Psychological Behaviour Management Introduction
Behaviour management is the means by which the dental health team effectively and effiently performs dental treatment and thereby instils a positive dental attitude in the patient. It can be broadly classified into psychological management and pharmacological management.
Table of Contents
Psychological behaviour management refers to the application of various techniques on the basis of the theories of child psychology. It is described in detail in this chapter. Pharmacological methods are applied to children with whom psychological methods cannot be used.
Read And Learn More: Paediatric Dentistry Notes
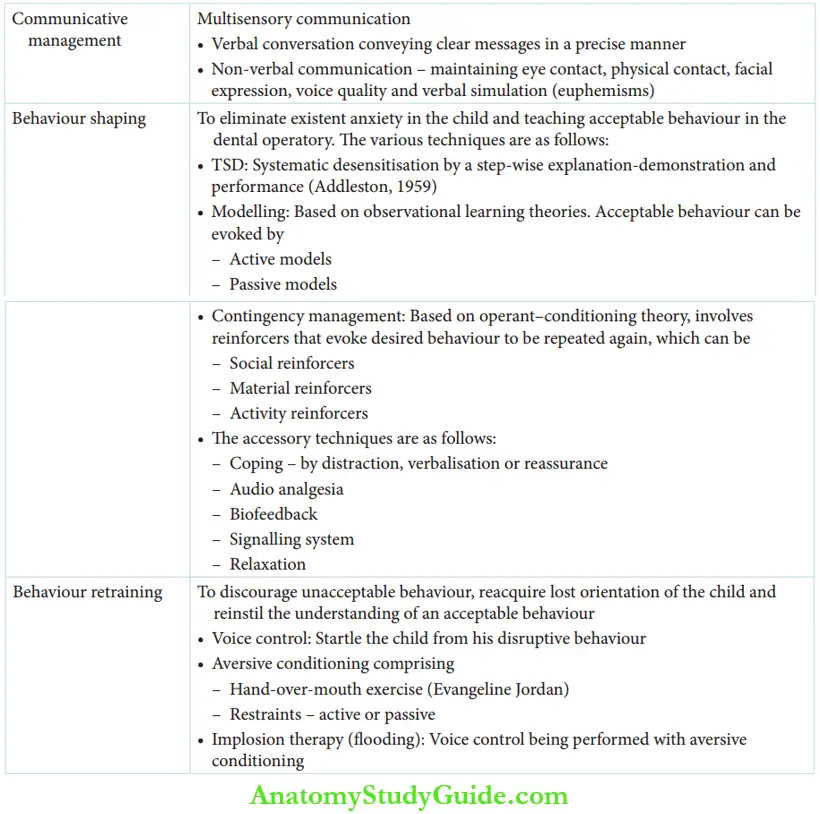
Psychological management can be applied by the following methods:
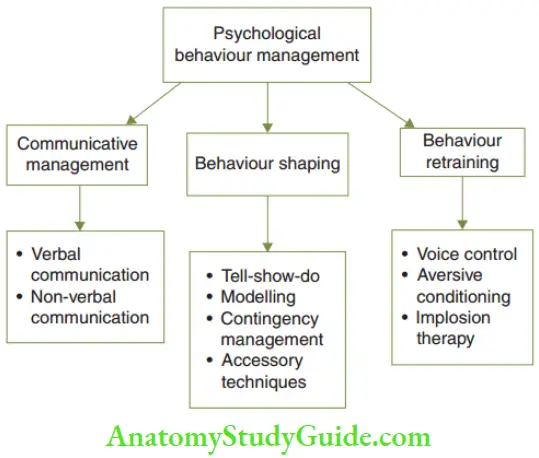
- Communicative management: Establishing a relationship and a line of management of behaviour by way of effective communication
- Behaviour shaping: Teaching children the accepted/desired behaviour in the dental operatory
- Behaviour reshaping/retraining: Discouraging unacceptable behaviour and retraining the child to resume acceptable behaviour by aversive modes
Communicative Management
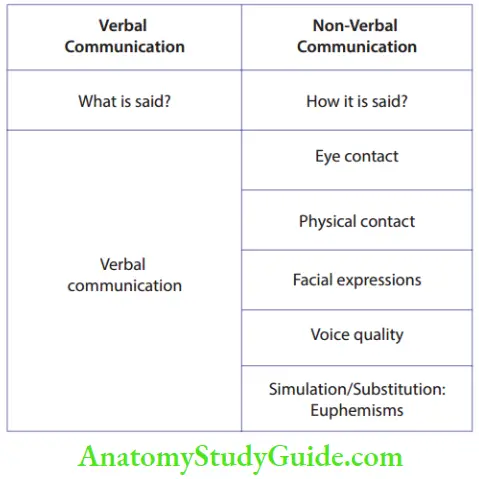
Establishing effective communication with a child in the dental operatory is one of the primary strategies of behaviour management. This communicative management comprises verbal and non-verbal communication.
When verbal conversation is clubbed with nonverbal means such as eye contact, physical contact, voice modulation and warm facial expression, it is called multisensory communication. With such communication, the following can be achieved:
- Orientation is established with the child.
- Anxiety is reduced and the child is made comfortable.
- The child is able to receive instructions for behaviour shaping in the dental operatory.
- Verbal Conversation [What Is Said] The dentist should converse in the child’s mother tongue preferably. The words and expressions should be comfortably understood by the child. It does not mean baby talk. The conversation should carry clear messages in a precise manner. Children cannot divide their attention between two sources simultaneously. They would hear neither. It implies that if the dentist is conversing with the child, the assistants and parent should be directed to refrain from the same.
- Non-Verbal Communication [How It Is Said] Non-verbal communication makes verbal communication more effective. The means of non-verbal communication are as follows:
- Maintaining eye-to-eye contact: Eyes do communicate. Maintenance of eye contact orients the child with the dentist. Communication is very effective when eye contact is persistently maintained.
- Physical contact: Gentle patting on the back, holding hands and stroking the head or the hands of the child are modes of making the child feel secure. These actions bring down anxiety and make the child feel comfortable.

-
- Facial expression: A gentle smile on the face of the dentist while conversing makes the child feel more inviting and comfortable. Authentic and warm facial expressions make communication more effective.
- Voice quality: Th pitch, amplitude and tone of the voice of the dentist can express kindness, love and firmness. The intonation of the voice helps to keep the child oriented with the conversation.
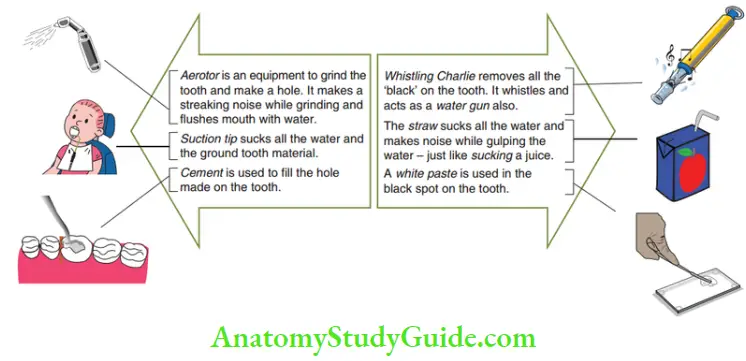
- Verbal simulation and substitution of expression: Communication is most effective in the mother tongue of the child. Foreign, offensive and unpleasant expressions can be made acceptable to the child by verbal communication. This is done by substitution of those expressions with words that are more familiar to the child and pleasant to hear. This verbal substitution is called euphemism. The euphemisms are highlighted in Figure. Euphemisms are not specific and there is no ideal euphemism for any material/equipment/ instrument. Dentists can use their own imagination and communicate in a way that the child can understand.
Behaviour Shaping
Behaviour shaping is a step-by-step teaching of the behaviour expected from the child in the dental operatory. This method makes the child aware of acceptable behaviour and eliminates anxiety. Communication has to be established before commencing behaviour shaping.
The common strategies used for behaviour shaping are as follows:
- Tell-show-do
- Modelling
- Contingency management
The acceptable behaviour of the child attained by these techniques can be retained for a sufficient time period when the techniques are applied in the right combination.
Th behaviour-shaping approaches work better when the child is motivated to follow the instructions. To enhance good behaviour, the following should be accomplished:
- The child’s stress tolerance should be improved.
- The pain threshold should be elevated.
- A feedback system should be established to intimate an increase in anxiety.
- The child should be distracted from the proceedings of the treatment.
- Tell-Show-Do The TSD or Tell-Show-Do technique was formalised by Addleston in 1959. It is a systematic technique of desensitising children from their anxiety and fear in the dental operatory. This mode of behaviour shaping is based on Bandura’s cognitive learning theory. The three steps involved in this technique are as follows:
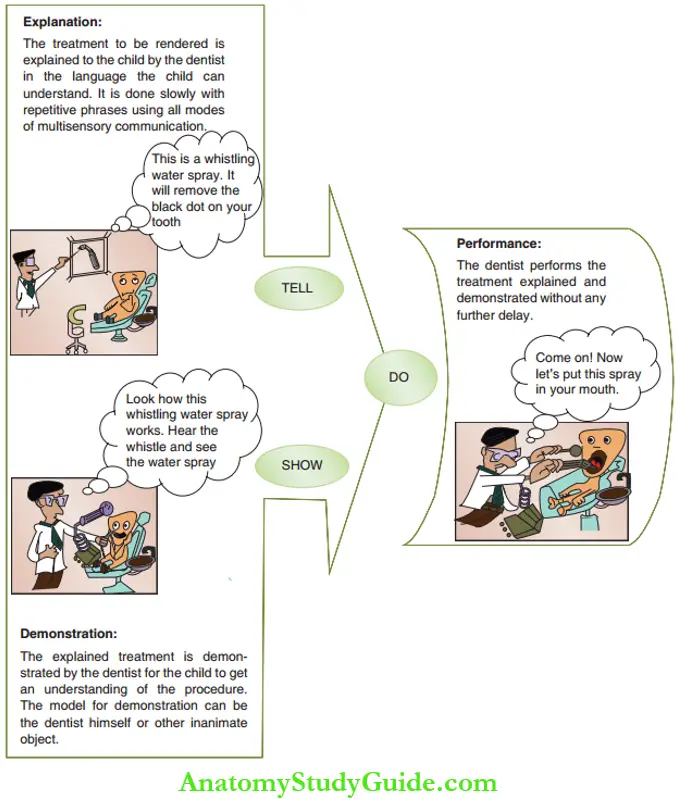
- Tell – Explanation
- Show – Demonstration
- Do – PerformanceThe logic behind this technique is that the child’s participation in the procedure decreases his anxiety. An oral explanation of the procedure removes imaginary negative thoughts. Demonstration of the same allows the child to learn more about the procedure. With this awareness, the child cooperates with a peaceful mind and a positive attitude during the procedure.
- Modelling is a mode of behaviour shaping based on the observational learning approach. It takes its origin from Watson’s behaviourism and Bandura’s cognitive learning theories. The child will learn to behave in the dental operatory by observing the acceptable behaviour demonstrated by active or passive models.
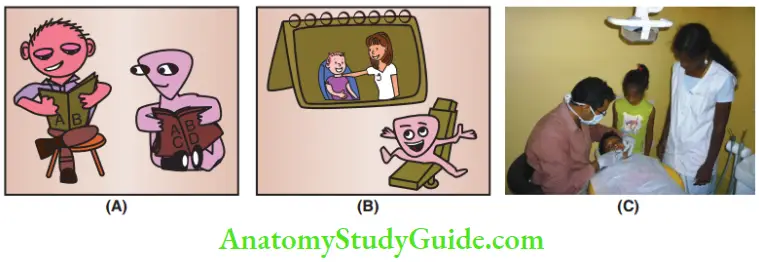 1. (A) Active model – The child repeats what is being demonstrated.
1. (A) Active model – The child repeats what is being demonstrated.
2. (B) Passive model – The child sees a well-behaved kid in a picture and wishes to be the same way.
3. (C) Clinical picture of an active model (sibling of the patient).- Active models (live models): An older child/sibling, preferably of the same sex, serves as an active or a live model. He can influence the younger child to learn acceptable behaviour.
- Passive models: The child can observe acceptable behaviour exhibited by children in a movie clip or in a series of photographs. These are passive models. The modelling technique works best in 4–6-year-old children. Active models and audiovisual screening of passive models are very effective means of modelling. The age and sex of the child in comparison should be appropriate. Modelling also conveys the positive outcome of a desired behaviour. For example, the model who demonstrated the expected behaviour may be appreciated either verbally or with a small gift. The observing child is motivated to perform the same action.
- Contingency management The contingency management approach of behaviour shaping helps the child to learn the desired behaviour readily with the help of reinforcers. It is based on Skinner’s operant conditioning theory The reinforcers are used when the child displays the desired response. This motivates the child to behave in the same manner throughout the procedure. The reinforcers can be social, material and activity reinforcers.
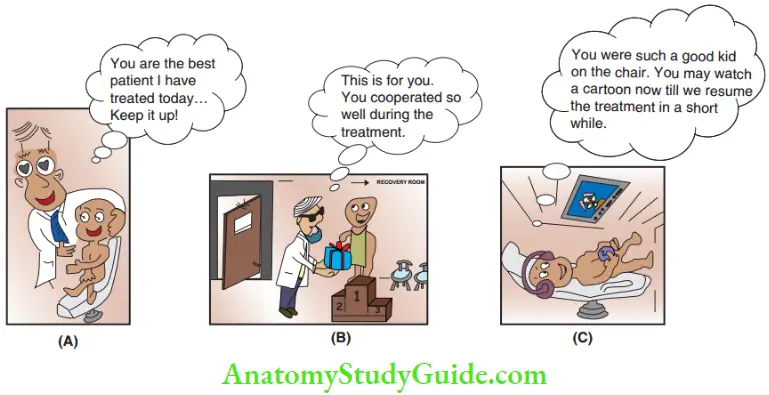 1. (A) Social reinforcer,
1. (A) Social reinforcer,
2. (B) material reinforcer and
3. (C) activity reinforcer.- Social reinforcer: It can be a warm facial expression of the dentist when the child behaves in an expected manner. The child’s behaviour can be appreciated by gentle patting, a small hug or a hand around the child’s shoulder. The child can be complemented by saying ‘You are the best patient I have had today’, ‘You are really helping me today’, ‘You are too good and brave’ or ‘I never knew you were such a good child’, etc. Immediate reinforcement of good behaviour is more effective than delayed rewards.
- Material reinforcer: A child who displays good behaviour can be rewarded with a post-operative gift It has to be mentioned that it is a token of appreciation for good behaviour. This encourages the child to behave in the desired manner in future appointments. Framing a deal with the child like promising to give a post-operative gift for good behaviour is better called bribery. Children try to negotiate the deal and demand more than what is required for their behaviour. Such a deal should be strictly discouraged. The post-operative material reinforcer should be a surprise to the child.
- Activity reinforcer: Children can be allowed to perform their favourite activities such as hugging a soft toy or watching a cartoon during the treatment. This reinforces the child to exhibit similar behaviour more frequently.
- Accessory Techniques The accessory techniques that can complement the three major behaviour-shaping techniques are discussed in the following text.
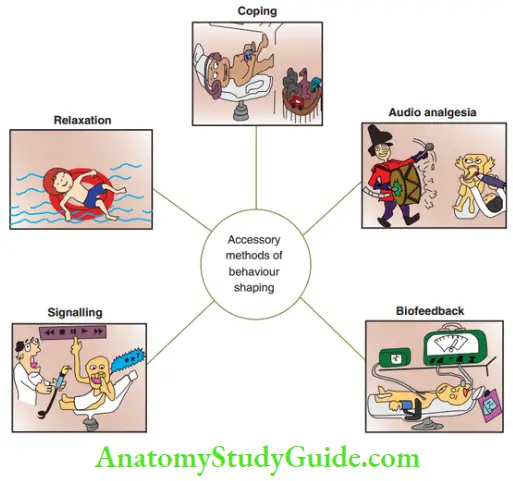
- Coping: It is a method that helps the child to encounter the stress associated with a psychologically and organically painful experience. These coping mechanisms are best suited for children
- Distraction or displacement of attention from the source of stress (dental treatment): This can be done by asking an interesting question to the child or by allowing the child to hug his favourite toy during treatment. Listening to music or watching a cartoon on the wall- or ceiling-mounted television can also distract the child from stress.
- Verbalisation: This allows children to express their fears. Communication relieves tension. However, it has to be curtailed when children keep talking to waste time during treatment.
- Reassurance: The authority figure, a dentist in this case, should establish a close relationship of trust with the child. The child, who is under the stress of undergoing treatment, should be made to feel completely protected by the authority figure (dentist). With this assurance, the child feels secure for the entire length of the procedure performed by the authority figure (dentist).
- Audio analgesia (white noise): It is a method of reducing pain and associated stress by a sound stimulus. The intensity of the sound is so high that the patient finds it difficult to listen to anything else. It works on the principle of distraction or displacement of attention from the source of stress.
- Biofeedback: It is a system that obtains signals from physiological functions such as electromyographic activity, electroencephalographic activity, heart rate and blood pressure. The system intimates any increase in anxiety, stress, discomfort and pain. The physiological functions are monitored continuously. The monitoring device is sufficiently sensitive to detect momentary changes. The responses are intimated to the dentist as a visual or an auditory signal. The dentist, in turn, reassures the patient and helps in reducing the anxiety of the patient.
- Signalling system: Signalling is a mode of coping proposed by Musselemann. It works on the principle of verbalisation. The child is instructed to communicate any pain/discomfort during treatment by raising his hand. The treatment can be momentarily paused on receiving the signal.
- Relaxation: It involves conscious training given to the child to relax when stressful situations are encountered. The child can perform certain basic exercises for relaxation. Clinically, it is less applicable as it involves learning or teaching of a series of basic exercises for relaxation. It may require several months to learn the exercises and reinforcement sessions of at least 15 minutes each day.
- Coping: It is a method that helps the child to encounter the stress associated with a psychologically and organically painful experience. These coping mechanisms are best suited for children
Behaviour Reshaping/Retraining
Not all children subdue or comply with behaviour-shaping techniques. Some children may exhibit disruptive behaviour. A child with disruptive behaviour may exhibit some or all of the features shown.
Generally, mentallyretarded, physically handicapped and very young children who are emotionally immature display disruptive behaviour. Normal children who have the potential to cooperate but are unwilling also exhibit disruptive behaviour. The strategy resorted to managing these children is referred to as behaviour reshaping/retraining/reframing.
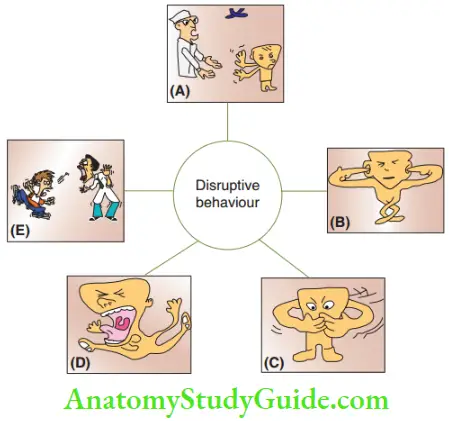
1. (A) Deliberate lack of orientation with the dentist.
2. (B) Non-compliance to the dentist’s instructions.
3. (C) Non-compliance to open the mouth.
4. (D) Loud cry and movement of body and extremities.
5. (E) Attempts to harm self or the dentist with instruments.
Behaviour is reshaping or retraining methods are used in a child exhibiting disruptive behaviour so that it can be handled with behaviour-shaping techniques thereafter. The objectives of behaviour retraining (reframing) are as follows:
- Acquire the orientation of the child with a higher stimulus of voice.
- Communicate the objective and outcome of the treatment to the child.
- Restrain the movement of the body/extremities of the child to prevent harm to self and others.
The various techniques used for behaviour retraining are as follows:
- Voice control
- Aversive conditioning
- Hand-over-mouth exercise (HOME) and its variants
- Physical restraints
- Implosion therapy
The modes of behaviour retraining, especially aversive conditioning, have to respect the laws of society and be distinctly different from physical/emotional child abuse. It should not be directed to indulge harm to children. Parental awareness and consent are mandatory by law and professional ethics before the use of any mode of behaviour retraining.
- Voice Control Voice control refers to a modification in the dentist’s voice. The dentist should resort to a louder tone of greater amplitude, pitch and intensity to dominate the interaction with the child. The objective of voice control is to startle the child. This will control the disruptive behaviour and the child will hear the dentist. In simpler terms, it is gaining the attention of a screaming child. Once the dentist has dominated the interaction and gained the child’s attention, he can resort to a softer tone appropriate to the activity of the child. Voice control may also be used in implosion therapy.
- Aversive Conditioning Aversive conditioning is based on the learning theory of Skinner’s operant conditioning and it works on the learned pattern of punishment (type 4). A certain stimulus of high magnitude is applied to remind the child of his unacceptable behaviour. It helps in regaining the child’s orientation by restraining the hyperactive behaviour. Subsequently, modes of behaviour shaping can be applied. The two constituent modes of aversive conditioning are physical restraints and HOME.
- Physical restraints: These are the modes to restrict the movement of the body, extremities and head of the child. Adequate mouth opening is allowed. Physical restraints can be active or passive.
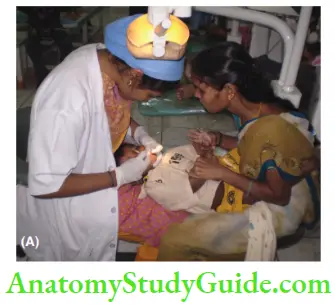
- Active restraints: These include the participation of the dentist, dental assistant or parent in restraining the movement of the child’s head, body or extremities. The lap-to-lap position and patient-over-parent manoeuvre involve the parents in restraining the movement of their child.
- Passive restraints: The primary objective of using passive restraints is to regain the orientation of the child and prevent the child from harm. The violent movement of the extremities may disturb the dental gadgets being used for the procedure and thus hurt the child. Potentially cooperative children become receptive to communication with physical restraints. Modes of behaviour shaping can be again attempted in such cases.

The following are used to restrict body movement and sustain mouth opening:- Triangular sheets, Papoose board, bean bags and wrapping devices are used to restrain the body.
- Pedi-wraps, Velcro straps, towels and taps are used to fasten the extremities.
- Head positioners can restrain unacceptable movement of the head.
- Mouth props or rubber bite blocks can be used to sustain adequate mouth opening.
- Active restraints: These include the participation of the dentist, dental assistant or parent in restraining the movement of the child’s head, body or extremities. The lap-to-lap position and patient-over-parent manoeuvre involve the parents in restraining the movement of their child.
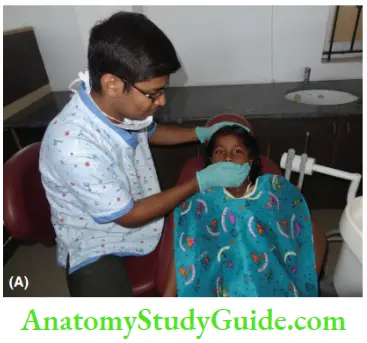
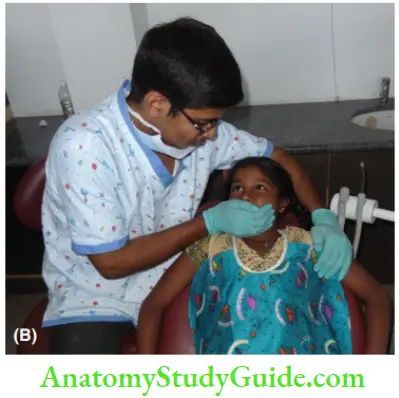
- Hand-over-mouth exercise (HOME): This technique was referred to as ‘aversion’ by Krammer, ‘restraint discipline’ by Wright and Feasby, ‘emotional surprise therapy’ by Lampshire and handover-mouth exercise by Levitas. This technique was popularised by Evangeline Jordan. The dentist keeps the hand on the mouth of the child. This muffles the loud cry of the child so that the dentist can be heard well. The dentist moves closer to the child and speaks in a soft tone. The expected behaviour is communicated to the child. This exercise should be done preferably with a gloved hand for not more than 15–20 seconds and not more than twice during an appointment. This technique is indicated for normal children who are momentarily hysterical, definite or belligerent. Behaviour-shaping methods can be reattempted when the verbal outburst of the child is stopped and attention is regained.
HOME is contraindicated in the following cases:- Very young children with whom communication cannot be established
- Mentally challenged and physically handicapped children
- Frightened children
- Children with respiratory distressThis behaviour reframing technique can be used in conjunction with physical restraints. The variants of this exercise are as follows:
- Hand over the mouth with airway restriction (HOMAR)
- Using a dry towel
- Using a wet towelHOMAR is done with the hand kept on the mouth and nose for a very short episode. However, this technique is explicitly unaccepted by a few authors.
- Physical restraints: These are the modes to restrict the movement of the body, extremities and head of the child. Adequate mouth opening is allowed. Physical restraints can be active or passive.
- Implosion Therapy When voice control is used in conjunction with HOME and physical restraints, the mode of behaviour retraining is called implosion therapy. It is also called flooding as the child is exposed to numerous stimuli. The child is thwarted and falls into the groove for establishing communication
Summary
- Behaviour management is defined as the ways and means by which the dental health team effectively and efficiently performs dental treatment and thereby instils a positive dental attitude in the patient.
- Psychological behaviour management consists of the following:
- Communicative management
- Behaviour shaping
- Behaviour retraining
Leave a Reply