Salivary Gland
Salivary glands are exocrine glands situated in the orofacial region. Their chief function is the synthesis, storage and secretion of saliva. The salivary glands are
Table of Contents
- Compound: As they have more than one tubule entering the main duct
- Tubuloacinar: The acini constitute the secretory units
- Merocrine: Only the secretions from the cell are released
Read And Learn More: Oral Histology Notes
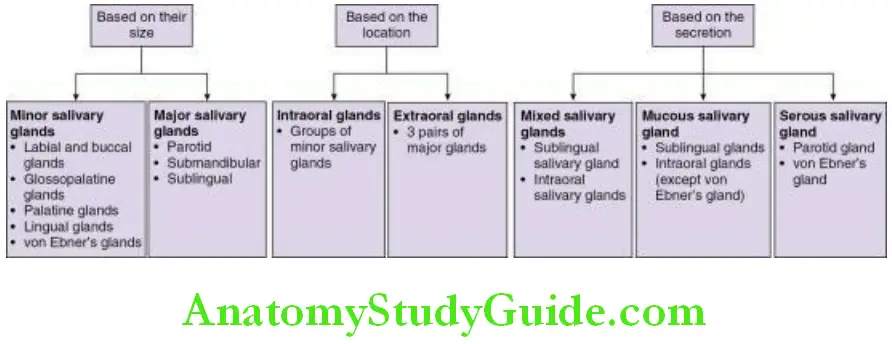
Classification Of Salivary Glands:
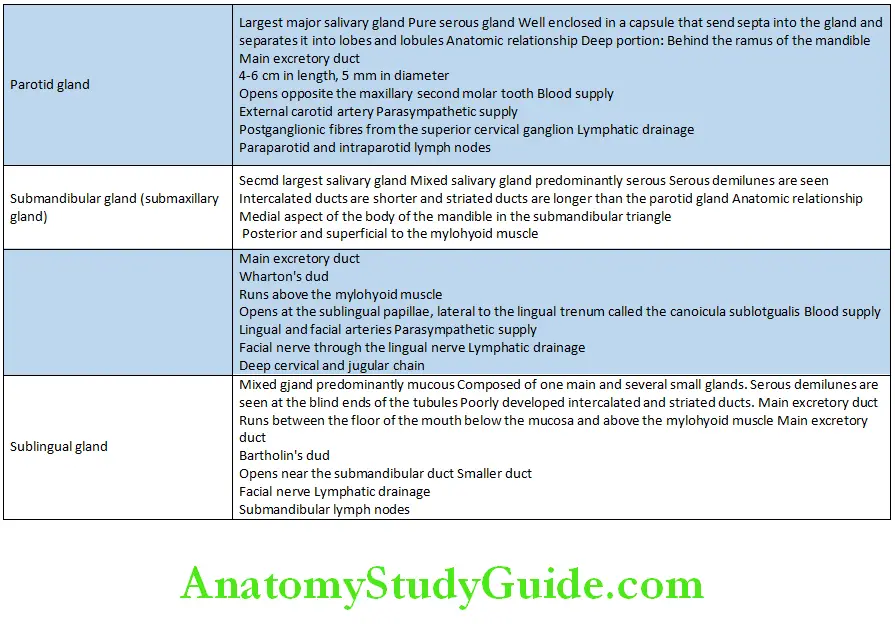
Major Salivary Glands:
Minor Salivary Glands
They are located beneath the epithelium in most parts of the oral cavity . The minor salivary glands contain numerous small groups of secretory units without a distinct capsule. They open into the oral cavity through short ducts.
- Number: 600–1000 in the oral cavity and oropharynx
- Absent in the Gingiva
- Anterior raphae region of the hard palate
- Anterior two-third of the dorsum of the tongue
Myoepithelial Cells Salivary Glands
Minor Salivary Glands
Minor Salivary Glands
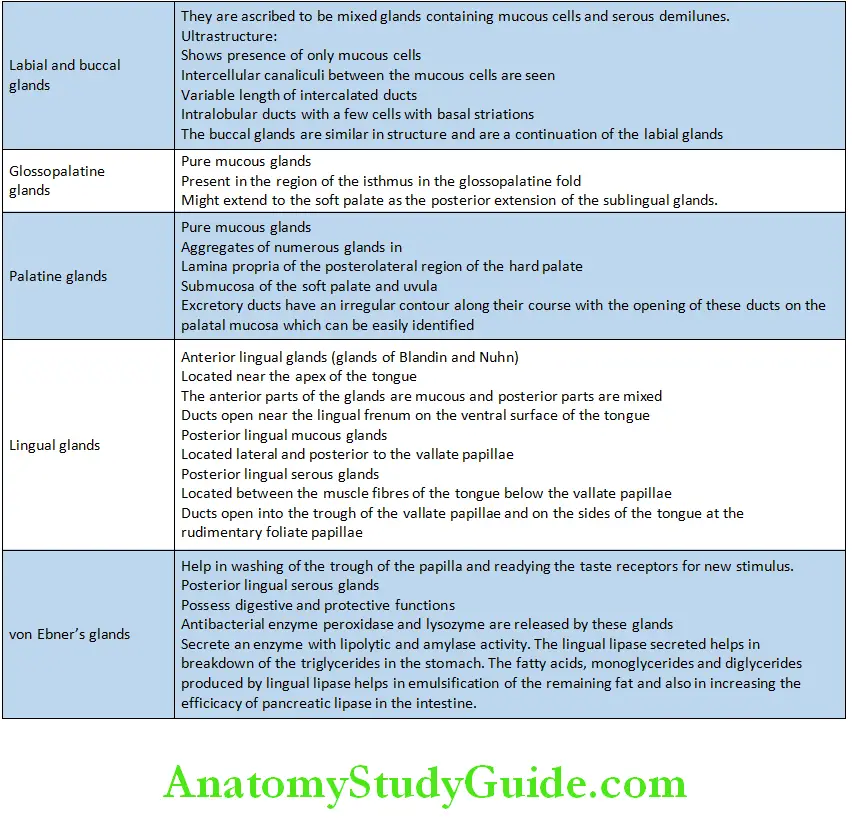
- Labial and buccal glands
- Glossopalatine glands
- Palatine glands
- Lingual glands
- von Ebner’s glands
Acini Salivary Gland
Development Of The Salivary Glands
- The development of the salivary glands begins with the appearance of solid epithelial buds extending from the developing oral cavity into the underlying mesenchyme.
- This epithelial tissue gives rise to the secretory part of the salivary gland.
- The neural crest cells give rise to the surrounding connective tissue.
- Parotid gland is the first to develop at the angle of the stomodeum.
- The epithelial buds for the development of the parotid gland extend
towards the developing ear to form solid cords (6th week of intrauterine life). - Cords canalize to form ducts and rounded ends of the ducts form secretory acini which later become functional.
- The epithelial buds for the development of the parotid gland extend
Myoepithelial Cells Salivary Glands
- Submandibular gland is the second gland to develop
- The epithelial buds grow posterior and lateral to the tongue and later
canalize to form the ducts and acini (6th week of intrauterine life).
- The epithelial buds grow posterior and lateral to the tongue and later
- Sublingual gland
- Multiple buds appear (10th week of intrauterine life) in the paralingual sulcus of the developing mouth that develop parts of the gland and later canalize.
Acini Salivary Gland
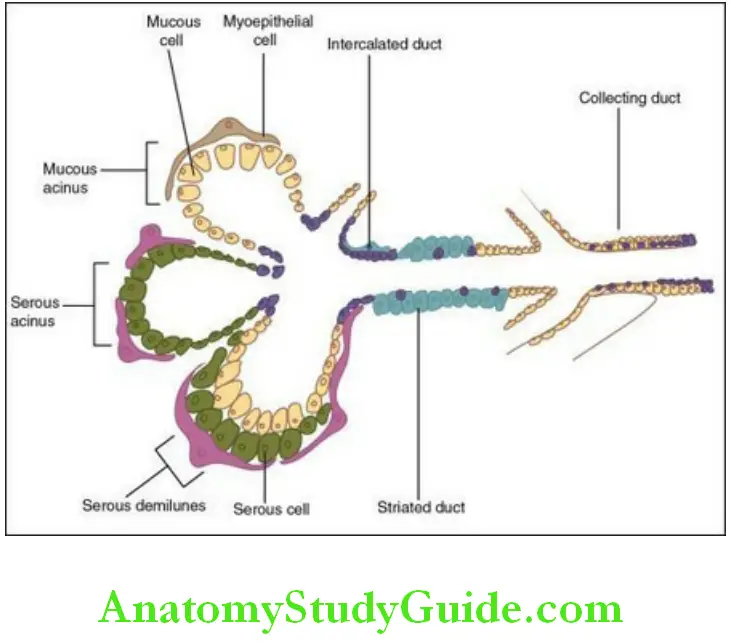
Structure Of An Acinus
Acinus is the basic functional and terminal secretory unit of a salivary gland.
- It is made up of epithelial secretory cells, i.e. serous and the mucous cells arranged in a spherical or tubular shape with a central lumen.
- The cells in the acini are present as a single layer on a basement membrane.
- The junctional complexes formed by tight, intermediate junction and desmosomes separate the intercellular spaces of the apical ends of the cells from the lumen.
- The junctional complexes hold the cells of the acinus and regulate their permeability.
- Tight junctions seal the secretory cells and control the paracellular ion influx.
- Myoepithelial cells are present on the surface of the acini.
- Ductal system:
- Lumen: It is star shaped due to the extension of the lumen between cells called intercanaliculi.
- The lumen continues with a series of ducts that merge with each other and form a larger duct which merges into the main excretory duct.
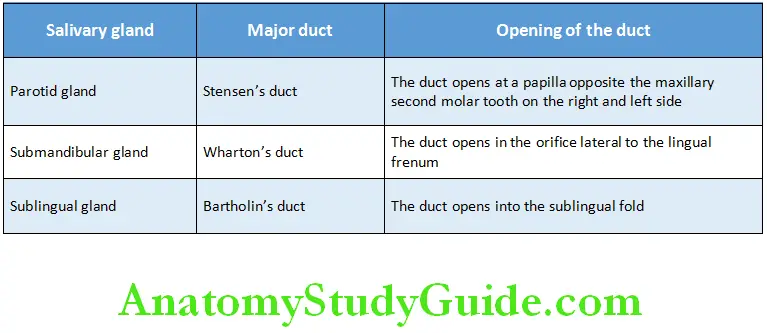
Ducts Of Major Salivary Glands
Salivary Glands Structure:
- Epithelial/parenchymal component
- Connective tissue/mesodermal component
Components Of The Salivary Gland:
Myoepithelial Cells Salivary Glands
Epithelial component:
- Comprises
1. Terminal secretary acini
2. Serous acini
3. Mucous acini
4. Seromucous acini - Myoepithelial cells
- Ductal system
Connective tissue component
- Intercalated duct
- Striated duct
- Excretory duct
Serous Acini
The acini of the parotid glands are serous; however, mucous cells may also be seen.
- It consists of a basement membrane and serous cells. The acini are spherical in shape.
- The lumen present in the centre of the acini is narrow.
- Intercellular canaliculi are evident.
- They produce secretory glycoproteins with less carbohydrate content
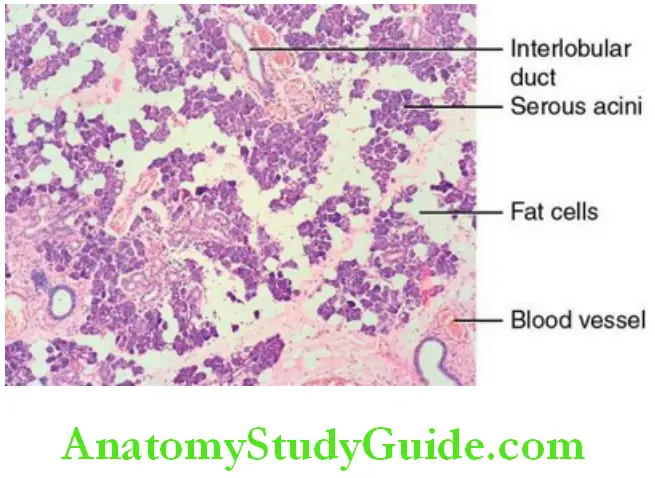
Serous cell:
The serous cells have a granular appearance in routine haematoxylin and eosin–stained sections. The secretory parenchyma is divided into lobes and further into lobules by the connective tissue. The connective tissue comprises blood vessels, nerves and the collecting ducts.
Serous Acini:
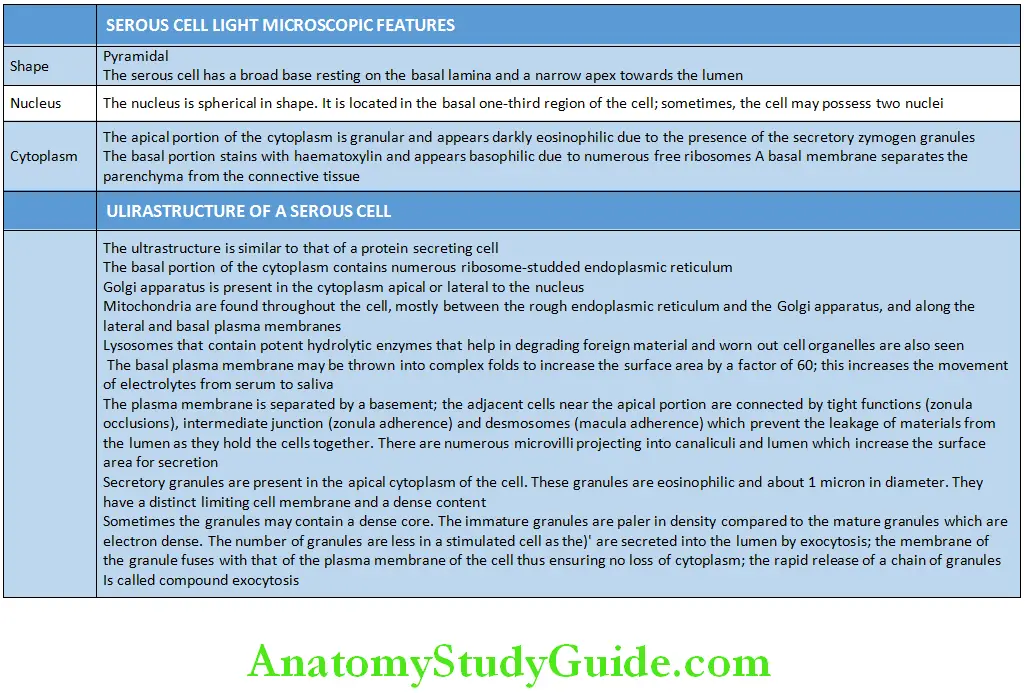
Serous cells are specialized cells that are capable of synthesis, storage and secretion of proteins. The light microscopic and ultrastructural features of serous cells are given in Table.
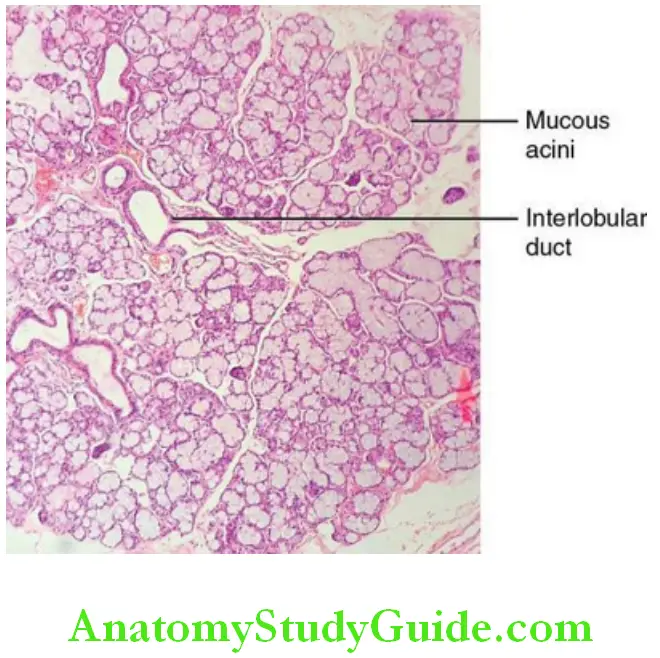
Mucous Acini
These cells are also specialized cells that can synthesize, store and secrete salivary products. The secretions from these cells are mucinous.
- The mucous acini are elliptical in shape and larger than the serous acini.
- The acini are pale as the secretions do not take up routine stains.
- The lumen is larger.
- Intercellular canaliculi are absent.
- They produce secretory glycoproteins with more carbohydrate content.
Acini Salivary Gland
Mucous cell:
Shape of the cell:
- The mucus cells are pyramidal in shape.
Myoepithelial Cells Salivary Glands
Nucleus:
- The nucleus of the cell is oval or flattened in shape and located just above the basal plasma membrane.
- The nucleus and a thin rim of cytoplasm are compressed against the base of the cell.
Cytoplasm:
- In routine histological sections, the apical cytoplasm appears empty except for a trabecular network formed by thin strands of the cytoplasm.
- It contains smaller amounts of proteins linked to greater amounts of carbohydrates (sialic acids sulfated sugars).
- The mucous cell does not stain darkly with haematoxylin and eosin stain.
- Due to carbohydrate content, the mucous cell can be seen clearly when special stain for carbohydrates such as periodic acid–Schiff stain and alcian blue stain.
Ultrastructure of a mucous cell:
- The cell membrane exhibits infoldings but are less extensive than the serous cell.
- The infoldings help in increasing the surface area for diffusion of minerals and water from the tissue fluid needed for the production of saliva.
- The cell membrane shows lesser microvilli than the serous cell.
- The rough endoplasmic reticulum is limited to a narrow band of cytoplasm along the base and lateral borders of the cell. They are also seen in the cytoplasm between the mucous droplets.
- The mitochondria and other organelles are also primarily limited to this band of basal and lateral cytoplasm.
- The Golgi apparatus is large, consisting of several stacks of 10–12 saccules sandwiched between the basal rough endoplasmic reticulum and mucous droplets.
Acini Salivary Gland
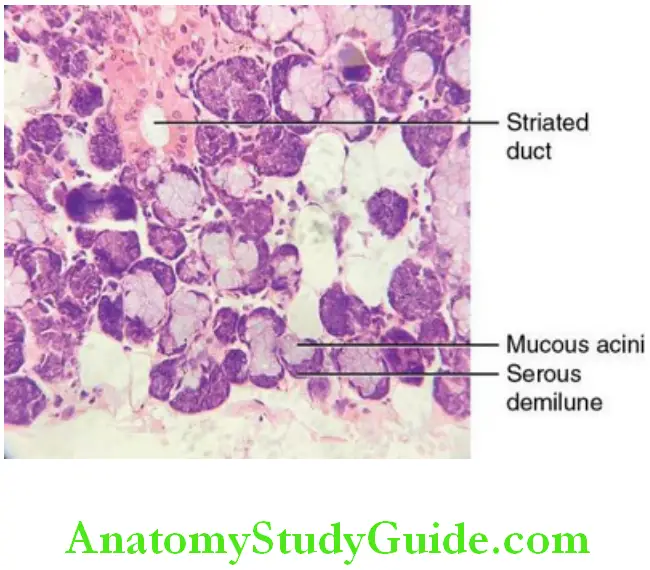
Mixed Salivary Gland/Acini
In the mixed salivary gland acini, both serous and mucous cells are present.
- The acini are tubular in shape.
- The acini comprise predominantly mucous cells or predominantly serous cells based on proportion of the acini.
- A crescent of seromucous cells called ‘Demilune Giannuzzi’ cap the mucous acini.
- These seromucous cells discharge their secretion into the tubular lumen via intercellular canaliculi running between the mucous cells
Myoepithelial Cell
The myoepithelial cells are epithelial cells with smooth muscle-like function and closely related to the secretory acini and intercalated duct cells.
- They lie between the basal lamina and basal membranes of the parenchymal cells.
- They have a small stellate shaped or spider-like body with a flat nucleus.
- The cell has numerous (four to eight) branching cytoplasmic processes that radiate from the cell body. These cytoplasmic processes embrace the secretory and duct cells.
- Their appearance is similar to that of an octopus sitting on a rock or a basket cradling the secretory unit, hence the name basket cell.
- Usually, one myoepithelial cell is associated with a secretory end piece. Rarely two/three are seen for a secretory end piece.
- The myoepithelial cells that are related to the intercalated ducts are often spindle shaped and have fewer processes.
- At times, the cell body is found on the duct region and the process extending backwards to the secretary units.
Electron microscopic appearance:
- The myoepithelial cell appears as though one of its processes is lying in the groove on the surface of a secretory or duct cell.
- The processes are filled with longitudinally oriented fine filaments (myofilaments) that are about 6 nm thick.
- Small dense bodies are frequently present between the thin filaments; these are also present in smooth muscle cells, where they appear to form a cytoskeletal network in association with 10 nm diameter filaments.
- The usual cytoplasmic organelles are largely restricted to the cytoplasm around the nucleus. Many micropinocytotic vesicles or caveolae are located on the plasma membranes of the myoepithelial cells.
- The body of the cell containing the nucleus, often lies in the space where the basal regions of two or three parenchymal cells come together.
- The plasma membrane of the myoepithelial cell closely parallels the basal membrane of the parenchymal cell. Sometimes the two are connected by means of desmosomal junctions.
Myoepithelial cells are considered to have contractile function, helping to expel the secretions form the lumina of the secretory units to the ducts.
The evidence for this
- Immunofluorescent studies indicate the presence of actin and myosin and related protein in myoepithelial cells. The structure of the myoepithelial cells is similar to smooth muscle due to the presence of actin and myosin proteins, microfilaments, desmosomal attachments and the dark bodies
- Measurements of ductal pressure after appropriate stimulation suggest a contractile process
- Cinemicrography of individual secretory units stimulated to secrete in vitro reveals a regular pulsatile movement of the entire unit.
Functions of Myoepithelial Cells
- Increase the salivary outflow from the acini.
- Decrease the backflow of saliva.
- Decrease the luminal volume.
- Influence the secretory pressure in the duct.
- Support the underlying parenchyma.
- Help saliva to flow by overcoming the increase in peripheral resistance.
- Help in maintaining the polarity of the cell and the structural organization of the acinus by sending signals to the acinar secretory cells.
- Provide signals to the secretory cells.\
- Produce proteins with tumour suppressor function such as proteinase inhibitors that are barriers to epithelial neoplasms.
- Protect the salivary gland tissue.
Acini Salivary Gland
Ductal System
The acini are connected with hollow tubes and then to ducts which progressively grow larger from the inner to the outer portion of the salivary gland.
- Each duct is lined by different type of epithelial cells.
- Ducts also play a role in the production and the modification of saliva.
- The length and type of the ducts also varies with the type of glands.
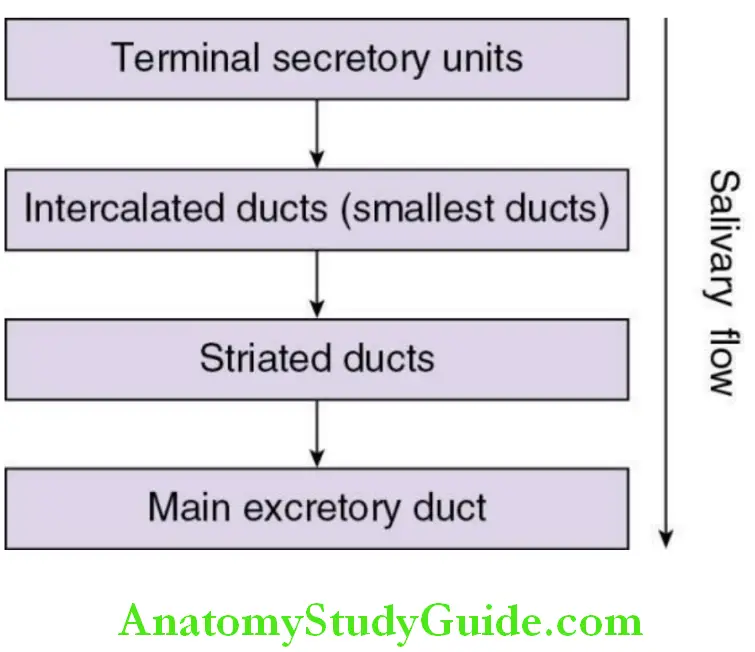
Based on the location the ducts are of the following types.
Types of ducts
1. Intralobular duct (secretory ducts):
- Intercalated duct
- Striated duct
2. Interlobular duct
- Excretory duct
Intercalated ducts:
Light microscopy:
- They are the smallest and the most distal of all ducts.
- They connect the lumen of the acini to the striated duct.
- This duct is usually compressed between secretary units.
- They are lined by a single layer of low cuboidal cells with scanty cytoplasm.
Ultrastructure:
- It resembles a serous cell.
- The cells are attached to each other at the apical region by several desmosomes.
- Rough endoplasmic reticulum is present in the basal cytoplasm along with nucleus and Golgi apparatus.
- The ductal cells close to the secretary units contain a few small secretary granules.
- Myoepithelial cell body and their processes are present around the cell.
Functions of intercalated ducts:
- The cells of this duct secrete antibacterial proteins, lactoferrin and lysosomes.
- They modify the contents of saliva by secretion and absorption.
- The intercalated duct cells are pluripotent cells that can differentiate into acinar cells or other parenchymal cells to help replace damaged cells in the straited duct or the end piece.
Striated Duct:
The striated ducts are the largest among the intralobular ducts. They collect saliva from the intercalated and carry it into the excretory ducts.
Striated Duct Light microscopy:
- Lined by a layer of tall columnar epithelial cells.
- The cells have a centrally placed large and spherical nucleus.
- The cytoplasm is abundant and appears eosinophilic. Multiple striations are present at the basal end of the cells.
Striated Duct Ultrastructure:
- Multiple deep infolding of the plasma membrane in the basal cytoplasm.
- Abundant vertically aligned large mitochondria are present in the portion of the cytoplasm between the infoldings of the basal plasma membrane.
- The combination of these infolding and mitochondria accounts for striations seen in light microscopy. Infoldings and numerous mitochondria indicate that the cell takes part in active transport electrolytes and water.
- Rough endoplasmic reticulum, Golgi apparatus, smooth endoplasmic reticulum and small granules are present in the perinuclear cytoplasm.
- The apical cytoplasm may contain branching, tubular, smooth endoplasmic reticulum, small secretory granules of moderate density. Lysosomes, small peroxisomes and bundles of
- cytoplasmic filaments, free ribosomes are also present. Short microvilli project into the lumen from the apical surface.
- Apical junctional complexes and desmosomes join the adjacent cells.
- The cells of the striated duct secrete kallikrein.
Acini Salivary Gland
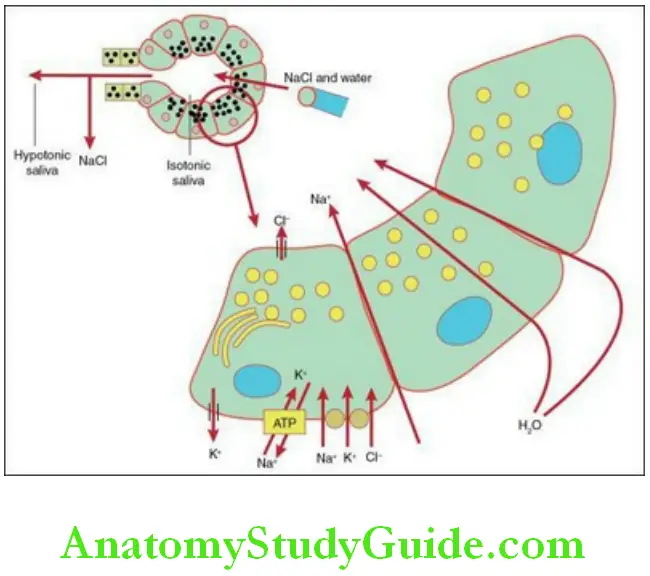
Modification of saliva in the striated duct:
In the striated duct, electrolyte resorption and secretion takes place .
- When the saliva enters the striated duct,
- It is isotonic or slightly hypotonic to plasma with the sodium and chloride composition approximately equal to that of plasma.
- The potassium concentration is significantly higher than that of plasma.
- The bicarbonate concentration is variable.
- The striated duct actively reabsorbs sodium from the primary secretion and secretes potassium and bicarbonates. Chloride follows the electrochemical gradient established by sodium reabsorption.
- At an increased flow rate, as the saliva is in contact with the ductal epithelium for a short period of time, sodium reabsorption is less efficient and the concentration of sodium in saliva is increased.
- In order to facilitate this event, the basal region of the striated duct cells contains high concentration of the transport enzyme (Na and K)–activated adenosine triphosphatase.
- The reabsorption of Na+ and Cl− is more than the secretion K+ and HCO−3 which leads to hypotonic saliva in the lumen of the duct.
Excretory Duct:
The intralobular ducts formed by the joining of striated ducts enlarge and are surrounded by layers of connective tissue. These ducts then become large and nonstriated to become the excretory ducts which are interlobular.
- This duct is lined by pseudostratified columnar epithelium.
- There are tall columnar cells and smaller basal cells, mucous goblets cells and ciliated cells. Few cells that are eosinophilic and loaded with mitochondria are also seen. These cells are called oncocytes. Striations may be maintained in the cells.
- The epithelium undergoes transition from stratified epithelium to cuboidal epithelium and then to stratified squamous epithelium as it merges with the epithelium of the oral cavity.
- Lymphocytes and macrophages are seen at the base of the ductal epithelium.
Excretory Duct Functions of the ducts:
- Transport of saliva from secretary units to the oral cavity.
- Modifies the primary saliva secreted by the secretary units.
- Intercalated ducts secrete lactoferrin and lysozyme.
- Striated ducts secrete kallikrein.
- Brings about resorption and secretion of the electrolytes.
- Striated ducts actively reabsorb sodium and secretes potassium and carbonate.
Connective Tissue Of The Salivary Glands
Stroma: Glycoproteins and proteoglycans
Fibres: Collagen fibres and oxytalan fibres
Cells: Fibroblasts, macrophages, mast cells, leukocytes, fat cells and plasma cells
Blood supply: highly specialized.
The arteries enter the gland along with the excretory ducts. They branches out into the individual lobules of the gland. There is dense concentration of capillaries around the striated duct as immense ionic exchange takes place. One or more arteries are seen around the intercalated duct and the secretory units. Arterio-venous anastomoses is seen around the excretory duct. The venous drainage venous return is accompanied by venae comitantes.
Salivary Glands Nerve supply:
The main branch of the nerve follows the course of the blood vessels. The nerve fibres break into terminal plexus in the connective tissue. Nerve bundles with unmyelinated axons surrounded by cytoplasmic process of Schwann cells supply the blood vessels, myoepithelial cells, ductal cells and the secretory cells.
- The neural innervations follow two patterns, namely epilemmal and hypolemmal.
- In the epilemmal type, the axons remain in the connective tissue separated by the basement membrane.
- When these axons are close to the secretory cell, they lose their Schwann cell covering and the adjacent exoplasm contains many vesicles containing transmitter substances.
- When a nerve impulse passes through the axons neurotransmitters are released and diffuses 100–200 nm across the basement membrane and influences the secretory cell.
- In the hypolemmal type, axons penetrate the basement membrane and lose their Schwann cell covering. These nerve endings run close to the secretory cell at a distance of 10–20 nm from them.
Formation Of Saliva
- The nucleus of the cell instructs the cell to synthesize serous saliva. The messenger RNA carries the signal from the nucleus into the cytoplasm. The ribosomes on the rough endoplasmic reticulum contain nucleic acids.
- Under the direction of the messenger RNA, amino acids (preproteins) in proper sequence are synthesized by the ribosomes. A NH2 terminal extension of about 15–30 amino acids (signal sequence) is attached to the chain of amino acids.
- The amino acid chains along with the signal sequence emerge from the ribosomes. There are specific receptors on the membrane of the rough endoplasmic reticulum. The signal sequence binds to the receptors on the rough endoplasmic reticulum and crosses the membrane and enters the cisternal space of the rough endoplasmic reticulum.
- In the cisternal space of RER, signal peptidase (a proteolytic enzyme) digests the signal sequence amino acids.
- From the RER vesicle bud off and enter the cis face of the Golgi apparatus. Within the Golgi apparatus, glycosylation of the amino acids takes place.
- This glycosylation begins in the RER and ends in the Golgi apparatus. Asparagine, serine, proteins, galactose, mannose, fructose glucosamine, galactosamine and sialic acid, phosphates and sulphates are added.
- In the trans face, the material is packed into vacuoles of various sizes and density and is known as immature granules, presecretory granules or condensing vacuoles. The granules have a light fluorescent content. They become concentrated as it is being transported and are packaged and called secondary granules.
- These granules bud off into the apical cytoplasm and are now called zymogen granules. The zymogen granules fuse with the apical plasma membrane. The apical plasma membrane ruptures and contents of the zymogen granules are discharged into the lumen of the acini.
- This process is called exocytosis. During exocytosis, there is no loss of the plasma membrane.
- When the stimulation for saliva secretion is increased, these granules form a string in the cytoplasm and release their content into the preceding granules in order to secrete saliva into the lumen rapidly. This is known as compound exocytosis.
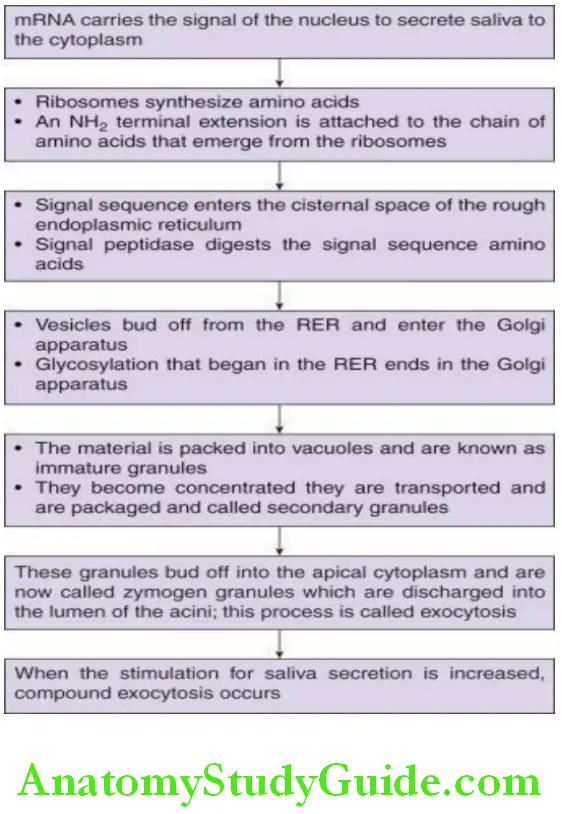
A similar process takes place in the mucous acini except that more amount of carbohydrates are added in the Golgi apparatus. The process of drainage of the mucous content is known as the apocrine process. In this process, at times, the apical plasma membrane is also released into the lumen. Later, that part of the apical plasma membrane is reconstructed. This is known as apocrine secretion.
Acini Salivary Gland
Control Of Salivary Secretion
- Formation of the salivary macromolecules, water and electrolytes is controlled by the autonomic nervous system. The neurotransmitters released from the vesicles in the nerve endings adjacent to the acini and the ducts stimulate them to discharge their products and secrete water and electrolytes. The neurotransmitters interact with specific receptors on the acinar cells.
- Stimulation of the adrenergic, cholinergic and substance P receptors increases the permeability of calcium into the cell. There are rapid changes in the membrane phospholipid metabolism that results in the release of calcium from intracellular stores such as endoplasmic reticulum or the plasma membrane. The increased calcium levels in the cytoplasm causes an efflux of potassium ions.
- Protein stimulation is mediated through the adrenergic receptor. Stimulation of the adrenergic receptors activates the plasma membrane receptor adenylate cyclase. This enzyme catalyses the formation of 3–5′ cyclic adenosine monophosphate from adenosine triphosphate.
- The increased concentration of cyclic adenosine monophosphate activates cyclic AMP-dependent kinase, an enzyme that phosphorylates other proteins that are involved in the process of exocytosis.
- Cyclic adenosine monophosphate can also stimulate the release of calcium from cytoplasmic organelles. Hence, calcium ions are a common intracellular mediator for all the receptors.
- β-Adrenergic (sympathetic) stimulation: Protein secretion
- α-Adrenergic and cholinergic: Water and electrolytes formation
Factors that affect salivary secretion:
- Minimum at birth; salivary amylase is absent
- Volume increases by 2–3 months and salivary amylase appears
- Old age: secretory reserves are decreased but constituents are stable
- Secretion: 0.1 mL/min to 4.0 mL/min when stimulated
Saliva
- Amount of saliva secreted: 1–1.5 L/day, 10–200 µL/min/gland
- pH 6.7–7.4
- Mixed saliva: Serous, mucous and mixed secretions
- Rate of wound healing is faster because of the presence of epidermal growth factor in saliva
Constituents of saliva
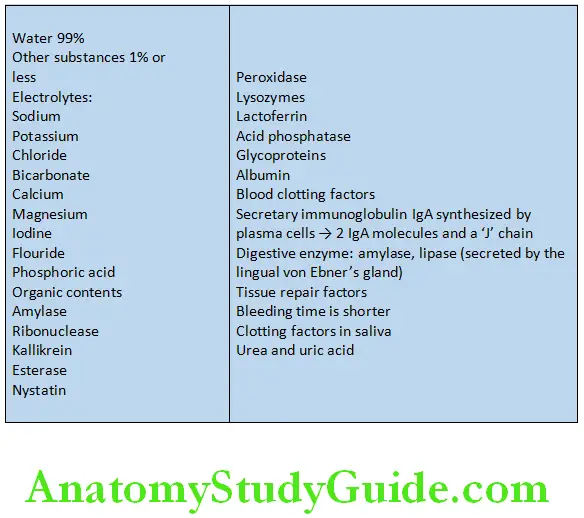
The composition of the saliva that is secreted by the major salivary glands differs from each other.
- Parotid gland: Watery saliva, rich in amylase, protein-rich proteins and glycoprotein
- Submandibular gland: Mucin-rich saliva
- Sublingual gland: Viscous saliva rich in proteins
Whole saliva:
- The secretions of the major and minor salivary glands, desquamated epithelial cells, microbes and their products white blood cells, serum constituents, gingival crevicular fluid, food remnants put together is called whole saliva.
Mixed saliva:
- The stimulated saliva is also called mixed saliva.
Saliva Volume:
- 750–1000 mL/day
- 60% – submandibular glands
- 30% – parotid glands
- Less than 5% – sublingual glands
- Approximately 1% – minor salivary glands
Saliva Resting flow rate:
- Whole saliva: 0.2–0.4 mL/min
- Parotid gland: 0.4 mL/min
- Submandibular gland: 0.1 mL/min
Factors that affect composition of saliva:
- Time of secretion
- Rate of flow
- Contribution from the different glands
- Circadian rhythm
- Duration and nature of the stimulus
Functions Of Saliva
1. Saliva Digestion:
- It helps in the formation the bolus.
- Helps in solubility of food and taste by providing a fluid environment by the action of digestive enzymes.
- For example, α-amylase; it breaks the α-1–4 glycoside links.
- Lingual lipase helps in digestion of dietary lipids.
2 Saliva Protective Function:
- Prevents the desiccation of the soft tissues in the oral cavity due to continuous secretion of the oral cavity.
- It helps in flushing of the debris and non-adherent bacteria
- Lubrication of the oral, oropharyngeal and oesophageal mucosa by mucin and other glycoproteins.
- Lowers the temperature and protects from chemical and thermal insults; dilutes oral acids and protects the mucosa.
- The buffering action is primarily due to bicarbonates and phosphates.
- Urea and ammonia due to the metabolism of salivary proteins and peptides decreases the pH and thus increases the acidity. Thus, the pH is maintained.
- Acquired enamel pellicle is formed on the tooth surface by the salivary glycoproteins. This reduced the solubility and promotes the remineralization of the enamel. Increase in the concentration of calcium and phosphates on the surface of a tooth increases the surface hardness of enamel and the resistance to decalcification.
- Antibacterial properties: Lysozymes produced by the acinar cells help in hydrolysing the cell wall of the bacteria leading to lysis of the cell. Peroxidase thiocyanate is converted to hypothiocyanite with the help of hydrogen peroxide hypothiocyanite which lysis of the polysaccharide bacterial cell wall.
- Uric acid and ascorbic acid secreted by the parotid gland decreases oxidant stress and maintains the integrity of the epithelium.
- Immunoglobulins:
- Predominantly IgA
- IgG and IgM are also secreted
- Secretory IgA, which comprises of two IgA chains and a J chain, act as a mucosal paint and has the capacity to clump or agglutinate microorganisms.
- They inhibit the adherence of the microorganisms to the oral tissues.
- Lactoferrin binds to iron and thereby iron is not available for bacterial metabolism.
3. Saliva Tissue Repair Factors:
- The bleeding time of oral wounds is much shorter and the clotting time is much faster. The rate of wound healing is faster because of the presence of epidermal growth factor in saliva that is secreted by the submandibular salivary glands.
4. Saliva Speech:
- Saliva helps in speech as it keeps the tissues in the oral cavity moist and lubricated.
5. Saliva Mastication and deglutition:
- Saliva helps in digestion by making the food moist and braking it down into smaller particles.
- Saliva decreases the temperature of the food and also helps in bolus formation.
6. Saliva Taste:
- Aids in the perception of taste as it contains protein called gustin that is necessary for the growth and maturation of the taste buds.
7. Saliva Excretion:
- Saliva is not usually not lost to metabolism but is reabsorbed in the GIT. Few substances from blood enter saliva and hence saliva can be aroute for excretion.
Clinical Considerations
Age changes:
- Replacement of the parenchymal tissue by fatty tissue
- Resting flow rate is less in older individuals but the quantity and composition in healthy older individuals is in younger adults.
Xerostomia:
- Decrease in the secretion of saliva is known as xerostomia.
- Some of the causes are Sjögren syndrome, side effect of chemotherapy, or radiation, medications such as anticholinergic drugs, antihypertensives, antipsychotic, drugs used in the treatment of Parkinsonism.
- It leads to difficulty in mastication, swallowing, speech.
- Increased susceptibility to caries, oral infections, ulcers of the oral mucosa, increased incidence of periodontal disease and candida infections.
Sialorrhoea/Ptyalism:
- Excessive secretion of saliva
Mucocoele and ranula:
- The damage or severance of the ducts of the sublingual and minor salivary glands leads to extravasation of the mucous in the soft tissues. The persistence of this extravasation leads to a mucocoele.
- Mucocoele of a sublingual gland is called a ranula.
- The ranula may elevate the tongue
- It may be painless
- It may produce a swelling
- Treatment: Surgical intervention
Nicotinic stomatitis:
- Hyperkeratinization around the opening of the duct of the minor salivary glands due to heat from the tobacco combustion in smokers.
- This is due to inflammation of the ductal openings which are seen as red macules in a white background on the mucosa of the palate.
Enlargement of the parotid gland:
The causes include
Starvation
- Alcoholism
- Pregnancy
- Diabetes mellitus
- Liver disease
- Protein deficiency
Sialoliths:
- Sialoliths may be the cause for the blockage in the main collecting duct of major salivary glands.
Diagnostic Uses of Saliva:
‘Saliva lacks the drama of blood, the sincerity of sweat and the emotional appeal of tears – Yet, it is a useful diagnostic fluid’.
- Developmental defects of salivary gland are very rare.
- Benign and malignant tumours such as pleomorphic adenoma, adenolymphoma, adenoid cystic carcinoma and mucoepidermoid carcinoma arise in the salivary gland.
- Saliva is an important source to provide information on metabolism and drug clearance.
- Saliva is a diagnostic tool for monitoring systemic disease.
- Useful for assessing the caries activity status of an individual.
- Hormone levels may be monitored.
- Estimation of the electrolyte levels may help in diagnosis of salivary gland or systemic diseases.
Salivary Gland Synopsis
- Salivary glands are exocrine glands situated in the orofacial region. Their chief function is the synthesis, storage and secretion of saliva.
- The major salivary glands are parotid, submandibular and sublingual salivary glands.
- The minor salivary glands are the labial and buccal glands, glossopalatine glands, palatine glands, lingual glands and von Ebner’s glands.
- Acini are the basic functional and terminal secretory units of a salivary gland and are made up of epithelial secretory cells, i.e. serous and the mucous cells.
- The ducts of the parotid, submandibular and sublingual glands are Stensen’s, Wharton’s and Bartholin’s ducts, respectively.
- The acini of the parotid glands are serous are spherical in shape with a narrow central lumen.
- The serous cells have a granular appearance in routine haematoxylin and eosin–stained sections.
- Mucous cells are also specialized cells that can synthesize, store and secrete salivary products.
- The secretions from these cells are mucinous. The mucous acini are elliptical in shape and larger than the serous acini.
- The acini are pale as the secretions do not take up routine stains.
In mixed salivary gland acini, both serous and mucous cells are present.
- The myoepithelial cells are epithelial cells with smooth muscle-like function and closely related to the secretory and intercalated duct cells.
- Myoepithelial cells are considered to have contractile function, helping to expel the secretions form the lumina of the secretory units and ducts.
- The acini are connected with hollow tubes and then to ducts which progressively grow larger from the inner to the outer portion of the salivary gland.
- Each duct is lined by a different type of cell based on the location in the gland.
- Ducts also play a role in the production and the modification of saliva.
- The length and type of the ducts also varies with the type of glands.
- Intercalated ducts are the smallest and the most distal of ducts and connects the lumen of the acini to the striated duct.
- The striated ducts are the largest among the intralobular ducts. They collect saliva from the intercalated and carry it into the excretory ducts.
- The intralobular ducts formed by the joining of striated ducts enlarge and are surrounded by layers of connective tissue.
- These ducts then become large and non-striated to become the excretory ducts which are interlobular. They transport saliva from the secretary units to the oral cavity.
- Formation of the salivary macromolecules, water and electrolytes is controlled by the autonomic nervous system.
Age, duration, and nature of stimulus can also affect the rate of formation of saliva.
- Amount of saliva secreted is 1–1.5 L/day, 10–200 µL/min/gland. The pH is 6.7–7.Rate of wound healing is faster because of the presence of epidermal growth factor in saliva.
- The composition of saliva secreted by major salivary glands differs from each other.
- Parotid gland: Watery saliva, rich in amylase, protein rich proteins and glycoprotein.
- Submandibular gland: Mucin-rich saliva.
- Sublingual gland: Viscous saliva rich in proteins.
- The secretions of the major and minor salivary glands, desquamated epithelial cells, microbes and their products white blood cells, serum constituents, gingival crevicular fluid, food remnants put together is called whole saliva. The functions of saliva are digestion, protective, tissue repair, speech, taste and excretion.
Leave a Reply