Tissue Fluid And Edema Definition
Tissue fluid is the medium in which cells are bathed. It is otherwise known as interstitial fluid. It forms about 20% of ECF.
Table of Contents
Functions Of Tissue Fluid
- Because of the capillary membrane, there is no direct contact between blood and cells. And, the tissue fluid acts as a medium for the exchange of various substances between the cells and the blood in the capillary loop.
- Oxygen and nutritive substances diffuse from the arterial end of the capillary through the tissue fluid and reach the cells. Carbon dioxide and waste materials diffuse from the cells into the venous end of capillary through this fluid.
Read And Learn More: Medical Physiology Notes
Formation Of Tissue Fluid
Formation of tissue fluid involves two processes:
- Filtration
- Reabsorption
1. Filtration
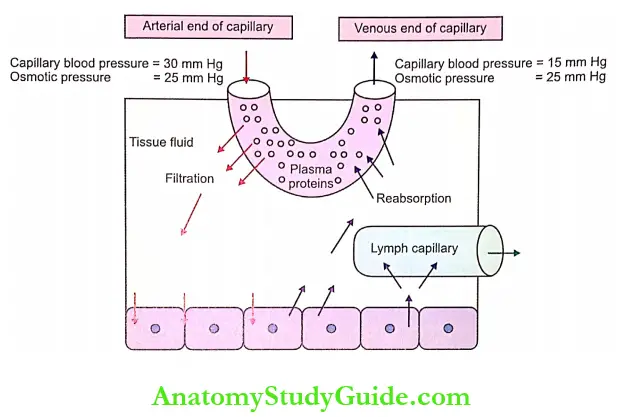
- Tissue fluid is formed by the process of filtration. Normally, the blood pressure (also called hydrostatic pressure) in arterial end of the capillary is about 30 mm Hg.
- This hydrostatic pressure is the driving force for the filtration of water and other substances from blood into tissue spaces. Along the course of the capillary, the pressure fails gradually and, it is about 15 mm Hg at the venous end.
- The capillary membrane is not permeable to large molecules, particularly plasma proteins. So, these proteins remain in the blood and exert a pressure called oncotic pressure or colloidal osmotic pressure. It is about 25 mm Hg.
- The osmotic pressure is constant throughout the circulatory system and it is an opposing force for the filtration of water and other materials from capillary blood into the tissue space.
- However, the hydrostatic pressure in the arterial end of the capillary (30 mm Hg) is greater than the osmotic pressure. And, the net filtration pressure of 5 mm Hg is responsible for continuous filtration.
Starling’s Hypothesis: The determination of net filtration pressure is based on Starling’s hypothesis. Starling’s hypothesis states that the net filtration through capillary membrane is proportional to the hydrostatic pressure difference across the membrane minus the oncotic pressure difference. These pressures are called Starling’s forces.
2. Reabsorption
- The fluid filtered at the arterial end of capillaries is reabsorbed back into the blood at the venous end of capillaries. Here also, the pressure gradient plays an important role.
- At the venous end of capillaries, the hydrostatic pressure is less (15 mm Hg) and the oncotic pressure is more (25 mm Hg).
- Due to the pressure gradient of 10 mm Hg, the fluid is reabsorbed along with waste materials from the tissue fluid into the capillaries. About 10% of filtered fluid enters the lymphatic vessels.
- Thus, the process of filtration at the arterial end of the capillaries helps in the formation of tissue fluids and the process of reabsorption at the venous end helps to maintain the volume of tissue fluid.
Applied Physiology Edema
Applied Physiology Edema Definition
- Edema is defined as swelling caused by excessive accumulation of fluid in tissues. It may be generalized or local. Edema that involves the entire body is called generalized edema.
- Local edema is the one that occurs is specific areas of the body such as the abdomen, lungs and exteriors like feet, ankles, and legs. The accumulator. of fluid may be inside or outside the cell.
Types Of Edema: Edema is classified into two types depending upon the body fluid compartment where the accumulation of excess fluid occurs:
- Intracellular edema
- Extracellular edema.
1. Intracellular Edema: Intracellular edema is the accumulation of fluid inside the cell. It occurs because of three reasons:
- Malnutrition
- Poor metabolism
- Inflammation of the tissues.
- Edema due to Malnutrition
- Malnutrition occurs because of poor intake of food or poor circulatory system through which the nutritive substances are supplied.
- Due to the lack of nutrition, the ionic pumps of the cell membrane are depressed leading to poor exchange of ions. Especially, the sodium ions leaking into the cells cannot be pumped out.
- Excess sodium inside the cells causes endosmosis resulting in intracellular edema.
- Edema due to Poor Metabolism: Poor metabolism is caused by poor blood supply. Poor blood supply leads to lack of oxygen. It results in poor function of cell membrane and edema as explained above.
- Edema due to Inflammation of Tissues: During inflammation of the tissues, usually the permeability of cell membrane increases. This causes the movement of many ions including sodium into the cells resulting in endosmosis and intracellular edema.
Extracellular Edema: Extracellular edema is defined as the accumulation of fluid outside the cell. It occurs because of two reasons:
- Abnormal leakage of fluid from capillaries into interstitial space
- Obstruction of lymphatics that leads to prevention of fluid return from interstitial fluid back into blood.
The common conditions which lead to extracellular edema are:
- Heart failure
- Renal disease
- Decreased amount of plasma proteins
- Lymphatic obstruction
- Increased endothelial permeability.
- Edema due to Heart Failure: Edema occurs in heart failure because of various reasons such as:
- Failure of heart to pump blood: Failure of the heart to pump blood from veins to arteries causes an increase in venous pressure and capillary pressure.
- This leads to increased capillary permeability and leakage of fluid from blood into interstitial fluid causing extracellular edema.
- Fall in blood pressure during heart failure: It decreases the glomerular filtration rate in the kidneys. So, the amount of sodium and water excreted by kidneys decreases resulting in sodium and water retention.
- Because of this, the volume of blood and body fluid increases. This in turn increases the capillary hydrostatic pressure. These two factors together can increase the accumulation of fluid causing extracellular edema.
- Low blood supply to kidneys during heart failure: It increases renin secretion which in turn increases the secretion of aldosterone.
- Aldosterone increases the reabsorption of sodium and water from renal tubules into ECF resulting in development of extracellular edema.
- Pulmonary Edema
- Pulmonary edema is the accumulation of fluid in pulmonary interstitium. In left heart failure, the blood is easily pumped into pulmonary circulation by right ventricle.
- However, the blood can not return from lungs to left side of the heart because of weakness of this side of the heart.
- This increases pulmonary vascular pressure leading to leakage of fluid from capillaries into the pulmonary interstitium. It causes pulmonary edema which can be life-threatening.
- Edema due to Renal Diseases – Generalized Edema
- In renal disease, the kidneys fail to excrete electrolytes particularly sodium and water which leads to retention of water and electrolytes.
- Because of this, the fluid leaks from blood into interstitial space causing extracellular edema. Initially, the edema develops in the legs, but later it progresses to the entire body (generalized edema).
- Edema due to Decreased Amount of Plasma Proteins
- When the amount of plasma proteins decreases, the collagen osmotic pressure decreases. Because of this, the permeability of the capillary increases resulting in teased capillary filtration.
- So, more amount of water out of the capillary. It accumulates in the tissue space resulting in extracellular edema.
- The amount of plasma proteins decreases during the conditions like malnutrition, liver diseases, renal diseases, burns, and inflammation.
- Edema due to Lymphatic Obstruction – Lymphedema
- Lymphedema is the edema that is caused by lymphatic obstruction. It is common in filariasis.
- During this disease, the parasitic worms live in the lymphatics and obstruct the drainage of lymph. The accumulation of lymph along with cellular reactions leads to swelling that is very prominent in the legs and scrotum.
- The repeated obstruction of lymphatic drainage in these regions results in fibrosis and development of elephantiasis.
- Elephantiasis: Elephantiasis is a disorder of the lymphatic system characterized by the thickening of skin and extreme enlargement of the affected area most commonly limbs (legs), genitals, certain areas of the trunk, and parts of head.
- Edema due to Increased Endothelial Permeability: The permeability of the capillary endothelium increases in conditions like burns, inflammation, trauma, allergic reactions, and immunologic reactions which lead to oozing out of fluid. This fluid accumulates leading to the development of edema.
Pitting And Non-Pitting Edema
- Interstitial fluid is present in the form of a gel that is almost like a semisolid substance. It is because, the interstitial fluid is not present as fluid but is bound in a proteoglycan meshwork.
- It does not allow any free space for the fluid movement except for a diameter of about a few hundredths of a micron.
- Normal volume of interstitial fluid is 12 liters and it exerts a negative pressure of about 3 mm Hg. It applies a slight suction effect and holds the tissues together.
- However, in abnormal conditions, where, the interstitial fluid volume increases enormously, the pressure becomes positive. Most of the fluid becomes free fluid that is not bound to proteoglycan meshwork.
- It flows freely through tissue spaces, producing a swelling called edema. This type of edema is known as pitting edema because, when this area is pressed with the finger, displacement of fluid occurs producing a depression or pit.
- When the finger is removed, the pit remains for few seconds, sometimes as long as one minute, till the fluid flows back into that area.
- Edema also develops due to swelling of the cells or clotting of interstitial fluid in the presence of fibrinogen. This is called nonpitting edema because it is hard and a pit is not formed by pressing.
Leave a Reply