Essentials Of Dental Caries Introduction
Dental caries is a progressive, irreversible, microbial disease affecting the hard tissues of the teeth exposed to the oral environment. It results in demineralisation of the inorganic constituents and the dissolution of the organic constituents. This leads to cavity formation.
Table of Contents
Dental caries is significantly important in pediatric dentistry. In children, periodontal disease is relatively rare and the incidence of malocclusion is less and occurs late. Dental caries is a major dental ailment compromising the health and function of primary teeth.
Read And Learn More: Paediatric Dentistry Notes
This, prevention, early management of initial carious lesions, restoration of established carious lesions, and rehabilitation of advanced carious lesions are the mainstay of pediatric dentistry practice.
The establishment of an infective focus, seeding of infection onto the developing permanent tooth, and spread of dentoalveolar infection are dental issues incited by dental caries. Loss of masticatory efficiency, compromised aesthesis, mispronunciation of labiodental sounds, and development of abnormal oral habits (following a prematurely extracted grossly carious tooth) are functional compromises arising due to carious primary teeth.
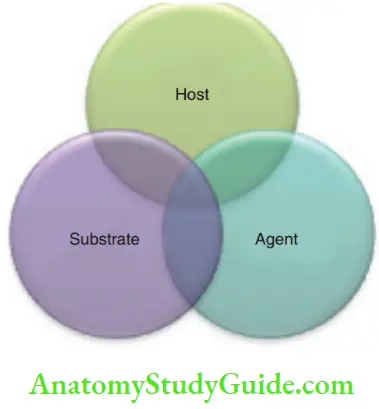
- Aetiology Of Dental Caries Dental caries is a multifactorial disease. Numerous factors have been clubbed into three major classes by Keyes and Fitzgerald. They described the etiology as the ‘Triad’. The three major factors that can cause dental caries are the host, agent, and substrate.
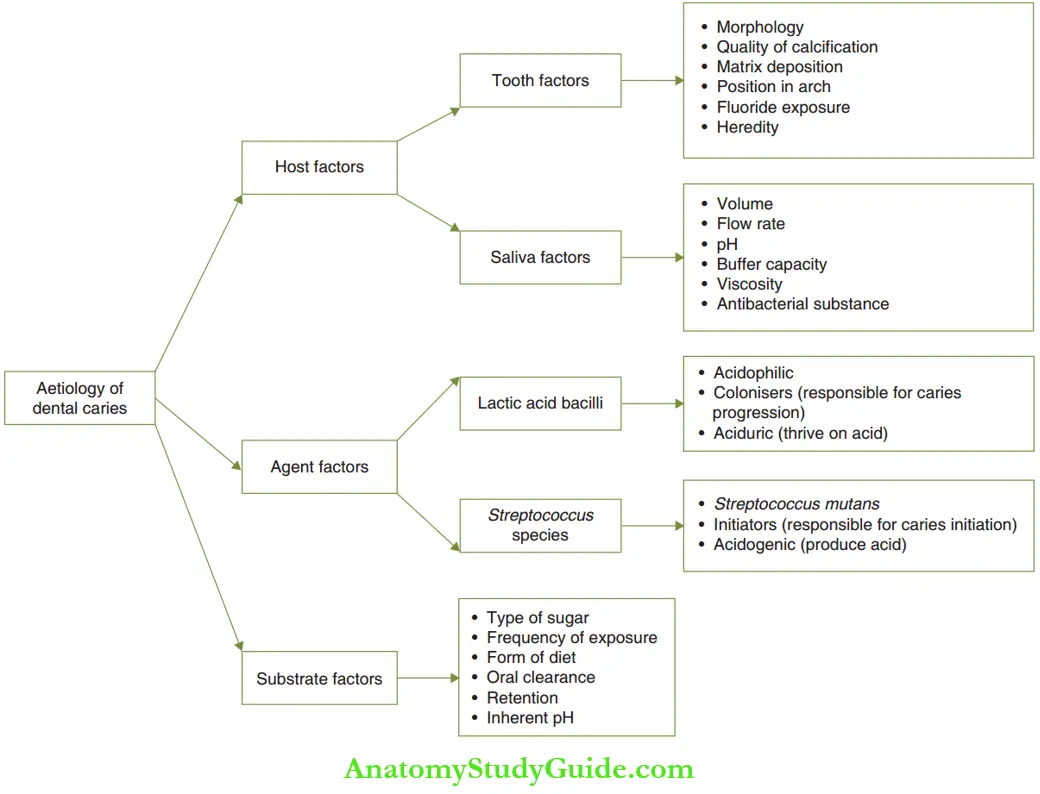
- Host factors pertain to the individual (host). They are discussed in Table.
- Tooth factors: Th morphology of the tooth, quality of calcification and matrix deposition play an important role in the incidence of caries. Apart from these, the position of the tooth in the arch, heredity, and fluoride exposure also influence the occurrence of caries.
- Salivary factors: These include volume, flow rate, buffering capacity, viscosity, and pH of saliva. Buffering capacity or the ability of saliva to prevent a decrease in pH is due to the bicarbonate ion concentration. Adequate buffering capacity will prevent a decrease in pH even with an increase in hydrogen ion concentration. The antibacterial substances in saliva include salivary lysozyme, lactoperoxidase, and IgA. The presence of these substances decreases caries incidence.
- Agent factors indicate the microbial agents causing the decay.
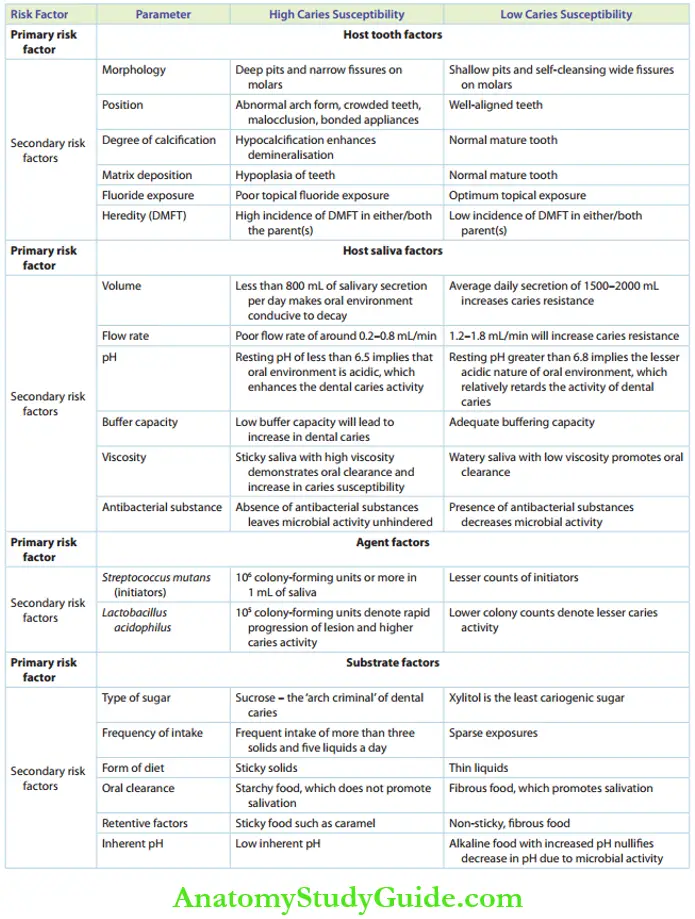
- Causative of initiation of decay or initiators: streptococcus species, especially Streptococcus mutans, are the initiators. They are acidogenic bacteria, that is, they produce acids. They are responsible for the initiation of caries. The initiators (Streptococcus species) are absent in the mouth of the newborn. They are demonstrated in the oral cavity only after the eruption of the first primary tooth. ‘Mutans streptococci’ is the term used to denote the seven species of streptococci of which one is S. mutans.
- Causative of progression of decay or colonizers: Colonisers are the acidophilic, lactic acid bacilli (LAB or lactobacilli) species. They are responsible for the progression of caries activity. Lactic acid bacilli are aciduric in nature, that is, they thrive on acids.
- Substrate factors are associated with the food
- Quality of diet: This refers to the type of sugar consumed. Sucrose is the ‘arch criminal’ of dental caries. It is the most cariogenic sugar as it has two high-energy bonds. Xylitol cannot be metabolised in the oral cavity. Hence, it is the least cariogenic sugar.
- Form of diet: Sticky solid food such as groundnut candy increases the susceptibility of caries, unlike thin liquids such as sugarcane juice.
- Frequency (eating habit): Frequent intake of more solids and liquids per day increases caries susceptibility when compared to sparse intake.
- Oral clearance of food: Starchy food does not promote salivation and hence increases caries. Fibrous food increases salivation, thus lowering caries susceptibility.
- Retentivity of food: Sticky food substances such as caramel adhere to the pits, thereby causing decay. Non-sticky and fibrous foods lower caries potential.
- Inherent pH: Th low inherent pH causes high susceptibility of caries. Alkaline food substances with an increased pH counter the inherent low pH due to microbial activity, thus lowering caries susceptibility.
- Table Summarises the role of each factor in the occurrence of caries. Newbrun (1982) added the fourth-factor ‘time’, thus converting the triad into a ‘tetrad’. The tetrad represents the primary risk factors of dental caries All the independent factors in each factor class are called secondary risk factors.

- Host factors pertain to the individual (host). They are discussed in Table.
- Pathogenesis
- The microbial initiators act upon a sugar substrate, that is, dietary carbohydrate. These sugars are metabolized by a glycolytic pathway, the end product of which is lactic acid. The lactic acid is produced in a few minutes following the ingestion of carbohydrates. The formation of acid implies an increase in hydrogen ion concentration or a decrease in the oral pH. This initiates demineralization of the enamel or dentin. The pathogenesis of dental caries is depicted.
- The tooth surface is made of hydroxyapatite [Ca(PO4)6(OH)2]. It is in equilibrium in a neutral environment saturated with calcium and phosphate. At a pH of 5.5 or lesser, H + ions react with the phosphate group in the aqueous environment. This converts phosphate to hypophosphate. The hydroxyapatite crystal, which contains hypophosphate instead of phosphate, then tends to dissolve quicker. This process is described as demineralization.
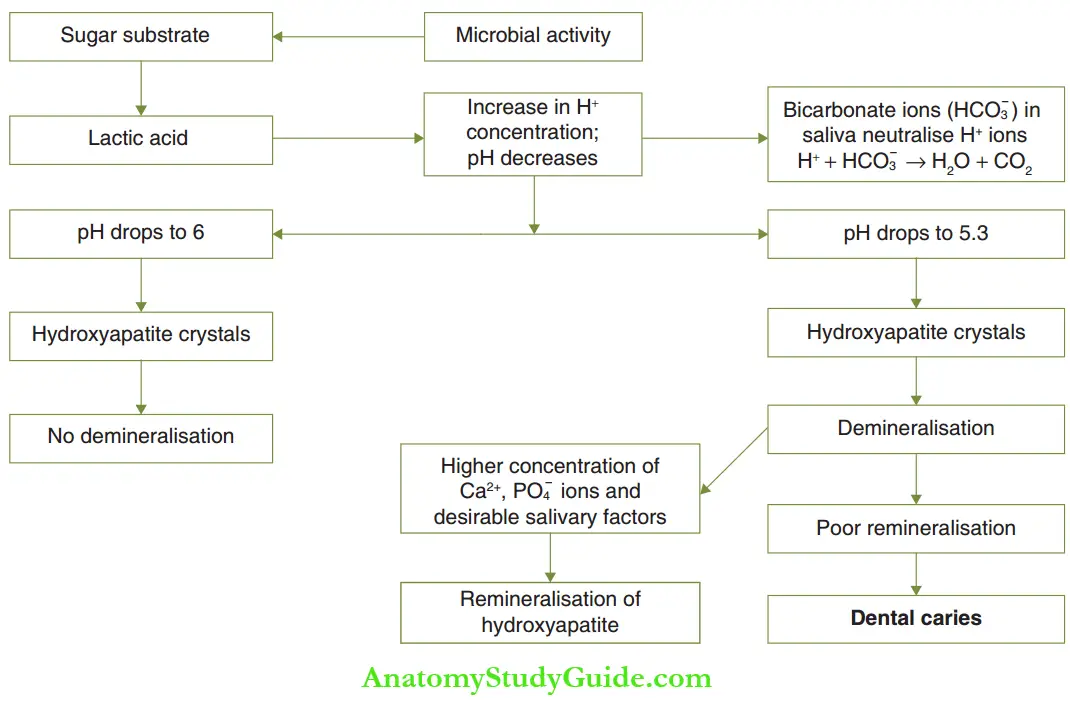
- The dissolution of hydroxyapatite is less likely to happen at an acidic pH, ranging from 5.5 to 7. A pH of 5.5 or below, at which demineralisation is set to occur, is termed critical pH. It is called Stephan’s constant.
- An acidic pH can be converted into a neutral pH of around 7 by the saliva. A common ion effect is demonstrated in a neutral pH environment when there are sufficient calcium and phosphate ions in the immediate surroundings. This inhibits hydroxyapatite dissolution and enables the rebuilding of partly dissolved apatite crystals. This is termed remineralization.
- Dental caries occurs due to a prolonged imbalance between demineralization and remineralization in the oral cavity. The demineralizing factors overwhelm the remineralization over a period of time. The ‘time’ taken for the imbalance to incur, causing frank dental decay, can be related to the fourth factor given by Newbrun, the ‘time’ factor in Newbrun’s tetrad.
Susceptibility To Dental Caries
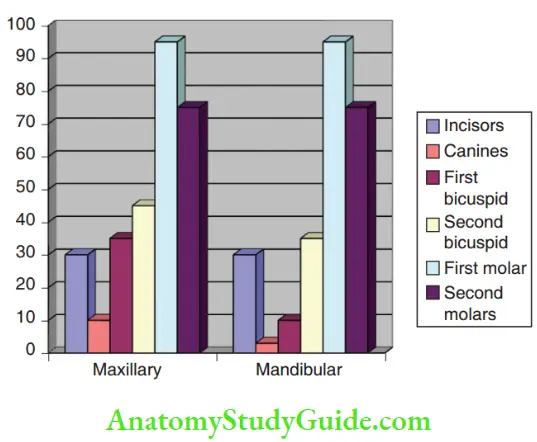
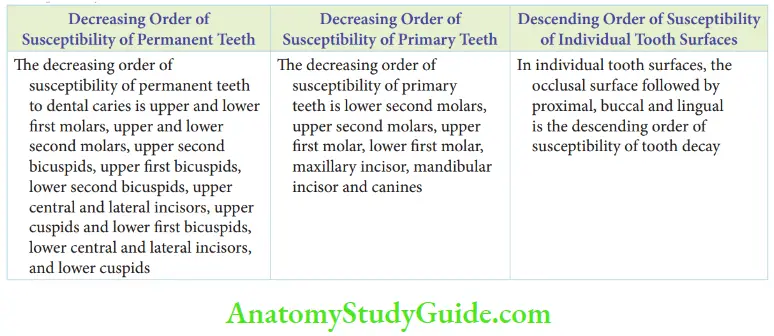
Maxillary teeth have been reported to be more commonly attacked by dental caries than mandibular teeth. However, the difference is marginal. This may be due to the fact that saliva tends to pool around mandibular teeth because of gravity. The buffering activity of saliva prevents demineralisation.
The individual permanent and primary tooth susceptibility charts are shown.
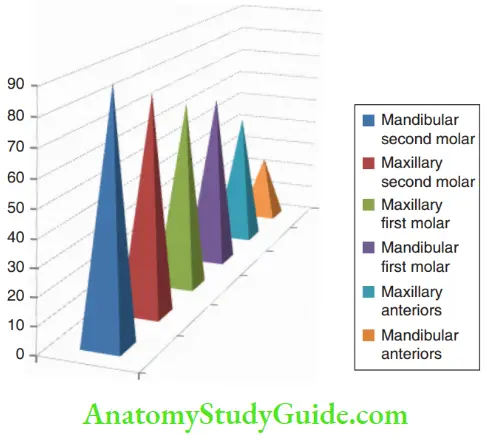
- The second molars are more susceptible to dental caries than the first molars although they erupt later than the first molars. It is most probably because of the following reasons:
- The length of officers per unit occlusal surface area is greater in second molars.
- The depth of pits is greater.
- Buccal pits are also deep. (They are absent on maxillary and mandibular first permanent molars.)
In individual tooth surfaces, the occlusal surface is more susceptible to caries followed by proximal, buccal, and lingual surfaces in descending order. It is due to the fact that substrate retentive pits and fissures are present on the occlusal surfaces. The proximal surfaces are not directly exposed at tooth brushing.
So, they are prone to decay after occlusal surfaces. Buccal and lingual surfaces have fissures and pits extending from occlusal surfaces. Buccal pits are deeper than lingual pits, which make buccal surfaces more prone to decay than lingual surfaces.
Terminologies In Cardiology
Specific terms are used to denote the location or activity or rate of progression of the dental caries.
- Occult Caries (Hidden Caries) Occultcaries or hidden caries is where the occlusal surface of the tooth appears intact and caries cannot be clinically identified. Occult caries is common in the mandibular permanent molars, most specifically the first molar. It has been reported to be prevalent to a range of 2.2–50%. Occult caries can occur in the pre-eruptive stage as well as in the post-eruptive stage. Pre-eruptive occult caries or simply pre-eruptive caries is identified in the unerupted molars on an OPG. They appear as radiolucencies under an intact occlusal surface. It has been described as an intracoronary resorption process. No treatment can be carried out till the eruption of the tooth. Pulp involvement and dentoalveolar abscess formation may possibly coincide with the tooth eruption. Post-eruptive occult caries can be identified with the help of bitewing radiographs. However, it is difficult to determine if it is a post-eruptive hidden caries or an existing pre-eruptive hidden caries. Post-eruptive caries is a carious process where an intact occlusal surface and a pronounced sub-surface demineralization coexist. The th surface is intact due to an enhanced remineralisation process resulting from topical fluoride exposure by dentifrices. The lesion may ‘explode’ into a symptomatic tooth resulting from pulpal/periradicular pathology as the cause is concealed and active. Hence, the lesion is also referred to as a ‘fluoride bomb’. The lesion may be explored by cavitating through the intact occlusal surface, and appropriate pulpal treatment or restorative management can be carried out.
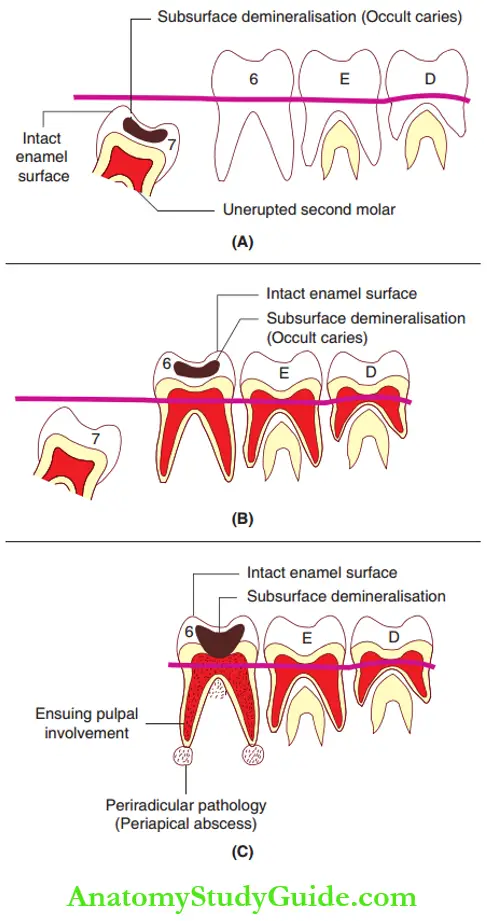
1. (A) on an unerupted second molar,
2. (B) on an erupted first molar and
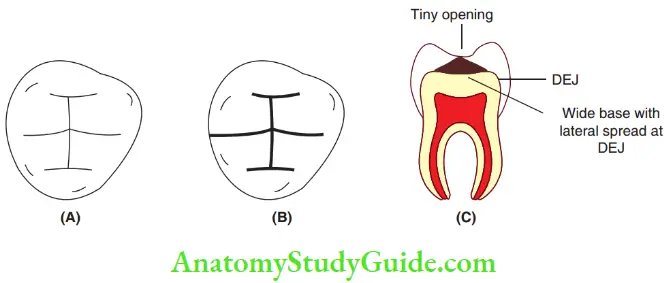
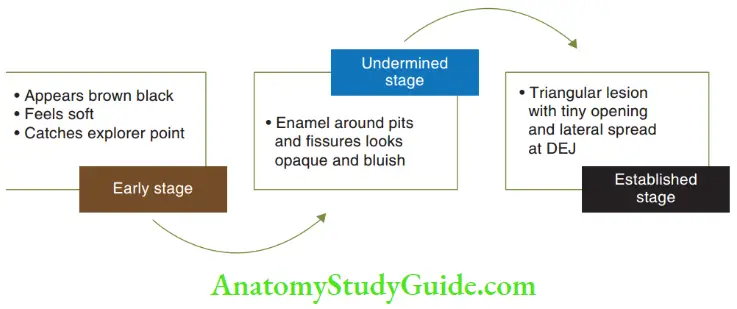
2. (C) ensuing into pulpal and periradicular pathology. - Pit And Fissure Caries The carious pit and fissures may appear brown or black\ in the early stages. The lesion feels slightly sof and catches a fie explorer point. Th enamel bordering the pit or figure may appear opaque and bluish-white as it becomes undermined. This undermining occurs due to the lateral spread of caries at the dentin enamel junction. This, there may be a large surface area of carious involvement with only a tiny point of opening simulating a triangle.
- Smooth Surface Caries Smooth surface caries involve the tooth surface that is devoid of pits and fissures. Proximal caries occurring on mesial/distal surfaces and cervical caries occurring on buccal (labial) and lingual (palatal) surfaces are smooth surface caries lesions. They are generally preceded by the formation of dental plaque. Proximal caries begin just below the contact point. In the early stage, it appears as a faint, white opacity of the enamel without apparent loss of continuity of the enamel\ surface. This white, chalky spot becomes slightly roughened owing to superficial decalcification of the enamel. As caries penetrate the surface, the enamel surrounding the lesion assumes a bluish-white appearance. Cervical caries extend from the area opposite to the gingival crest occlusal to the convexity of the tooth surface on buccal (labial) or lingual (palatal) surfaces. Thus, a typical cervical carious lesion is a crescent-shaped cavity. It begins as a slightly roughened chalky area that gradually becomes excavated.
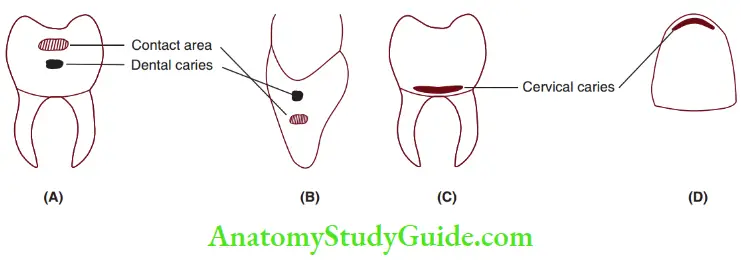 1. (A) molar/premolar and
1. (A) molar/premolar and
2. (B) incisor/canine. Cervical caries on
3. (C) molar/premolar and
4. (D) incisor/canine.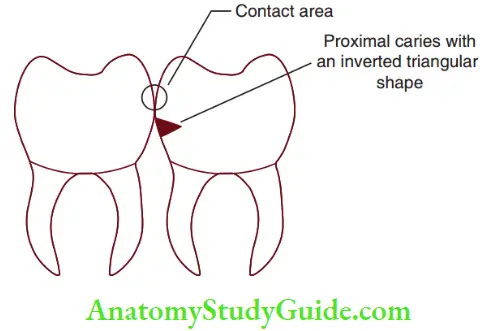
- Acute Dental Caries Acute dental caries run a rapid clinical course and result in early pulp involvement. The process is so rapid that there is little time for the deposition of secondary dentin. The dentin is usually stained light yellow. Rampant caries is a kind of acute dental caries affecting children.
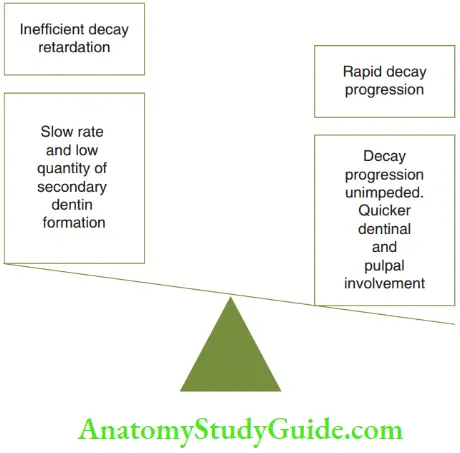
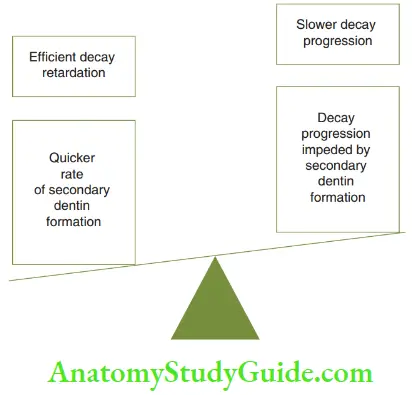
- Chronic Dental Caries Chronic caries progresses slowly and tends to involve the pulp much later than does acute caries. Carious dentin is often stained deep brown. The cavity is generally shallow with a minimum softening of dentin. There is little undermining of enamel. Symptoms such as sensitivity, pain on stimulation, or spontaneous pain are not common features of chronic caries unlike in acute caries.
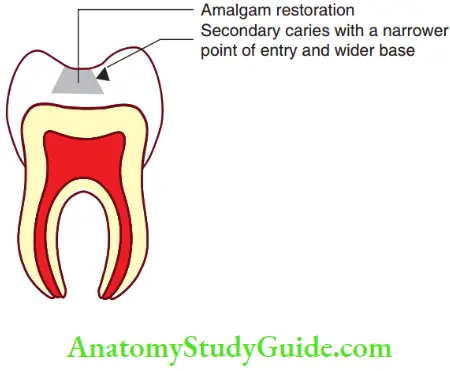
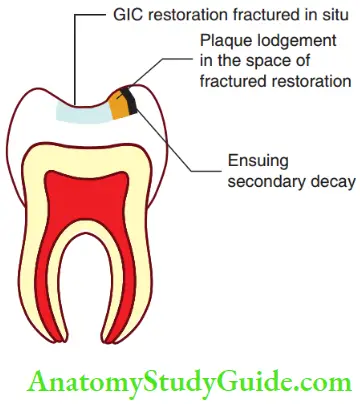
- Recurrent Caries Caries that occur in the immediate vicinity of a previous restoration is called recurrent caries. It usually occurs due to inadequate extension of the original restoration. The renewed caries follow the same general pattern as the primary caries, that is, as a triangular pattern, with the narrow apex at the point of entry and a broader base into enamel/dentin. Recurrent caries occurs with fractured amalgam and composite restorations. Fractured GIC and RMGIC restoration do not get infected with secondary decay easily owing to the fluoride release from the restoration. However, when the portion of fracture of fluoride-releasing cement is larger, secondary caries may ingress from the margin not in contact with the fractured restoration.
- Arrested caries Caries that become static or stationary and do not show any tendency for further progression is called arrested caries. It commonly occurs on occlusal surfaces. It is characterized by a large, open cavity in which there is lack of food retention. The superficially softened and decalcified dentin is gradually burnished until it becomes a brown-stained, polished, hard surface. This has been described as the eburnation of dentin. Topical fluoride application from dentifrices and food materials adds to the remineralization of the carious surface. Arrested caries can sometimes be seen on the proximal surfaces of teeth where the adjacent tooth has been extracted.
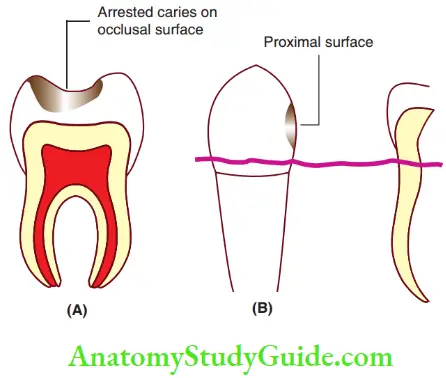 1. (A) Arrested caries on the occlusal surface and
1. (A) Arrested caries on the occlusal surface and
2. (B) arrested caries on the proximal surface of tooth with adjacent edentulous spaces - Radiation caries The development of rampant caries in patients undergoing radiation therapy in the head and neck region is referred to as radiation caries. Del Regato, in 1939, observed that xerostomia was a complication of radiation therapy and postulated that caries development may be due to modification of salivary secretion. As a consequence of irradiation, three forms of dental defects have been described by Frank et al. in 1965.
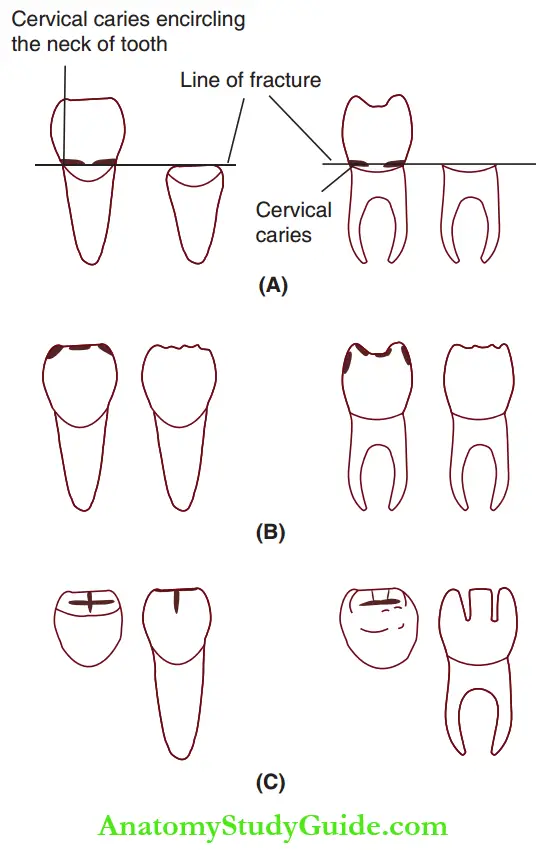
1. (A) Cervical caries encircling the neck of the tooth.
2. (B) Discolouration and wearing away of incisal and occlusal surfaces.
3. (C) Caries at incisal or occlusal edges spreading into labial/buccal and palatal/lingual surfaces.- The caries-like lesions usually completely encircle the neck of the tooth. Amputation of the crown may occur in this type of lesion.
- The second type of lesion begins as brown to black discoloration of the crown. The occlusal surfaces and incisal edges wear away.
- The third type of lesion begins as a spot depression, which spreads from the incisal or occlusal edges on labial/buccal or lingual surfaces.
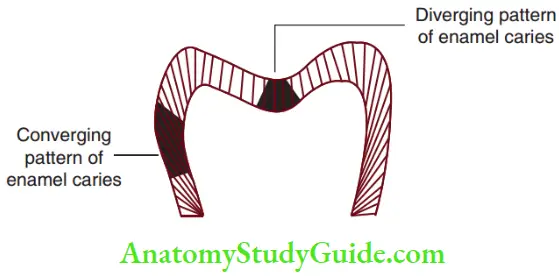
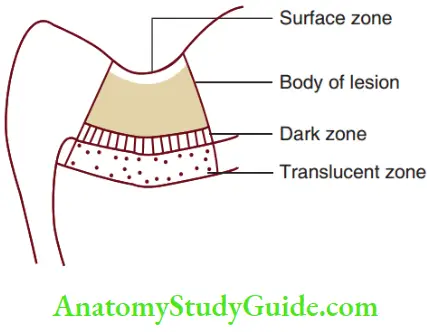
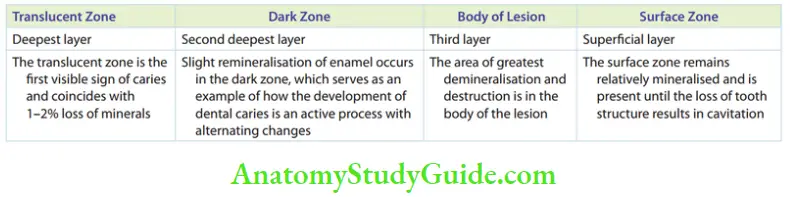
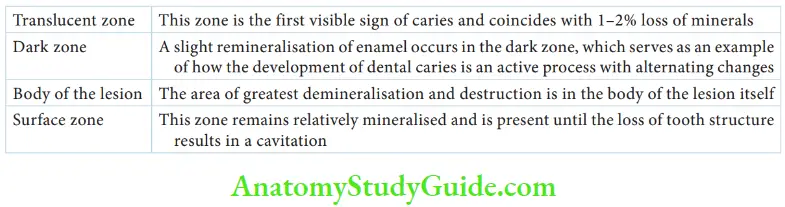
- Enamel Caries Enamel rods in the enamel structure run perpendicularly from the tooth surface towards the dentin. Demineralization of the enamel by acid follows the direction of these enamel rods. This permits the bacteria to penetrate the dentin. The involvement of enamel by caries follows the direction of the enamel rods. Two different triangular patterns are observed – converging in proximal surfaces and diverging at pits and fissures. These patterns are coherent with the enamel rods’ orientation. The loss of enamel crystals and progression of dental caries can be visualized in four distinct zones under a light microscope. From the deepest layer of the enamel to the enamel surface, four relatively discreet zones, namely the translucent zone, dark zone, the body of the lesion, and surface zone, can be identified. There is demineralization below the intact surface layer. This is referred to as subsurface demineralisation.
- Dentinal Caries Dentinal caries begins with the spread of the process along the dentin enamel junction. There is a rapid involvement of more dentinal tubules, each tubule acting as a tract leading to the pulp. Dentinal changes can be described clearly as early and late changes.
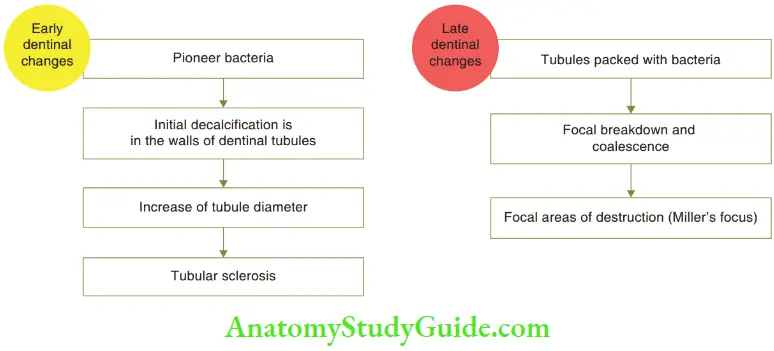
- Early changes: Initially, few bacteria invade the dentinal tubules before any carious alteration takes place in the dentin. These forefront bacteria are called pioneer bacteria. Distinctly, only one type of bacteria is present in each tubule. As microorganisms penetrate deep into the dentin, they get separated from their carbohydrate source. Still, the bacteria thrive on the high protein content of the tubule. th bacteria erode the walls of the dentinal tubules by decalcification. This enhances the tubule diameter. The decalcification is very high to the extent that it appears in coherence with the intertubular substance resembling a plain sheet of glass. This change is called sclerosis of dentin.
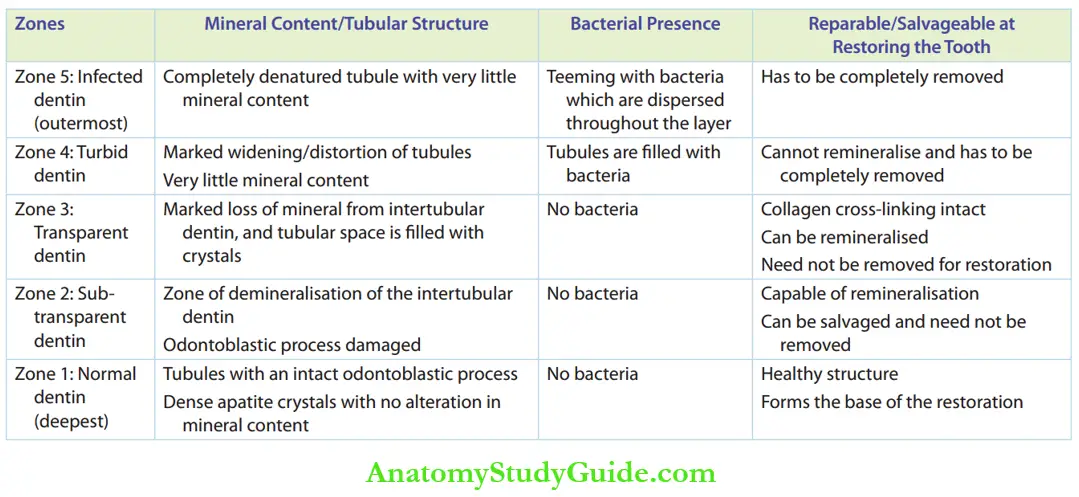
- Late changes: The diameter of the tubule increases as the bacteria get packed into them. There is focal coalescence and breakdown of dentinal tubules. Ovoid areas of destruction parallel to the course of tubules filed with necrotic debris further expand the size of the tubule. This produces compression and distortion of the adjacent tubules. This is described as the liquefaction foci of Miller. Dentin being part of pulp–the dentin complex is able to mount a reparative response. The various zones of dentinal caries are normal dentin (most deep), sub-transparent dentin, transparent dentin, turbid dentin, and infected dentin (most superficial). Affected dentin is the dentin that is altered and can be salvaged. It is the soft demineralized dentin that is not yet invaded by bacteria. It includes zones 1, 2, and 3 – transparent, sub-transparent, and apparently normal zones. It lies beneath the infected dentin and is usually not removed during cavity preparation in anticipation that this part of the dentin will get remineralized. Infected dentin is the dentin that is altered and has to be removed during cavity preparation. It is the soft demineralized dentin contaminated with bacteria. The collagen is irreversibly denatured and there is no possibility of remineralisation. It is dark brown or black in color. It includes zones 4 and 5.
- Root-Surface Caries (Caries Over Cementum And Dentin) Root caries is similar to enamel caries demonstrating sub-surface demineralisation. Unlike enamel caries, the surface may appear softened at an early stage of lesion development. Bacteria penetrate at an earlier stage than in enamel caries. The surface layer of caries over cementum is relatively well mineralised. Interestingly, although these lesions may appear rather extensive (wide), they are seldom more than 0.5–1 mm deep. This slow rate of bacterial invasion and tissue degradation gives the opportunity for these lesions to be arrested by plaque control with fluoride toothpaste. The first international conference on the declining prevalence of dental caries was held at the Forsyth Dental Centre in Boston in June 1982. The incidence of caries and the impact of dental education, dental research, and dental practice were evaluated. AdeclineinthecariesprevalencewasfoundinUS, UK, Denmark, Ireland, Netherlands, Norway, Scotland, and Sweden. The cause for this widespread decline in the prevalence of dental caries is multifactorial. However, the use of refined carbohydrate foods had increased more rapidly in these countries than the knowledge of oral hygiene and the increase in dental manpower.
Essentials Of Dental Caries Summary
- Dental caries is a multifactorial disease. The causative agents are enlisted in Table.
- The pathogenesis of dental caries can be summarised as follows:
- A sugary substrate that is acted on by the microbial initiators.
- The sugars are metabolized by the microbial glycolytic pathway.
- The end product of glycolysis is lactic acid.
- The formation of acids implies an increase in hydrogen ion concentration (H +) or a decrease in pH.
- The hydrogen ion can initiate a demineralization of enamel/dentin.
- Susceptibility to dental caries
- The zones in enamel caries are as follows:
- The changes in dentinal caries are as follows:
- Early dentinal changes: Sclerosis in case of mild, slowly progressing caries with pioneer bacteria. Initial decalcification in the walls of dentinal tubules with each tubule having one specific group of microorganism.
- Late dentinal changes: As bacteria get packed into the tubule, there is focal coalescence and breakdown of few dentinal tubules. This is called the liquefaction foci of Miller.
Leave a Reply