Periodontal ligament
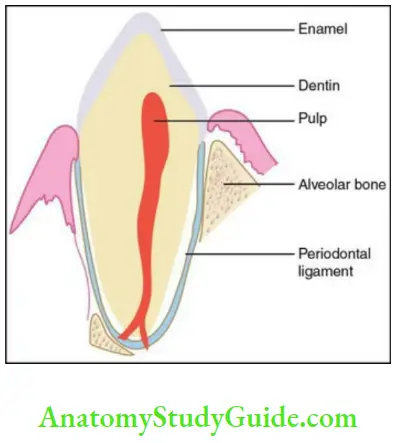
Periodontal ligament (PDL) is a soft, specialized connective tissue situated between the cementum covering the root of the tooth and the bone forming the socket wall
Table of Contents
Salient Features Of The Periodontal Ligament
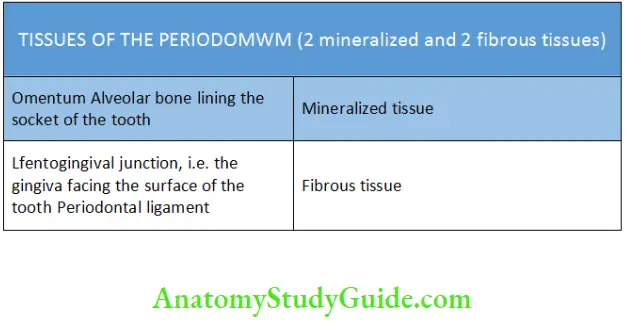
Periodontal ligament is a part of the supporting apparatus of the tooth called the periodontium which comprises four tissues.
Tissues of the Periodontium
| Body Fluids | Muscle Physiology | Digestive System |
| Endocrinology | Face Anatomy | Neck Anatomy |
| Lower Limb | Upper Limb | Nervous System |
Read And Learn More: Oral Histology Notes
The periodontal ligament occupies the space between the cementum and the periodontal surface of the bone. This space is called periodontal ligament space.
Fibroblast
- Periodontal ligament Width
- It ranges from 0.15 to 0.38 mm.
- Thinnest portion being in the middle third of the root.
- It varies with teeth and the functional state of the periodontium. It is decreased in nonfunctional teeth and increased in teeth under heavy load or stress.
- It is narrow in permanent teeth than deciduous.
- It also decreases with age.
- Periodontal ligament Extent:
- Coronally: Most apical part of the lamina propria of the gingiva
- Apically: Continuous with the pulp through the apical foramen
Clinical consideration: Infection may spread from the gingiva and the pulp to the PDL and the periapical tissues
- Periodontal ligament Radiographic appearance:
- The PDL appears as a radiolucent space of 0.4–1.5 mm width between
the radiopaque lamina dura and the radiopaque cementum.
- The PDL appears as a radiolucent space of 0.4–1.5 mm width between
Fibroblast
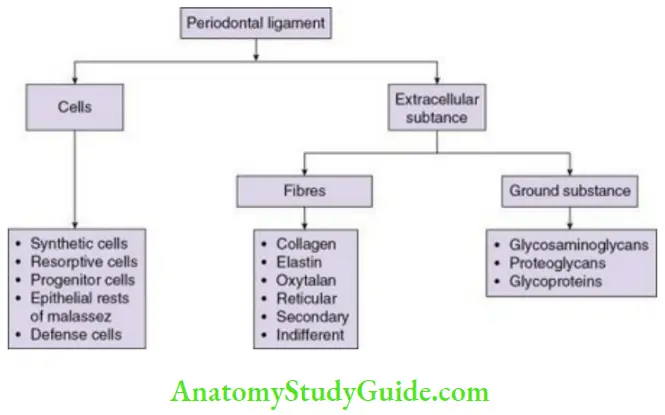
Components Of The Periodontal Ligament
Development Of The PDL

- The development of the periodontal ligament begins with the formation of the root and before eruption of the tooth.
- The cervical loop is formed by the proliferation of the inner and the outer enamel epithelium. This sheath of cells grows apically to form the Hertwig’s epithelial root sheath (HERS), which is placed between the dental papilla and the dental follicle. It later encompasses the dental papilla to separate it from the dental follicle.
- The cells of the dental follicle between the HERS and the alveolar bone are of two types:
- Mesenchymal cells of the dental follicle
- Perifollicular mesenchyme
Mesenchymal cells of the dental follicle: They are bound by the alveolar bone and dental follicle. The cells are small, stellate shaped, widely spread and randomly oriented.
- As the formation of the root continues the cells of the perifollicular area attain polarity, increase in volume, synthesize and deposit collagen fibrils and glycoprotein in the developing PDL.
- Undifferentiated stem cells are present in the developing and mature PDL that differentiate into fibroblasts, cementoblasts and osteoblasts.
Fibroblast
Development of the principal fibres of the PDL:
- Just before and immediately after the tooth erupts, the active fibroblasts lying close to the cementum of the coronal one-third of the root become aligned obliquely to the long axis of the tooth.
- The first bundles of collagen are the precursors of the alveolar crest fibre group. These are the only group that can be histologically identified immediately after tooth eruption.
- Sets of fibres grow from the cemental surface and the osseous surface of the developing alveolar process. These elongate towards each other and fuse in the midline by covalent bonding and cross linking of individual molecules of collagen.
- The horizontal group of fibres are formed completely as the tooth makes contact with the antagonist. They are seen around the coronal one-third of the root.
- The oblique groups of fibres are formed in the middle third of the root and mature as the eruption continues and occlusion is established.
- Once the apical group of fibres are formed the formation of the PDL is complete.
Cells Of Periodontal Ligament
Periodontal ligament Synthetic cells
- Osteoblasts
- Cementoblasts
- Fibroblasts
Periodontal ligament Resorptive cells
- Osteoclasts
- Cementoclasts
- Fibroblasts
Periodontal ligament Progenitor cells
Periodontal ligament Epithelial cell Rests of Malassez
Periodontal ligament Defence cells
- Mast cells
- Macrophages
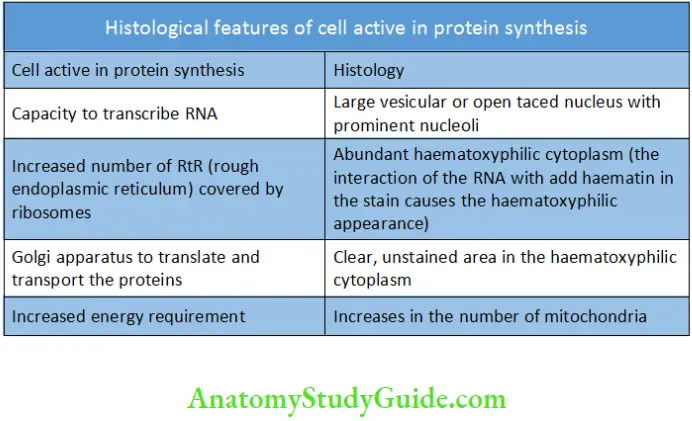
Salient Features Of Synthetic Cells
A cell that produces protein must satisfy the criteria given in Table
Histological Features of Cell Active in Protein Synthesis
Synthetic Cells:
Osteoblasts
- Osteoblasts form bone and are located along the surface of the alveolar bone/lining the socket of the tooth.
- When bone covers external surfaces like medullary cavities, it is covered by periosteum comprising two distinct layers but the bone lining the inner surface of the dental socket comprises a single cellular layer, which is a modified endosteum.
Fibroblast
Synthetic Cells Origin:
- Osteoblasts are derived from pluripotent mesenchymal cells.
Synthetic Cells Microscopic features:
- Shape: Cuboidal
- Basophilic cytoplasm
- Prominent round nucleus at the base
- Numerous mitochondria, vesicles and rough endoplasmic reticulum (RER)
- Localized and extensive Golgi apparatus
Synthetic Cells Fibroblasts:
Fibroblasts are the most numerous in the PDL.
They are placed parallel to the collagen fibres, which are best visualized in longitudinal sections.
Synthetic Cells Origin:
- Ectomesenchyme of the dental papilla and dental follicle.
Synthetic Cells Variations:
- Based on functional criteria: Fibroblasts on the bony side of the PDL have more alkaline phosphatase than on the side of the tooth.
- Based on development: Fibroblasts adjacent to the cementum develop from the ectomesenchymal cells of the dental papilla and the ones near the bone develop from the perivascular mesenchyme.
Synthetic Cells Microscopic features:
- Fibroblasts are large cells with abundant cytoplasm and numerous organelles associated with protein synthesis
- Large nucleus and prominent nucleoli
- Extensive RER, well-formed Golgi apparatus and many secretory granules
- They also possess long, thin cytoplasmic extensions.
- These cells are present in the PDL in varying stages of differentiation.
- Fibroblasts contain contractile elements like actin and myosin, which helps in generating contractile force required for tooth movement. Hence, they can also be termed as myofibroblasts.
Synthetic Cells Functions:
- Production of collagen, elastin fibres, and the ground substance comprising proteoglycans, glycoproteins and glycosaminoglycans
- Fibroblasts are unique in performing both synthesis and degradation of collagen fibres by the secretion of collagenase enzyme, thereby degrading the collagen molecules. This helps in maintenance of both turnover and homoeostasis.
- They maintain the width of the PDL by the prevention of encroachment by bone and cementum into the PDL space.
Cementoblasts
Cementoblasts are present bordering the periodontal surface of cementum.
Cementoblasts Origin:
- Cementoblasts are derived from undifferentiated mesenchymal cells and are similar to osteoblasts.
Fibroblast
Cementoblasts Microscopic features:
- Cuboidal
- Abundant cytoplasm
- Large vesicular nucleus
- The organelle for the synthesis of proteins are present in the cytoplasm
Cementoblasts Functions:
- Cementoblasts are in varying stages of differentiation and named as cementoblasts as they form cementum and also maintain the width of PDL.
Cementoblasts Resorptive cells:
Osteoclasts
Osteoclasts are cells that cause resorption of bone
Osteoclasts Origin:
- Fusion of circulating blood monocyte precursors
Osteoclasts Microscopic Features
- Larger ones are multinucleated; smaller ones are mononucleated
- Eosinophilic cytoplasm
- Under light microscopy osteoclasts are mostly present in resorption bays called Howship’s lacunae. The plasma membrane adjacent to bone is raised in folds as they are being resorbed and are termed as ruffled/striated border.
Osteoclasts Ultrastructure:
- Abundant lysosomes and mitochondria.
- Numerous Golgi saccules and free ribosomes with little RER.
Osteoclasts Fibroblasts:
Fibroblasts help in degradation of collagen by phagocytosis. The degradation is intracellular and extracellular.
Fibroblast
Cementoclasts:
Cementoclasts are similar to osteoclasts
- Occasionally found in the healthy and normal PDL.
- Mononuclear or multinucleated cementoclasts may be seen in Howship’s
lacunae on the surface of the cementum. - Help in the resorption of cementum.
Cementoclasts Progenitor cells:
- Progenitor cells cells replace the differentiated cells after they are lost at the end of their life span or due to trauma. They help in maintaining the homoeostasis by being a source for new cementoblasts, fibroblasts and osteoblasts through adult life.
- They are present in large numbers adjacent to the blood vessels and enter the PDL from the adjacent endosteal spaces.
- These cells have a small nucleus and little cytoplasm.
Cementoclasts Epithelial rests of malassez:
Epithelial rests of Malassez are remnants of Hertwig’s epithelial root sheath. They are normal components found in the PDL throughout life.
- They remain near the surface of the root as strands, networks, islands or tubelike structures. They are numerous in the furcation area.
- They can be differentiated from fibroblasts as follows:
-
- Closely packed cuboidal cells
- Prominent darkly stained nucleus
- Scanty cytoplasm
- Poorly developed Golgi apparatus and RER
- Mitochondria distributed throughout the cytoplasm
Distribution varies with age:
- More in children, lesser in number in adults
- Common in the apical region till the second decade; later seen more cervically in the gingiva above the alveolar crest.
Fate of the rests of Malassez:
- They can persist as resting, degenerating or proliferating cell masses. They can degenerate with age or may calcify to form cementicles.
- They can be the proliferating and etiologic factor for many pathologic cysts and tumours.
Defence cells:
Mast Cells
- Mast are round, small defence cells with a diameter of 12–15 microns.
- Mast cells have numerous cytoplasmic granules which are highlighted in special stains. Sometimes, there is degranulation and granules are present outside the cell in those sections.
- The granules in mast cells contain inflammatory mediators like heparin, histamine and serotonin. They also regulate endothelial and fibroblast cell populations by histamine release.
Macrophages:
Macrophages are defence cells involved in phagocytosis. They are derived from blood monocytes, thus usually found near blood vessels.
They can be differentiated from the fibroblasts as they have:
- Numerous microvilli, lysosomes and membrane bound vesicles.
- Less number of RER and Golgi complex.
Fibroblast
Macrophages Function:
- Phagocytosis of dead cells
- Secretion of growth factors to regulate fibroblast proliferation
Eosinophils
- Rarely seen
- May help in phagocytosis
Extracellular substance:
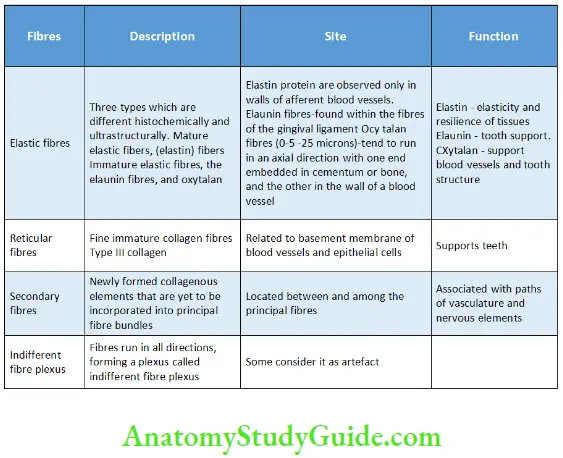
Fibres of the Periodontal Ligament Collagen fibres
The main types of collagen in the PDL are
- Type I collagen
- 80% of the collagen
- Contains two identical alpha 1 and a chemically different alpha 2 chains
- Low in hydroxylysine and glycosylated hydroxylysine
- Type III collagen
- 20% of the collagen
- Contains three identical alpha 1 chains
- Rich in hydroxyproline and poor in hydroxylysine
- It is covalently linked to Type I collagen
- It is found near the attachment sites of the Sharpey’s fibres into the alveolar bone
- Involved in turnover of collagen, tooth mobility and diameter of the collagen fibril
- Small quantities of Type V and VI collagens
- Type V coats the cell surfaces and other collagen
- It increases in periodontal inflammation
- Type VI maintains the integrity and elasticity of the extracellular matrix
- Traces of Type IV and VII collagen are associated with epithelial cell rests and blood vessels.
- Type XII collagen is believed to be present in the PDL when the ligament is fully functional.
Collagen occurs as bundles of approximately 5 microns in diameter. These bundles are called principal fibres. The collagen bundles are made up of smaller units called the collagen fibrils.
Tropocollagen To Collagen
Collagen to principal fibres
Tropocollagen molecules
↓
Collagen fibrils
↓
Collagen bundles
↓
Principle fibre groups
(alveolodental ligament)
Fibres Of The Periodontal Ligament:
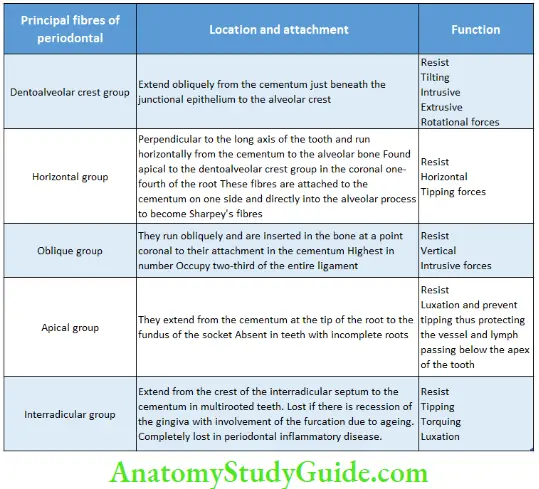
Principal fibres of the periodontal ligament
The fibre bundles that exit the cementum and alveolar bone proper to form the PDL are termed as principal fibres.
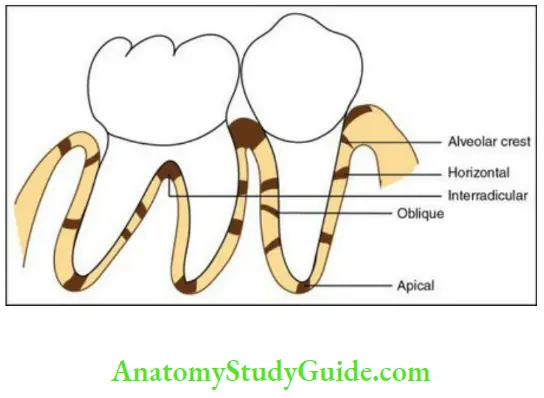
Two main groups of these fibres are named according to their location with respect to the teeth.
The gingival group is located around the necks of the teeth, and the dentoalveolar group surrounds the roots of the teeth.
The dentoalveolar fibre group consists of five differently oriented principal fibre groups named according to their origin and insertion in the dentoalveolar process.
Fibroblast
Principal Fibres of the Periodontal Ligament
Note on the dentoalveolar crest group of fibres: Confusion exists about anatomic differentiation of the periodontal alveolar crest group, from an immediately superjacent gingival fibre group, the dentoperiosteal fibres. This is due to the intertwining of the collagenous components.
The ones below the height of each interdental bony septum are periodontal and the ones above are gingival
Gingival fibres:
These fibres support the free gingiva, bind the attached gingiva to the tooth and the bone and also link one tooth to the other.
Dentogingival fibres:
- Most numerous
- Extend from the cervical cementum into the lamina propria of the gingiva
Alveologingival fibres:
- Extend from the alveolar into the lamina propria of the gingiva
Dentoperiosteal fibres:
- Extend from the cementum into the periosteum of the alveolar crest and the vestibular and oral surfaces of the alveolar bone
Circular fibres:
- Encircle the tooth in a collar like fashion and intermingle with other fibres
Transseptal fibres:
Also called the interdental ligament
These fibres extend interproximally between teeth and are found in the connective tissue of the gingiva. They extend from the cementum of one tooth and pass over the interdental alveolar crest and are inserted into the cementum of the adjacent tooth.
Sharpey’s fibres
When collagen fibres are embedded between cementum on one side of the periodontal space and alveolar bone on the other side, they are termed as Sharpey’s Fibres.
- Sharpeys fibres are numerous but smaller at their attachment into the cementum than alveolar bone.
- The fibres are subject to tensional forces as the Sharpey’s fibres are mineralized at right angles to the long axis of the fibres.
- They are fully mineralized in primary acellular cementum and partially in cellular cementum and bone.
- Transalveolar fibres are the Sharpey’s fibres that pass through the alveolar process and continue as principal fibres of the adjacent PDL or mingle labially and lingually with the fibres of the periosteum covering the outer cortical plates.
Fibroblast
Intermediate Plexus
The most recent concept was that the fibres that cross the periodontal space branch and join the neighbouring fibres forming a three-dimensional network and a zone of distinct appearance. Ultrastructural studies have concluded that this is an artefact. Based on the types, the fibres (other than collagen) are described As Follows
Fibres of the Periodontal Ligament
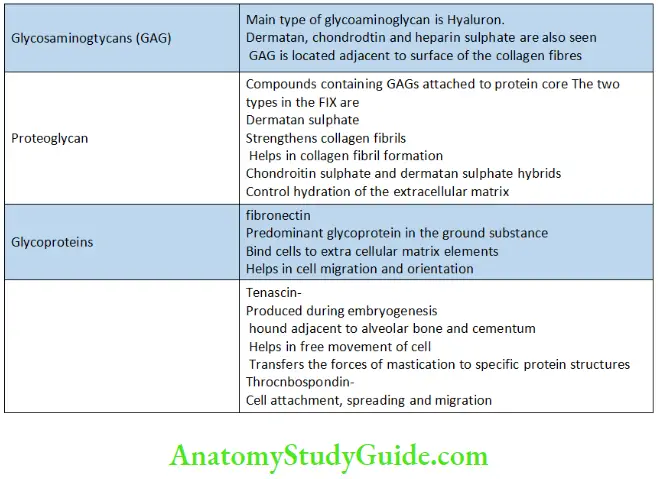
Ground Substance
This is a gel-like substance in which all the fibres are suspended. It contains 70% water. The ground substance is secreted by fibroblasts. The features of the ground substances are as Follows
Ground Substance of the Periodontal Ligament
Structures In The Connective Tissue
The loose connective tissue that contains:
- Blood vessels
- Lymphatics
- Nerves
- Irregularly arranged collagen fibres
Blood vessels
The PDL is richly vascular.
Arterial supply
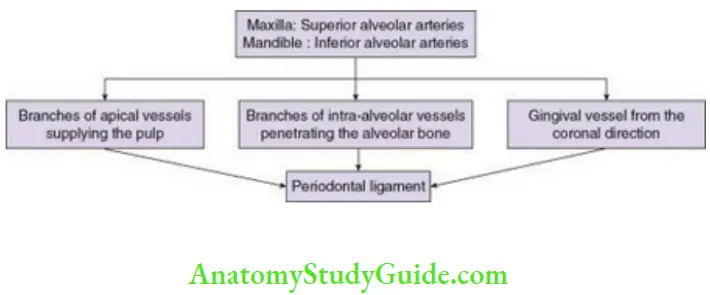
- Arterioles and capillaries form a rich network in the alveolar half of the PDL. The apex and the cervical part of the ligament are supplied by a rich plexus.
- There are numerous fenestrations in the capillaries of the PDL. There is increased diffusion and filtration through the fenestrated capillaries, which provides the metabolic requirement due to high rate of turnover of the PDL.
- The cervical plexus of capillary loops in the gingival crevice encircle the tooth. There is anastomosis between the circular plexus and the vessels of the gingiva and the PDL. This might help in rapid distribution and reverse flow of blood under occlusal load.
- Blood supply increases from incisors to molars in the PDL.
- Single-rooted teeth: Highest in the gingival third followed by apical and then middle third.
- Multirooted teeth: Highest in gingival third, equal in middle and apical third.
Venous drainage
- Accompany their arterial counterparts
- Larger channel diameter
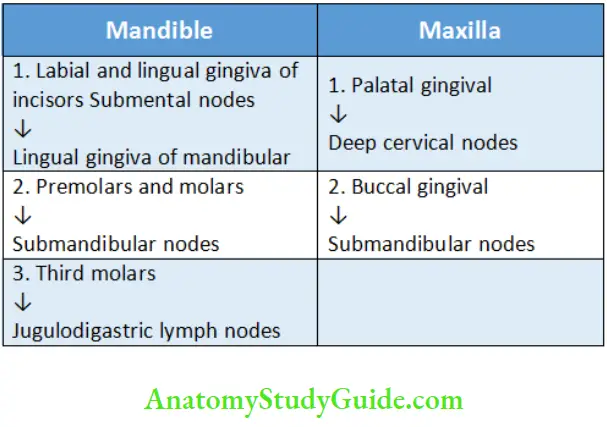
Lymphatic drainage
The lymphatic flow is from the PDL to the alveolar bone and then to the lymph nodes of the head and neck.
Lymphatic Drainage Of The Periodontal Ligament
Nerves of the PDL:
Two types of nerves innervate the PDL:
Sensory: Associated with touch, pressure, pain, proprioception sensations.
Autonomic: Associated with the vessels of the PDL.
The innervations of the PDL are through the dental branches of the alveolar nerves that pass through the perforations of the socket and branches of intraalveolar nerves passing through the bone.
Functions Of The Periodontal Ligament
The PDL has the following functions:
- Supportive
- Sensory
- Nutritive
- Homeostatic
- Eruptive
- Physical
Periodontal Ligament Supportive
The compression and widening of the PDL and periodontal space due to forces of mastication provides the support for the tooth under stress. The collagen fibres in the compressed ligament in combination with water and other molecules from the ground substance behave like a cushion.
Pressure from the vascular component acts like a hydraulic cushion for the tooth.
Periodontal Ligament Sensory
The PDL is supplied with abundant receptors and nerves that sense any movement in function. The PDL nerve fibres transmit sensation of touch, pressure and pain. Mechanoprotection protects both supporting structures of the tooth and the substances of the crown from excessive masticatory forces.
Periodontal Ligament Nutritive
The blood vessels of the ligament provide the essential nutrients for the ligament’s vitality and for the hard tissue of cementum and alveolar bone. The blood vessels are also concerned with the removal of catabolites.
Periodontal Ligament Homoeostatic
Cells of the PDL can resorb and synthesize the extracellular substance of the connective tissue of the ligament, alveolar bone, and cementum. Preservation of the width of the PDL throughout mammalian lifetime is an important measure of PDL homeostasis. In a nonfunctional tooth, the extracellular substance may be lost due to decrease in the synthesis of substances needed to replace structural molecules reabsorbed during
normal turnover and the PDL width might be decreased with concomitant cementum deposition. But, if the function of the tooth is restore then the process is reversible.
Periodontal Ligament Eruptive
The cells, vascular elements and extracellular matrix proteins of the PDL function in a collective manner to enable limited eruption of the teeth to adjust their position while they are firmly attached to the socket. PDL provides space and acts as a medium for cellular remodelling and thus continued eruption and approximal shift takes place.
Periodontal Ligament Physical
- Offers resistance to impact from occlusal forces
- Transmits occlusal force to the bone
- Provides a soft tissue ‘casing’ to protect the vessels and nerves from injury by mechanical forces
Periodontal Ligament Cementicles:
These are calcified bodies found in the PDL of older individuals. Degenerated epithelial cells can be the source of formation of these cells. Cementicles can either fuse together or join with the cementum. When they are attached to the cementum they are termed excementoses.
Clinical Considerations
Thickness of the Periodontal Ligament
- Thin in functionless and embedded teeth
- Thick in teeth under excess load or stress
Restorative/Prosthetic/Orthodontic Treatment
- The supporting structures of the tooth which is not in function for a long time should be given time to adapt to load which is suddenly placed due to a restoration, bridges, teeth opposing dentures or after orthodontic treatment.
Acute Trauma
- Accidental blow or trauma to the PDL may cause resorption of the cementum, tearing of the fibre bundles, haemorrhage and necrosis, resorption of adjacent bone and widening of the PDL space.
- This repairs on elimination of the trauma.
- Occlusal trauma leads to damage of the intraalveolar tissues and may not cause changes in the gingiva.
Orthodontic Treatment
- It depends on deposition and resorption of the bone and the PDL. Heavy forces Can lead to necrosis of the PDL and bone.
Pathologic Lesions
- Pathologic lesions commonly occur in the PDL in the periapical region. Diseases occurring in the pulp can pass into the apical periodontal tissue leading to granulation tissue formation and thus periapical granuloma.
Chronic Inflammatory Periodontal Disease
- Most common infection of the PDL.
- The PDL and the bone may be destroyed.
- It can lead to mobility of the tooth and further loss too.
- Treatment: Surgical techniques such as GTR (guided tissue regeneration), grafts, Bioglass. Bioactive molecules such as growth factor, cytokines, natural bone minerals have also been used.
Periodontal ligament Synopsis
- PDL is a soft, specialized connective tissue situated between the cementum covering the root of the tooth and the bone forming the socket wall.
- It is a part of the supporting apparatus of the tooth called the periodontium which comprises four tissues. It occupies the space between the cementum and the periodontal surface of the bone. This space is called the PDL space.
- Cells of the PDL:
- Synthetic cells – osteoblasts, cementoblasts, fibroblasts
- Resorptive cells – osteoclasts, cementoclasts, fibroblasts
- Progenitor cells
- Epithelial cell rests of Malassez
- Defence cells – Mast cells, Macrophages
- The main type of collagen in the PDL is Type I collagen. Type III collagen is about 20% of the collagen. Traces of Type IV and VII collagen are also present.
- Collagen occurs as bundles of approximately 5 microns in diameter
- These bundles are called principal fibres. The collagen bundles are made up of smaller units called the collagen fibrils
- Two main groups of these fibres are named according to their location with respect to the teeth. The gingival group is located around the necks of the teeth, and the dentoalveolar group surrounds the roots of the teeth.
- The dentoalveolar fibre group consists of five differently oriented principal fibre groups which include the alveolar crest, horizontal, oblique group, apical and interradicular group. Gingival fibres include dentogingival, alveologingival, dentoperiosteal and circular. When collagen fibres are embedded between cementum on one side of the periodontal space and alveolar bone on the other side, they are termed as Sharpey’s fibres.
- Ground substance is a gel-like substance in which all fibres are suspended. It contains 70% water.
- The functions of the PDL are supportive, sensory, nutritive, homeostatic eruptive and physical.
- Cementicles are calcified bodies found in the PDL of older individuals.
Leave a Reply