Clinical Examination Of Poisoning Case
Question 1. Enumerate the clinical features in general that would help you in diagnosing the poison ingested.
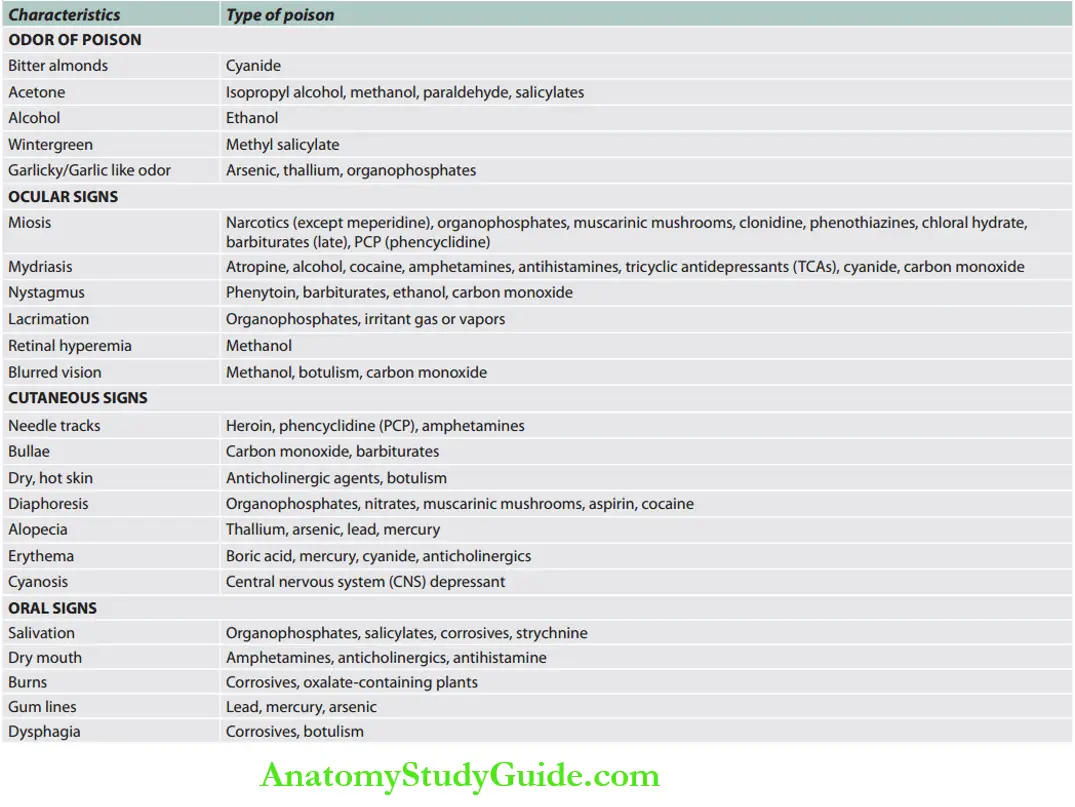
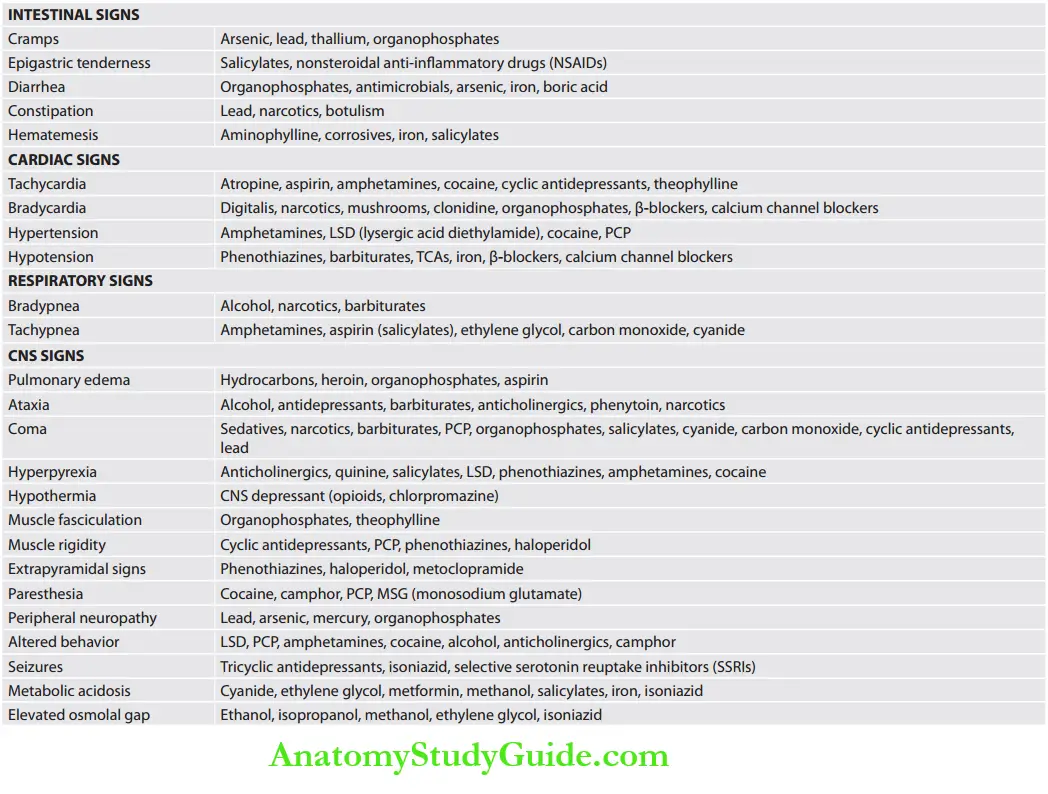
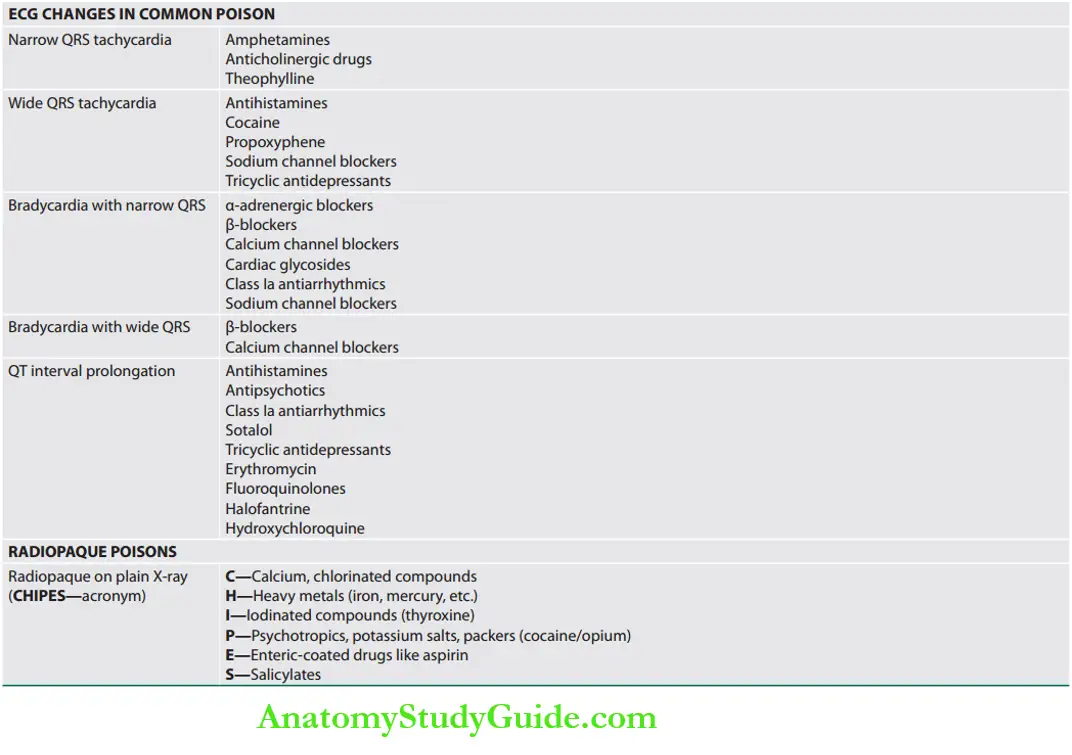
Answer: Accidental or intentional poisoning produces a wide range of symptoms and signs.
Table of Contents
Therefore, meticulous history and physical examination are of paramount importance in recognizing the poisoned patient.
Initial management should be focused on acute stabilization and supportive care till the correct substance is identified. Various parameters in clinical assessment determine the type of poisons.
Read And Learn More: General Medicine Question And Answers
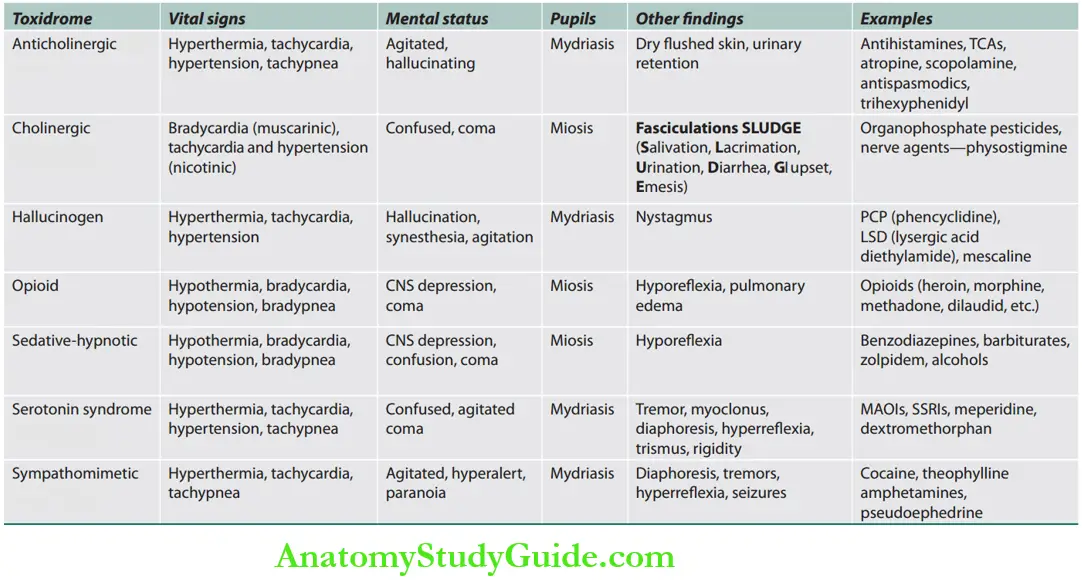
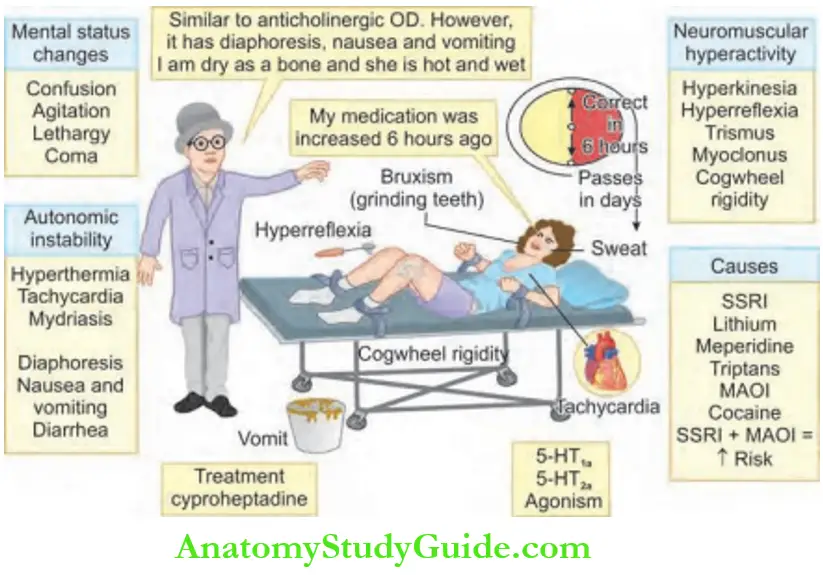
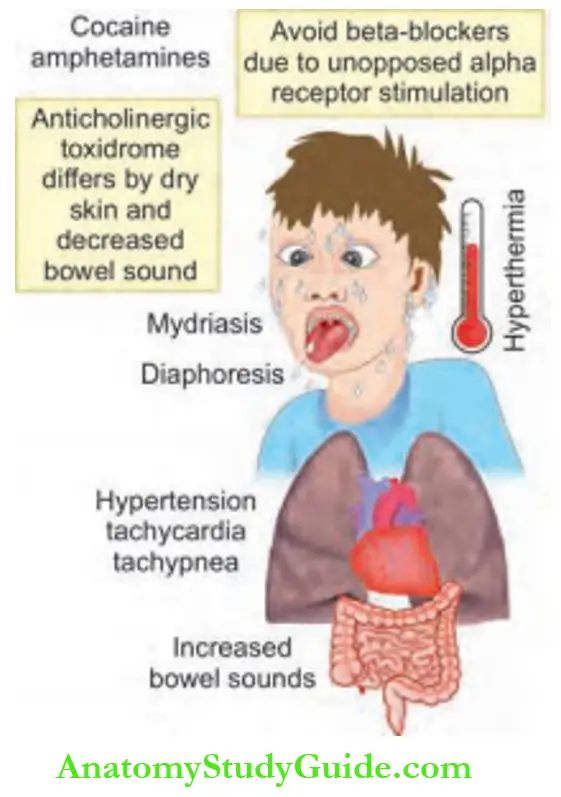
Toxidromes
Question 2. List the common toxidromes that are commonly encountered in clinical practice.
Answer: Based on history and clinical findings, it may be possible to define a syndrome associated with certain poisons. This is called toxidrome/toxic syndrome.
Management of Patients with Poisoning
Question 3. Describe the initial approach to the stabilization of the patient who presents with poisoning. (or) Describe basic methodologies in the treatment of poisoning: decontamination, supportive therapy, antidote therapy, and procedures of enhanced elimination.
Answer:
Management/Treatment
Management of Patients with Poisoning Goals of Treatment
Management of Patients with Poisoning These include:
- Support of vital signs,
- Diagnostic testing,
- Reduce absorption of the toxin,
- Enhance of poison elimination, and
- Neutralize toxin.
In the poisoned patient, diagnostic evaluation and therapeutic interventions often are initiated simultaneously.
1. Management of Patients with Poisoning Supportive Care
Patients who are seriously poisoned must receive early appropriate management.
The outcome depends on appropriate nursing and supportive care, and on appropriate treatment of complications.
Management of Patients with Poisoning The aims are:
To maintain physiologic homeostasis till poison is eliminated from the body and the patient resumes normal physiological functions.
As with any unstable or critically ill patient, the resuscitation [airway, breathing, circulation (ABC)] with basic life support takes priority.
To prevent and treat secondary complications: Supportive therapy for the central nervous system (e.g., cerebral edema), cardiopulmonary system (e.g., pulmonary edema, pneumonia), and renal system with proper care for coma, seizures, hypotension, bedsores, arrhythmias, sepsis, thromboembolic disease, coagulopathy, hypoxia, and acute renal failure.
2. Management of Patients with Poisoning Diagnostic testing
General tests
- Complete blood count
- Serum electrolytes, blood urea nitrogen (BUN), and creatinine
- Liver function test
- Arterial blood gas
- Electrocardiogram
- Urine pregnancy test in all women of childbearing age
- Radiographic studies—radiopaque poisons.
Management of Patients with Poisoning Specific tests
- Measurement of drug or toxin concentrations in body fluids (blood, urine, lavage fluid)
3. Reduce Absorption of the Toxin
- Inhalational exposure: Evacuation from the toxic environment and provision of supplemental oxygen.
- Dermal exposure: Removal of contaminated clothing and shower or irrigation of affected site (dust before shower for dry chemical).
- For eye exposure: Removal of chemicals by copious irrigation of the affected eye by up to 1 L of saline or symptomatic improvement occurs.
- Oral exposure: Inducing emesis, performing gastric lavage, activated charcoal, whole bowel irrigation, and cathartics.
Management of Patients with Poisoning Gastric decontamination
Emesis induction: Forced emesis, if the patient is awake (using saline, ipecac).
- Gastric lavage should be considered for life-threatening poisons that cannot be treated effectively with other therapies.
Time of lavage: Gastric lavage decreases absorption by 42% if done at 20 minutes and by 16% if performed at 60 minutes.
Method: Performed by first aspirating the stomach and then repetitively instilling and aspirating fluid. The choice of fluid is tap water— 5–10 mL/kg.
- Left lateral position better and delays spontaneous absorption.
Management of Patients with Poisoning Contraindication: Unprotected airway, comatose patients, corrosive poisoning, kerosene (hydrocarbons) poison, and patients with convulsions.
Complications of gastric lavage.
- Aspiration pneumonia
- Perforation of the esophagus
- Laryngospasm/hypoxia/tension pneumothorax
- Tachycardia and cardiac dysrhythmias
- Fluid and electrolyte imbalance — hypernatremia; water intoxication
Activated charcoal administration: 25–100 g activated charcoal mixed with water to form a slurry should be administered at a rate of not less than 12.5 g/h through a nasogastric tube.
- Multidose-activated charcoal at a rate of at least 12.5 g/h is useful in poisoning with carbamazepine, dapsone, phenobarbital, quinine, theophylline, and phenytoin.
- Fuller’s earth (2 g/kg in water; maximum 150 g in water) be given as soon as possible per oral or via a nasogastric tube.
- Cathartics: Sorbitol, magnesium citrate, magnesium sulfate, and sodium sulfate as cathartics for patients who have ingested materials that are absorbed slowly.
- Dilution—milk/other drinks: Advised only after the ingestion of corrosives (acids, alkali).
- Whole bowel irrigation: 1,500–2,000 mL/h through a nasogastric tube.
- It is performed by administering a bowel-cleansing solution containing electrolytes and polyethylene glycol by gastric tube.
- It may be used for potentially toxic ingestions of sustained-release or enteric-coated drugs or to remove illicit drugs.
- Contraindications are GI hemorrhage, ileus, and hemodynamic instability.
Endoscopic or surgical removal of ingested substances may be useful in rare situations (e.g., ingestion of a potentially toxic foreign body that fails to transit the gastrointestinal tract).
4. Management of Patients with Poisoning Enhance Poison Elimination
- Indications: Increased elimination is possible only if The drug is distributed predominantly in the ECF (extracellular fluid) and drugs that have a low protein binding.
- Methods: Keep a good urine output of 150–200 mL/h.
-
- Alkalinization of urine using sodium bicarbonate to produce urine with a pH ≥ 7.5: For salicylate, methotrexate, and phenobarbital poisoning.
Read And Learn More: General Medicine Question And Answers
Extracorporeal removal:
-
- Hemodialysis: For barbiturates, salicylates, acetaminophen, valproate, alcohols, and glycols.
- Hemoperfusion: For theophylline, digitalis, paraquat, and lipid-soluble drugs (aminoglycosides, vancomycin, and metal chelate complexes).
- Exchange transfusion: Useful in cases of massive hemolysis, severe methemoglobinemia, or sulfhemoglobinemia.
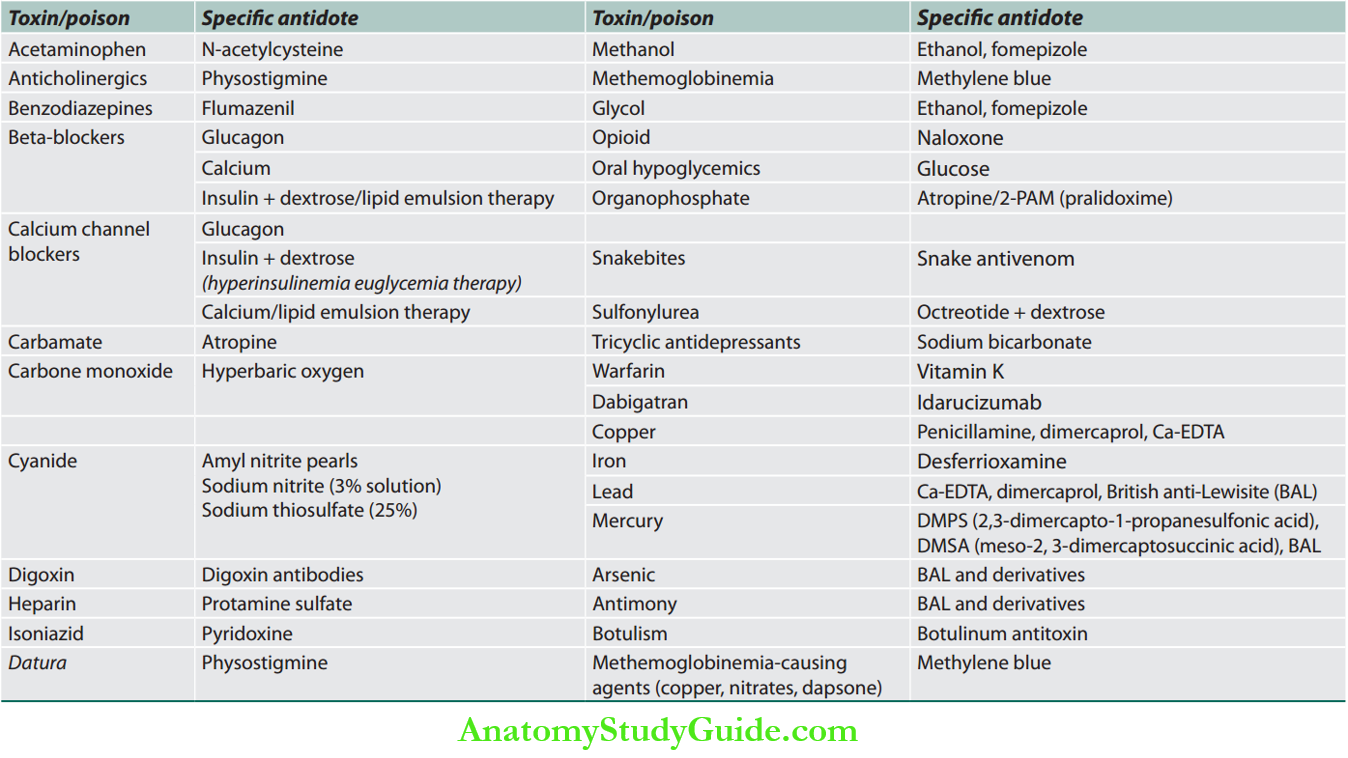
5. Management of Patients with Poisoning Neutralize Toxin
Antidotes may prevent absorption, bind and neutralize poisons directly, antagonize end-organ effects, or inhibit conversion to more toxic metabolites.
Question 4. Write a short note on an antidote.
Answer:
Neutralize toxins/poisons by toxin-specific antidotes.
Insecticide Poisoning
Question 5. Discuss the clinical manifestations, diagnosis, complications, and management of organophosphorus and carbamate poisoning.
Answer:
Organophosphate and Carbamate Poisoning
Organophosphorus (OP) compounds are widely used as pesticides in developing countries and are a common cause of poisoning.
Classification of Organophosphate and Carbamate.
Insecticide Poisoning Mode of intoxication: It may occur through ingestion, inhalation, or dermal absorption.
Classification of organophosphate and carbamate.
- Organophosphorus
- Diethyl organophosphorus: Quinalphos, chlorpyriphos, diazinon, triazophos, phorate, dimethoate, parathion-ethyl
- Dimethyl organophosphorus: Monocrotophos, dichlorvos, acephate, malathion, fenthion, methamidophos, and phosphamidon
- Carbamate: Methomyl
- Organochloride: Endosulfan, endrin
- Pyrethroids: Cypermethrin, alpha-cypermethrin, deltamethrin, cyhalothrin
- Neonicotinoid: Imidacloprid, acetamiprid
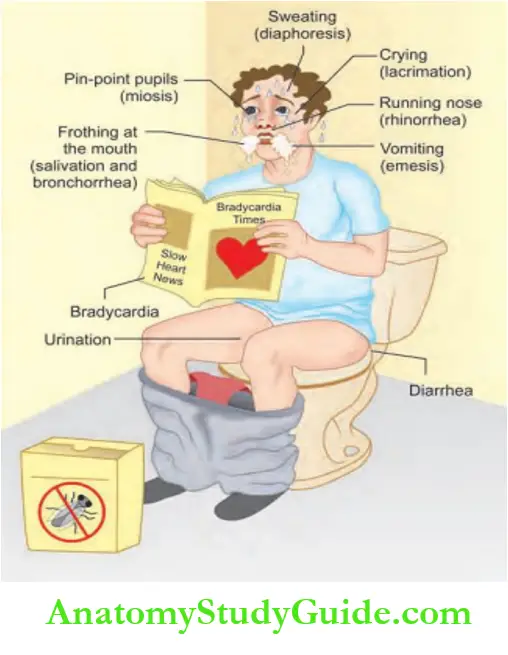
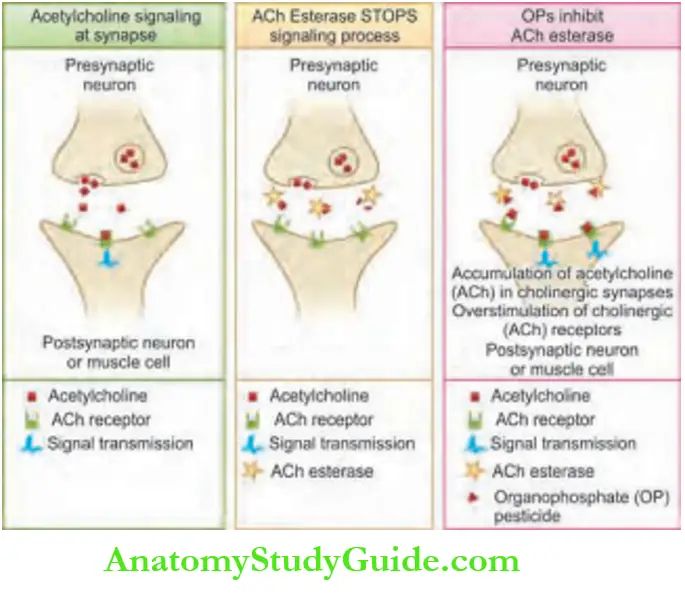
Insecticide Poisoning Mechanism of OP Toxicity.
- OP compounds irreversibly bind to the serine-OH group at the active site of acetylcholinesterase (AChE) and phosphorylate. This inactivates the enzyme AChE.
- It leads to the accumulation of acetylcholine (ACh) in cholinergic synapses.
- Spontaneous hydrolysis of the OP-enzyme complex allows the reactivation of the enzyme.
- However, the loss of a chemical group from the OP-enzyme complex prevents further enzyme reactivation, a process known as “aging”.
- Aging is characterized by the loss of alkyl group + the strengthening of covalent bonds.
- Phosphorylated AChE is very stable. Inhibition of enzyme activity → accumulation of ACh in the synapse and neuromuscular junction (NMJ).
- It causes overstimulation of cholinergic receptors. After aging has taken place; a new enzyme needs to be synthesized before function can be restored.
Clinical Course after Acute Poisoning
Question 6. Write a short essay/note on clinical signs of organophosphorus poisoning.
Answer:
Clinical Course after Acute Poisoning Triphasic Illness
1. Acute cholinergic syndrome
- Onset: Cholinergic symptoms within the first 24 hours.
- Features
- SLUDGE = Salivation, Lacrimation, Urination, Defecation, Gastric Emptying
- BBB = Bradycardia, Bronchorrhea, Bronchospasm
2. Intermediate syndrome
- Onset: 24–96 hours after poisoning, after the cholinergic phase settles, seen in 10–40% of cases.
- Mechanism: Excess Ach at NMJ causes downregulation of nicotinic receptors and muscles affected.
- Features: Characterized by proximal neck muscle weakness, decreased deep tendon reflexes (DTRs), cranial nerve abnormalities (bulbar), and respiratory insufficiency.
- Duration: Lasts for a few days to about 3 weeks
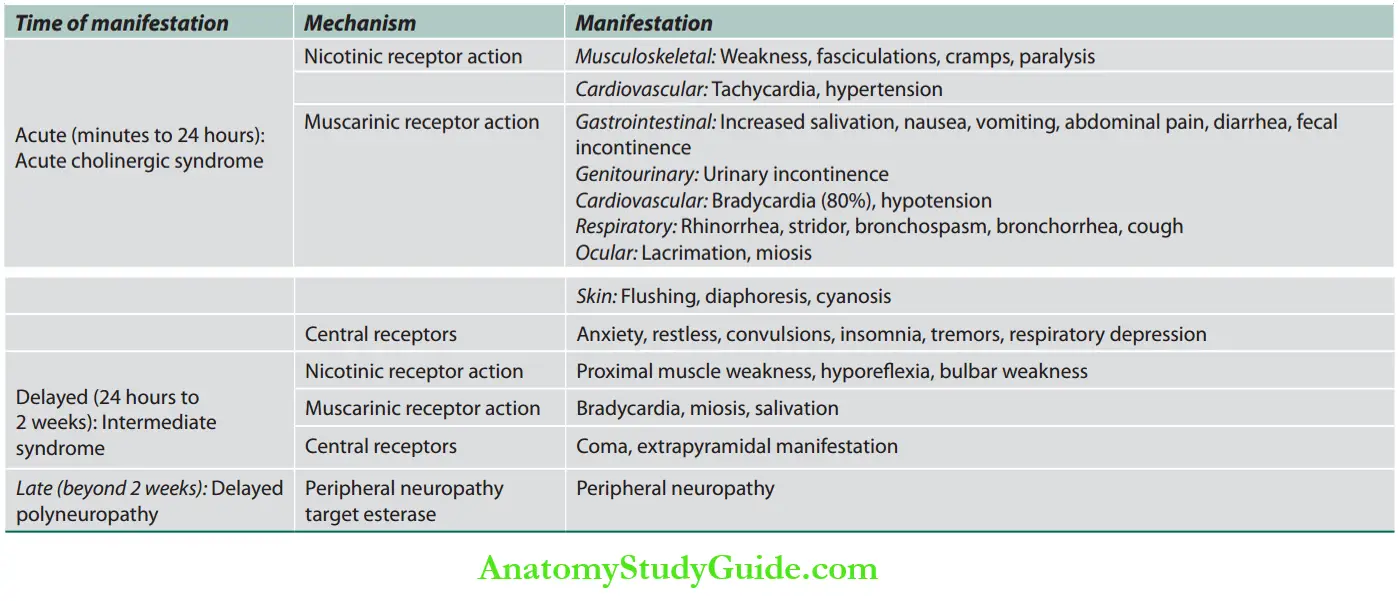
3. OP-induced delayed polyneuropathy (OPIDN)
- Onset: 1–3 weeks after acute exposure.
- Mechanism: Due to degeneration of long myelinated nerve fibers. Pure motor or sensor-motor.
- Features: Characterized by cramps in the legs, numbness and paresthesia in the distal upper and lower limbs, shuffling gait, foot and wrist drop.
- Other features are: wasting, DTR reduced/absent, and pyramidal tract signs absent.
Recovery is incomplete
Question 7. Discuss the management of organophosphorus poisoning.
Answer:
Diagnosis of Organophosphate Poisoning
- Clinical diagnosis:
- Dreisbach’s severity ofOP poisoning is presented
- Laboratory:
- Red cell cholinesterase
- Plasma [Pseudo, Butyryl (Bu)] cholinesterase
- Electrocardiogram (ECG): The most common ECG abnormality was
prolonged QTc and sinus tachycardia. - Arterial blood gas (ABG): Hypoxemia.
Management of Organophosphate
Acute Cholinergic Syndrome
Steps
- Assess and record the 15-point Glasgow Coma Scale (GCS).
- Measure pulse rate and blood pressure and auscultate the lungs.
- Make patients lie down in the left lateral position: With the head lower than the feet.
- Start oxygen.
- Intubate, if the patient has respiratory distress. Start atropine quickly to reduce bronchorrhea responsible for respiratory distress.
- Set up an infusion of 0.9% normal saline. Aim at systolic blood pressure >80 mm Hg and urine output >30 mL/h.
- Remove the contaminated clothes and thoroughly wash the skin with soap and water.
- Perform gastric decontamination with gastric lavage once the patient is stabilized and within 2 hours of ingestion.
- Skin exposure would require irrigation of the skin with copious amounts of water and liberal use of soap.
- Eye exposure should be irrigated with copious amounts of normal saline.
- Give activated charcoal (50 g in 200 mL) (Not much benefit due to rapid absorption of the poison into the blood).
Organophosphorus poisoning Drugs Used
1. Atropine
- Early use of sufficient doses of atropine is lifesaving in patients with severe toxicity. It reverses ACh-induced bronchospasm, bronchorrhea, bradycardia, and hypotension.
- When the diagnosis is uncertain:
- Atropine challenge test: To be performed, if not sure that the patient has consumed OP.
- Inject 0.6–1 mg IV atropine: If the pulse rate goes up by 25/minute or skin flushing develops, the patient has mild or no toxicity, or OP poisoning is unlikely.
Organophosphorus poisoning Dose and mode of administration of atropine
- Bolus
- Inject 1.8–3 mg (3–5 mL) of atropine bolus.
- Check three things after 5 minutes: Pulse, blood pressure, and chest crepitations.
- Aim for heart rate > 80 beats/minute, SBP > 80 mm Hg, and a clear chest.
- If the above-mentioned objectives are not achieved, double the atropine dose every 5 minutes.
- Review the patient every 5 minutes. Once these parameters start improving, repeat the last same or smaller dose of atropine.
- If there is persistent and satisfactory improvement in these parameters after 5 minutes, atropine infusion can be planned.
Organophosphorus poisoning Atropine infusion
- Calculate the total dose of atropine required for rapid atropinization.
- Start hourly atropine infusion at 10–20% of the total dose of atropine required for atropinization.
- Most patients do not need > 3–5 mg/h of atropine infusion.
- Use a three-point checklist (secretions, heart rate, pupils) to reduce infusion rate by 20% every 4 hours once the patient is stable.
- Target endpoints for atropine infusion are presented
- Target endpoints for atropine infusion.
- Clear chest on auscultation
- Heart rate > 80 beats/minute (WHO recommends > 100 bpm)
- Systolic BP >80 mm Hg
- Pupils no longer pinpoint
- Dry axillae
- Bronchorrhea is the most important sign for titrating the dose of atropine once the patient is stable.
Atropine toxicity = absent bowel sounds + fever + confusion/delirium
- Stop atropine infusion for 60 minutes, if the patient has developed atropine toxicity. Restart infusion at a lower rate, once the temperature comes down and the patient gets calm.
If atropine is contraindicated, glycopyrrolate can be used for bronchorrhea. Glycopyrronium bromide can be an alternative for peripheral symptoms (0.2 mg IM stat repeated 6 hourly).
Question 8. Write a short essay/note on pralidoxime (2-PAM).
Answer:
2. Pralidoxime (2-PAM): Pralidoxime reactivates acetylcholinesterase enzymes by removing the phosphoryl group deposited by the organophosphate.
- Only to treat organophosphorus-poisoned patients.
- Bolus dose: 30 mg/kg (i.e., 1–2 g for adults) in 100 mL normal saline over 15–30 minutes.
- Maintenance dose: Continuous infusion of 8–12 mg/kg/h.
- PAM must be given by infusion. Go slow, both for bolus and maintenance.
- A fast infusion can cause vomiting, hypertension, cardiac arrhythmia, or cardiac arrest.
- Give PAM until atropine is no longer required.
3. Benzodiazepines
- Agitation and seizures: Diazepam 10 mg slow IV push, repeated as necessary. Up to 30–40 mg of diazepam per 24 hours can be given.
Supportive measures
- Mechanical ventilation, vasopressors, antibiotics, diuretics (if pulmonary edema), early enteral feeding, physiotherapy
Chronic Organophosphate Poisoning
Pralidoxime Clinical features
- Delayed polyneuropathy (OPIDN)
- Neuropsychiatric disorder
Triorthocresyl phosphate (TOCP) poisoning is associated with polyneuropathy also called a singer Jake Paralysis.
Owing to the consumption of ginger which was used in the manufacture of bootleg alcohol and was adulterated with TOCP.
It usually manifests after about 10–20 days and causes distal predominant neuropathy.
Pralidoxime Diagnosis: Clinical diagnosis, by suspicion and exclusion.
Pralidoxime Treatment: Not established. Only supportive measures.
Carbamates
Question 9. Discuss the management of carbamate poisoning.
Answer:
- Examples: Sevin, Baygon, Lannate, carbaryl, and aldicarb.
- Medicinal forms include physostigmine, pyridostigmine, and neostigmine.
- Cholinesterase inhibitors are structurally related to organophosphates.
- Transiently and reversibly inhibit cholinesterase (<6 h). Regeneration of enzymes occurs within minutes to hours; therefore, aging does not occur.
Carbamates Symptoms of intoxication are similar to organophosphates but are of shorter duration.
- Carbamates do not effectively penetrate into CNS, so less central toxicity and no seizures.
- Atropine therapy is usually not needed for longer than 6–12 hours.
- Avoid pralidoxime (2-PAM): Since irreversible binding does not occur, it is not needed and potentially can worsen some carbamate poisonings.
Organochlorine Poisoning
Question 10. Write a short essay on organochlorine poisoning.
Answer:
Classification of Organochlorine
Dichlorodiphenylmethane: DDT, methoxychlor Hexachlorocyclohexane: Lindane Cyclodienes
- Aldrin, chlordane, dieldrin
- Endrin, endosulfan, heptachlor
- Chlordecone (kepone): Mirex
Acute organochlorine poisoning
- Prodromal symptoms: Tremor, ataxia, myoclonus, dizziness, confusion, paresthesia of mouth, nausea, vomiting.
- Typical presentation: Status epilepticus followed by respiratory failure, cardiac arrhythmias, rhabdomyolysis, and acute renal failure.
Organochlorine Poisoning Treatment
- Control seizure: The same way as “status epilepticus”: Benzodiazepines, phenobarbital, phenytoin.
- Prevent complications.
Subacute Organochlorine Poisoning
- Hyperexcitability stage: Tachycardia, tremor, hyperreflexia.
- Treatment
- Symptomatic treatment: Anxiolytic
- Enhance elimination: Cholestyramine.
Chronic Organochlorine Poisoning
- Organochlorine insecticides interfere with endocrine and reproductive systems.
- Individuals who work with insecticides show low sperm count and motility, infertility, and abortion.
- The insecticides can be carcinogenic to animal
Organochlorine Poisoning Paraquat Poisoning
- Paraquat is a common herbicidal poison with a very high case fatality (>50%).
- The toxicity is related to the generation of oxygen species which cause cellular damage via lipid peroxidation, activation of NF-
- κB, mitochondrial damage, and apoptosis.
- Ingestion of large amounts results in fulminant organ failure: pulmonary edema, cardiac, renal, and hepatic failure.
- Smaller quantities mainly damage the lung and kidneys.
- Acute kidney injury sets in rapidly. The lung involvement occurs in two phases: acute alveolitis which occurs within 1–3 days followed by secondary fibrosis.
- Severe mucosal erosions with bleeding are seen in the GIT and acute hepatitis is seen.
- There is no specific antidote available. Activated charcoal and Fuller’s earth can minimize further absorption. Gastric lavage is contraindicated.
- Treatment is supportive, with oxygen supplementation, and nutritional support.
- Hemodialysis and hemoperfusion are imitated for renal failure.
- Immunosuppression with cyclophosphamide, MESNA, methylprednisolone, and dexamethasone has been used to prevent fibrosis.
- Antioxidants like vitamins C and E, N-acetylcysteine, desferrioxamine, and salicylic acid have also been tried.
Snakebite/Ophitoxemia
Question 11. Enumerate the local poisonous snakes and describe the distinguishing marks of each. Discuss the clinical manifestations, diagnosis, and management of snakebites.
Answer:
Classification of poisonous snakes
1. Elapidae (neurotoxic): Examples:
- Common cobra/nag or kalsap or Naja naja
- King cobra: Raj Nag or Naja Hannah or Naja Bungarus
- Krait: Subgrouped into:
- Common krait or Bungarus caeruleus;
- Banded krait or Bungarus fasciatus;
- Coral snake;
- Tiger snake;
- Mambas and
- Death adder.
2. Viperidae (vasculogenic): They are grouped into:
- Pitiless vipers: These include: Russell’s viper and saw-scaled viper
- Pit vipers: These include: pit viper—Crotalidae and the common green pit viper.
3. Hydrophidae (myotoxic): About 20 types of sea snakes are found in India. All are poisonous.
India recorded a staggering 1.2 million snakebite deaths in the 20-year period from 2000 to 2019 with an average of 58,000 deaths caused by snakebite annually.
Around 70% of these deaths occurred in limited, low-altitude, rural areas of eight states—Bihar, Jharkhand, Madhya Pradesh, Odisha, Uttar Pradesh, Andhra Pradesh (including Telangana), Rajasthan, and Gujarat.
Snakes may be venomous or nonvenomous. When a venomous snakebite, it may excrete venom.
Snake venom is a toxin (hematotoxin, neurotoxin, or cytotoxin).
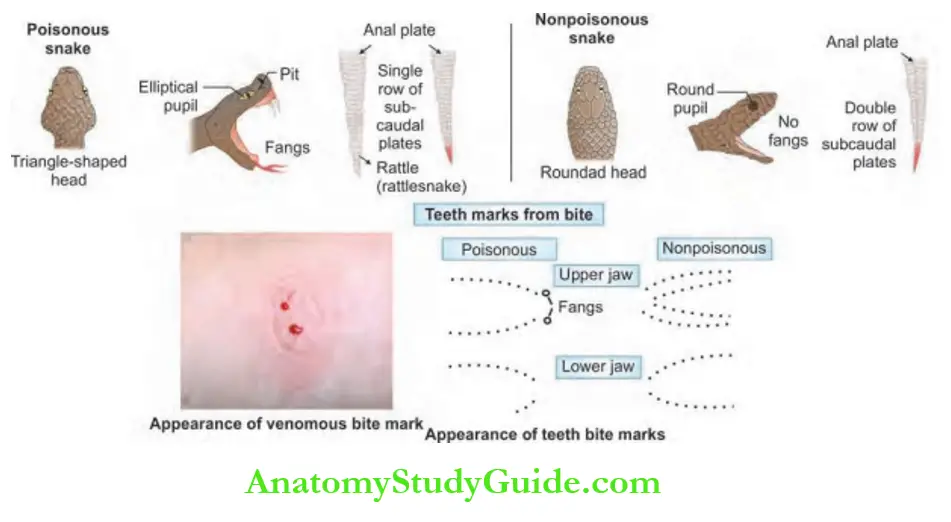
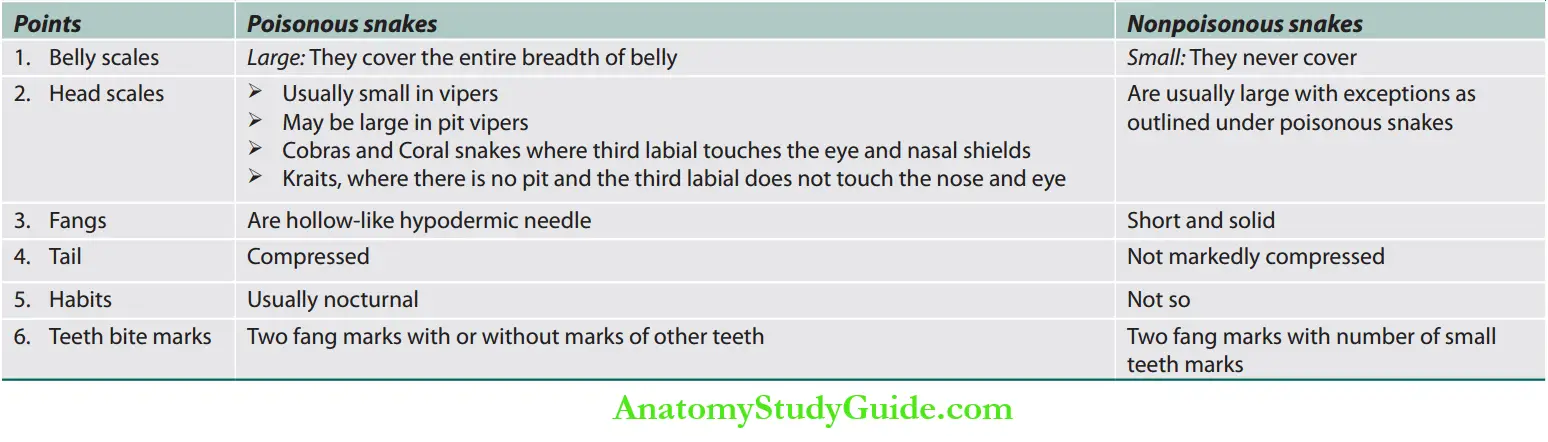
Composition of snake venom Teeth bite marks the difference between poisonous and nonpoisonous snakes.

Poisonous: Two fang marks with or without marks of outer teeth.
Nonpoisonous: Two fang marks with a number of small teeth marks.
Differences between poisonous and nonpoisonous snakes.
Clinical Features of Snakebite
Question 12. Discuss:
- Clinical features of poisonous snakebite.
- Cobra bite envenomation—features and treatment
Question 13. Write a short essay/note on the complications of poisonous (cobra) snakebite.
Answer: Signs, symptoms, and complications of snakebite.
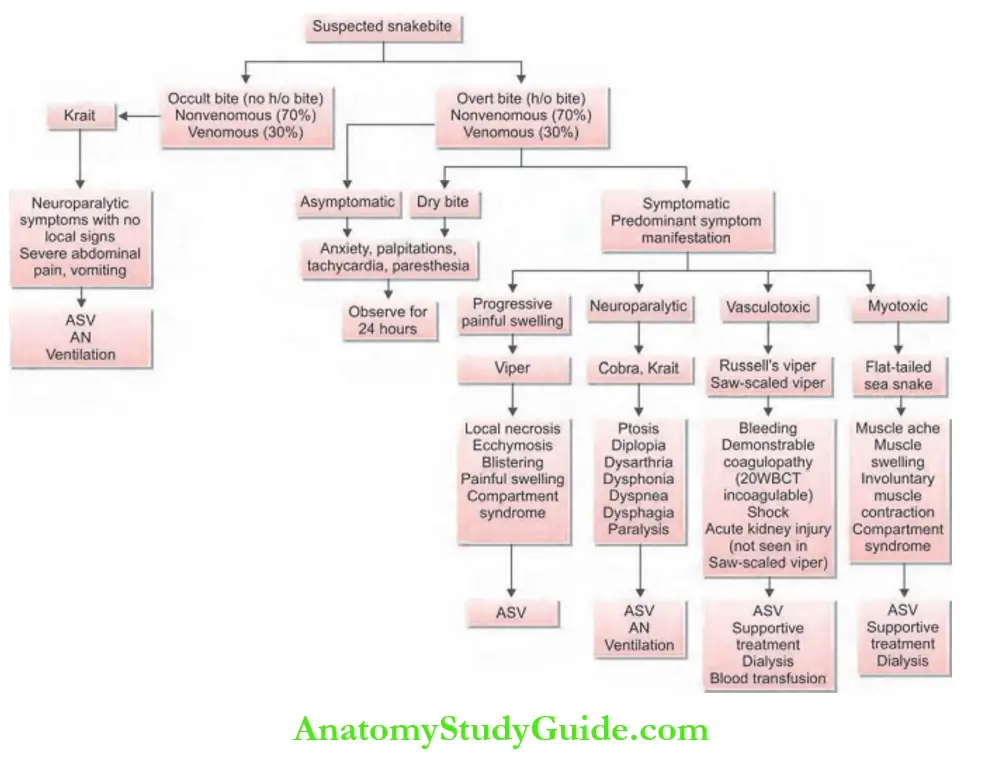
Asymptomatic (dry bite): Significant proportion of snakebites do not result in envenomation.
Patients without clinical features of local or systemic envenomation should be closely observed for 24–48 hours.
Prognosis Assessment in Snakebite
- Time of bite
- Activity at the time of the bite
- First aid action taken since the bite
- Clinical examination
- Twenty minutes whole blood clotting test (WBCT)
Clinical Features of Snakebite Laboratory Investigations
Bedside 20-minute whole blood clotting test(20-WBCT)
- Place 2 mL of freshly sampled venous blood in a small glass test tube and leave it undisturbed for 20 minutes at ambient temperature. Gently tilt the test tube to see if the blood is still liquid; the patient has hypofibrinogenemia as a result of venom-induced consumption coagulopathy.
- Nonspecific: Hemogram, serum creatinine, serum amylase, creatine phosphokinase (CPK).
- Prothrombin time (PT), fibrinogen degradation product (FDP), and fibrinogen level in viper bite as it interferes with
the clotting mechanism. - LFT, ABG, and electrolyte: For systemic manifestation.
- Urine examination: For proteinuria, myoglobinuria.
- ECG: Nonspecific changes such as bradycardia and atrioventricular (AV) block.
Question 14. Describe the initial approach to the stabilization of the patient who presents with snakebite.
Answer:
Hymenoptera Management
- The first aid currently recommended is based on the mnemonic: “Do it RIGHT”.
- R = Reassure the patient. Seventy percent of all snakebites are from nonvenomous species.
- Only 50% of bites by venomous species actually envenomate the patient.
- I = Immobilize in the same way as a fractured limb. The use of bandages or cloth is to hold the splints and should block the blood supply or apply pressure.
- Do not compress by tight ligatures, because they can be dangerous! (Loose ligatures to block lymphatic flow can be used?)GH = Get to Hospital immediately.
- Traditional remedies have NO PROVEN benefit in treating snakebite
- T = Tell the physician about any systemic symptoms that develop on the way to the hospital (e.g., ptosis)
Hymenoptera Specific treatment
- Antisnake venom (ASV)
- Indications for ASV are presented.


Question 15. Enu moderates the indications and describes the pharmacology, dose, adverse reactions, and hypersensitivity reactions of antisnake venom.
Answer: The classification of the severity of snakebite is presented.
Dosage of ASV: Ideally administer within 4 hours but effective, if given within 24 hours:
- In mild cases, 5 vials (50 mL); in moderate cases, 5–10 vials; and in severe cases, 10–20 vials.
- Additional infusions containing 5–10 vials are infused until the progression of swelling ceased and systemic symptoms are disappeared.
Mode of administration: ASV is given slowly as an IV injection or infusion at the rate of 2 mL/minute.
ASV dilute 5–10 mL/kg body weight of normal saline or 5% dextrose and infused over 1 hour.
ASV should never give locally at the site of snakebite. No change in dose for children or pregnant women.
Repeat dose of ASV
- In vasculogenic or hemotoxic envenomation: Administer ASV every 6 hours until coagulation (WBCT) is restored.
- In neuroparalytic or neurotoxic envenomation: Initial dose of ASV 10 vials stat as an infusion to be followed by 2nd dose of 10 vials if no improvement within 1st hour (total 20 vials).
Adverse reaction of ASV: It may develop in 20% of patients
Adverse reactions of antisnake venom (ASV).
1. Early anaphylactic reaction: It may develop within 10 minutes to 3 hours. Patients should be monitored closely.
Treatment of anaphylactic reaction:
- Discontinue ASV
- Adrenaline: 1:1,000 IM (0.5 mg/kg in adults and 0.01 mg/kg in children).
- It can be repeated every 5 minutes, if necessary.
- H1 antihistaminic: IV 1 mg of chlorpheniramine maleate (CPM)
- IV hydrocortisone
- Once the patient has recovered, restart ASV slowly for 10–15
minutes keeping the patient under close observation. Then resume the normal drip-rate.
2. Late serum sickness: Develop in 1–12 days. Characterized by fever, nausea, vomiting, diarrhea, arthritis, nephritis, myoglobinuria, etc.
Pharmacology Treatment consists of:
- Oral antihistaminic: a 5-day course of oral antihistaminic. For adults—CPM is 2 mg/6 hour and for children—0.25 mg/kg/day in a divided dose.
- Prednisolone: For patients who fail to respond within 24 hours.
Pharmacology Dose: 5 mg/6 hours in adults and 0.7 mg/kg/day in divided doses in children.
An algorithm approach to the identification of the type of snakebite is presented.
2. Supportive therapy
- For coagulopathy: If it does not reverse after ASV therapy, fresh-frozen plasma, cryoprecipitate (fibrinogen, factor VIII), fresh whole blood, and platelet concentrate can be administered.
- Management neurotoxic (neuroparalytic) envenomation
- ASV alone is not sufficient.
- Tracheostomy, endotracheal intubation, and mechanical ventilation.
- Atropine neostigmine (AN) dosage schedule: Atropine 0.6 mg followed by neostigmine (1.5 mg) to be given IV stat and repeat dose of neostigmine 0.5 mg with atropine every 30 minutes for 5 doses.
- Thereafter to be given as a tapering dose at 1, 2, 6, and 12 hours.
- Glycopyrrolate: About 0.25 mg can be given before neostigmine in place of atropine as glycopyrrolate does not cross the blood-brain barrier.
- Renal failure: Hemodialysis/peritoneal dialysis.
- Capillary leak syndrome: Methylprednisolone (10 mg/kg Q8H) × 3 days.
- Compartment syndrome: Fasciotomy.
- Surgical debridement of the wound
- Care of bitten part: Antibiotic prophylaxis and tetanus toxoid.
Scorpion Bite
Question 16. Describe the diagnosis, initial approach stabilization, and therapy of scorpion envenomation.
Answer:
Scorpion venom:
It is clear, colorless toxalbumin and can be classified as either neurotoxic or hemolytic.
Toxicity is more than a snake. However, during the bite only a small quantity is injected.
Venom is a strong autonomic stimulator and releases a large amount of catecholamine from adrenals.
Mortality (except in children) is negligible and can cause acute pancreatitis.
Signs and Symptoms
1. In the case of hemolytic venom:
- The reaction is predominantly local and simulates the viper snakebite. However, the scorpion sting bite shows only one hole in the center of the reddened area at the site of the bite.
- The extremity will have severe pain and edema.
2. In the case of neurotoxic venom:
- Symptoms are similar to a cobra bite.
- Usually no mark reaction in the local area.
- Symptoms: Nausea, vomiting, severe restlessness, paralysis, fever, cardiac arrhythmia, convulsions, cyanosis, coma, and respiratory depression. Death may occur within hours from pulmonary edema and cardiac failure.
Diagnosis is confirmed by enzyme-linked immunosorbent assay (ELISA) testing.
Scorpion Bite Treatment
- Immobilize the limb and apply a tourniquet above the sting
- Pack sting in ice, incise and use suction, and wash with a weak solution of ammonia, borax, or potassium permanganate
- A local anesthetic (2% novocaine or 5% cocaine) is injected at the site of the pain
- A specific antivenom is available for most species
- Calcium gluconate IV to control local swelling
- Adrenergic symptoms (hypertension and/or pulmonary edema): Prazosin (selective peripheral alpha-1 adrenergic antagonist)
- Barbiturate to reduce convulsions
- Morphine is contraindicated. Give IV fentanyl 1 mg/kg for pain
- Atropine is valuable to prevent pulmonary edema
- Treatment of massive pulmonary edema: By oxygen, IV aminophylline or nitroprusside, NIV/CPAP
Hymenoptera (Bee, Wasp, Hornet) Stings
Question 17. Describe the diagnosis initial approach stabilization and therapy of bee sting allergy.
Answer:
- Hymenopteran stings only cause local inflammation in most people.
- Symptoms include pain, swelling, pruritis, and bleeding.
- Large, local reactions (LLRs) develop in about 10% of Hymenoptera stings and are due to be immune IgE-mediated.
- In sensitized individuals, a single sting may result in rapid and potentially fatal anaphylaxis with hypotension (shock), bronchospasm, and angioedema.
- Intramuscular 0.1% adrenaline can be lifesaving.
- Mass attacks by bees can be life-threatening even in nonsensitized individuals, through the direct action of venom causing hemolysis, rhabdomyolysis, pulmonary edema, acute renal failure, and adrenergic effects.
- No antivenom is available.
- Treatment is symptomatic.
Corrosive Poisoning
Question 18. Enumerate the common corrosives used in your area and describe their toxicology, clinical features, prognosis, and approach to therapy.
Answer:
Common corrosive poisons:
- Acids (hydrochloric, acetic, sulfuric, lactic, oxalic, carbolic)
- Alkalis (sodium and potassium, soaps, detergents)
- Heavy metal salts (sublimate)
- Others: Formalin, iodine tincture
Corrosive Poisoning Clinical Features
- Clinical presentation of corrosive injuries in the upper gastrointestinal tract.
- Acids cause coagulation necrosis while alkalis cause liquefactive necrosis.
- The patient complains of oropharyngeal, epigastric, or retrosternal pain associated with dysphagia or odynophagia, and/ or hypersalivation, nausea, vomiting, and hematemesis.
- Severe forms can damage the larynx and also cause endotracheal or bronchial necrosis with mediastinitis, also perforation of the stomach may occur.
- Late complications are esophageal strictures and stenosis, gastric stenosis of the antrum and pylorus, esophageal and stomach cancer.
Corrosive Poisoning Treatment
- Treatment mainly is to prevent complications.
- Lavage is contraindicated.
- Upper gastrointestinal (UGI) endoscopy should be performed during the first 24 hours after ingestion in order to evaluate the extent of esophageal and gastric damage, establish a prognosis and guide therapy.
- Grading of corrosive injury based on endoscopy:
- 0: Normal mucosa
- 1: Erythema/hyperemia
- 2a: Superficialulcer/erosion/friability/hemorrhage/exudates
- 2b: Findings in 2a + deep discrete/circumferential ulcers
- 3a: Scattered/focal necrosis (black/gray discoloration)
- 3b: Extensive/circumferential necrosis of mucosa
- Antibiotics are recommended for grade 3 injury and suspected gastrointestinal perforation.
- Proton pump inhibitors and H2 blockers are routinely recommended.
- Nutrition is planned according to the endoscopic grade of the lesions.
- Patients with grade 1/2a can tolerate oral feeds and those with grade 2b/3a will require nasoenteral feeding. Patients with grade 3b lesions require gastrostomy/ jejunostomy for enteral feeding and may also require total parenteral nutrition.
- 30% of patients usually develop esophageal strictures within 2 months which will need endoscopic dilatation or surgery.
Common Drug Overdosages
Question 19. Enumerate the commonly observed drug overdose in your area and describe their toxicology, clinical features, prognosis, and approach to therapy. (or) Write a short essay/note on benzodiazepine overdose and management.
Answer: Sedative Drug Poisoning
Common Drug Overdosages Benzodiazepines Poisoning
Common Drug Overdosages Mode of Action
- Benzodiazepines (BZDs) exert their effect via modulation of the gamma-aminobutyric acid-A (GABA-A) receptor.
- Gamma-aminobutyric acid is the main inhibitory neurotransmitter of the central nervous system.

Clinical Features of Overdosage
Oral benzodiazepines taken in overdose without a contestant rarely cause significant toxicity.
The classic presentation of a patient with an isolated BZD overdose consists of CNS depression with normal vital signs.
- Toxic symptoms: Sedative action on the CNS.
- Large doses: Neuromuscular blockade.
- Intravenous injection: Peripheral vasodilation, fall in BP, shock.
Propylene glycol (1,2-propanediol) is the diluent used in parenteral formulations of diazepam and lorazepam which itself causes cardio- and neurotoxicity.
Of note, most intentional ingestions ofBZDs involve a contestant, the most common being ethanol.
Common Drug Overdosages Acute poisoning
Mild: Drowsiness, ataxia, weakness.
Moderate to severe: Vertigo, slurred speech, nystagmus, partial ptosis, lethargy, hypotension, respiratory depression, coma (stages 1 and 2).
COMA (Stage 1): Responsive to painful stimuli but not to verbal or tactile stimuli, without any disturbance in respiration or BP.
COMA (Stage 2): Unconscious, not responsive to painful stimuli, no disturbance in respiration or BP.
General Diagnostic Testing
Check glucose, to rule out hypoglycemia as the cause of any alteration in mental status.
Acetaminophen and salicylate levels, to rule out these common co-ingestions.
Electrocardiogram, as it affects the QRS or QTc intervals. Pregnancy test in women of childbearing age.
Life Supportive Procedures and Symptomatic/Specific Treatment
- Airway, breathing, and circulation
- Endotracheal intubation
- Assisted ventilation
- Supplemental oxygen intravenous fluids, inotropes, if needed.
General Diagnostic Testing Decontamination
Gastrointestinal decontamination with activated charcoal (AC) (usually of no benefit in cases of isolated BZD ingestion and increases the risk of aspiration).
Antidote Treatment: Flumazenil
- Mode of action: Competitive antagonism. Complete reversal of benzodiazepine effect with a total slow IV dose of 1 mg.
- Administered in a series of smaller doses beginning with 0.2 mg and progressively increasing by 0.1–0.2 mg every minute until a cumulative total dose of 3.5 mg is reached.
- Remediation occurs within 0.5–2 hours.
- Side effects: Nausea, vomiting, arrhythmias, convulsions.
- Contraindication: Status epilepticus.
Barbiturate Poisoning
Question 20. Write a short essay on the clinical features and treatment of barbiturate poisoning.
Answer:
- Nonselective CNS depressants.
- Mode of action: Direct CNS depressants bind to GABA
receptors→ and prolong the opening of the chloride channel. Inhibits excitable cells of the CNS.
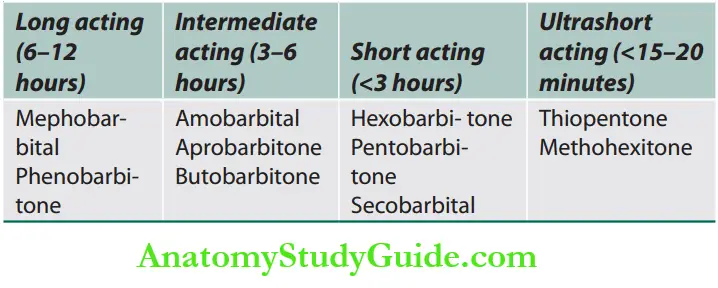
Barbiturate Poisoning Classification
Barbiturate Poisoning Signs and Symptoms
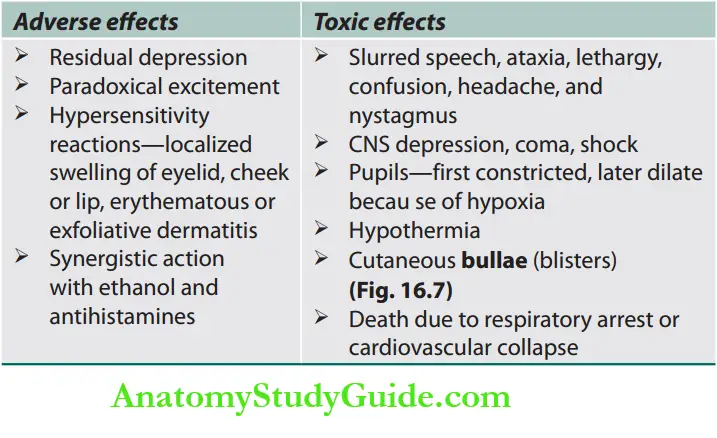
Management of Barbiturate Poisoning
- No specific antidote.
- Barbiturate poisoning is more dangerous than benzodiazepine poisoning.
- Management is supportive.
- Cardiorespiratory support.
- Clean the airways by thorough suctioning and insertion of oral airways.
- If the patient is comatose, prompt intubation is strongly advocated because of the worsening of respiratory failure.
- Correction of dehydration by CVP-guided fluid therapy depending on the serum electrolytes.
- Treat hypotension by intravenous infusion of plasma expanders and vasopressors.
- In refractory cases, steroids are given.
Measures to prevent absorption:
- Gastric lavage
- Activated charcoal is administrated orally or by nasogastric tube.
Measures for removal of barbiturates:
- Frequent doses of activated charcoal
- Forced diuresis with alkalization of urine
- Hemodialysis and hemoperfusion.

Analgesic Poisoning
Paracetamol (Acetaminophen) Poisoning
Question 21. Write a short essay on paracetamol poisoning and its treatment.
Answer:
- Toxicity is unlikely to result from a single dose of <150 mg/kg in children or 7.5–10 g for adults.
- Toxicity is likely with single ingestions > 250 mg/kg or those >12 g over a 24-hour period.
- Virtually all patients who ingest doses in excess of 350 mg/kg develop severe liver toxicity unless appropriately treated.
Mechanism of Paracetamol Toxicity
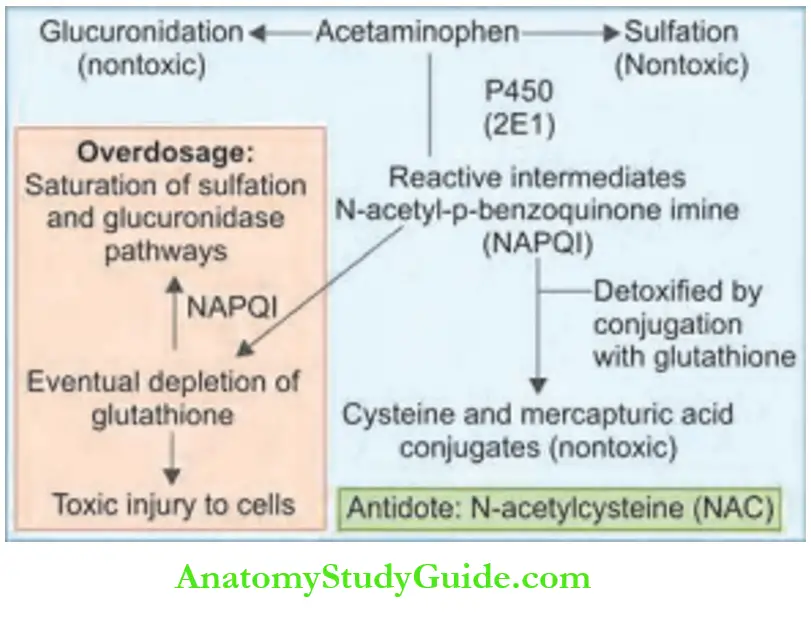
Toxicity is due to the formation of an intermediate reactive metabolite, which binds covalently to cellular proteins, leading to cell death. This causes hepatic and occasionally renal failure.
In therapeutic doses, the toxic intermediate metabolite is detoxified in reactions requiring glutathione. With overdose, glutathione reserves become depleted.
Clinical Manifestations of Toxicity
- Stage I (0.5–24 hours)
- No symptoms; nausea, vomiting, and malaise.
- Stage II (24–72 hours)
- Subclinical elevations of hepatic aminotransferases (AST, ALT).
- Right upper quadrant pain, with liver enlargement and tenderness.
- Elevations of prothrombin time (PT), total bilirubin, and oliguria and renal function abnormalities may become evident.
- Acute kidney injury is primarily due to acute tubular necrosis.
- Stage III (72–96 hours)
Fulminant hepatic failure: Jaundice, confusion (hepatic encephalopathy), a marked elevation in hepatic enzymes, hyperammonemia, a bleeding diathesis, hypoglycemia, lactic acidosis, renal failure (25%), and death.
- Stage IV (4 days to 2 weeks)
- The recovery phase usually begins by day 4 and is complete by 7 days after the overdose.
Treatment Options
- Activated charcoal: May reduce absorption by 50–90%.
- Gastric lavage: Only for massive ingestions (e.g., > 600 mg/kg).
- Antidote: N-acetylcysteine (NAC)
- Properties:
- Mechanism of action (MOA): A glutathione precursor.
- Limits the formation and accumulation of NAPQI.
- Powerful anti-inflammatory and antioxidant effects.
Dosage and administration:
- IV infusion.
- 150 mg/kg over 15 minutes; 50 mg/kg over the next 4 hours; 100 mg/kg over the next 16 hours up to 36 hours.
- Most effective, if started within 8–10 hours after ingestion.
- Beyond 8 hours, NAC efficacy progressively decreases. The oral N-acetylcysteine regimen consists of a 72-hour oral course given as a 140 mg/kg loading dose followed by 17 doses of 70 mg/kg every 4 hours (total dose of 1,330 mg/kg).
Alternate medication: Oral methionine.
Liver transplantation
Indications for liver transplantation for paracetamol poisoning (King’s College Criteria).
- Acidosis (pH <7.3)
- PT (prothrombin time) >100 sec
- Creatinine >3.4 mg/dL
- Grade 3 encephalopathy (or worse)
- It is life-saving for fulminant hepatic necrosis
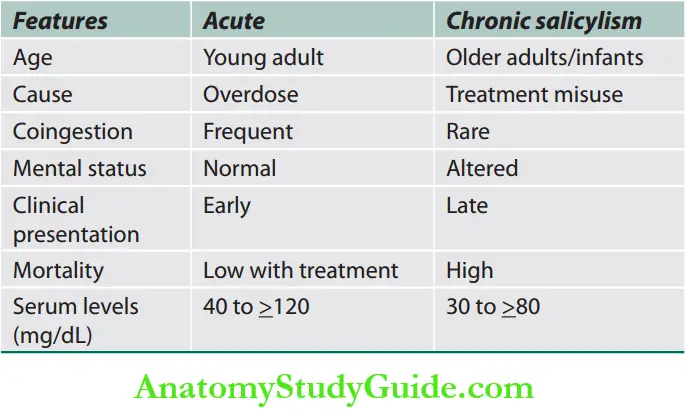
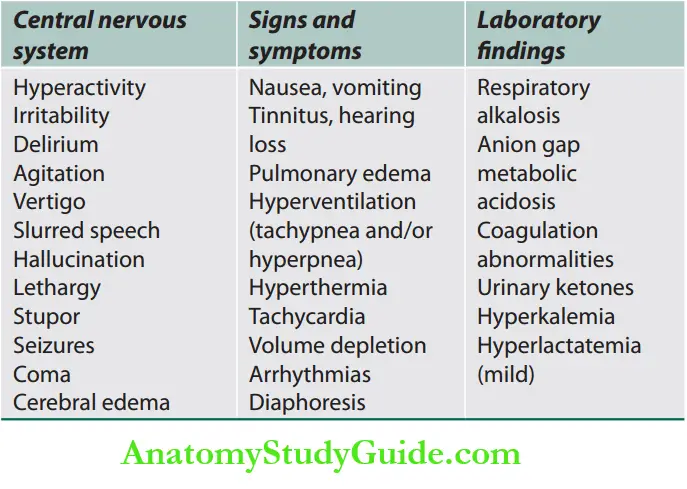
- Aspirin Toxicity
Question 22. Write a short note on salicylate poisoning and its management.
Answer:
Mechanism of toxicity
- Acetylsalicylic acid (ASA) is hydrolyzed to salicylic acid. Responsible for therapeutic and toxic effects.
- Direct stimulation of respiratory center: Medulla.
- Uncouples oxidative phosphorylation:
- Increase in O2 consumption and CO2 production
- Increase respiration leads to respiratory alkalosis.
- Renal excretion of bicarbonate, Na and K: Metabolic acidosis.
- Inhibition of mitochondrial respiration: Increase pyruvate and lactic acid → metabolic acidosis.
- Disruption of Kreb’s cycle metabolism and glycolysis → hyperglycemia, ketonemia.
Signs and symptoms
ASPIRIN mnemonic.
- Altered mental status (lethargy—coma)
- Sweating/diaphoresis
- Pulmonary edema
- Increased vital signs (hypertension, increased respiratory
rate, tachycardia) - Ringing in the ears
- Irritable
- Nausea and vomiting
Salicylate poisoning can occur in two settings—acute toxicity and chronic toxicity.
Management of Aspirin Overdose
- Initial supportive therapy
Specific Management
- Decreasing absorption
- Activated charcoal: Given in those who have taken > 250 mg/kg body weight < 1 hour ago.
- Gastric lavage: It is advised in patients who have taken > 500 mg/ kg body < 1 hour ago.
- Increasing drug elimination
Urinary alkalinization:
- Alkalinizing urine from pH 5–8 increases renal elimination of ASA from 1.3 to 100 mL/minute.
- Serum half-life decreases from 48 to 6 hours.
- This is done by giving an infusion of sodium bicarbonate.
Absolute indications for hemodialysis in aspirin toxicity.
- Renal failure
- Congestive heart failure
- Acute lung injury
- Persistent CNS disturbances
- Progressive deterioration in vital signs
- Severe acid-base or electrolyte imbalance, despite appropriate treatment.
- Hepatic compromise with coagulopathy
- Salicylate concentration (acute) >100 mg/dL (in the absence of the above)
Hemodialysis
- Used in a severe life-threatening overdose.
- Aims to correct the acid-base disturbances while removing the salicylate.
Cyanide Poisoning
Question 23. Write a short essay on the management of cyanide poisoning.
Answer:
Cyanide
- Present in bitter almonds (250 mg CN/100 g plant tissue), cassava (104 mg CN/100 g plant tissue), wild cherries (140–370 mg CN/100 g plant material), and other foods.
- Used extensively in industry for fumigation, electroplating, and mining activities.
Routes of exposure to cyanide.
- Gas: Inhalation (e.g., hydrogen cyanide and cyanogen chloride)
- Liquid: Inhalation (aerosol), ingestion, skin contact (e.g., hydrocyanic acid)
- Solid: Inhalation, ingestion, skin contact (e.g., cyanide salts)
Clinical Manifestations of Cyanide Poisoning
- Onset of cyanide poisoning
- Inhalation (rapid onset, seconds to minutes), ingestion, and skin contact (delayed onset, 15–30 minutes).
- Death may occur within 6–8 minutes after inhalation of a high concentration of 2–5 mg/kg it is lethal.
- Mechanism: Inhibits mitochondrial cytochrome oxidase and an “asphyxiating” agent.
The common final pathway for cyanide intoxication is cellular hypoxia.
- Metabolic acidosis: Nonspecific symptoms.
- CNS: Dizziness, nausea, vomiting, drowsiness, tetanus, trismus, hallucinations.
- CVS: Dysrhythmia, hypotension. Tachycardia and hypertension may occur transiently in the early stages.
- Respiratory: Dyspnea, initial hyperventilation followed by hypoventilation, and pulmonary edema. Cyanosis is not apparent, since blood is adequately oxygenated
Laboratory Diagnosis
- Blood cyanide levels can be estimated, but empiric treatment is almost always required before laboratory results are available.
- High anion gap metabolic acidosis.
- Arterial and venous pO2 may be elevated.
Cyanide Poisoning Treatment
- Activated charcoal: For alert, asymptomatic patients following ingestion.
- Supplemental oxygen: 100% for suspected exposure. Supportive care.
- Sodium nitrite:
- Mechanism: Forms methemoglobin, competes with cytochrome oxidase for free cyanide; combines with cyanide to form cyanmethemoglobin.
- Dose:
- Adults: 300 mg IV over 5 minutes; slower if hypotension develops and
- Children: 0.12–0.33 mg/kg IV infused as above.
- Amyl nitrite: 0.3 mL inhaled can be repeated after 3–5 minutes.
- The second-line agent is used when sodium nitrite is not available.
- Sodium thiosulfate:
- Mechanism: Sulfur donor promotes rhodanese activity, and detoxifies cyanide as it is released from cyanmethemoglobin. Directly detoxifies cyanide by conversion to thiocyanate; too slow to be useful as a first-line intervention.
- Dose:
- Adults: 12.5 g IV over 10–20 minutes following administration of sodium nitrite and
- Children: 412.5 mg/kg IV over 10–20 minutes.
Cyanide Poisoning Hydroxocobalamin
- Mechanism: Direct-binding agent, chelates cyanide.
- Dose: 4–5 g IV
- Dicobalt edetate is an intravenous chelator of cyanide that can be used.
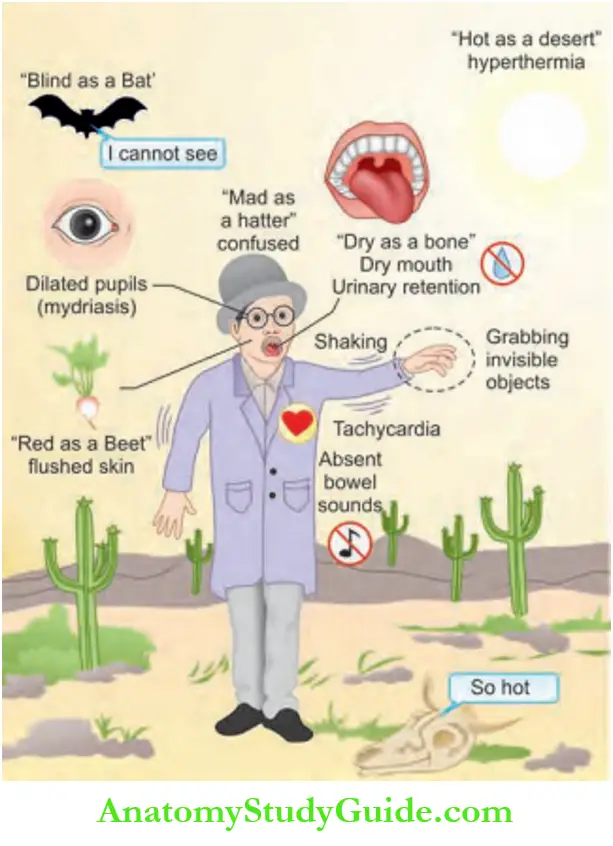
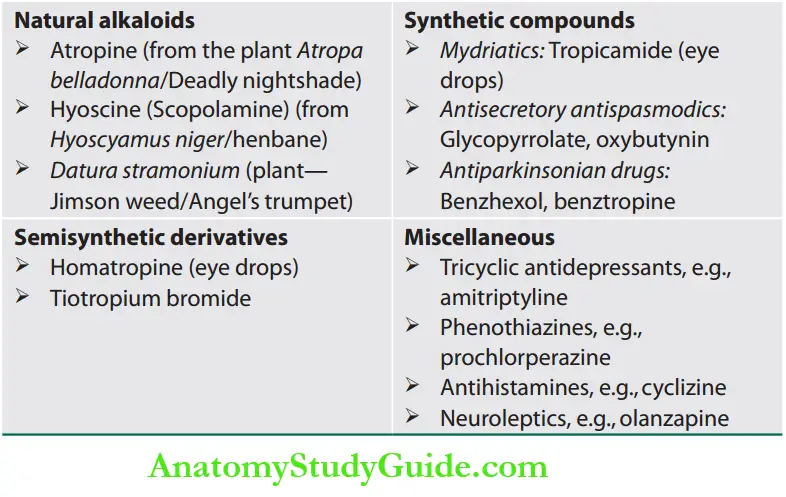
Anticholinergic Toxidrome
Question 24. Write a short essay/note on the causes of the anticholinergic syndrome.
Answer:
Causes of Anticholinergic Toxidrome
Plant Poisons
Question 25. Enumerate the common plant poisons seen in your
area and describe their toxicology, clinical features, prognosis, and specific approach to detoxification. (or) Write a short essay/note on clinical features and management of datura poisoning.
Answer:
Neurotoxic Plant Poisons
Datura Poisoning
- Datura stramonium (jimson seed) causes anticholinergic syndrome.
- The active toxic agents include atropine and scopolamine.
- Atropine and related compounds block acetylcholine at the receptor sites of postganglionic synapses of the cholinergic nerves.
- All the parts of the datura plant are poisonous, but the seeds and fruit are the most toxic.
- Mode of poisoning: Most popular mode of poisoning is by mixing the seeds in sweets and given to others with the intention of theft.
Plant Poisons Clinical features
- Toxic symptoms often appear within 30 minutes of ingestion and last for 24–48 hours.
- Clinical features include tachycardia and the other features are described as “blind as a bat, mad as a hatter, red as a beet, hot as a hare, dry as a bone, the bowel and bladder lose their tone, and the heart runs alone”.
- Hot as a hare: Cutaneous vasodilatation leading to anhidrotic hyperthermia.
- Blind as a bat: Ciliary muscle paralysis, mydriasis, dilated pupils.
- Dry as a bone: Anhidrosis, dryness of mouth, urinary retention, decreased bowel motility.
- Red as a beet: Cutaneous vasodilatation causing flushing.
- Mad as a hatter: CNS arousal, agitation, delirium, hallucinations.
- It can be fatal-producing stupor, coma, and convulsions. Death is due to respiratory paralysis or cardiovascular collapse.
Plant Poisons Management
- Gastric lavage and supportive therapy.
- Control of hyperthermia.
- The role of physostigmine, a cholinesterase inhibitor is not clear.
- Activated charcoal adsorbs the alkaloids.
- Benzodiazepines to treat agitation.
- Cardiotoxic Plant Poisons

Cardiotoxic Plant Poisons
Cardiotoxic plant poisons inhibit the Na+/K+-ATPase pump leading to an overall increase in intracellular Na+ ions and a secondary increase in intracellular Ca2+ levels.
Symptoms: On ingestion, they produce a burning sensation, abdominal pain, nausea, vomiting, diarrhea, dizziness, and numbness in the oral and perioral region.
The most important cardiotoxic effects are sinus bradycardia, varying degrees of heart block, ventricular ectopics, and ventricular tachycardia which can be fatal.
Management of Cardiotoxicity
- Atropine 0.6 mg, orciprenaline 10 mg to maintain heart rate around 80/minute. Severe bradycardia may need pacemaker insertion.
- Sodium bicarbonate 50 mL IV 6th hourly, if ABG shows acidosis.
Gastrointestinal Toxic Plant Poisons
- Ricinus communis contains ricin and Abrus precatorius contains abrin.
Cardiotoxic Plant Poisons Clinical Features
- Gastrointestinal upset, vomiting, diarrhea, abdominal pain, GI bleeding.
- Hematuria, acrocyanosis, shock, dehydration, and hemolysis.
- Abnormal liver function tests (LFTs) and renal function tests (RFTs).
Treatment: Supportive.
Opioid Poisoning
Question 26. Write a short essay/note on opiate overdosage, clinical features of opioid tolerance, and its management.
Answer:
Opium is extracted from poppy seeds (Papaver somniferum)
Opioid agonists: Morphine, heroin, hydromorphone, fentanyl, codeine.

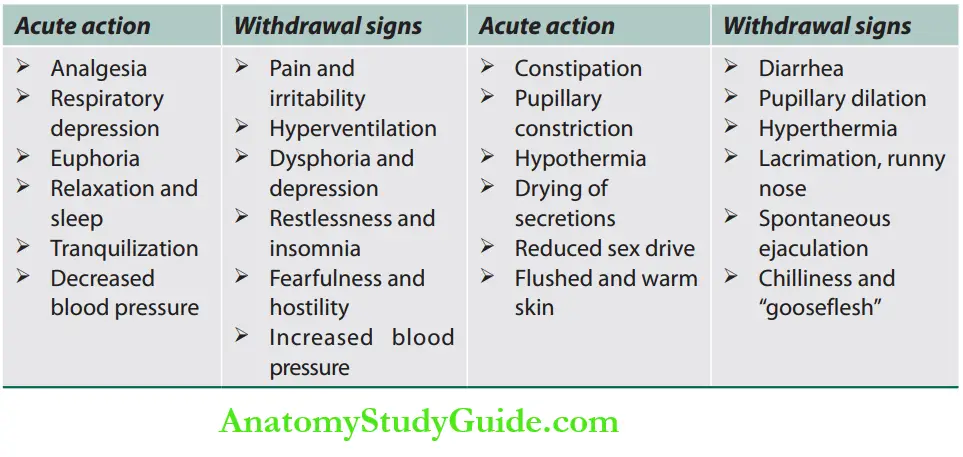
Opioid Poisoning Opioid Tolerance
- Tolerance is a diminished responsiveness to the drug’s action that is seen with many compounds.
- Tolerance can be demonstrated by a decreased effect from a constant dose of a drug or by an increase in the minimum drug dose required to produce a given level of effect.
- Physiological tolerance involves changes in the binding of a drug to receptors or changes in receptor transductional processes related to the drug of action.
This type of tolerance occurs in opioids.

- The molecular basis of tolerance involves glutaminergic mechanisms (glutamate—excitatory amino acid neurotransmitter).
- Physiological dependence occurs when the drug is necessary for normal physiological functioning—this is demonstrated by the withdrawal reactions.
- Withdrawal reactions are usually the opposite of the physiological effects produced by the drug.
- Opioid toxicity is related to opioid receptors in nonnociceptive pathways and counter-opioid responses.
- It is determined by genetics, organ function, and co-medications.
- Acute action and withdrawal signs of opioids
Carbon Monoxide
Question 27. Write a short note on carbon monoxide
poisoning—signs and symptoms.
Answer: Carbon monoxide (CO) is a colorless, odorless gas generated by faulty appliances burning organic fuels.
It is also present in vehicle exhaust fumes. It produces toxicity by binding with hemoglobin and cytochrome oxidase, which decreases the delivery of oxygen to tissue and inhibits cellular respiration.
Carbon Monoxide Clinical Features
Acute severe CO poisoning produces nonspecific symptoms such as headache, nausea, irritability, weakness, and tachypnea.
Skin changes, i.e., cherry red/pink discoloration of the skin are also seen.
Later, ataxia, nystagmus, drowsiness, and hyperreflexia may develop leading to coma, respiratory depression, cardiovascular collapse, and death.
Myocardial ischemia/infarction, cerebral edema, and rhabdomyolysis (with myoglobinuria and renal failure) may occur.
Long-term exposure can lead to Parkinsonism.
Treatment of Carbon Monoxide Poisoning
Treatment of opioid toxicity
- Ensure adequate ventilation
- Management of complications such as
Carbon Monoxide ARDS
- Antidote—Naloxone, Naltrexone
- MOA: Pure opioid antagonist competes and displaces narcotics at opioid receptor sites.
- Naloxone: IV (preferred), IM, intratracheal, subcutaneous: 0.4–2 mg every 2–3 minutes as needed.
Treatment of carbon monoxide poisoning
Administration of normobaric 100% oxygen is the therapy of choice for most cases, while hyperbaric oxygen therapy is reserved for severe poisonings.
Alcohol Poisoning
Methanol Poisoning
Question 28. Write a short note on toxicity, clinical features, and management of methanol poisoning.
Answer:
- Methanol is a mild CNS depressant.
- Metabolism: Methanol itself is not toxic. However, its metabolites namely formaldehyde and formic acid are responsible for its toxicity.
Methanol Poisoning Clinical Features
- Early clinical features are due to methanol, whereas late features are due to the methanol metabolite formic acid.
- Features due to methanol: Methanol produces nausea, vomiting, abdominal pain, headache, vertigo, confusion, obtundation, convulsions, and coma.
- Features due to formic acid: Metabolic acidosis and retinal injury.
- The retinal manifestations include clouding and diminished vision, dancing and flashing spots, dilated or fixed pupils, and hyperemia of the optic disc, retinal edema, and blindness.
- Other manifestations: Rapid breathing due to metabolic acidosis, myocardial depression, bradycardia, shock, and anuria.
- Complication: Putaminal necrosis produces rigidity, tremor, masked faces, and monotonous speech.
Methanol Poisoning Diagnosis
- Confirmation by measurement of serum methanol level, which is usually > 20 mg/dL.
- Methanol-induced formic acidosis can be confirmed by a large anion gap, low serum bicarbonate, and elevated serum formate levels.
- The osmolar gap is elevated due to methanol.
Ethylene Glycol Poisoning
- Produces similar symptoms as methanol poisoning; however, renal failure is more common.
- Treatment is on the same lines as methanol poisoning.
- Supplementation of thiamine and pyridoxine as cofactor therapy.
Ethanol Poisoning
- Alcohol belongs to the inebriant group of the neurotics class of poisons.
Stages of alcohol intoxication:
- Stage of excitement: Increased talkativeness, increased self-confidence, decreased sensory perception, loss of fine motor skills slowed information processing, and increased sexual desires.
- Stage of incoordination: Incoordination of thought, speech, impaired judgment, confusion, slurred speech, staggering gait, dilated pupils.
- Stage of narcosis: Deep sleep, rapid pulse, hypothermia, labored breathing, miosis → coma → death.
Patients can manifest with other complications like hematemesis, pancreatitis, and head injury.
Methanol Poisoning Management:
- Rule out more serious conditions such as head trauma, hypoxia, hypoglycemia, hypothermia, hepatic encephalopathy, and other metabolic derangements.
- ABG will reveal high anion gap acidosis.
- Gastric lavage is not helpful because of the rapid rate of absorption of ethanol from the gastrointestinal tract.
- Dextrose saline with 100 mg thiamine has to be administered.
- Benzodiazepines, first-generation (typical) antipsychotics, and ketamine can be used to control agitation.
- Hemodialysis is useful for severely elevated ethanol levels and severe acidosis.
- Post-recovery patients need psychotherapy and rehabilitation.
Aluminum Phosphide Poisoning
Question 29. Discuss the clinical features and management of aluminum phosphide poisoning.
Answer:
Aluminum phosphide (ALP) poisoning is known worldwide, especially in developing countries such as India. A lethal dose of ALP is 1–1.5 g.
Aluminum phosphide, when ingested, liberates a lot of phosphine gas → phosphine leads to noncompetitive inhibition of the cytochrome oxidase of mitochondria, blocking the electron transfer chain and oxidative phosphorylation, producing an energy crisis in the cells.
The severe toxicity of ALP particularly affects the cardiac and vascular tissues, which manifests as profound and refractory hypotension, congestive heart failure, methemoglobinemia, myocarditis, pericarditis and subendocardial infarction, cardiac arrhythmias, lactic acidosis, and respiratory failure.
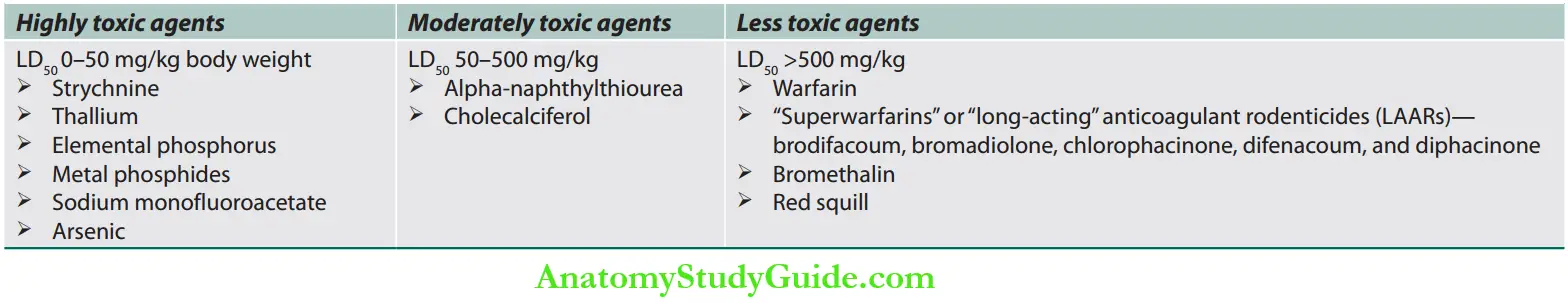
Rodenticide Poisoning
Question 30. Discuss the clinical features and management of rodenticide poisoning.
Answer:
Classification of Rodenticide Poisons
Rodenticide Poisoning Management
In the early stages:
Gastrointestinal decontamination
Correction of systemic acidosis with sodium bicarbonate.
Ethanol therapy: Indicated in patients with visual symptoms or methanol levels exceeding 20–30 mg/dL.
Ethanol blocks the conversion of methanol to formic acid by inhibiting alcohol dehydrogenase.
Rodenticide Poisoning Hemodialysis: Indicated
- when the methanol level exceeds 50 mg/dL,
- those with visual signs, and
- those with metabolic acidosis unresponsive to bicarbonate.
The antidote for methanol poisoning: 4-methyl pyrazole or fomepizole (15 mg/kg IV, followed by 10 mg/kg every 12 hours) is a direct, potent inhibitor of alcohol dehydrogenase.
It may be more effective than ethanol, which is a competitive antagonist.
Co-factor therapy: Leucovorin 50 mg IV or folic acid 50 mg IV every 6 hours is given in addition to ethanol or 4-methyl pyrazole.
It acts by enhancing the rate of degradation of formic acid to carbon dioxide.
Rodenticide Poisoning Management
It is supportive, and the main objective is to provide effective oxygenation, ventilation, and circulation till phosphine is excreted.
Gastric decontamination using activated charcoal, potassium permanganate and medicated liquid paraffin has been tried.
No definite antidote is available.
Rodenticide Poisoning Clinical Features
Yellow Phosphorous Poisoning
- In the first 24 hours post-ingestion, patients present with mild symptoms such as nausea and vomiting due to gastrointestinal irritation.
- In the next 24–72 hours, patients may remain asymptomatic. There may be a rise in bilirubin levels and liver enzymes at this stage.
- After 72 hours, they can manifest with acute liver failure (ALF), coagulopathy, hypotension, cardiac arrhythmias, and acute kidney injury. Central nervous system involvement occurs as confusion, psychosis, hallucinations, and coma.
Aluminum and zinc phosphide poisoning
- Early features include nausea, vomiting, and epigastric pain due to the corrosive nature of phosphides.
- There may be a garlic odor in the breath of these patients.
- Phosphine gas is emitted from the emesis and feces of the affected.
- These features are rapidly followed by circulatory collapse, hypotension, myocarditis, pericarditis, acute pulmonary edema, and congestive heart failure.
Rodenticide Poisoning Coumarins
- The evidence of coagulopathy occurs 24–48 hours post-consumption once all the coagulation factors are depleted below 30% of normal.
- Mild-to-severe life-threatening hemorrhages can occur, which include mucocutaneous, gastrointestinal, genitourinary, and intracranial bleeds.
- These include epistaxis, hematuria, gastrointestinal bleeding, spontaneous ecchymoses, and hematomas.
- Intracranial bleeds are associated with high mortality.
- Paradoxical thrombosis has also been reported following LAAR toxicity. This has been attributed to the depletion of proteins C and S.
Management of Rodenticide Poisoning
- If there has been no bleeding, but the PT is prolonged, give vitamin K1 10–50 mg orally two to four times a day For prolonged PT with less severe bleeding, give vitamin K1 10–15 mg SC or IM.
- In severe hemorrhage with prolonged prothrombin time (PT) give vitamin K1 (phytomenadione) 20 mg by slow IV injection In severe bleeding, it may be necessary to give fresh frozen plasma, cryoprecipitate, or fresh blood.
- N-acetylcysteine (NAC) has been used
- Extracorporeal membrane oxygenation (ECMO)
- Liver transplantation
Copper Sulfate Poisoning
Question 31. Discuss the clinical feature and management of copper sulfate poisoning.
Answer:
- Used as an insecticide (blue color copper sulfate crystals)
- The clinical features of copper sulfate poisoning include erosive gastropathy (hematemesis and melena), intravascular hemolysis, methemoglobinemia, hepatitis, acute kidney injury, and rhabdomyolysis
The management of copper sulfate:
- Reducing absorption—dilution, and neutralizing with milk
- Chelation therapy—penicillamine/BAL.
- Methemoglobinemia is treated with methylene blue
- Supportive therapy—transfusion, hemodialysis, hyperbaric oxygen.
Leave a Reply