Renal Function Tests Properties And Composition Of Normal Urine
Knowledge of the properties and composition of normal urine is useful to understand renal function tests.
Table of Contents
Properties Of Urine
- Volume: 1000-1500 mL/day
- Reaction: Slightly acidic with pH of 4.5-6
- Specific gravity: 1.010-1.025
- Color: Normally, urine is straw colored
- Odor: Fresh urine has light aromatic odor.
- If stored for some time, the odor becomes stronger due to bacterial decomposition.
Read And Learn More: Medical Physiology Notes
Composition Of Urine
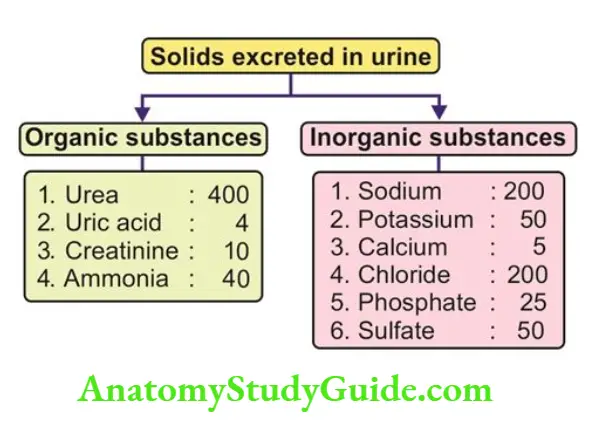
Urine consists of water and solids. The solids include organic and inorganic substances.
Renal Function Tests
Renal function tests are the group of tests that are performed to assess the functions of the kidney. The renal function tests are of three types:
- Examination of urine alone
- Examination of blood alone
- Examination of blood and urine.
Examination Of Urine — Urinanalysis
Routine examination of urine or urinalysis is a group of diagnostic tests performed on the sample of urine.
Usually, urinalysis includes three types of tests.
- Physical examination
- Microscopic examination
- Chemical analysis
Urine Physical Examination
1. Urine Volume: The increase in the volume of urine indicates the presence of diseases such as chronic renal failure, diabetes insipidus, glycosuria, and an increase in protein catabolism.
2. Urine Color: Normally urine is straw-colored. The abnormal coloration of urine is due to several causes such as jaundice, hematuria, hemoglobinuria, medications, excess of urobilinogen, ingestion of beetroot, or color added to food.
3. Urine Appearance
- Normally urine is clear. It becomes turbid in both physiological and pathological conditions.
- Normal causes for turbidity of urine are the precipitation of crystals, the presence of mucus, or vaginal discharge.
- The pathological conditions causing turbidity are presence of blood cells, bacteria, or yeast.
4. Urine Specific Gravity
- The specific gravity of urine is the measure of dissolved solutes (particles) in urine.
- Normally, it is 1.010-1.025. The specific gravity is low in diabetes insipidus and high in diabetes mellitus, acute renal failure, and excess medications.
5. Urine Osmolarity: Normally, the osmolarity of urine is 1200 mOsm/L. it Is decreased in diabetes insipidus.
6. Urine pH and Reaction
- Normal urine is slightly acidic with a pH of 4.5 to 6. Measurement of pH is useful in determining metabolic or respiratory acidosis or alkalosis.
- The pH decreases in renal diseases. In normal conditions, pH of urine depends upon diet.
- It is slightly alkaline in vegetarians and acidic in nonvegetarians.
Urine Microscopic Examination
Microscopic examination of centrifuged sediment of urine is useful in determining renal diseases.
1. Red Blood Cells: The presence of red blood cells in urine indicates glomerular disease such as glomerulonephritis.
2. White Blood Cells: Normally few white blood cells appear in high-power fields. The number increases in acute glomerulonephritis, an infection of the urinary tract, vagina, or cervix.
3. Epithelial Cells: Normally few tubular epithelial cells slough into the urine. The presence of many epithelial cells suggests nephrotic syndrome and tubular necrosis.
4. Casts: Casts are cylindrical bodies that are cast (molded) in the shape of the proximal convoluted tubules and collecting ducts.
- Casts may be hyaline, granular, or cellular in nature. Hyaline and granular casts which are formed by precipitation of proteins may appear in urine in small numbers.
- The number increases in proteinuria due to glomerulonephritis.
- Cellular casts are formed by sticking together some cells. Red blood cell casts appear in urine during glomerulonephritis and tubular necrosis.
- White blood cell casts appear in pyelonephritis. The epithelial casts are formed during acute tubular necrosis.
5. Crystals
- Several types of crystals are present in normal urine. The common crystals are the crystals of calcium oxalate, calcium phosphate, uric acid, and triple phosphate (calcium, ammonium, and magnesium).
- Abnormal crystals such as cystine crystals and tyrosine crystals appear in liver diseases.
6. Bacteria
- Bacteria are common in urine specimens because of normal microbial flora of the urinary tract, urethra and vagina and because of their ability to multiply rapidly in urine.
- So, the determination of bacteria in urine during suspected urinary tract infections requires culture studies.
Chemical analysis
- Chemical analysis of urine helps determine the presence of abnormal constituents of urine or the presence of normal constituents in abnormal quantities.
- Both findings reveal the presence of renal abnormality.
The common chemical tests of urine are:
1. Urine Glucose
- Glucose appears in urine when the blood glucose level increases above 180 mg/dL.
- Glycosuria (the presence of glucose in the urine) may be the first indicator of diabetes mellitus.
2. Urine Protein
- The presence of excess protein (proteinuria) particularly albumin (albuminuria) in urine indicates renal diseases.
- Urinary excretion of albumin in a normal healthy adult is about 30 mg of albumin per day.
- It exceeds this level in glomerulonephritis. It also increases fever and severe exercise.
3. Urine Ketone Bodies: Ketonuria (presence of ketone bodies in urine) occurs in pregnancy, fever, diabetes mellitus, prolonged starvation, and glycogen storage diseases.
4. Urine Bilirubin: Bilirubin appears in urine (bilirubinuria) during hepatic and posthepatic jaundice.
5. Urine Urobilinogen: Normally, about 1-3.5 mg of urobilinogen is excreted in urine daily. Excess of urobilinogen in urine indicates hemolytic jaundice.
6. Urine Bile Salts: The presence of bile salts in urine reveals jaundice.
7. Urine Blood
- The presence of blood in the urine (hematuria) indicates glomerulonephritis, renal stones, infection, or malignancy of the urinary tract.
- Hematuria must be confirmed by microscopic examination since chemical test fails to distinguish the presence of red blood cells or hemoglobin in urine.
8. Hemoglobin: Hemoglobin appears in urine (hemoglobinuria) during excess hemolysis.
9. Nitrite: The presence of nitrite in urine indicates the presence of bacteria in urine since some bacteria convert nitrate into nitrite in urine.
Examination Of Blood
1. Estimation of Plasma Proteins
Normal values of plasma proteins:
- Total proteins : 7.3 g/dL (6.4-8.3 g/dL)
- Serum albumin: 4.7 g/dL
- Serum globulin : 2.3 g/dL
- Fibrinogen : 0.3 g/dL
The level of plasma proteins is altered during renal failure.
2. Estimation of Urea, Uric Acid and Creatinine
- Normal values:
- Urea: 25-40 mg/dL
- Uric acid: 2.5 mg/dL
- Creatinine: 0.5-1.5 mg/dL
The blood level of these substances increases in renal failure.
Examination Of Blood And Urine
Plasma Clearance
- Plasma clearance is defined as the amount of plasma that is cleared off a substance in a given unit of time. It is also known as renal clearance.
- It is based on Fick s principle.
The determination of clearance value for certain substances helps in assessing the following renal functions:
- Glomerular filtration rate
- Renal plasma flow
- Renal blood flow.
To determine the plasma clearance of a particular substance, measurement of the following factors is required:
- The volume of urine excreted
- The concentration of the substance in urine
- The concentration of the substance in the blood.
- The formula to calculate clearance value is c=uv/p
- Where C – Clearance
- U = Concentration of the substance in urine
- V = Volume of urine flow and
- P = Concentration of the substance in plasma
Measurement of Glomerular Filtration Rate
- A substance that is completely filtered but neither reabsorbed nor secreted should be used to measure the glomerular filtration rate (GFR).
- Inulin is a substance that is completely filtered. And, it is neither reabsorbed nor secreted.
- So, inulin is the ideal substance used to measure GFR.
Insulin clearance: A known amount of inulin is injected into the body. After some time, the concentration of inulin in plasma and urine and the volume of urine excreted are estimated.
- For example, the concentration of inulin in urine is 125 mg/dL. The plasma concentration is 1 mg/dL.
- The volume of urine output is 1 mL/min. Thus, Creatinine clearance is also used to measure GFR accurately.
- It is easier than inulin clearance, because, creatinine is already present in body fluids and its plasma concentration is steady throughout the day.
- It is completely filtered and being a metabolite it is neither reabsorbed nor secreted.
- The normal value of GFR by this method is approximately the same as determined by inulin clearance.
Measurement of Renal Plasma Flow
- To measure renal plasma flow, a substance, which is filtered and secreted but not reabsorbed, should be used.
- Such a substance is para-amino hippuric acid (PAH). PAH clearance indicates the amount of plasma passed through kidneys.
- A known amount of PAH is injected into the body. After some time, the concentration of PAH in plasma and urine and the volume of urine excreted are estimated.
For example, the concentration of PAH in urine is 66 mg/dL. The plasma concentration is 0.1 mg/dL The volume of urine output is 1 mL/min.
Thus,
Renal plasma flow= Uv/P
=66×1/0.1
=660mL/min
Diodrast clearance also can be used to measure this.
Measurement of Renal Blood Flow
To determine renal blood flow value two factors are necessary:
- Renal plasma flow
- Percentage of plasma volume in the blood,
1. Renal plasma flow: Renal plasma flow is measured by using PAH clearance.
2. Percentage of plasma volume in the blood
- The percentage of plasma volume is indirectly determined by using PCV.
- For example, if PCV is 45%, the plasma volume in the blood is 100 – 45 = 55%, i.e. 55 mL of plasma is present in every 100 ml of blood.
- Renal blood flow is calculated with the values of renal plasma volume and % of plasma in blood by using a formula given below.
For example
Renal plasma flow is 660mL/min
The amount of plasma in the blood is 55%
Renal blood flow =660/55/100
=660×100/55
-0=1200mL/min
Leave a Reply