Shock And Haemorrhage
Shock Definition
Shock is defined as an acute failure of the circulatory system to supply blood in sufficient quantities or under sufficient pressure to the tissues. It is a syndrome characterised by hypoperfusion and severe dysfunction of vital organs.
Table of Contents
Shock Pathophysiology:
- Whenever there is hypoperfusion due to any reason, the body tries to compensate by releasing massive amounts of catecholamines (fight or flight response).
- This causes progressive vasoconstriction of cutaneous, muscular and visceral circulation in an attempt to preserve blood flow to the vital organs, the heart, brain and the kidneys. The heart rate increases resulting in an increase in cardiac output.
- Thus, in most cases, tachycardia is the earliest sign of shock. The peripheral vascular resistance also increases due to the catecholamine release which in turn causes the diastolic blood pressure to rise and helps to maintain organ perfusion.
- These compensatory mechanisms are effective in the early stages and are limited. In later stages, other vasoactive hormones such as histamine, bradykinin, β endorphins and other cytokines are also released.
- The hypoperfusion results in deprivation of oxygen and essential substrates at the cellular level causing a shift to anaerobic metabolism and development of lactic acidosis. With prolongation of shock, there is inadequate ATP production and the cells begin to lose their normal integrity.
- The electrical gradient across the cell membrane gets lost, the cell swells up eventually causing cellular death.
Read And Learn More: Basic Principles Of Surgery Notes
Types of Shock:
- Hypovolaemic shock: Loss of fluids or blood (haemorrhagic shock)
- Cardiogenic shock
- Distributive shock: Septic shock, anaphylactic shock, neurogenic shock
- Obstructive shock: Tension pneumothorax, cardiac tamponade, massive pulmonary embolism
Shock Clinical Features:
- Fast and feeble pulse, cold and clammy peripheries, and reduced urine output are prominent features of a person in shock.
- Depending on the stage of shock, the patient may be lethargic, confused, restless, delirious or even unconscious. The patient may develop tachypnea as a response to hypoxia (due to hypoperfusion of tissues) and lactic acidosis.
- The patient can show features specific to the cause of shock (bleeding in haemorrhagic shock, myocardial infarction in cardiogenic shock). Severe shock may progress to cardiac arrest.
Diagnosis Shock :
- Shock is mainly diagnosed by the clinical features. The patient will manifest with hypotension, tachycardia, tachypnea, obtundation or abnormal mental status, cold, clammy extremities, mottled skin, oliguria, metabolic acidosis, and hyperlactatemia.
- History and physical examination will lead to the diagnosis of shock and the cause of shock. Arterial blood gas showing a base deficit or high lactate values can reliably help in the diagnosis of shock.
General Principles of Resuscitation:
- The diagnosis and treatment of shock is always concurrent and treatment at any point must not be delayed due to any ongoing test/investigation for a good outcome.
- Monitoring should include clinical examination as well as a pulse oximeter, noninvasive blood pressure and electrocardiogram.
The basic management principle is to ensure better perfusion and oxygen delivery to the tissues. Assess ABC (airway, breathing and circulation).
- Assess airway: A patient in shock could be obtunded or even unconscious. Secure airway, if the patient is unable to maintain his airway. Give oxygen.
- Assess breathing: If the patient is apnoeic or is tachypneic and is not maintaining adequate gas exchange, one may need to initiate mechanical ventilation.
- Assess circulation: Circulation is inadequate in shock. The priority of resuscitation is to restore perfusion. Obtain two large bore peripheral intravenous access (18 or 16 G). Begin resuscitation with rapid infusion of 500 ml to a litre of Ringer lactate or isotonic saline.
Continue resuscitation with intravenous fluids, blood products or both as necessary and appropriate for the cause of shock to restore perfusion.
- In haemorrhagic shock, after the initial litre of intravenous fluid, packed cell volume, fresh frozen plasma and platelets will be needed to replace lost blood volume.
- Type-specific blood is preferred but in an emergency, O–ve packed cells can be given. If the facility is available, it is wiser to activate massive transfusion protocol (MTP) for more appropriate usage of blood products.
- A patient in hypovolaemic shock due to loss of fluids (as in severe diarrhoea) will require fluid replacement but may not need blood products to be transfused.
- Timely resuscitation in the initial phases includes infusion of appropriate quantity of isotonic electrolyte solutions and blood.
- Definitive control of haemorrhage and restoration of adequate circulating volume are the primary goals of management in haemorrhagic shock.
- A patient in septic shock and anaphylactic shock will also require intravenous fluids. However, a patient in cardiogenic shock will require infusion of vasopressors and inotropes.
- They are often given diuretics to prevent or treat pulmonary congestion. A patient in obstructive shock will need urgent relief of this obstruction.
- This can be done easily for tension pneumothorax (needle thoracostomy) and for cardiac tamponade (pericardiocentesis). However, it is more difficult to treat massive pulmonary embolism.
Shock End-points of Resuscitation:
- The initial end-points of resuscitation (to be achieved within a few hours) are a heart rate of < 100/min, blood pressure of 90/60 mmHg and oxygen saturation of 93–95%.
- As perfusion improves, one must aim for normalising homeostasis. The final end-point of resuscitation is a normal base deficit (eliminate metabolic acidosis). This should be achieved within 12–24 hours of admission.
Shock Specific Treatment:
Specific treatment for different types of shock depends on the cause and is given in the appropriate section.
Haemorrhage Classification
1. Depending on Nature of the Vessel Involved:
- Arterial haemorrhage: The blood jets out and is bright red in colour. Pulsation of the artery may be seen. It can be easily controlled, as it is visible.
- Venous haemorrhage: The blood does not jet out but oozes. It is dark red in colour. It is non-pulsatile, and difficult to control because the vein gets retracted.
- Capillary haemorrhage: The blood does not jet out but oozes out slowly. The blood is red in colour. It becomes significant, if there are bleeding tendencies.
2. Depending on the Timing of Haemorrhage:
- Primary haemorrhage: This occurs at the time of surgery.
- Reactionary haemorrhage: This occurs within 6–12 hours of surgery. The usual causes are hypertension in the postoperative period, violent sneezing, coughing, or retching. For example, the superior thyroid artery may bleed after thyroidectomy, if the ligature slips; hence, it is better to ligate it twice.
- Secondary haemorrhage: This occurs within 5–7 days of surgery. It is due to infection which eats away the suture material, causing sloughing of vessel wall (e.g. bleeding within 5–7 days of surgery for haemorrhoids).
3. Depending on the Duration of Haemorrhage:
- Acute haemorrhage: This occurs suddenly (e.g. oesophageal variceal bleeding due to portal hypertension).
- Chronic haemorrhage: This occurs over a period of time (e.g. haemorrhoids/piles, chronic duodenal ulcer, tuberculous ulcer of the ileum, diverticular disease of the colon).
4. Depending on the Nature of Bleeding:
- External haemorrhage/revealed haemorrhage (e.g. epistaxis, haematemesis).
- Internal haemorrhage/concealed haemorrhage (e.g. splenic rupture following injury, ruptured ectopic gestation, liver laceration following injury).
Clinical Notes:
- A patient who had undergone subtotal thyroidectomy for toxic goitre was shifted to the postoperative intensive care unit. Within 10 minutes, the nurse came to inform the surgeon that 450 ml of blood was collected in the ‘Redivac’ suction bottle.
- The dressing was opened and there was no large collection of blood in the surgical wound. The presence of a large haematoma was thus ruled out. The blood pressure (BP), which was previously under control, had shot up to 210/110 mmHg postoperatively, possibly due to pain.
- Careful monitoring and treatment reduced the BP to 140/90 mmHg. After 24 hours, the drainage was only 100 ml. The incision did not need re-exploration. This case illustrates reactionary haemorrhage due to hypertension.
Pathophysiology Of Haemorrhagic Shock
A loss of >30–40% blood volume results in a fall in blood pressure, and gross hypoperfusion of the tissues and vital organs, leading to haemorrhagic shock. Haemorrhagic shock can be classified as follows (American College of Surgeons) depending on the amount of blood lost and clinical features:
Classification of Haemorrhagic Shock:
Class 1:
- When blood loss is <750 ml (<15% of blood volume), it can be called mild haemorrhage. 60–70% of blood volume is present in the lowpressure venous system (capacitance vessels). 10% of the blood volume is present in the splanchnic circulation.
- When there is blood loss, peripheral venoconstriction takes place, which compensates for the loss of blood volume by shifting some blood into the central circulation. Some amount of blood volume correction also occurs due to withdrawal of fluid from the interstitial spaces.
- Apart from mild tachycardia and thirst, there may be no other symptoms or signs suggesting hypovolaemia. The blood pressure, urine output, and mentation are all normal.
Class 2:
- Loss of 750–1500 ml (15–30% of blood volume) results in moderate shock.
- Peripheral venoconstriction may not be sufficient to maintain circulation. Hence, adrenaline and noradrenaline (endogenous catecholamines) released from the sympathoadrenal system cause powerful vasoconstriction of both arteries and veins.
- Increased secretion of ADH causes retention of water and salt. Thirst increases.
- Clinically, the patient shows a heart rate of 100–120 beats/minute and an elevated diastolic pressure. The systolic pressure may remain normal.
- Urine output is reduced to about 0.5 ml/kg/h and the capillary refill time is more than the normal 2 seconds. Extremities may look pale and the patient is confused and thirsty.
Class 3:
- Loss of 1500–2000 ml (30–40% of blood volume) produces Class III shock. All the signs and symptoms seen in Class II haemorrhagic shock get worse.
- The patient’s systolic and diastolic blood pressures fall and the heart rate increases to around 120 beats/ minute. The pulse is thready.
- The respiratory rate increases to > 20/minute. Urine output drops to 10–20 ml/hour. The patient appears pale and is aggressive, drowsy, or confused.
Class 4:
- A blood loss of >2000 ml (>40% of blood volume) results in Class 4 shock. The peripheries are cold and ashen.
- The pulse is thready and >120/minute. The blood pressures are very low or unrecordable.
- The patient may be moribund.
- If persistent, other organs may get damaged:
- Mucosal ulcerations, upper GI bleeding, absorption of bacteria and toxins, bacterial translocation, and bacteraemia
- Liver: Reduced clearance of toxins
- Kidney: Acute renal failure
- Heart: Myocardial ischaemia, depression
- Lungs: Loss of surfactant, increased alveolocapillary permeability, interstitial oedema, and increased arteriovenous shunting result in acute lung injury (ALI).
- Multiorgan failure consequent to haemorrhagic shock is associated with a high mortality rate.
- Early diagnosis of bleeding and appropriate management is crucial to improve survival and outcome.
Management Of Haemorrhagic Shock
1. Treatment—General Measures:
- Hospitalisation
- A patient in haemorrhagic shock needs immediate resuscitation to prevent or minimise damage to the vital organs and tissues. Resuscitation and control of haemorrhage should happen simultaneously.
- O-M-IV: First, provide oxygen, attach a monitor to record vitals (heart rate, blood pressure, respiratory rate, and oxygen saturation) and obtain two large bore intravenous access.
- Remember O-M-IV for all critically ill patients: O for oxygen, M for monitor, and IV for intravenous access. Blood sample for investigations, blood grouping, and cross-matching should be sent at this stage.
- Care of all critically ill patients begins with A (airway), B (breathing), and C (circulation).
- Airway and breathing: Oxygen should be administered by face mask to all patients who are in shock, but are conscious and are able to maintain their airway. If unconscious, endotracheal intubation and ventilation with oxygen may be necessary.
Haemorrhagic Shock Circulation:
- Haemorrhage control (see below)
- Resuscitation and haemorrhage control must happen simultaneously.
- Two large peripheral lines (18 or 16 G) are preferred for initial resuscitation. Intravenous fluids, preferably at 40–42°C (crystalloids—Ringer lactate, or plasmalyte) are infused rapidly to restore volume.
- Send blood samples for investigations, blood grouping, and cross-matching.
- Dextrose-containing solutions are not recommended. Infusion of large amounts of isotonic saline may cause hyperchloraemic acidosis and is not recommended.
- Insertion of central lines is not recommended (unless done by skilled personnel), as it takes much longer to insert, requires expertise, and may be associated with complications.
- External jugular venous access is another option for quick transfusion of large amounts of fluids and blood products.
- If peripheral intravenous access is not available, an intraosseous needle may be inserted to infuse fluids into the bone marrow. All infusions that can be given intravenously can also be given intraosseously.
Haemorrhagic Shock Intraosseous Cannulation:
The bone marrow of long bones is in direct communication with the vascular tree and hence, anything injected into the bone marrow will reach circulation. Thus, when intravenous access is not available and access to the circulation is required in an emergency as in major trauma, burns, circulatory arrest, intraosseous needles can provide rapid and life-saving access to the circulation. This is most often performed in children but can be done in adults also in emergency circumstances.
- Contraindications: Fracture of the long bone being punctured, previous puncture of the same bone either at the same site or another site on the same bone, infection at the site, burn at entry site and inability to locate landmarks.
- Sites: Intraosseous puncture is most commonly made at the upper end of tibia, one finger-breadth below the tibial tuberosity on the medial surface. The other sites are lower end of femur, lower end of radius, manubrium sternum, iliac bone and the calcaneus.
- Needle: A large bore needle is required. A bone marrow aspiration needle with a guide such as Jamshidi needle is best suited for this procedure. Several others such as Sur-Fast intraosseous needle, Sussmane-Raszynski needle or the EZ-IO can be used. If these are not available, any large bore needle with stylet can be used for this purpose.

- Procedure: The limb to be used must be stabilized using a pillow or roll. Under aseptic precautions, the skin over the puncture site is anaesthetized using 2 ml of local anaesthetic.
- The bone is held steady with the nondominant hand and the needle held in the palm of the dominant hand such that the needle, wrist and elbow are in the same straight line.
- The bone is punctured with a rotatory movement through the skin and then the bone. Loss of resistance indicates entry of the needle into the marrow. Care must be taken not to penetrate the opposite surface of the bone.
- The operator must be careful and not place his hand in the needle path. The marrow may or may not be aspirated from the needle. A 10 ml syringe containing saline is connected to the needle. If the saline can be injected freely and without any extravasation, an infusion of saline or Ringer lactate can be commenced through the needle.
- A free flow of this solution may be obtained but may need to be injected, if there is resistance. Anything that can be given intravenously can also be given by the intraosseous route.
- Care must be taken to check the correct position of the needle. Puncture of the opposite surface of the bone must be avoided to prevent leakage of fluid through that hole into the tissues. The limb must be observed closely for any swelling due to extravasation.
- An intravenous access must be secured as soon as possible and the intraosseous line removed. Generally, an intraosseous line is removed in a few hours’ time but it can be used up to 48 hours.
- Complications: Infections at the site of insertion such as cellulitis, osteomyelitis can occur due to poor aseptic technique. Extravasation of fluid and compartment syndrome can occur, if not carefully watched. Fracture of the bone can also occur if excessive force is applied during insertion.
- The American College of Surgeons classification of haemorrhagic shock (as given above) may be used as a quick guide to gauge the amount of blood loss. If the patient is tachycardic (heart rate >120/min) and hypotensive (systolic blood pressure is <90 mmHg), the patient has Class III shock or higher and has lost >30–40% blood volume.
- Remember that the numbers given above are a rough guide. The actual clinical presentation may change with comorbid illnesses, other injuries, or concurrent medications.
- If infusion of 1–2 litres (in an adult) of Ringer lactate has not been successful in returning the vitals to normal values, the patient may have lost a large amount of blood and may be having ongoing bleeding. Such patients require transfusion of blood products (packed cells and fresh frozen plasma).
- It may be necessary to activate massive transfusion protocol (when available at the hospital), if the patient is bleeding profusely. Replacing the lost volume and controlling haemorrhage is important to restore perfusion and prevent tissue damage.
- Most blood banks do not issue whole blood (as it is uneconomical for a scarce commodity), and provide component therapy. In an actively bleeding patient who is in hypovolaemic shock, the ratio of packed cells : fresh frozen plasma : platelets would be 1:1:1.
- Generally, typed and cross-matched blood is given. However, if the shock is severe and the patient is in Class IV shock, O –ve blood may be given as a lifesaving measure. Subsequently, cross-matching needs to be done before giving type-specific blood.
- In cases where the haemostasis is not yet achieved, volume infusion should be controlled to maintain systolic BP at 80–90 mmHg till the bleeding can be stopped. This is called ‘hypotensive fluid resuscitation’ or ‘permissive hypotension’.
- Use of a fibrinolytic agent like tranexamic acid 1 g stat and then 8th hourly is advised to reduce bleeding.
- Once bleeding is controlled, infuse sufficient volume to allow blood pressure to reach normal levels as soon as possible (first phase of resuscitation).
- The second phase of resuscitation involves continuation of fluid therapy to ensure the base deficit is eliminated. This is important to ensure that the microcirculation is normal. This should happen within 12–24 hours (the earlier, the better).
- All through the resuscitation, it is important to maintain patient’s body temperature (by using warm air blowers, keep him covered). Hypothermia impairs coagulation, increases bleeding, depresses respiration and circulation, and increases the chances of infection.
- Use of inotropes and vasoconstrictors is not indicated, as they may harm tissue perfusion.
- However, if inotropes have been started as a lifesaving measure, an attempt should be made to wean them as soon as the volume status is corrected and the patient is stable.
2. Treatment—Specific Measures:
Control Haemorrhage:
1. Pressure and packing:
- This is the method of choice to stop bleeding when the bleeding site is accessible.
- Packing using roller gauze with or without adrenaline to control bleeding from the nose and scalp.
- Pressure packing the middle thyroid vein during thyroidectomy and the lumbar veins during lumbar sympathectomy.
- A Sengstaken tube is used to control bleeding from oesophageal varices—internal tamponade.
2. Position and rest:
- Elevation of the leg controls bleeding from varicose veins.
- Elevation of the head-end reduces venous bleeding in thyroidectomy—anti-Trendelenburg position.
- Sedation to relieve anxiety—midazolam in titrated doses of 1–2 mg intravenously may be given. This may help control blood pressure and the consequent bleeding.
3. Tourniquets:
Indications:
- Reduction of fractures
- Repair of tendons
- Repair of nerves
- When a bloodless field is desired during surgery
Contraindications: Patient with peripheral vascular disease. (The arterial disease may be aggravated due to thrombosis resulting in gangrene.)
Tourniquets Types:
- Pneumatic cuffs with a pressure gauge
- Rubber bandage
Tourniquets Precautions:
- Too loose a tourniquet does not serve the purpose.
- Too tight: Arterial thrombosis may occur, which may result in gangrene.
- Too long (duration of application): Gangrene of the limb.
Application of a tourniquet to control bleeding is not advised unless pressure bandaging has not been helpful because of possible ischaemia of the limb. Hence, if applied, the time of application must be noted down. Deflate as soon as possible within 45–60 minutes.
Tourniquets Complications:
- Ischaemia and gangrene
- Tourniquet nerve palsy1
Surgical methods to control haemorrhage:
- Application of artery forceps (Spencer Wells forceps) to control bleeding from veins, arteries and capillaries.
- Application of ligatures for bleeding vessels.
- Cauterisation (diathermy).
- Application of bone wax (Horsley’s wax, which is bee’s wax in almond oil) to control bleeding from cut edges of bones.
- Silver clips are used to control bleeding from cerebral vessels (Cushing’s clip).
- Surgical procedure: Laparotomy and splenectomy for splenic rupture, hysterectomy for uncontrollable postpartum haemorrhage, laparotomy for control of bleeding from ruptured ectopic pregnancy.
Hypovolaemic Shock
- Loss of blood—haemorrhagic shock
- Loss of plasma—as in burns shock
- Loss of fluid—dehydration as in gastroenteritis
Hypovolaemic Shock Features:
- The primary problem is a decrease in preload. The decreased preload causes a decrease in stroke volume. Clinical features depend on the degree of hypovolaemia and are similar to those of haemorrhagic shock.
- Severe (Class 3or 4) shock results in tachycardia, low blood pressure, and decreased urine output. The peripheries are cold and the patient may be confused or moribund (see Pathophysiology of haemorrhagic shock).
Hypovolaemic Shock Treatment:
- Replace the lost blood volume.
- The primary goal is to restore tissue perfusion and oxygenation as early as possible.
- Crystalloids: If crystalloids are used to replace blood loss, 1.5–2 times the lost volume need to be given. Ringer lactate is the crystalloid of choice.
- Large volumes of saline infusion may cause hyperchloraemic metabolic acidosis. 5% dextrose is not used to expand the intravascular volume, as it is hypotonic once dextrose metabolises.
- Colloids: When colloids are used to replace lost blood volume, a volume equal to the lost volume may be given. However, they are not preferred.
Hypovolaemic Shock:

- Crystalloids are preferred during the initial phase of resuscitation. If a large volume of blood is lost, transfuse blood products. Please refer to the management of hamorrhagic shock described earlier in this chapter.
Cardiogenic Shock
The blood flow is reduced because of an intrinsic problem in the heart muscle or its valves. A massive myocardial infarction may damage the cardiac muscle so that there is not much healthy muscle to pump blood effectively. Any damage (especially acute) to the valves may also reduce the forward cardiac output, resulting in cardiogenic shock.
Cardiogenic Shock Features:
- The primary problem is a decrease in contractility of the heart. The decreased contractility causes a decrease in stroke volume.
- Left ventricular pressures rise as forward cardiac output reduces. The sympathetic nervous system is activated, resulting in increased systemic vascular resistance.
- Clinically, the patient presents with tachycardia, low blood pressure, and decreased urine output.
- The jugular venous pulse may be raised, and an S3 or S4 gallop may be present.
- The lung fields may show bilateral extensive crepitations due to pulmonary oedema.
- The peripheries are cold, and the patient may be confused or moribund.
Cardiogenic Shock Treatment:
- The primary goal is to improve cardiac muscle function.
- Oxygenation can be improved by administering oxygen, either by a face mask or by endotracheal intubation and ventilation as necessary.
- Inotropes improve cardiac muscle contractility.
- Vasodilators such as nitroglycerine may dilate the coronary arteries and peripheral vessels, and improve tissue perfusion. Lowering systemic vascular resistance reduces impedance to forward cardiac output (afterload). However, the patient must be monitored closely to avoid excessive reductions in blood pressure.
- Intra-aortic balloon pump or ventricular assist devices may be used to augment cardiac output.
- If hypotension continues to be refractory, revascularisation (surgical or interventional) or valve replacement may be considered on an emergency basis.
Distributive Shock
In distributive shock, the afterload is excessively reduced, thereby affecting circulation. Distributive shock may occur in the following situations:
- Septic shock
- Anaphylactic shock
- Neurogenic shock
- Acute adrenal insufficiency
1. Septic Shock:
Septic shock Pathophysiology:
- Sepsis is the response of the host to bacteraemia/ endotoxaemia.
- It may be produced by gram-negative or gram-positive bacteria, viruses, fungi, or even protozoal infections.
- Severe sepsis may result in persistent hypotension despite adequate fluid resuscitation.
- Local inflammation and substances (especially endotoxin) released from organisms activate neutrophils, monocytes, and tissue macrophages.
- This results in a cascade of proinflammatory and anti-inflammatory cytokines and other mediators, such as IL-1, IL-8, IL-10, TNF-α, prostaglandin E1, endogenous corticosteroids, and catecholamines.
- This results in cellular chemotaxis, endothelial injury, and activation of the coagulation cascade.
Septic shock Features:
- These substances produce low systemic vascular resistance (peripheral vasodilatation) and ventricular dysfunction, resulting in persistent hypotension.
- Generalised tissue hypoperfusion may persist despite adequate fluid resuscitation and improvement in cardiac output and blood pressures. This is due to abnormalities in regional and microcirculatory blood flow. These abnormalities may lead to cellular dysfunction, lactic acidosis (anaerobic metabolism), and ultimately, multiorgan failure.
- Early phases of septic shock may produce evidence of volume depletion, such as dry mucous membranes and cool, clammy skin.
Disturbance of Procoagulant–Anticoagulant Balance:
-
- Inflammatory response in sepsis activates tissue factor which in turn activates coagulation
- Fibrinogen is converted to fibrin
- Lowered levels of natural anticoagulants such as protein C, protein S and antithrombin III Procoagulant—anticoagulant imbalance → diffuse microvascular thrombi
- After resuscitation with fluids, however, the clinical picture is typically more consistent with that of hyperdynamic shock. Features include tachycardia, bounding pulses with a widened pulse pressure, a hyperdynamic precordium on palpation, and warm extremities.
- Signs of possible infection depend on the source of sepsis. These may include fever, localised erythema or tenderness, consolidation on chest examination, abdominal tenderness, guarding, rigidity, and meningismus.
- Signs of end-organ hypoperfusion include tachypnoea, cyanosis, mottling of the skin, digital ischaemia, oliguria, abdominal tenderness, and altered mental status.
- Often, a definitive diagnosis cannot be made on the basis of initial clinical features; hence, empirical treatment for several possible conditions should be commenced.
Septic shock Treatment:
- Removal of the septic focus is an essential step and is a priority in the treatment of septic shock (example resection of gangrenous bowels, closure of perforation, appendicectomy).
- Early empirical antibiotic therapy should be administered to treat the precipitating infection. This must be given within the first hour of arrival.
- Supportive care: Oxygenation and, if necessary, endotracheal intubation and mechanical ventilation should be administered.
- Intravenous fluids: Restoration of intravascular filling pressures must be done using crystalloids, colloids, and blood as necessary.
- Crystalloids, such as isotonic saline or Ringer’s lactate, may be used. Large amount may be required, which may contribute to tissue oedema. Colloids restore intravascular volume faster and remain longer in the central circulation.
- However, they are expensive and often used in patients with a high-risk of pulmonary oedema (due to cardiac dysfunction) who may not tolerate large volume of fluids.
- Avoid hetastarch, as it may increase the risk of renal injury and mortality. If the patient is anaemic, blood transfusions may be required to raise haemoglobin levels to 8–10 g%.
- Vasoactive agents, such as norepinephrine, may be used to produce vasoconstriction and raise the systemic vascular resistance to normal. Dopamine, dobutamine, or adrenaline may need to be added. Vasopressin infusion may be useful in patients with refractory shock. All these potent drugs are given as infusions under careful and continuous monitoring of blood pressure, as well as cardiac filling pressures (central venous pressures).
Summary of Septic Shock:
- Early diagnosis of septic shock
- Empirical antibiotics initially
- Appropriate antibiotics after culture and sensitivity testing
- Ultrasonography, CT scan, and chest X-ray are key investigations
- Treatment of source of infection
- Pneumonia
- Drainage of pus
- Closure of perforation
- Resection of gangrene
- Early and aggressive resuscitation, supportive care and close monitoring in intensive care unit (ICU).
Clinical Notes:
- A 54-year-old lady was admitted to the casualty with low blood pressure and dyspnoea since one day. She had a history of fever, vomiting, and diarrhoea since 3–4 days, and was treated in a local nursing home. When she got worse, was referred to our hospital. In spite of fluid therapy, profound hypotension persisted, and within half an hour of arrival to the casualty, she suffered a cardiopulmonary arrest.
- Her trachea was immediately intubated, cardiopulmonary resuscitation (CPR) was given, and she was shifted to the intensive care unit for further management. She required high doses of dopamine, adrenaline, and noradrenaline to maintain blood pressure. A blood gas analysis showed severe metabolic acidosis (pH = 7.02, PaCO 2 = 35 mmHg, and HCO3– = 12 mmol/L).
- Considering the history, a diagnosis of septic shock was made when she continued to have hypotension even after her central venous pressures were normal. Peritoneal dialysis was done, as she was in oliguric renal failure. Haemodialysis was not possible, as she was hypotensive and on inotropes. A search for a septic focus was initiated. Ultrasound abdomen showed a dilated kidney and an obstructed urinary system.
- A DJ-stenting of the ureter, which was done to relieve the obstruction, drained pus. Once the pus was drained, appropriate antibiotics were given, and with continued cardiorespiratory support, she showed steady improvement. She was gradually weaned off the ventilator and inotropes, and was discharged from the hospital five weeks later. At discharge, she was fully conscious, stable, ambulant, and very grateful to the medical fraternity.
- This case illustrates the importance of resuscitation, cardiorespiratory support, removal of the septic focus, and antibiotics in the treatment of septic shock.
2. Anaphylactic Shock:
Anaphylactic Shock Features:
It occurs on exposure to an allergen that the patient is sensitive to. It may be pollen, foodstuffs, preservatives in the food, or a medication. Anaphylactic shock that occurs in the hospital is usually due to some drug allergy (e.g. to penicillin). Latex allergy is also being increasingly recognised.
The reaction may be in the form of mild rashes, with or without bronchospasm, or a full blown anaphylactic shock, wherein the patient presents with rashes, generalised oedema (including laryngeal oedema), bronchospasm and hypotension, and if not treated in time, cardiac arrest.
Anaphylactic Shock Treatment:
1. Primary:
- Oxygen and, if necessary, endotracheal intubation
and ventilation. - Adrenaline, 0.5–1 mg IM or 50–100 µg IV boluses, as necessary, to maintain blood pressure.
- Intravenous fluids—isotonic saline or Ringer lactate
- Leg-end elevation of bed.
2. Secondary:
Chlorpheniramine maleate
Hydrocortisone 100 mg intravenously If facilities exist, take a 10 ml sample of blood to analyse for serum tryptase levels. If raised, it confirms anaphylactic reaction.
3. Neurogenic Shock:
Causes: High spinal cord injury, vasovagal shock.
Features: Hypotension without tachycardia (more often bradycardia) that may deteriorate to cause shock and cardiac arrest.
Treatment: Intravenous fluids, inotropes, and vagolytics, as necessary.
4. Acute Adrenal Insufficiency:
Risk Factors:
Adrenal crisis occurs, if the adrenal gland is deteriorating, as in:
Risk Factors for Adrenal Crisis:
-
- Infection
- Trauma or surgery
- Adrenal gland or pituitary gland injury
- Premature termination of treatment with steroids such as prednisolone or hydrocortisone.
- Primary adrenal insufficiency (Addison’s disease)
- Secondary adrenal insufficiency (pituitary gland
injury, compression) - Inadequately treated adrenal insufficiency.
Acute Adrenal Insufficiency Features:
- Headache, profound weakness, fatigue, slow and lethargic movement, joint pain.
- Nausea, vomiting, abdominal pain, high fever and chills.
- Low blood pressure, dehydration, rapid heart and respiratory rates, confusion or coma.
Acute Adrenal Insufficiency Treatment:
- Care of airway, breathing, and circulation
- Intravenous fluids
- Hydrocortisone 100 mg intravenously every 6 h to provide mineralocorticoid activity
- Treat the precipitating factor
- Antibiotics as necessary
Obstructive Shock
In obstructive shock, there is impedance to either inflow or outflow of blood into or out of the heart. It may be due to cardiac tamponade or due to tension pneumothorax.
Cardiac Tamponade:
In cardiac tamponade, the pericardium is filled with blood or fluid, which hampers venous filling as well as outflow. Therefore, the cardiac output reduces drastically, even to zero. It is a medical emergency. Prompt recognition and treatment can save lives.
Cardiac Tamponade Causes:
- Injury to the heart due to trauma
- Perforation of vena cava or atrial walls during cannulation or intracardiac procedures
- Rupture of ventricular or aortic aneurysm
- Postoperatively after cardiac surgery
Pericarditis can lead to accumulation of fluid in the pericardial sac. This pericardial effusion tends to occur more slowly but can produce cardiac tamponade when there is large amount of fluid accumulation. It can be due to infections (bacterial or fungal), inflammatory causes (uraemia, systemic lupus erythematosus, rheumatoid arthritis), cancer or certain medications.
Cardiac Tamponade Features:
- The filling pressures of the left-sided and right-sided chambers equalise.
- Beck’s triad: Low blood pressure, muffled heart sounds and distended neck veins.
- The patients also have pulsus paradoxus where there is at least a 10% decrease in systolic blood pressure with inspiration.
- This can lead to cardiac arrest.
Cardiac Tamponade Treatment:
- This is a life-threatening condition and must be treated immediately, especially when acute.
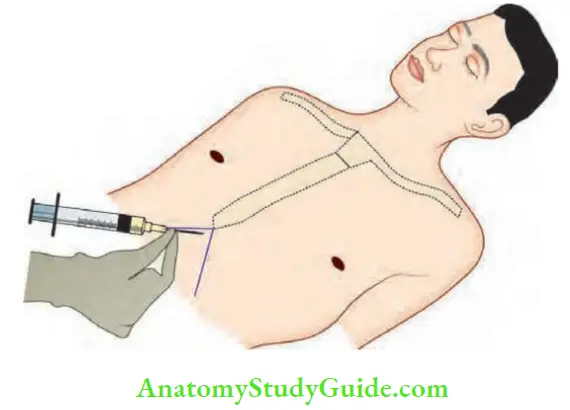
- Pericardiocentesis: Drain the pericardial cavity using a wide bore needle, attached to a syringe. It is inserted from the subcostal area, under the xiphoid process, pointing towards the left shoulder with continuous aspiration (Fig. 17.2). Use of ultrasound to perform this procedure under vision improves safety and is recommended.
- Decompression of the pericardial cavity allows venous filling of the heart and forward flow. Blood pressure improves immediately.
- Monitor electrocardiogram during this procedure. Watch for arrhythmias that can occur, if the needle stimulates the myocardium.
Tension Pneumothorax:
Tension Pneumothorax Causes:
- Lung injury due to trauma
- Ventilator-induced barotrauma
- Rupture of emphysematous bullae in a patient with chronic obstructive pulmonary disease.
Tension Pneumothorax Features:
- Profound cyanosis, distended neck veins
- Tachypnoea, dyspnoea, or respiratory arrest
- No air entry on the side of pneumothorax, hyperresonance to percussion
- Tachycardia, hypotension, and cardiac arrest
Tension Pneumothorax Treatment:
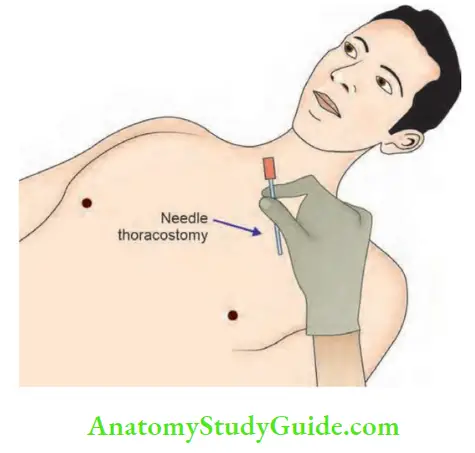
- A wide (large) bore needle/cannula (needle thoracostomy) must be inserted into the pleural cavity to drain the air. Traditionally, it was advised that the needle should be inserted in the midclavicular line in the 2nd intercostal space on the affected side.
- However, in adults diagnosed to have a tension pneumothorax, the current Advanced Trauma Life Support (ATLS) guidelines advise that the needle is inserted in the 5th intercostal space in the midaxillary line.
- This is followed by tube thoracostomy.
Indicators Of Fluid Responsiveness
Measurement of Cvp Has Been Used Traditionally As An Indicator Of Fluid Responsiveness. The Newer Ones Include Pulse Pressure Variation, Systolic Pressure Variation, Stroke Volume Variation, Inferior Vena Caval Diameter And Passive Leg Raising.
Central Venous Pressure (Cvp)
- Pressure in the intrathoracic great veins is called central venous pressure.
- It is the same as right atrial pressure.
- Normal CVP is 2–6 mmHg in a person breathing spontaneously. It is higher (8–12 mmHg) in a patient who is receiving mechanical ventilation.
- CVP is used as a surrogate measure of blood volume. A low CVP suggests hypovolaemia.
- In shock, measurement of CVP is useful for planning proper fluid management.
- Thus, it is desirable to monitor CVP while treating patients in shock.
- However, it must be remembered that CVP may also be affected by contractility of the right ventricle, changes in intrathoracic and intrapericardial pressures.
- Thus, a high CVP does not always indicate hypervolaemia. In such situations, other means of fluid responsiveness such as pulse pressure variation or systolic pressure variation, measurement of inferior vena caval diameter can be used.
Tension Pneumothorax Method:
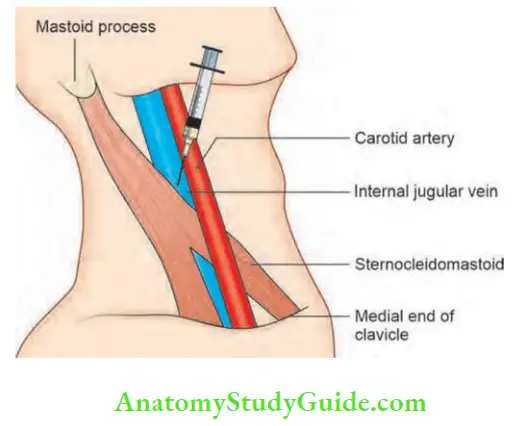
- The internal jugular vein (IJV) or subclavian vein are preferred routes of accessing the central veins.
- A 16-cm long IV catheter is introduced into the central vein with the patient supine, head down, and neck rotated to the opposite side.
- Head down position helps in engorging the vein. Ultrasound guidance to cannulation is now considered the standard of care.
- Seldinger’s technique is employed, and the catheter is advanced up to the junction of the superior vena cava and the right atrium (corresponding externally to the manubrium sterni).
- Aspirate through the lumen to check for free flow of blood into the connecting tube.
Access to Right Heart/Great Veins:
- Internal jugular vein
- Subclavian vein
- Median cubital vein
- External jugular vein
The tube is connected to an electronic pressure transducer. The ‘zero reference point’ must be at the midaxillary level, if the patient is in supine position, or at the manubriosternal joint if he is in the semireclining position (45°).
If the facility for using an electronic transducer is not available, a saline manometer may be used.
CVP must be measured at end-expiration when the influence of intrathoracic pressure on CVP is minimum.
Tension Pneumothorax Uses:
- If CVP is low, venous return should be supplemented by IV infusion, as in cases of hypovolaemic shock.
- When CVP is high, further infusion of fluids may result in pulmonary oedema.
- In cardiogenic shock, CVP may be normal or high, and it is affected by the reduced ventricular contractility. In such situations, therefore, it may not accurately reflect intravascular volume.
Tension Pneumothorax Complications:
- Pneumothorax
- Accidental carotid artery puncture
- Haematoma in the neck
- Bleeding
- Air embolism
- Infection
Dynamic indicators of fluid responsiveness: Such as stroke volume variation, systolic pressure variation and pulse pressure variation measure the changes in stroke volume, systolic pressure or pulse pressure respectively with changes in intrathoracic pressure.
- A variation more than 10–13% indicates fluid responsiveness (the patient’s haemodynamic parameters will respond to volume infusion). This parameter is useful when patients are being mechanically ventilated with a tidal volume of at least 8 ml/kg body weight.
Inferior vena cava diameter: This is a noninvasive method of measurement of fluid responsiveness. It is measured using ultrasound at a point where it enters the right atrium.
- Using M mode, the maximum and minimum diameter are measured. If the IVC diameter is <10 mm, the patient requires volume and if >25 mm, the patient is reasonably full. A variability >25% in IVC diameter with respiration (IVC collapsibility index) also indicates fluid responsiveness.
Passive leg raising: By about 30° will result in increased venous return. An improvement in haemodynamics with this reversible manoeuvre suggests need for volume replacement.
Photographs Of Patients With Septic Shock







Multiple Choice Questions
Questions 1. Which of the following medications is least preferred in the initial management of haemorrhagic shock?
- Oxygen
- Ringer lactate
- Packed cells
- Vasopressors
Answer: 4. Vasopressors
Questions 2. Which of the following solutions is best suited in the initial management of hypovolaemic shock?
- Normal saline
- Ringer lactate
- Hydroxyethyl starch
- Albumin
Answer: 2. Ringer lactate
Questions 3. Characteristic features of septic shock include the following e x c e p t:
- Hypotension
- Tachycardia
- Oliguria
- Alkalosis
Answer: 4. Alkalosis
Questions 4. Hyperbaric oxygen is helpful in the following conditions e x c e p t:
- Carbon monoxide poisoning
- Gas gangrene
- Decompression sickness
- Before chemotherapy
Answer: 1. Carbon monoxide poisoning
Questions 5. Regarding central venous pressure:
- Right internal jugular vein is the route of choice
- CVP is a reliable indicator of blood volume status
- CVP remains constant with respiration
- CVP is low in tension pneumothorax
Answer: 2. CVP is a reliable indicator of blood volume status
Questions 6. The following is NOT a feature of cardiac tamponade:
- Tachycardia
- Hypertension
- Muffled heart sounds
- High CVP
Answer: 2. Hypertension
Questions 7. Which of the following is a good indicator of fluid responsiveness in a spontaneously breathing patient:
- Stroke volume variation
- Inferior vena caval diameter
- Systolic blood pressure
- Heart rate
Answer: 2. Inferior vena caval diameter
Questions 8. During haemorrhage, if the systolic blood pressure is normal but diastolic blood pressure is high, the patient may be in Class ______ shock.
- 1
- 2
- 3
- 4
Answer: 2. 2
Questions 9. In haemorrhagic shock, if the patient has lost 30–40% blood volume, he is in Class ______ shock.
- 1
- 2
- 3
- 4
Answer: 3. 3
Questions 10. Tension pneumothorax is a reason for which of the following types of shock?
- Hypovolaemic shock
- Obstructive shock
- Distributive shock
- Septic shock
Answer: 2. Obstructive shock
Questions 11. The drug of choice in anaphylactic shock is:
- Adrenaline
- Histamine
- Promethazine
- Chlorpheniramine
Answer: 1. Adrenaline
Questions 12. The ‘zero reference point’ for arterial pressure transducers in seated patients should be at the:
- Level of the nipple
- Level of the manubriosternal junction
- Level of the xiphoid process
- Level of the radial artery
Answer: 2. Level of the manubriosternal junction
Questions 13. The central venous pressure is high in which type of shock?
- Hypovolaemic shock
- Anaphylactic shock
- Septic shock
- Obstructive shock
Answer: 4. Obstructive shock
Questions 14. Translocation of bacteria from which organ may lead to multiorgan failure (and thus, this organ is called ‘motor of multiorgan failure’)?
- Kidney
- Brain
- Gut
- Liver
Answer: 3. Gut
Questions 15. The route of choice for administering adrenaline in anaphylactic shock is:
- Intramuscular
- Intravenous
- Subcutaneous
- Inhalational
Answer: 2. Intravenous
Questions 16. Which is the blood product of choice in bleeding patients with a fibrinogen concentration of <100 mg/L?
- Packed cells
- Fresh-frozen plasma
- Platelets
- Cryoprecipitate
Answer: 4. Cryoprecipitate
Questions 17. Beck’s triad is a feature of:
- Cardiac tamponade
- Tension pneumothorax
- Pulmonary thromboembolism
- Massive myocardial infarction
Answer: 1. Cardiac tamponade
Questions 18. The following is NOT a feature of tension pneumothorax:
- Reduced breath sounds
- Dullness on percussion
- Low blood pressure
- Hypoxia
Answer: 2. Dullness on percussion
Questions 19. Intra-aortic balloon pump is used in which type of shock:
- Hypovolaemic shock
- Obstructive shock
- Cardiogenic shock
- Septic shock
Answer: 3. Cardiogenic shock
Your comment is awaiting moderation.
Uniswap