of the penis, and
- Dorsal arteries of the penis.
1. Deep arteries: Deep arteries are also called cavernosal arteries.
1. Features:
- They are larger of the two terminal branches of the internal pudendal/ artery of the penis/ clitoris.
- They are given behind the pubic angle.
- They pierce the perineal membrane.
2. They are the principal arteries for filling the lacunae of erectile tissue during the erection of the penis.
3. Each deep artery of the penis runs lengthwise in the corpus cavernous and gives off numerous branches.
4. These arteries give rise to minute arteries that directly open into the cavernous spaces.
5. In the flaccid state of the penis, these vessels project in the lacunae as looped or spiral vessels and are hence termed “helicine arteries.”
2. Dorsal artery of the penis or of the clitoris
1. Features:
- It is the smaller of the two terminal branches of the internal
pudendal/ artery of penis/ clitoris. - It is given behind the pubic angle.
- It traverses the sphincter urethrae and then pierces the perineal membrane.
2. It passes upward between the crura of the penis or clitoris.
3. It runs on the dorsal surface of the penis or the clitoris beneath the deep fascia of the penis called Buck’s fascia. The dorsal artery runs on the dorsal aspect of the penis.
4. It runs lateral to the deep dorsal vein and medial to the dorsal nerve of the penis.
5. It supplies circumflex branches to the corpora cavernosa and corpus spongiosum.
6. Therefore, corpora cavernosa receives blood both from the deep and the dorsal arteries of the penis.
7. The circumflex branches end by anastomosing in the coronal sulcus.
8. They supply the glans penis and its overlying skin.
Names changed after particular events and landmarks:
Note: The artery of the penis is the continuation of the pudendal artery distal to the perineal branch. The pudendal artery is called artery of the penis in deep perineal space.
8. Applied Anatomy:
1. During dissections of the anal canal, the inferior rectal vessels are encountered in the ischioanal fossa.
2. They must be secured before division.
3. They tend to retract laterally to the canal, where they can cause troublesome bleeding.
4. The common cause of painful swelling in the perineum is the perineal abscess.
5. It is due to the infection carried by a small branch of internal pudendal artery.
6. There may be infection during episiotomy.
7. This may interrupt the blood flowing through the internal pudendal artery.
8. This results in painful perineal swelling.
“Know the vessels n nerve ur ashamed off”:
Introduction: The internal pudendal artery: The word pudendal means ashamed off.
It supplies all the structures that we are ashamed off. It is also the chief artery of urogenital ![]() .
.
The structures supplied by internal pudendal artery include major portion of the skin and all of the deeper structures, including the erectile tissue of the penis/clitoris.
However, the testis, epididymis, and the scrotal layers surrounding these have their own blood supply.
A tale of internal pudendal artery:
- The simile of internal pudendal artery A house has 3 rooms.
- They are room R1, R2 and R3.
- The R1 has 2 windows W1 and W2.
- There is a water tank near the roof and a canal.
- The canal is fixed to the lower part of outer wall of R1.
- The water tube is called A.
- The area outside the house near the window represents gluteal region.
- The water passes from the roof of R1 to R3.
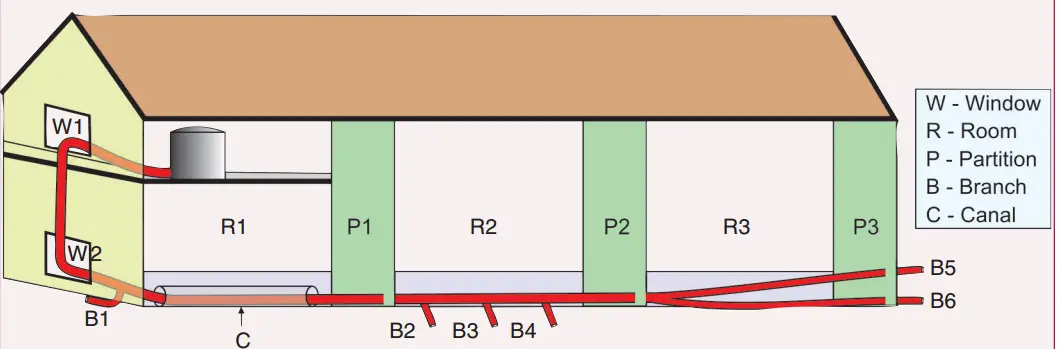
The simile of internal pudendal artery:
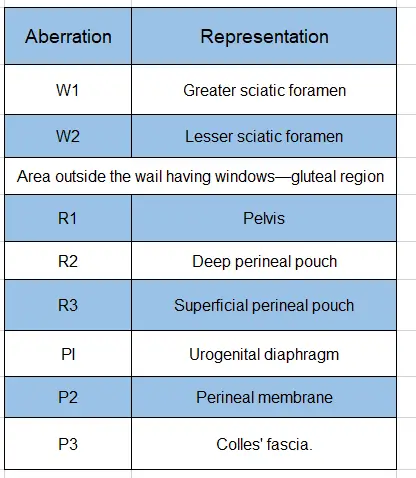
Branches of internal pudendal artery:
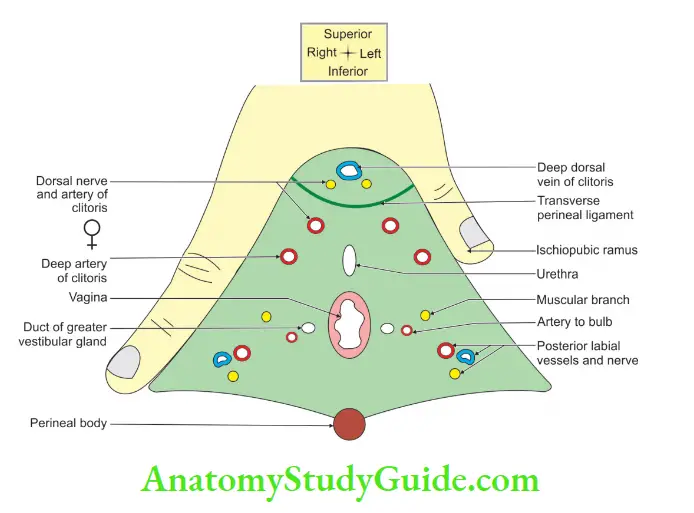
Structures Piercing Perineal Membrane In Female
Following are the structures piercing the perineal membrane in female ♀
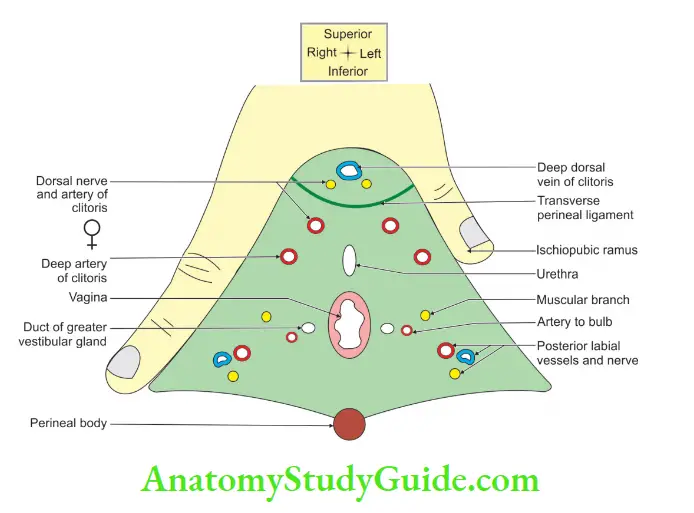
1. Urethra
2. Vagina
3. Arterie
- Artery to the bulb of the vestibule
- Deep artery of clitoris
- Dorsal artery of clitoris and
- Posterior labial arteries.
4. Nerves
- Nerve to bulb of vestibule
- Posterior labial nerve, and
- Muscular branches of perineal nerve supplying superficial perineal muscles.
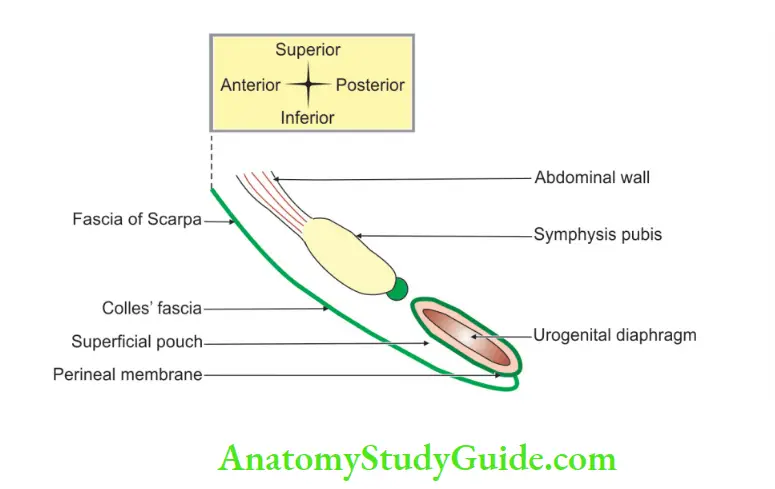
Perineal Membrane
It is an unyielding sheath of fibrous tissue which separates the superficial and deep perineal pouch.
It forms the inferior boundary of deep perineal pouch and superior boundary of superficial perineal pouch.
Urogenital Diaphragm
Introduction: It is a musculofascial partition across the pubic arch and separates the pelvic cavity from the anterior part of the pelvic outlet.
1. Formation
- Sphincter urethrae: It encircles the membranous urethra and consists of superficial and deep fibres.
- Deep transversus perinei
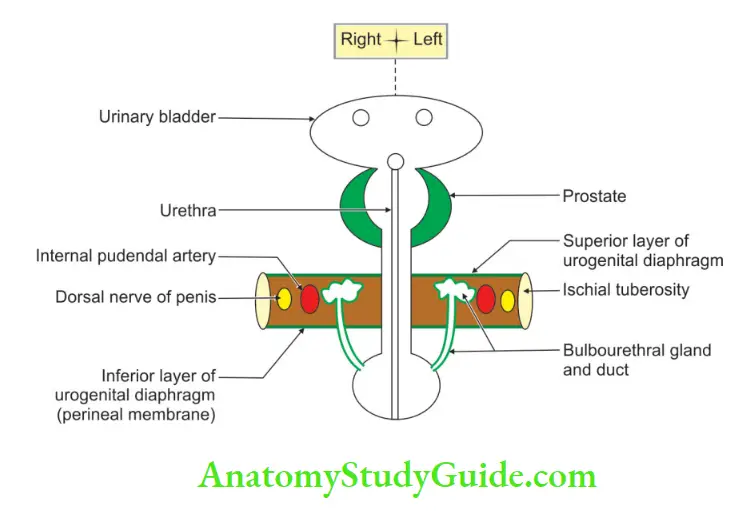
2. Nerve supply
Both muscles are supplied by muscular branches of the perineal nerve, branch of pudendal nerve.
3. Structure piercing in
- Male ♂: Urethra.
- Female ♀: Vagina and urethra.
4. Relations
Below: Contents of superficial perineal pouch.
Above:
- Apex of prostate (in male ♂ ) or neck of the urinary bladder (in female ♀ ).
- Anterior fibres of both levator ani muscles.
- Anterior recesses of ischiorectal fossae.
In front:
A ![]() lar gap between the arcuate pubic ligament and the transverse perineal ligament. It transmits the deep dorsal vein of the penis or clitoris.
lar gap between the arcuate pubic ligament and the transverse perineal ligament. It transmits the deep dorsal vein of the penis or clitoris.
Behind: Ischiorectal fossae and their contents.
5. Actions
It supports the prostate or the bladder.
In females ♀, it constricts the vagina.
It fixes the perineal body.
The sphincter urethrae exerts voluntary control of micturition and expels the last drops of semen and urine.
6. Rupture of the urethra
The rupture of the urethra is common beneath the pubis by a fall on a sharp object.
This causes extravasation of the urine:
1. Rupture of the urethra, superficial to the perineal membrane results in extravasation of the urine in the superficial perineal pouch.
2. It accumulates in the scrotum> penis>anterior abdominal wall, >deep to the fascia of the Scarpa and extends up to the axilla.
3. Rupture of the urethra, deep to the perineal membrane produces extravasation of the urine in the extraperitoneal space of the pelvis.
4. It accumulates in the anterior abdominal wall.
Perineal Membrane (inferior fascia of the urogenital diaphragm)
Introduction: It is an unyielding sheath of fibrous tissue. It separates superficial and deep perineal pouches.
It forms the inferior boundary of the deep perineal pouch and the superior boundary of the superficial perineal pouch.
1. Gross
1. Dimensions: Anteroposterior dimension 3.5 cm.
2. Disposition: Horizontal in erect posture.
3. Attachments:
- Anteriorly and on either side: Ischiopubic rami.
- Posteriorly and on either side: Anterior part of the ischial tuberosity.
- Anterior border forms the transverse perineal ligament.
- The posterior border fuses to the perineal body and superiorly to a superior layer of the urogenital diaphragm.
- It fuses interiorly with Colles’ fascia.
2. Structuring piercing
In male ♂:
1. Urethra in the midline
2. Ducts of the bulbourethral gland
3. Arteries
- Artery to the bulb
- Posterior scrotal artery, is a branch of the perineal artery (a branch of an internal pudendal artery).
- Urethral artery, a branch of the artery of the penis
- Deep artery of the penis and (a branch of a perineal artery).
- Dorsal artery of penis.
4. Nerves
- Nerve to the bulb, a branch of nerve to bulbospongiosus (a branch of perineal nerve).
- Posterior scrotal nerve.
- Branches of perineal nerve to the superficial perineal muscle.
Note:
1. The shape and size of the perineal membrane in males are represented by the space present between the index and middle fingers.
2. The shape and size of the perineal membrane in females are represented by the space present between the index finger and thumb.
Openings in the perineal membrane in males are shown by the index and middle fingers of the right hand. The index and middle fingers represent ischiopubic rami of the left and right side, respectively
In female ♀:
1. Urethra
2. Vagina
3. Arteries
- Artery to the bulb of the vestibule
- Deep artery of clitoris
- Dorsal artery of the clitoris, and
- Posterior labial arteries.
4. Nerves
- Nerve to the bulb of vestibule
- Posterior labial nerve, and
- Muscular branches of the perineal nerve supply superficial perineal muscles.
3. Applied anatomy
The urethra passing through the perineal membrane is called the membranous urethra. It is the shortest and least dilatable part of the urethra and does not contain any glands.
Openings in the perineal membrane in females are shown by the thumb and index finger of the right hand. The thumb and index finger represent ischiopubic rami of the left and right sides, respectively.
Question 4: Describe the superficial perineal pouch under the following heads
1. Boundaries
2. Contents, and
3. Applied anatomy.
Answer:
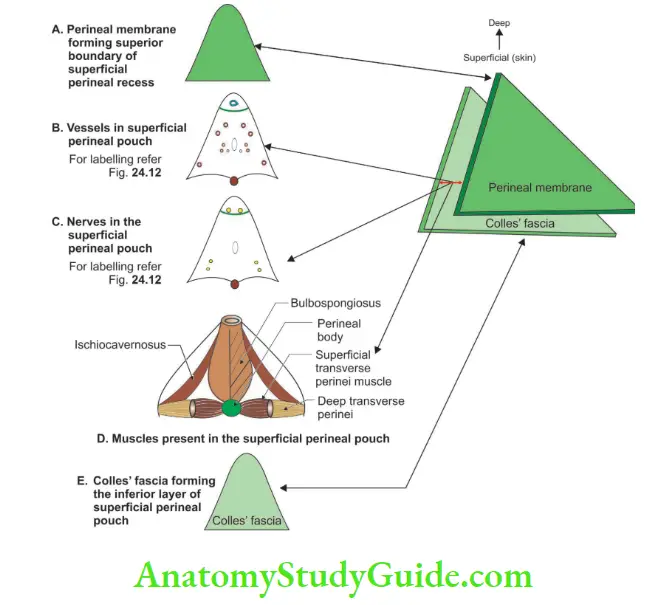
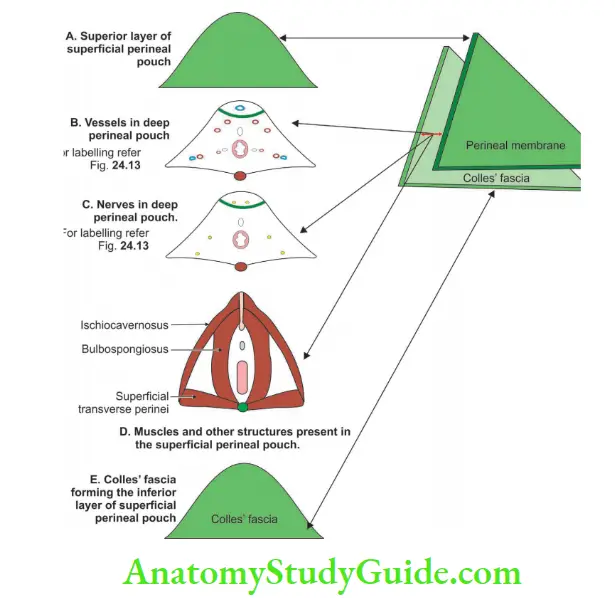
Superficial Perineal Introduction
It is the space between the Colles’ fascia and the perineal membrane (inferior layer of the urogenital diaphragm).
1. Boundaries:
There are two ways of describing the boundaries of the perineal pouch. In anatomical position, the terms superior or roof and inferior or floor are used. While dissecting, the terms superficial and deep are used.
- Superficially or floor by Colles’ fascia.
- Deep or roof by the perineal membrane.
- On each side by the ischiopubic rami.
- Posteriorly, the space is closed by the fusion of the perineal membrane with the Colles’ fascia.
- Anteriorly, it is opened. It is continuous with the spaces of the scrotum, the penis and the anterior abdominal wall.
2. Contents:
The superficial perineal pouch male ♂:
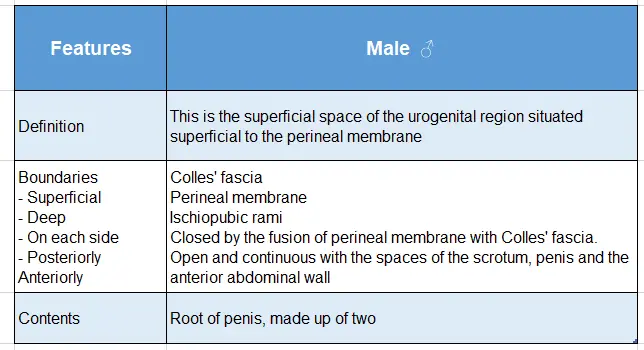
The superficial perineal pouch male ♂ (Contd) :
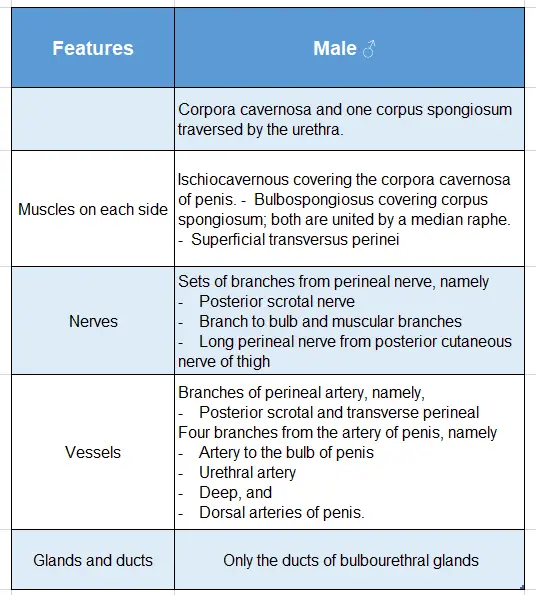
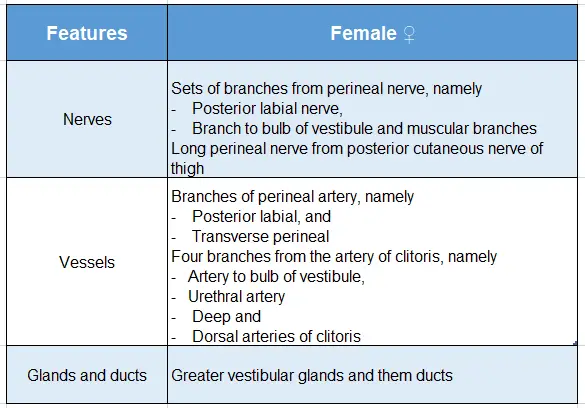
The superficial perineal pouch female ♀:
The superficial perineal pouch female ♀ (Contd):
3. Applied Anatomy
1. Injury to the bulb of the penis causes rupture of the superficial perineal pouch. It results from
- Straddle injury (forceful blow to the perineum when sitting, standing or walking with legs apart.)
- Creating false passage while passing the transurethral catheter.
- Rupture of blood vessels in superficial perineal pouch.
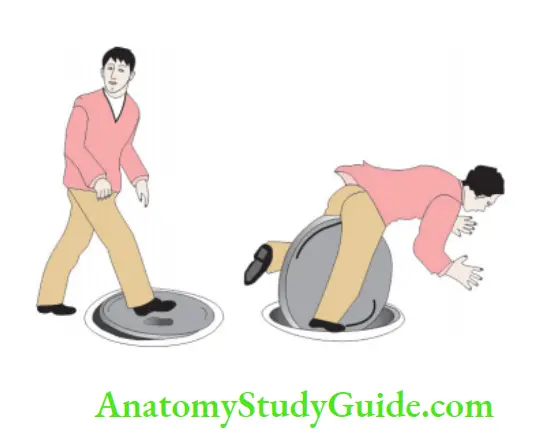
The rupture of the spongy urethra results in the extravasation of urine into the superficial perineal pouch. This results from straddle injury, such as falling on a metal beam
2. There is extravasation of urine in the rupture of the superficial perineal pouch.
3. The direction of extravasated urine is decided by the attachment of the perineal fascia.
4. The direction of accumulation of urine is as follows
- Loose connective tissue in scrotum >
- Around penis >
- Anterior abdominal wall deep to the membranous layer and superficial to rectus sheath >
- May extend to the axilla.
5. The urine cannot pass
- Into thighs because the membranous layer blends with fascia lata.
- Anal because superficial and deep layers of perineal fascia are continuous with each other.
Question 5: Describe the deep perineal pouch under the following heads
1. Boundaries
2. Contents, and
3. Applied anatomy.
Answer:
Deep Perineal Introduction:
It is the space between the superior and inferior fascia of the urogenital diaphragm.
1. Boundaries:
- The inferior or superficial layer is by the perineal membrane (inferior layer of the urogenital diaphragm).
- Superior or deep by the superior layer of the urogenital diaphragm.
- On each side by the ischiopubic rami.
- Posteriorly, the space is closed by the union of the perineal membrane.
- With the superior fascia of the urogenital diaphragm (fusion of superior and inferior layer of the urogenital diaphragm).
- Anteriorly, it is closed by the union of the perineal membrane with the superior fascia of the urogenital diaphragm.
- At the transverse perineal ligament.
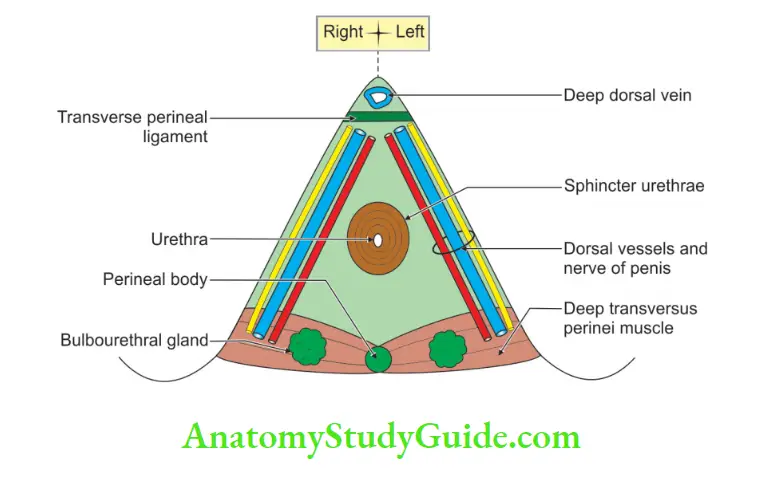
2. Contents:
1. In male ♂:
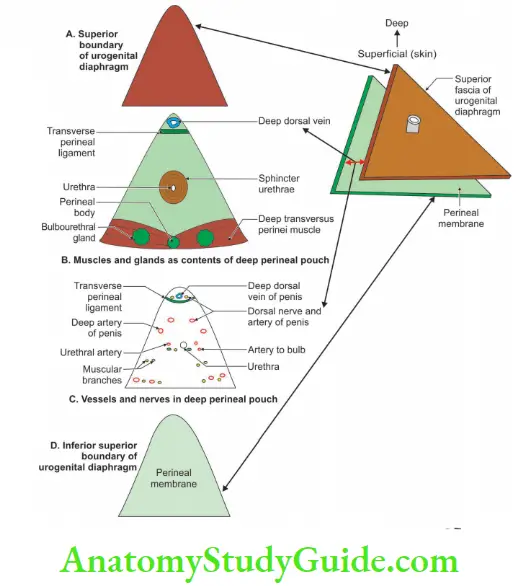
Structures:
- The membranous urethra, and.
- Bulbourethral gland.
Muscles:
- Sphincter urethrae.
- Deep transverse perinei.
Nerves:
- Dorsal nerve of the penis (pudendal nerve)
- Muscular branches from the perineal nerve.
Vessels: Artery of the penis, a branch of the internal pudendal artery.
2. In female ♀:
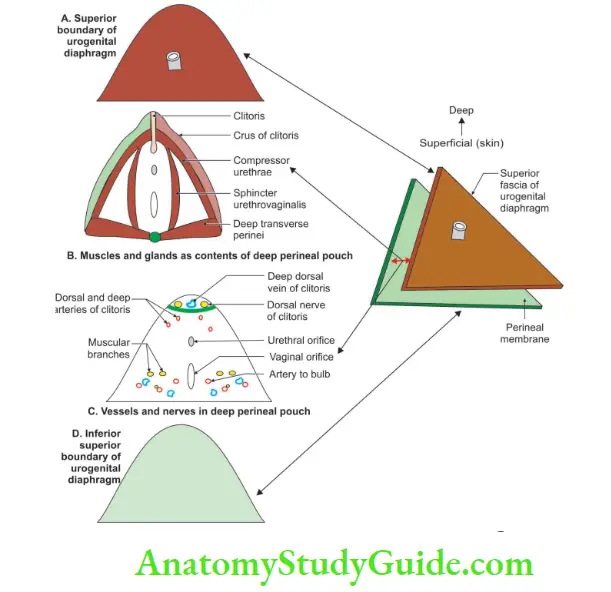
Structures:
- Urethra, and
- Vagina
Muscles
- Sphincter urethrae.
- Deep transverse perinei.
Nerves
- Dorsal nerve of the clitoris.
- Muscular branches from the perineal nerve.
Vessels: Artery of the penis, a branch of the internal pudendal artery.
3. Deep Perineal Applied Anatomy:
1. Fracture of the pelvic girdle is one of the causes of rupture of the urethra in the deep perineal pouch.
2. The urine and blood accumulate in the following sequence.
- Deep perineal pouch
- Around prostate
- Around bladder
3. Superficial to the peritoneum and deep to rectus sheath.
Leave a Reply