Rationale Of Endodontic Treatment Notes
Endodontic pathology is mainly caused by injury to the tooth which can be physical, chemical, or bacterial. Such injury can result in reversible or irreversible changes in the pulp and periradicular tissues. These resultant changes depend on the intensity, duration, pathogenicity of the stimulus, and the host defense mechanism.
Table of Contents
The changes that occur are mediated by a series of inflammatory and immunological reactions (in the vascular, lymphatic, and connective tissues). All these reactions take place to eliminate the irritant and repair any damage. However, certain conditions are beyond the reparative ability of the body and need to be treated endodontically to aid the survival of the tooth.
The rationale of endodontic therapy is the complete debridement of the root canal system followed by three-dimensional obturation.
Read And Learn More: Endodontics Notes
Theories Of The Spread Of Infection
- The focus of infection:
- It refers to a circumscribed area of tissue, which is infected with exogenous pathogenic microorganisms and is usually located near a mucous or cutaneous surface.
- Focal infection:
- It is a localized or general infection caused by the dissemination of microorganisms or toxic products from a focus of infection.
Mechanism of Focal Infection:
Two most accepted mechanisms considered responsible for initiation of focal infection are
- Metastasis of microorganisms from infected focus by an either hematogenous or lymphomatous spread
- Carrying of toxins or toxic by-products through the bloodstream and lymphatic channels to a site where they may initiate a hypersensitive reaction in tissues.
For example, in scarlet fever, erythrogenic toxin liberated by infected streptococci is responsible for cutaneous features of this disease.
Oral Foci of Infection:
Possible sources of infection in the oral cavity which may later on setting up distant metastasis are
- Infected periapical lesions such as
- Periapical granuloma
- Periapical abscess
- Periapical cyst
- Teeth with infected root canals
- Periodontal diseases with special reference to tooth extraction
Culprit Of Endodontic Pathology
Many studies have shown that root canal infections are multifactorial in nature. In 1965, Kakehashi found that when dental pulps of conventional and germ-free rats were exposed to their own oral microbial flora, the conventional rats showed pulpal and periapical lesions, whereas the germ-free rats did not show any development of lesions.
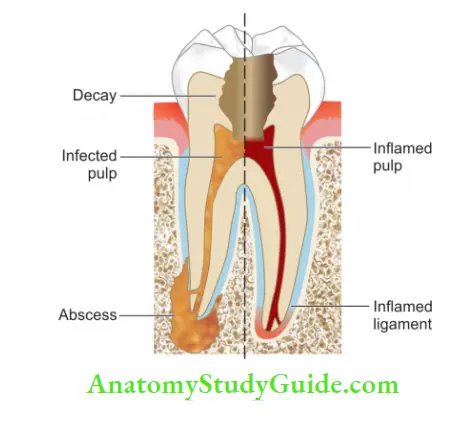
So he described the importance of microorganisms for the development of pulpal and periapical pathologies.
Portals for Entry of Microorganisms:
- Dental caries (most common route)
- Open dentinal tubules
- Accessory and lateral canals which connect pulp and periodontium
- Though defective restorations with marginal leakage
- Anachoresis (microorganisms are transported in the blood to an area of inflammation where they establish an infection).
Inflammation
Inflammation is defined as a local physiological response of living tissue to an irritant or injury. The objective of inflammation is to limit the spread or eliminate the irritant and repair damage to the tissues. Inflammation can result from
- Physical agents like cold, heat, mechanical trauma, or radiation
- Chemical agents like organic and inorganic poisons
- Infective agents like bacteria, viruses, and their toxins
- Immunological agents like antigen-antibody cell-mediated reactions.
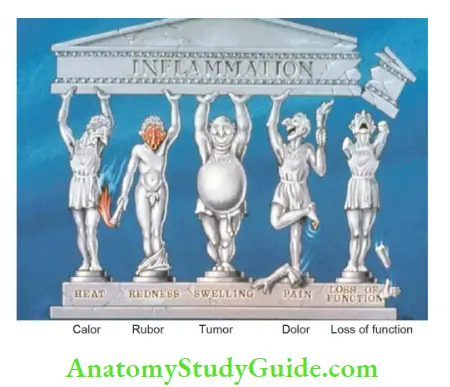
Signs of Inflammation:
Roman writer Celsus in the 1st century AD gave the following four cardinal signs of inflammation (Celsus Tetrad):
- Rubor (redness)
- A tumor (swelling due to filtration of macromolecules and flids in the affected area)
- Calor, i.e., Heat (due to vasodilatation and blood inflow in the affected area)
- Dolor (pain due to effect of cytotoxic agents on nerve endings)
- Virchow later added the fifth sign function laser (loss of function due to changes in the affected tissue).
Types of Inflammation:
- Acute inflammation (dominated by polymorphonuclear neutrophils and macrophages)
- Chronic inflammation (dominated by lymphocytes, macrophages, and plasma cells)
Tissue Changes Following Inflammation:
Two types of tissue changes are seen following inflammation:
1. Degenerative changes in the pulp can be
- Fibrous
- Resorptive
- Calcifi
- Continuous degeneration of tissue can cause thrombosis of blood vessels resulting in necrosis
- Suppuration is another form of degeneration that can occur due to injury to polymorphonuclear cells. This injury causes the release of proteolytic enzymes, resulting in the liquefaction of dead tissues leading to suppuration.
- Proteolytic enzymes digest not only leukocytes but also adjacent dead tissue. An abscess can result even in the absence of microorganisms because of chemical or physical irritation. For example, the sterile abscess is formed in the absence of microorganisms
- If the irritant is weak and the reaction is not great, serous exudate is formed consisting of serum, lymph, and fibrin
Three requisites necessary for suppuration are:
- Tissue necrosis
- Presence of polymorphonuclear leukocytes (PMNLs)
- Digestion of the necrotic material by proteolytic enzymes released by injured polymorphonuclear cells
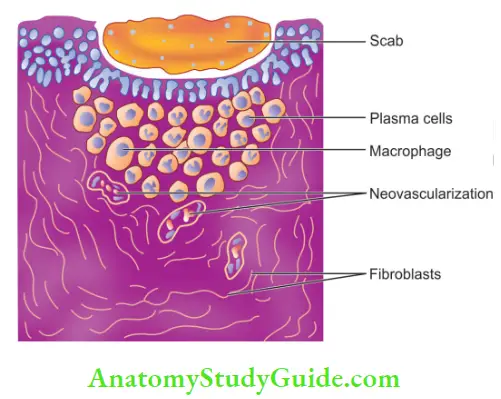
2. Proliferative changes
- Proliferative changes are produced by irritants mild enough to act as stimulants. These irritants may act as both irritants and stimulants, for example, Calcium hydroxide.
- In the center of the inflamed area, the irritant may be strong enough to produce degeneration or destruction, whereas at the periphery, the irritant may be mild enough to stimulate proliferation.
- Principal cells of proliferation or repair are the fibroblasts, which lay down cellular fibrous tissues.
- In some cases, collagen fiers are substituted by dense acellular tissue. In either case, it results in the formation of fibrous tissue. The destroyed bone may also be replaced by the formation of fibrous tissue.
Inflammatory Cells-
Neutrophils:
- Along with basophils and eosinophils, polymorphonuclear (PMN) neutrophils are called granulocytes because of the presence of granules in the cytoplasm.
- These are the first cells to migrate from vessels to the site of inflammation.
- These are attracted to inflammatory sites because of chemotactic factors produced by bacteria or by complement. For bacteria to be recognized, they must be coated in opsonins, and the process is called antibody opsonization.
- Neutrophils engulf and kill bacteria by forming phagosomes into which hydrolytic enzymes and reactive oxygen species are secreted.
- Production of enzymes and lactic acid during phagocytosis lowers the tissue fluid pH to 6.5. It results in the death of PMNs and thus the release of proteolytic enzymes (pepsin and cathepsin), prostaglandins (PGs), and leukotrienes (LTs).
- All these changes result in the breakdown of the tissue and, thus, the formation of an abscess (dead PMNs and debris).
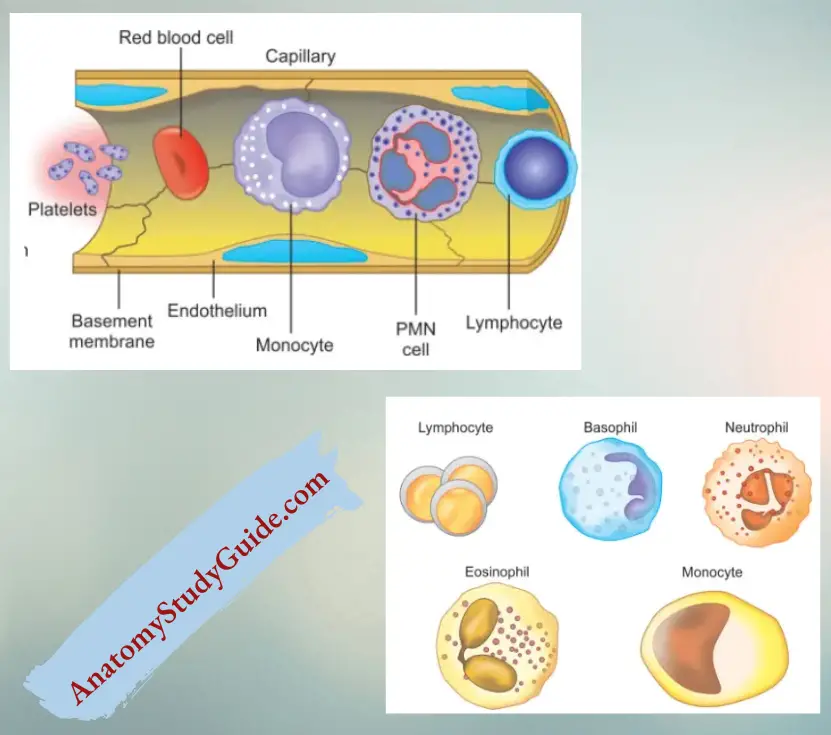
Eosinophils:
Eosinophils have many functional and structural similarities with neutrophils like their formation in bone marrow, phagocytosis, presence of granules in the cytoplasm, bactericidal and toxic action against many parasites.
Macrophages:
- When PMNs fail to remove bacteria, circulating monocytes reach the site of inflammation and change into macrophages.
- These macrophages are slow-moving and remain at the site of inflammation for a longer time (approximately 2 months). This results in the development of chronic inflammation.
Macrophages perform the following functions:
- Help in phagocytosis and pinocytosis
- Perform immunological function
- Secrete lysosomal enzymes
- Secrete complement protein and PGs
- Provide antigen to the immunocompetent cells
- Act as a scavenger of dead cells, tissues, and foreign bodies
- Fuses with other macrophages to produce multinucleated giant cells like osteoclasts, dentinoclasts, and foreign body giant cells
Lymphocytes:
1. These are the most numerous cells (20%–45%) after neutrophils.
2. Two types of lymphocytes are seen in apical periodontitis:
- T-lymphocytes
- T-helper cells: Present in the acute phase of lesion expansion.
- T–suppressor cells: Predominate in later stages preventing rapid expansion of the lesion.
- B-lymphocytes:
On getting signals from antigens and T-helper cells, they transform into plasma cells and secrete antibodies. Their number increases in hypersensitivity state and prolonged infection with immunological response
Osteoclasts:
- In the physiologic state, preosteoclasts remain dormant as monocytes in periarticular bone. During apical periodontitis, they proliferate and fuse on stimulation by cytokines and other mediators to form osteoclasts.
- The osteoclasts are responsible for the demineralization of the bone and enzymatic dissolution of the organic matrix at the osteoclast–bone interface. This results in bone resorption.
Epithelial Cells:
- Cytokines and other mediators stimulate the dormant cell rests of Malassez.
- These cells undergo division and proliferation which results in inflammatory hyperplasia.
Nonspecific Mediators Of Periradicular Lesions
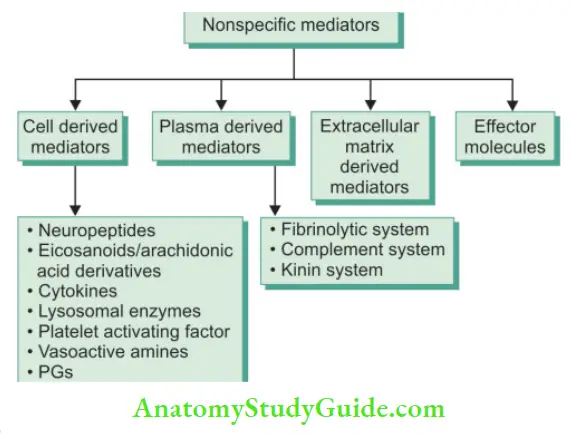
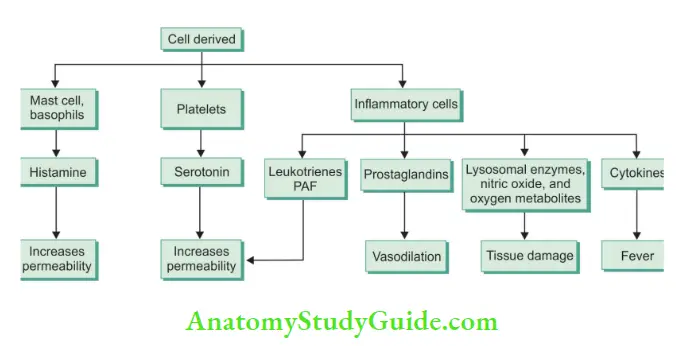
Cell-Derived Mediators
- Neuropeptides:
- These are produced following tissue injury by the somatosensory and autonomic nerve fiers. These include:
- Substance P (SP):
- Causes vasodilatation, increased vascular permeability, and blood flow.
- Calcitonin-gene-related peptide (CGRP): Causes vasodilatation.
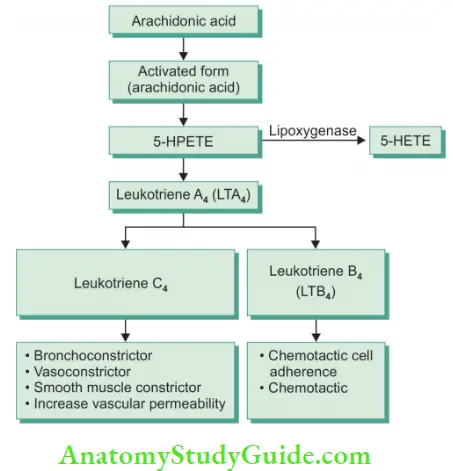
Eicosanoids:
Injury to cells releases membrane phospholipid, arachidonic acid which is metabolized by either cyclooxygenase pathway or lipo-oxygenase pathway to form PGs or LTs, respectively. These PGs and LTs involve in the inflammatory process.
- PGs like PGE 2, PGD2, PGF2a, PGI2 are commonly found in inflammatory lesions.
- LTs like LTB4, LTC4, LTD4, and LTE4 are commonly found in periradicular lesions.
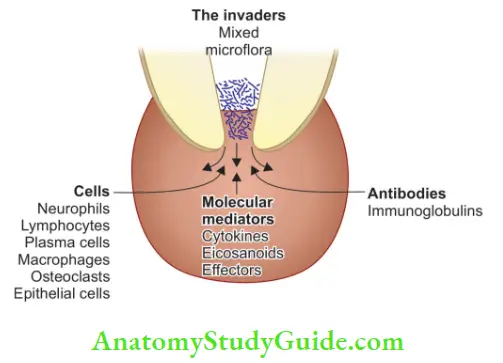
Cytokines:
These are low molecular weight polypeptides secreted by activated structural and hematopoietic cells. Different cytokines like interleukins and tumor necrosis factor (TNF) cause the development and perpetuation of periradicular lesions.
Proinflammatory cytokines
- ILI: Effects of ILI are
- Enhance leukocyte adhesion to endothelial walls
- Stimulate PMNLs and lymphocytes
- Activate the production of PGs and proteolytic enzymes
- Increase bone resorption
- Inhibit bone formation
- IL1 β is predominant in cases of periapical pathology.
- IL6: It is secreted by lymphoid and nonlymphoid cells and causes inflammation under the influence of IL1, TNFα, and interferon γ (IFN). It is seen in periapical lesions.
- IL8: It is produced by macrophages and fibroblasts under the influence of IL1β and TNFα and is associated with acute apical periodontitis.
Chemotactic cytokines:
- TNF:It is seen in chronic lesions associated with cytotoxic and debilitating effects. TNFα is seen in chronic apical lesions and root canal exudates.
- Colony stimulating factor (CSF):They are produced by osteoblasts and regulate the proliferation of PMNLs and preosteoclasts.
- Growth factors (GFs):These are the proteins produced by normal and neoplastic cells that regulate the growth and differentiation of non-hematopoietic cells. They can transform normal cells to neoplastic cells and are known as transforming GFs (TGF)
Two types of GFs:
- TGFα (produced by malignant cells)—not seen in periapical lesions.
- TGFβ (produced by normal cells and platelets) Thy counters the adverse effects of inflammatory host response by
- Activating macrophages.
- The proliferation of fibroblasts.
- Synthesis of connective tissue fibers and matrices.
Lysosomal Enzymes:
Lysosomal enzymes such as alkaline phosphatase, lysozyme, peroxidases, and collagenase cause an increase in vascular permeability, leukocytic chemotaxis, bradykinin formation, and activation of the complement system.
Platelet Activating Factor:
- It is released from IgE-sensitized basophils or mast cells.
- It causes an increase in vascular permeability, chemotaxis, adhesion of leukocytes to endothelium, and bronchoconstriction.
Vasoactive Amines:
- Vasoactive amines such as histamine and serotonin are present in mast cells, basophils, and platelets.
- They cause an increase in tissue permeability, vasodilation, and vascular permeability.
Prostaglandins:
- These are produced by the activation of the cyclo-oxygenase pathway of arachidonic acid metabolism.
- Periradicular lesions show the presence of high levels of PGE. 2. Torbinejad et al. found that periarticular bone resorption can be inhibited by the administration of indomethacin, an antagonist of PGs
Plasma Derived Mediators
Fibrinolytic System:
- The fibrinolytic system is activated by the Hageman factor which causes the activation of plasminogen.
- This results in the release of fibrinopeptides and fibrin degradation products which cause an increase in vascular permeability and leukocytic chemotaxis.
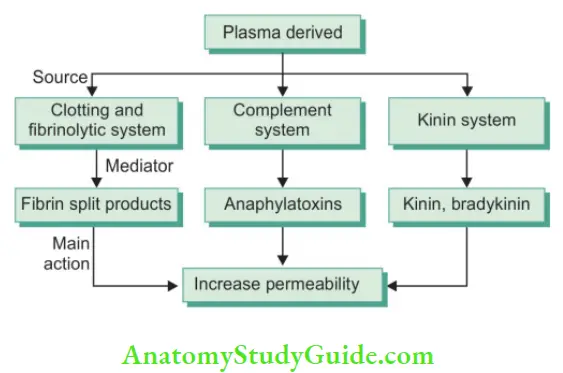
Complement System:
Trauma to periapex can result in the activation of the kinin system which in turn activates the complement system.
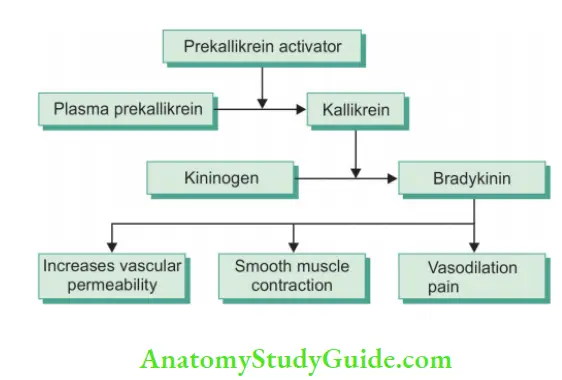
Kinin System:
- These are produced by proteolytic cleavage of kininogen.
- The release of kinins causes smooth muscle contraction, vasodilation, and an increase in vascular permeability.
Effector Molecules:
The inflammatory process in periradicular pathosis causes the destruction of cells and degradation of the extracellular matrix by enzymatic effector molecules produced in the following pathways like:
- Osteoclast-regulated pathway
- Phagocyte-regulated pathway
- Plasminogen-regulated pathway
- Metalloenzyme-regulated pathway [matrix metalloproteinases (MMPs)]
- Collagen (proteins) based matrices are degraded by MMPs.
Antibodies
These are produced by plasma cells and are of two types:
- Polyclonal antibodies are nonspecifi-like IgE-mediated reactions that interact with antigens resulting in the release of certain chemical mediators like histamine or serotonin.
- Monoclonal antibodies, like IgG and IgM, interact with bacteria and their by-products to form antigen–antibody complexes that bind to platelets resulting in the release of vasoactive amines which increase vascular permeability and chemotaxis of PMNs. Monoclonal antibodies exhibit antimicrobial effects.
- In acute abscess, the complex enters the systemic circulation. The concentration of these complexes returns to normal levels after endodontic treatment.
- In chronic lesions, the Ag–Ab complexes are confined within the lesion and do not enter into the systemic circulation.
Role Of Immunity In Endodontics
The immune system of a human being is a complex system consisting of cells, tissues, organs as well as molecular mediators that act together to maintain the health and well-being of the individual. Cells and microbial irritants interact with
each other through a number of molecular mediators and cell surface receptors resulting in defense reactions.
Immunity is of two types:
- Innate immunity
- Acquired/adaptive immunity
1. Innate Immunity:
- Innate immunity is responsible for the initial nonspecific reactions.
- It consists of cells and molecular elements which act as barriers to prevent the dissemination of bacteria and bacterial products into the underlying connective tissue.
- Cells providing innate immunity are neutrophils, monocytes, eosinophils, basophils, NK cells, dendritic cells, and odontoblasts.
2. Acquired/Adaptive Immunity:
- It involves the release of specific receptor molecules by lymphocytes which recognize and bind to foreign antigens
- Adaptive immunity is provided by
- T lymphocytes that release T-cell antigen receptors
- B lymphocytes that release B-cell antigen receptors or immunoglobulins
Histopathology of Periapical Tissue Response to Various Irritants:
The root canal of teeth contains various irritants because of pathologic changes in the pulp. Penetration of these irritants from infected root canals into the periapical area can lead to the formation and perpetuation of periradicular lesions. Periradicular tissue has an unlimited source of undifferentiated cells which can participate in inflammation and repair.
Depending upon severity and duration of the irritant, the host response to periradicular pathosis may range from slight inflammation to extensive tissue destruction. Reactions involved are highly complex and are usually mediated by nonspecific and specific mediators of inflammation.
Endodontic Implications
Fish described the reaction of periradicular tissues to bacterial products, noxious products of tissue necrosis, and antigenic agents from the root canal. He established an experimental focus of infection in the guinea pigs by drilling openings in the jaw bone and packing it with wool fiers saturated with a broth culture of microorganisms.
Fish in 1939 said that the zones of infection are not an infection by themselves but the reaction of the body to infection. This he concluded that the removal of this nidus of infection will result in the resolution of infection.
Four well-defied zones of reaction were found during the experiment :
- Zone of infection (PMN and microorganisms)
- Zone of contamination (round cells, lymphocytes, and toxins)
- Zone of irritation (macrophages, histiocytes, and osteoclasts)
- Zone of stimulation (fibroblasts, osteoblasts, and collagen fibers)
1. Zone of Infection:
- In Fish’s study, infection was confined to the center of the lesion and microorganisms were confined to that area only.
- This zone is characterized by polymorphonuclear leukocytes and microorganisms along with the necrotic cells and destructive components released from phagocytes.
- Microorganisms which are not destroyed by PMNs enter in Haversian canals or in the bone matrix during drilling in bone.
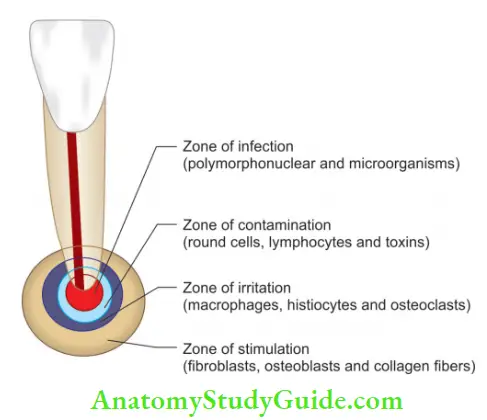
2. Zone of Contamination:
- Around the central zone, Fish observed the area of cellular destruction.
- This zone was not invaded by bacteria, but the destruction was due to toxins discharged from microorganisms in the central zone.
- Round cell infiltration, lymphocytes, osteocyte necrosis, and empty lacunae were found in this zone.
3. Zone of Irritation:
- It is found away from the central lesion because toxins get more diluted.
- This zone is characterized by macrophages, histiocytes, and osteoclasts. Degradation of collagen framework by phagocytic cells and macrophages, osteoclasts attacking the bone tissue is found.
- Histologic picture simulates the body’s attempt to repair.
4. Zone of Stimulation:
- It is found at the periphery because toxins are mild enough to act as stimulants.
- In response to this stimulation, fibroblasts and osteoblasts secrete collagen fiers.
- These collagen fiers act as a wall of defense around the zone of irritation and as a scaffolding on which the osteoblasts synthesize new bone.
Knowledge gained from the Fish study can be applied for a better understanding of the reaction of periradicular tissues to a nonvital tooth. A root canal is the main source of infection. Microorganisms present in root canals are rarely motile.
Though they do not move from the root canal to the periapical tissues, they can proliferate sufficiently to grow out of the root canal. The metabolic by-products of these microorganisms or toxic products of tissue necrosis may also get diffused to periradicular tissues. As the microorganisms enter in the periradicular area, they are destroyed by the polymorphonuclear leukocytes.
But if microorganisms are highly virulent, they overpower the defensive mechanism and result in the development of periradicular lesions. Toxic by-products of microorganisms and necrotic pulp in the root canal are irritating and destructive to the periradicular tissues.
These irritants along with proteolytic enzymes (released by the dead polymorphonuclear leukocytes) result in the formation of pus. This results in the development of chronic abscesses.
At the periphery of the destroyed area of osseous tissue, toxic bacterial products get diluted sufficiently to act as stimulants. This results in the formation of a granuloma. After this, fibroblasts come in play and build fibrous tissue, osteoblasts restrict the area by the formation of sclerotic bone. Along with these if epithelial rests of Malassez are also stimulated, it results in the formation of a cyst.
Kronfeld’s Mountain Pass Theory
Kronfeld gave the mountain pass concept in 1939 to understand the close relationship between pulp and periodontium. He employed the Fish concept to explain the tissue reaction in and around the granulomatous area.
Zone A:
Kronfeld compared the bacteria in the infected root canal with the army of enemies embedded behind “high and inaccessible mountains.” The apical foramen serves as mountain passes.
Zone B:
Army tries to descend through the mountain pass to invade into plains (periarticular tissue) beyond the mountain pass. Another army in the plains takes care of the invaders. By forming trenches and reinforcement in the form of acute and chronic inflammatory cells it tries to block the advances of enemies.
These defenders are white blood cells and other cells of granulomatous tissue. This corresponds to the accumulation of white blood cells near the root apex.
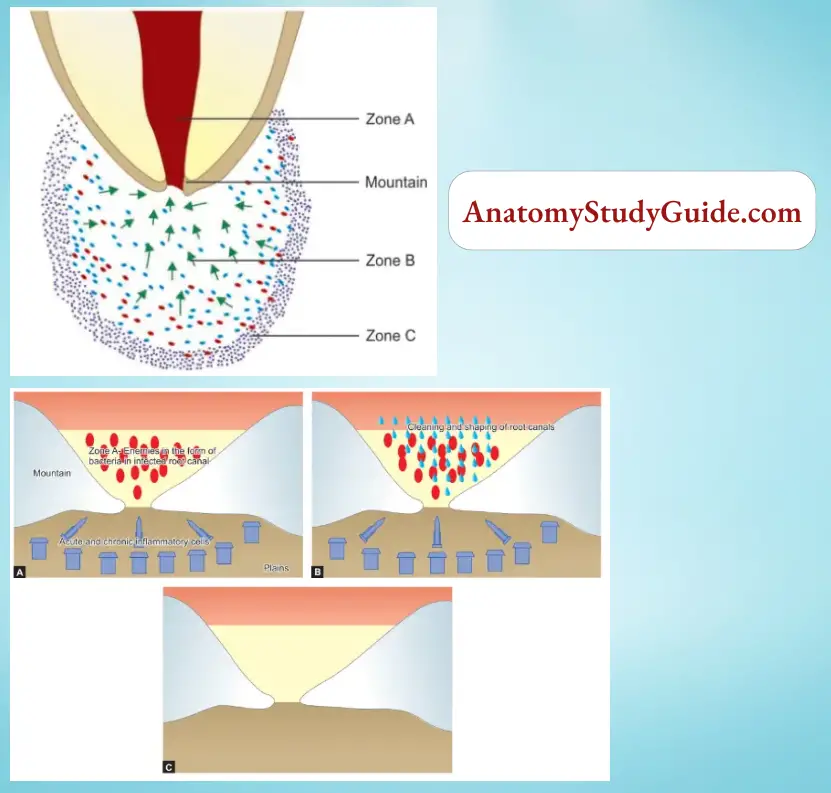
When a few invaders enter the plain through a mountain pass, they are destroyed by the defenders (leukocytes). A mass attack of invaders results in a major battle, analogous to acute inflammation.
Zone C:
Between the battle of invaders and defenders, if bacteria win and invade the plains, it results in septicemia or acute alveolar abscess or they may get destroyed by defenders. Only complete elimination of invaders from their mountainous entrenchment eliminates the need for defense forces in “plains.”
Once this is accomplished, the defending army of leukocytes withdraws, local destruction created by battle is repaired (granulation tissue), and the environment returns to its normal pattern. This explains the rationale for the nonsurgical endodontic treatment for teeth with periapical infection.
Complete elimination of pathogenic irritants from the canal followed by three-dimensional fluid impervious obturation will result in complete healing of the periapical area.
Rationale Of Endodontic Therapy
The rationale of root canal treatment relies on the fact that nonvital pulp, being avascular, has no defense mechanisms. Affected tissues within the root canal undergo autolysis and resulting breakdown products diffuse into the surrounding tissues causing periapical irritation associated with the portals of exit even in the absence of bacterial contamination.
Therefore, endodontic therapy must seal the root canal system three-dimensionally so as to prevent tissue fluids from percolating in the root canal and toxic by-products from both necrotic tissue and microorganisms from regressing into the periradicular tissues.
Endodontic therapy includes:
- Nonsurgical endodontic treatment
- Surgical endodontic treatment
Nonsurgical endodontic treatment includes three phases:
1. Access preparation:
The rationale for this is to create a straight-line path for the canal orifice and apex.
2. Shaping and cleaning:
For complete elimination of vital or necrotic pulp tissue, microorganisms, and their by-products.
3. Obturation:
To have a three-dimensional well-fitted root canal with a fluid-tight seal so as to prevent percolation and microleakage of periapical exudate into root canal space and to prevent infection by completely obliterating the apical foramen and other portals of communication.
The rationale of surgical endodontic treatment:
The rationale of surgical endodontics is to remove the diseased tissue present in the canal and around the apex and retrofit the root canal space with biologically inert material so as to
achieve a fluid-tight seal.
Leave a Reply