Rectum And Anal Canal
Prostatic Urethra Introduction
Situation: The part of urethra passing through the prostate gland is prostatic urethra.
Table of Contents
Peculiarities: It is the zvidest and most dilated part of the male ♂ urethra. It is the narrozvest at the junction with the membranous urethra.
1. Internal features: Posterior wall of the prostatic urethra shows following features.
- The urethral crest, is a median longitudinal ridge of mucous membrane.
- The colliculus seminalis, an elevation on the middle of the urethral crest.
- The prostatic utricle, a blind sac about 6 mm long, which lies within the prostate.
- There is an orifice on the elevation through which prostatic utricle opens into the urethra.
- On each side of this orifice, there are openings of the ejaculatory ducts.
- There are two vertical grooves called prostatic sinuses situated one on each side of urethral crest.
- Each sinus presents the openings of 20 to 30 prostatic glands.
Read And Learn More: General Histology Question And Answers
Urethral Sphincters
1. Urethral Sphincters Proximal (internal) :
- It is formed by condensation of intermediate circular fibres of urinary bladder.
- It is involuntary. It is supplied by autonomous nerves. They are derived from vesical plexus.
- It is damaged in men in following situations.
- Bladder neck surgery
- Transurethral resection of prostate
- Functions: It may maintain continence when external sphincter has damaged.
2. Urethral Sphincters Distal (external):
It is also called sphincter urethrae membranacea.
- Components:
- Urethral smooth muscle
- Urethral striated muscle (of rhabdosphincter). It is most important component as it is capable of sustained contractions.
- Pubourethral part of levator ani.
- It is inserted into perineal body.
- Situation: Deep perineal pouch.
- Nerve supply: It is voluntary and supplied by perineal branch of pudendal nerve.
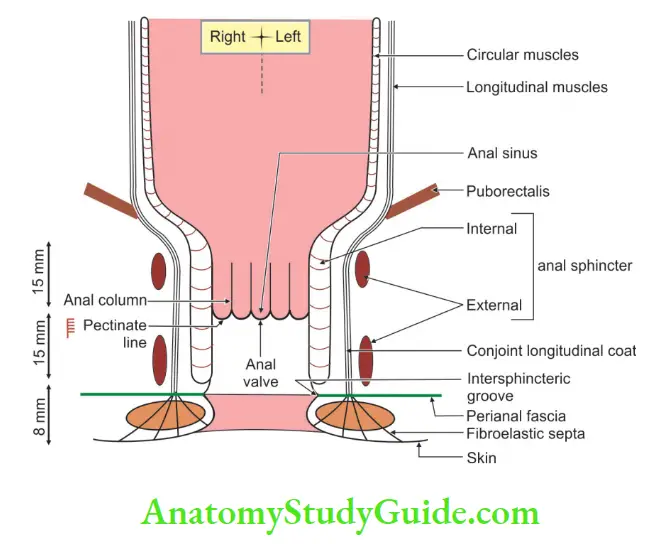
Internal Anal Sphincter
- It is involuntary in nature.
- It is local condensation of circular muscle coat.
- It surrounds the upper 3/4th, i.e. 30 mm of the anal canal.
- It extends from the upper end of the canal to the white line of Hilton.
Anal Sphincters
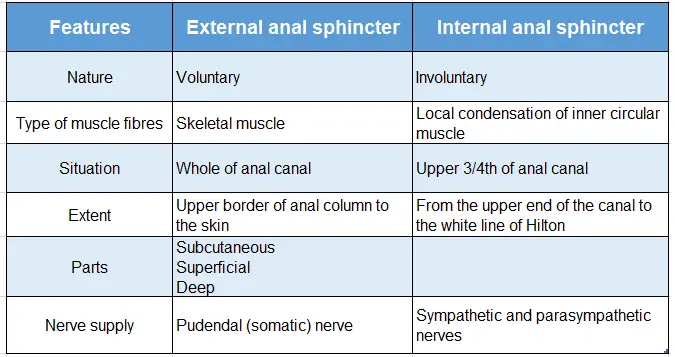
Anal sphincters external and internal:
Mucosal Folds Of Rectum
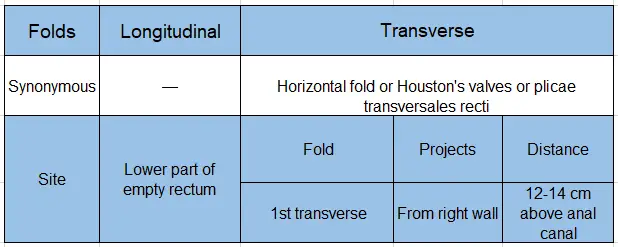
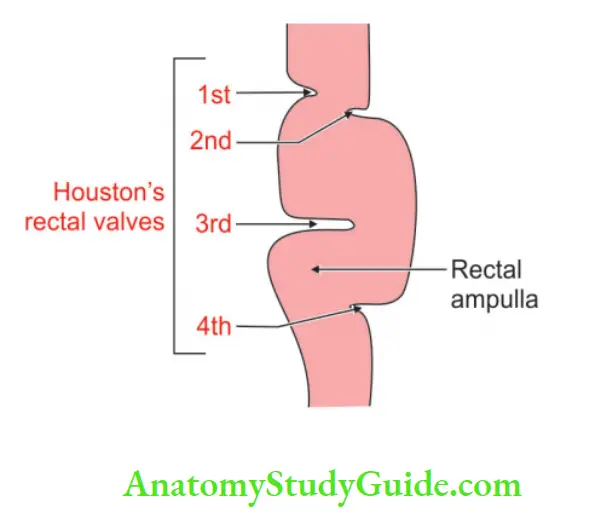
Two types of folds: Longitudinal and transverse
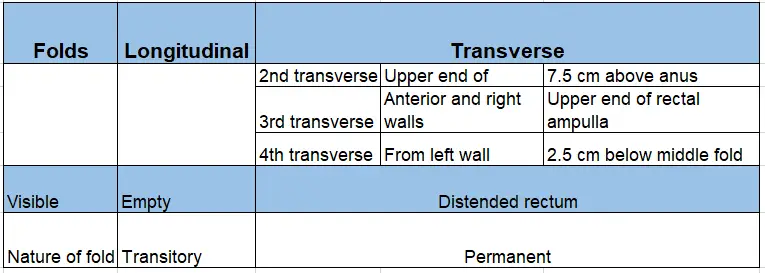
Two types of folds: Longitudinal and transverse (Contd.)
Question – 1: Describe the rectum under the following heads
1. Gross anatomy
2. Development, and
3. Applied anatomy.
Answer:
Rectum Of Introduction It is the distal part of hindgut and is present between sigmoid colon and anal canal.
1. Gross Anatomy:
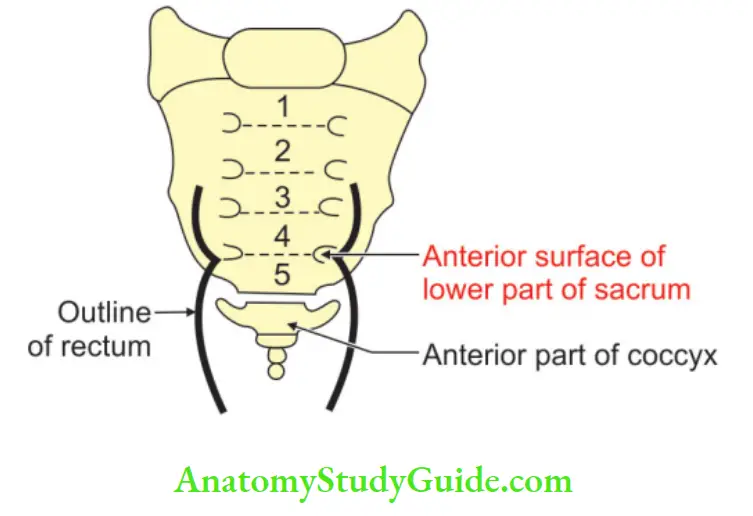
1. Situation: It is situated in the posterior part of lesser pelvis.
- It lies in front of lower three pieces of sacrum and the coccyx.
- It begins as a continuation of the sigmoid colon at the level of vertebra S3.
- It ends by becoming continuous with the anal canal.
- Length: 12 cm.
2 . External features
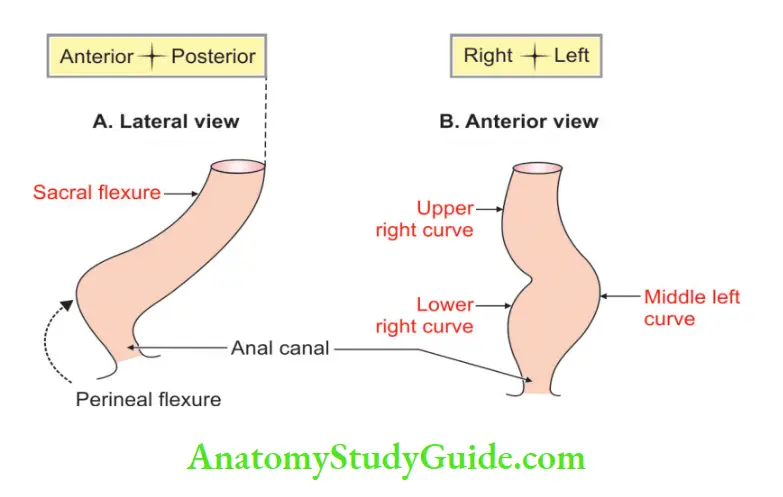
3. Course and direction: It lies in the median plane. It shows two types of curvature in its course .
1. One curvature is in the beginning and other at the end.
2. Two anteroposterior curves
- The sacral flexure of the rectum follows the concavity of the sacrum and coccyx.
- The perineal flexure of the rectum is the backward bend at the ano¬rectal junction.
- Three lateral curves.
-
- Upper lateral: Upper lateral curve is convex to the right.
- Middle lateral: Middle lateral curve is convex to the left and is most prominent.
- Lower lateral: Lower lateral curve is convex to the right.
4. Relations:
1. Peritoneal relations:
- In the upper one-third, the peritoneum covers the anterior and lateral surfaces of the rectum.
- In the middle one-third, the peritoneum covers only the anterior surface.
- In the lower one-third, there is no peritoneum.
2. Visceral relations:
1. Anteriorly:
Male ♂ :
- Upper two-thirds
- Coils of the intestine pros
- The rectovesical pouch contains a sigmoid colon.
- Lower one-third
- Urinary bladder
- The terminal part of the ureters
- Seminal vesicles
- Ductus deferens, and
- Prostate.
Female ♀ :
- Upper two-thirds: Rectouterine pouch containing coils of small intestine.
- Lower one-third: Lower part of the vagina.
2. Posterior: Relations are the same in males ♂ and females ♀
- Bones: Lower three pieces of the sacrum, and coccyx
- Ligament: Anococcygeal ligament.
- Muscles
- Piriformis
- Coccygeus, and
- Levator ani.
- Vessels:
- Median sacral
- Superior rectal, and
- Lateral sacral.
- Nerves:
- Sympathetic chain
- Ganglion impar (unpaired)
- Anterior primary rami of S3, S4, S5 and
- 1st coccygeal nerve, and the pelvic splanchnic nerves, lymph nodes lymphatics and fat.
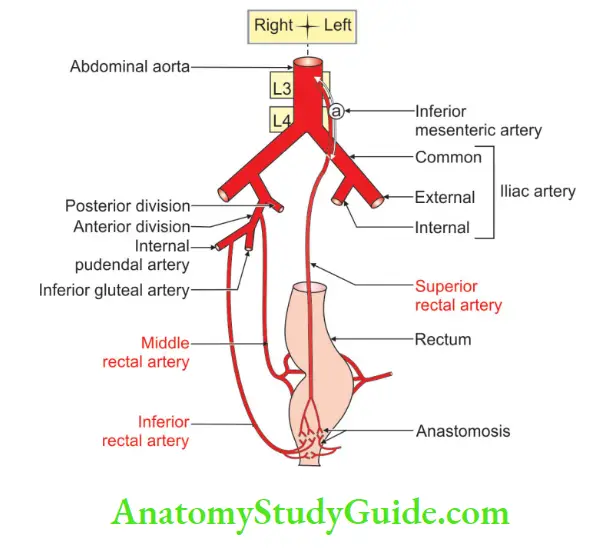
5. Blood supply:
- Arterial supply:
- The main blood supply of the rectum is by the superior rectal artery. It is the continuation of the inferior mesenteric artery.
- The muscle wall of the rectum receives from the middle rectal artery which is a branch of the internal iliac artery.
- Small branches from the median sacral artery supply the back of the rectum.
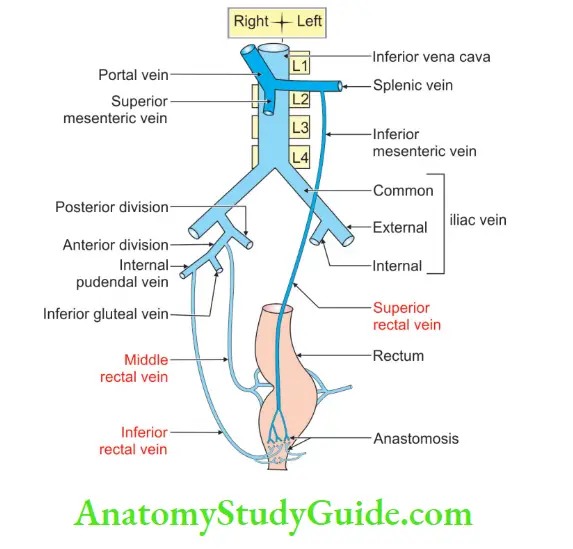
- Venous drainage: There is a very free anastomosis between the tributaries of the venous system.
- Superior rectal vein: The tributaries of this vein begin in the anal canal. It passes upward in the rectal submucosa. It pierces the muscular coat and unites to form a superior rectal vein. It continues upward as the inferior mesenteric vein.
- Middle rectal vein: It drains mainly the muscular wall of the rectal ampulla. It opens into an internal iliac vein.
6. Nerve supply: It is supplied through superior rectal and inferior hypogastric plexuses.
- The sympathetic fibres are derived from L1 and L2. These are vasoconstrictor and inhibitory to the rectal musculature and motor to the internal sphincter.
- Parasympathetic fibres are derived from S2, S3 and S4. These are motor to the musculature of the rectum and inhibitory to the internal sphincter.
- The sensations of the distension of the rectum are also carried by the parasympathetic nerve.
- Pain sensations are carried by both parasympathetic and sympathetic nerves.
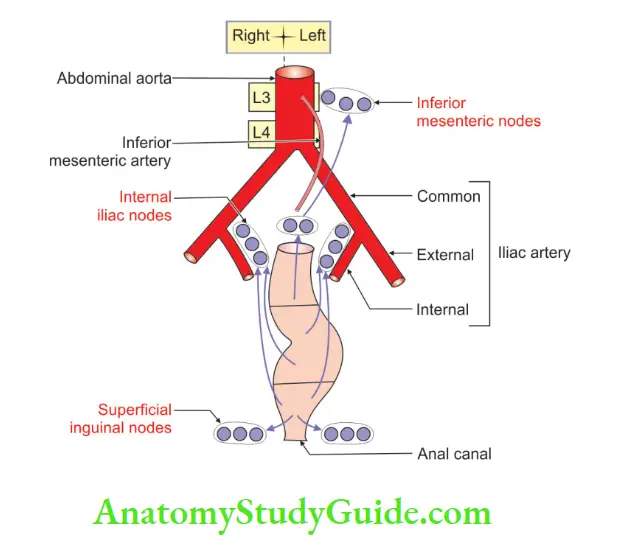
7. Lymphatic drainage: The lymphatics of the rectum run along the arteries.
- The lymph vessels in the mucous membrane provide the first filter. The lymphatic vessels pierce the wall of the rectum.
- The lymphatics from the lower half of the rectum pass along the middle rectal vessels > internal iliac nodes.
2. Development:
Chronological age: It develops in the 4th week of intrauterine life.
Germ layer: Endoderm and mesoderm.
Site: Caudal part of hindgut.
Source: The epithelium of the
- The upper part of the rectum is derived from the epithelium of the hindgut.
- The lower part of the rectum is derived from the dorsal part of the endodermal cloaca.
- Smooth muscles and connective tissues are derived from splanchnopleuric intra-embryonic mesoderm, surrounding the cloaca.
Anomalies:
- Imperforate anus: The commonest cause of imperforate anus is persistence of the anal membrane.
- Congenital rectovesical or rectourethral fistula.
- Congenital rectovaginal fistula.
- Ectopic anus.
3. Applied Anatomy:
- Per rectal examination: The following structures can be palpated by a finger passed per rectum.
- In male ♂: In males, the posterior surface of the prostate, seminal vesical and vasa differentia are palpated.
- In females ♀: In females, the perineal body and the cervix are palpated.
- Proctoscopy: It is a visualization of the rectum and anal canal by proctoscopy.
- Sigmoidoscopy: It is a visualization of the sigmoid colon by sigmoidoscopy.
- Prolapse of rectum: It may be
- Incomplete or mucosal prolapse of the rectum.
- Complete prolapse or procidentia: The whole thickness of the rectal wall protrudes through the anus.
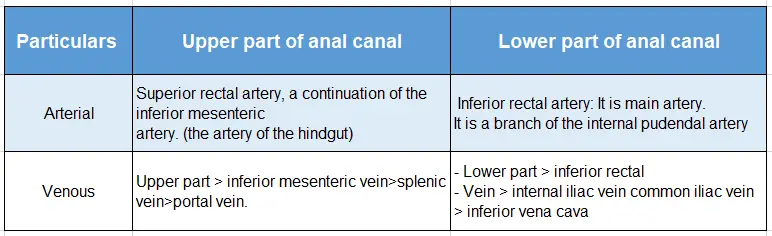
Blood Supply Of Anal Canal
Blood supply of anal canal:
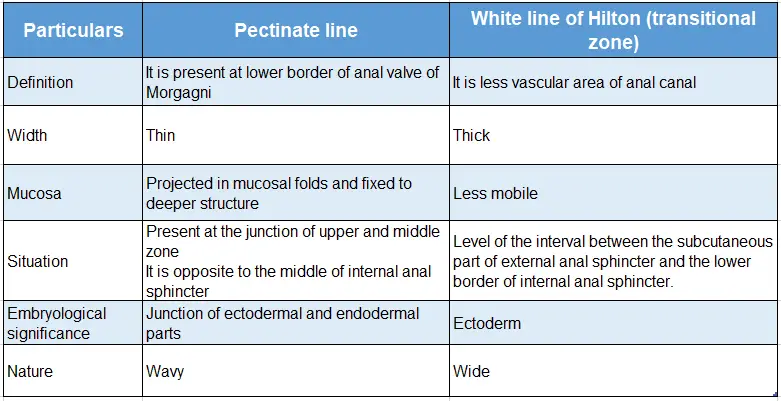
White And Pectinate Lines Of Anal Canal
White and pectinate lines of the anal canal:
Question – 2: Describe the anal canal under the following heads
1. Gross anatomy
2. Development, and
3. Applied anatomy.
Answer:
Anal Canal Introduction:
The terminal part of the large intestine is called the anal canal. It is devoid of
- Sacculations
- Taenia coli
- Appendices epiploic ae
1. Anal Canal Gross Anatomy:
1. Situation: It is situated in the anal ![]() between two ischiorectal fossae.
between two ischiorectal fossae.
- Length: It is 4 cm long and situated about 4 cm in front and below the tip of the coccyx.
- Direction: Downwards, and backward.
2. Anal Canal External features:
- Extent: It extends from anorectal flexure (½ below and 1” in front of the tip of the coccyx) to the vertical slit between two buttocks.
3. Anal Canal Relations:
1. Anterior relations are the structure at the base of urogenital ![]() .
.
- Perineal body
- In male ♂:
- Bulb of penis
- Bulbospongiosus muscle
- In female ♀: Lower part of the vagina.
- In male ♂:
2. Anal Canal Posterior: Anococcygeal ligament.
4. Laterally:
- In the upper part: Levator ani.
- In the lower part: External anal sphincter.
5. Interior of the anal canal: It is divided by pectinate and Hilton’s white line into parts
- Upper part (above the pectinate line)
- Length is 15 mm. It is lined by a mucous membrane which shows 6-10 vertical folds.
- These folds are called anal columns of Morgagni. They are prominent in children. They are ill-defined in adults.
- The lower end of the anal columns is united to each other by short transverse folds of mucous membrane.
- These folds are called anal valves.
- Above each valve, there is a depression which is called the anal sinus.
- There are about 10 mucous-secreting anal glands. They open into the anal sinuses.
- The anal valves together form a transverse line called the pectinate line.
- The middle part (between pectinate and Hilton’s lines):
- This region is called the pecten or transitional zone.
- There is no abrupt change in the esophagus to the stomach.
- The lower limit of the pecten has a whitish appearance, hence it is called the white line of Hilton.
- It is about 15 mm in length.
- It is lined by a mucous membrane, which is bluish in appearance.
- It contains a dense venous plexus which lies between the mucosa and muscle coat.
- Mucous is less mobile as compared to the mucosa of the upper part.
- Anal fissures are present in this zone.
- Lower part (cutaneous) (below Hilton’s line):
- It is about 8 mm long.
- It is lined by true skin containing sweat glands, sebaceous glands, and hair follicles.
- The lining epithelium is stratified squamous keratinized.
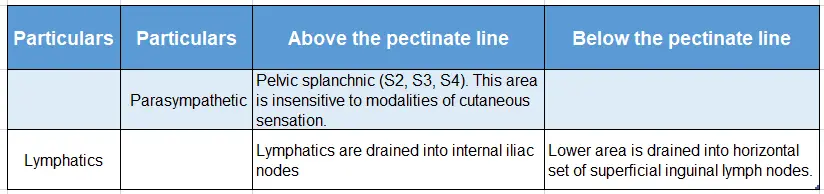
Blood supply, nerve supply, and lymphatics of the anal canal:
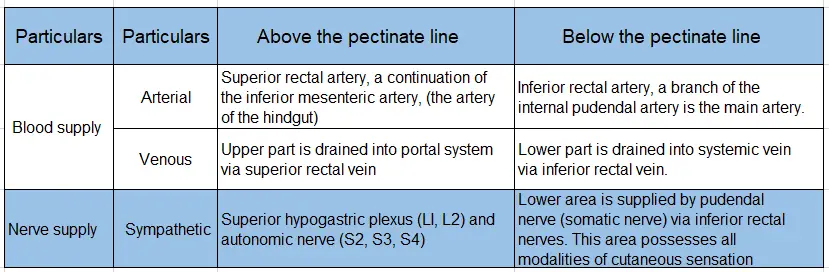
Blood supply, nerve supply, and lymphatics of the anal canal(Contd):
2. Anal Canal Development:
Chronological age: It develops in the 7th week of intrauterine life.
Germ layer: Endoderm and ectoderm.
Site: Terminal part of the hindgut.
Sources:
- The upper two-thirds of the anal canal develops from the terminal part of the hindgut.
- The lower one-third develops from the proctodaeum.
Anomalies:
- Imperforate anus occurs in 1:5000 infants. It is more common in males ♂.
- It results from abnormal development of anorectal septum.
- Anal agenesis: The anal canal may end blindly.
- Anal stenosis.
3. Anal Canal Applied Anatomy:
- Anal fissure: The lower end of anal columns is connected by small folds called anal valves.
- In chronic constipated persons, the anal valves may be torn due to.
- fecal mass catching on the fold of the mucous membrane.
- The elongated ulcer is called anal fissure, which is very painful.
- Perianal abscess is due to the trauma to anal mucosa caused by fecal matter.
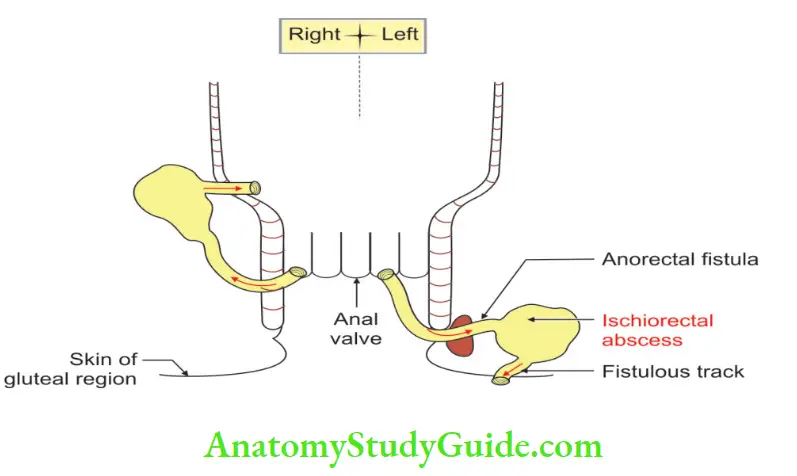
- Anal fistulae are due to the spread of inadequately treated anal abscesses. If the abscess opens only on one surface, it is called a sinus.
- Incontinence associated with rectal prolapse is due to trauma and spinal cord injury.
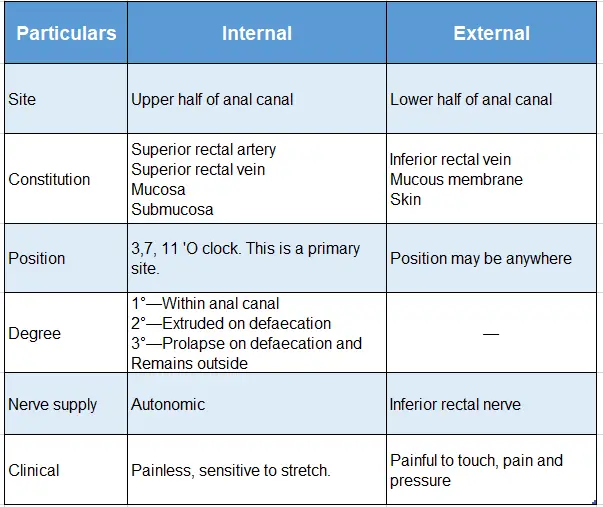
- Hemorrhoids are saccular dilatations of the internal rectal venous plexus.
- They occur above the pectinate line and are, therefore, painless.
- They bleed profusely during straining at stool.
6. Anal Canal Causes:
- Vessels are poorly supported by connective tissue
- They are valveless.
- Venous return decreases during defecation.
- Predisposing conditions
- Portal hypertension resulting from cirrhosis
- Pregnancy
- Cancerous tumor.
- Chronic constipation
- Precipitating factors
- Familial tendency associated with leg vein varicosities.
- The most dependent part of portal circulation
Leave a Reply