Small And Large Intestines
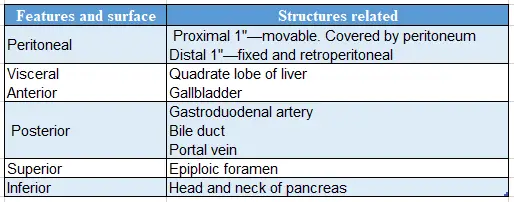
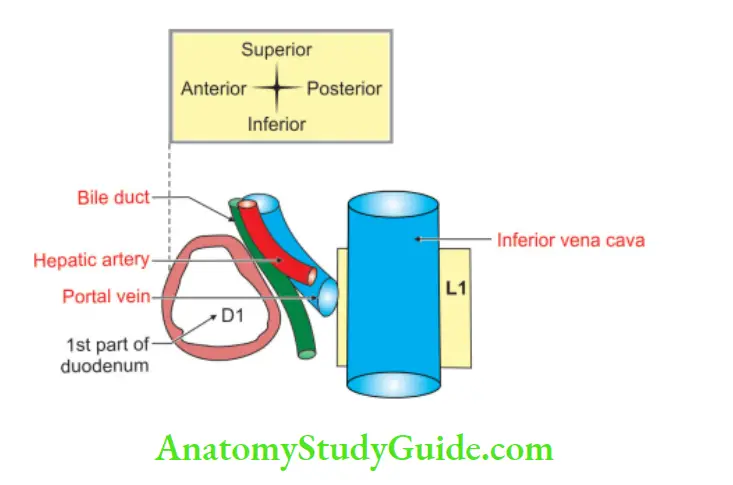
Relations of 1st part of duodenum
Relations of 1st part of the duodenum:
Table of Contents
Read And Learn More: General Histology Question And Answers
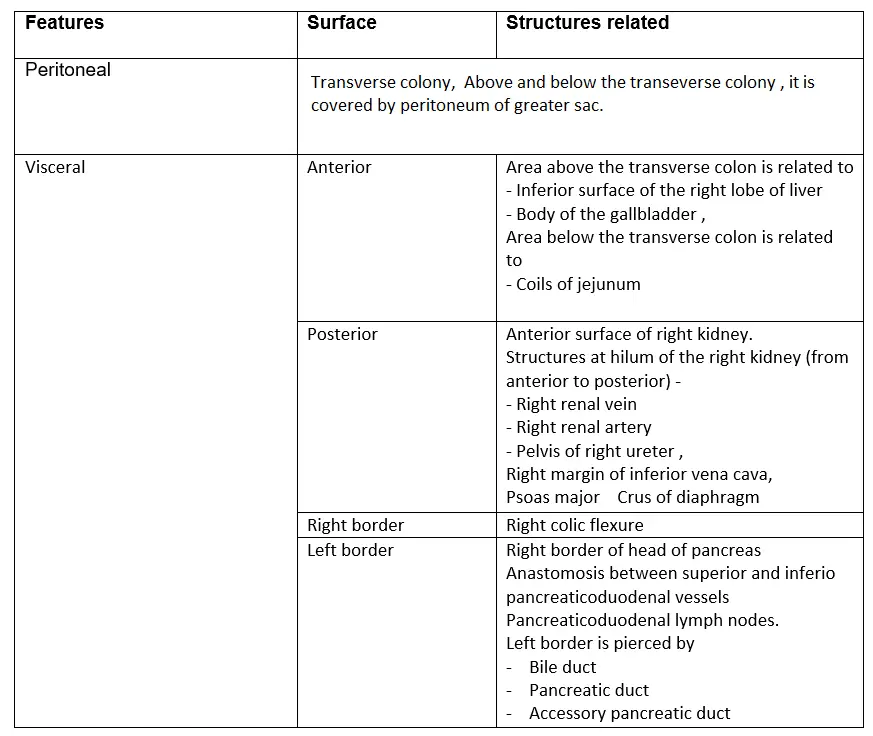
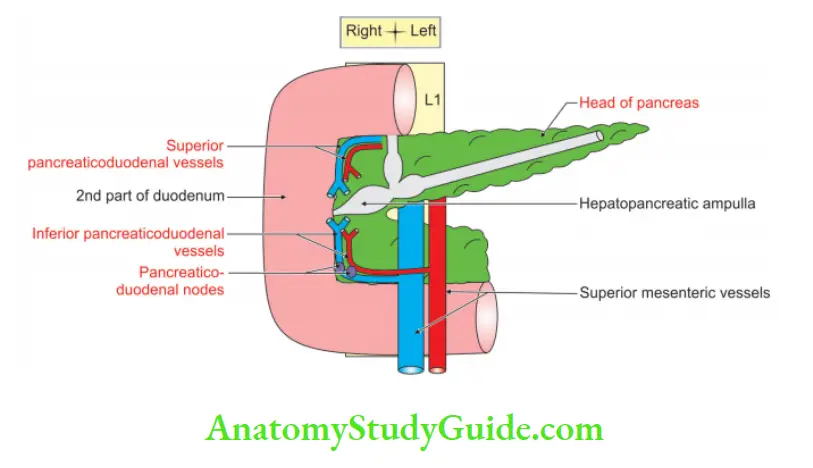
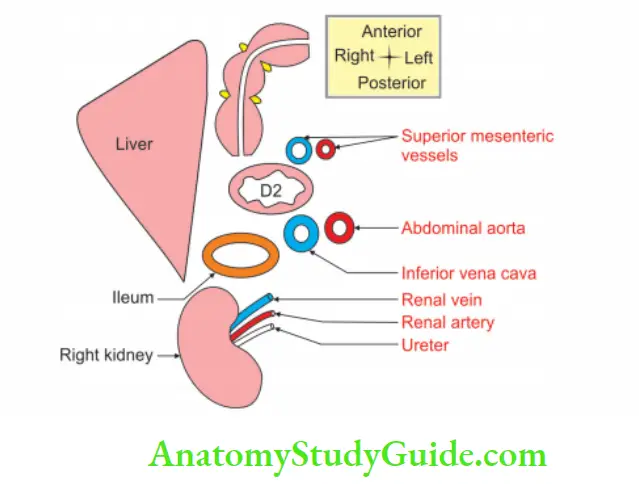
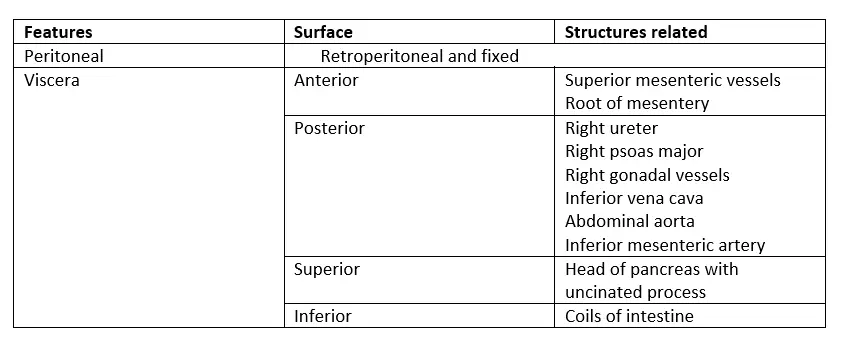
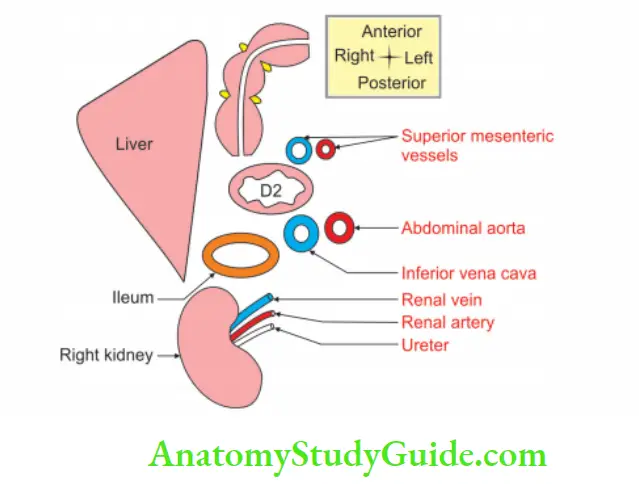
Relations of 2nd part of duodenum
Relations of 2nd part of the duodenum:
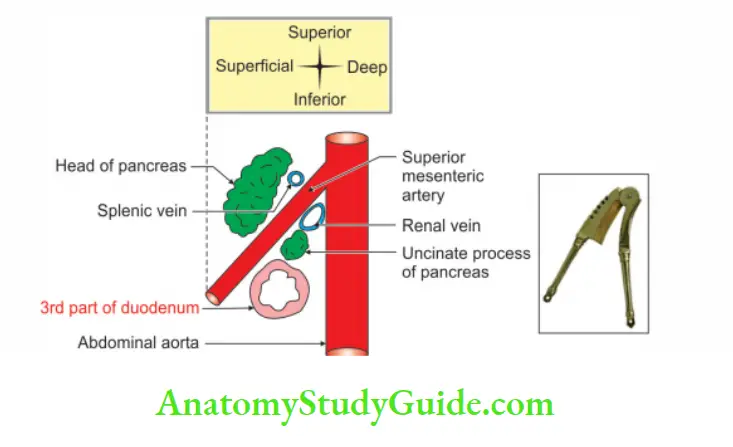
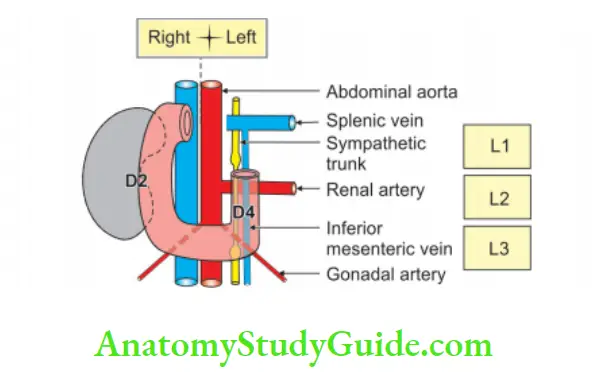
Relations of 3rd part of duodenum
Relations of 3rd part of the duodenum:
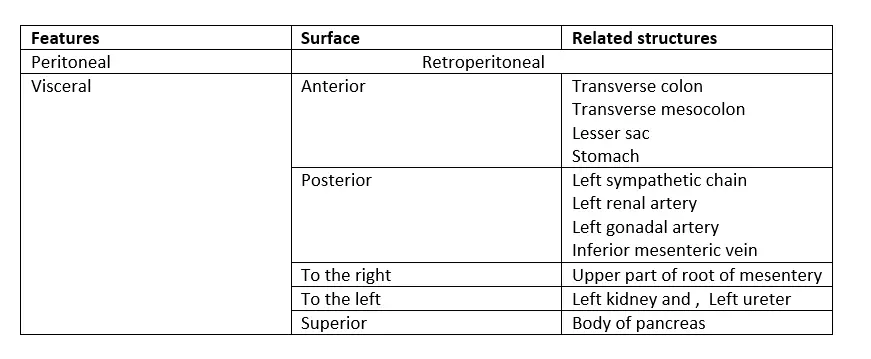
Relations of 4th part of duodenum
Relations of 4th part of the duodenum:
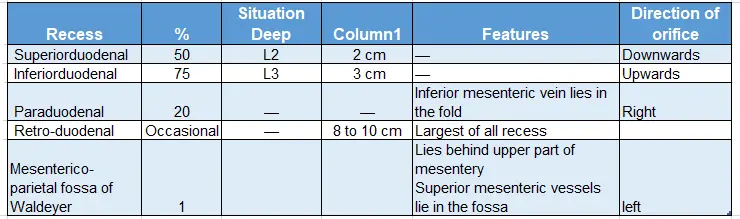
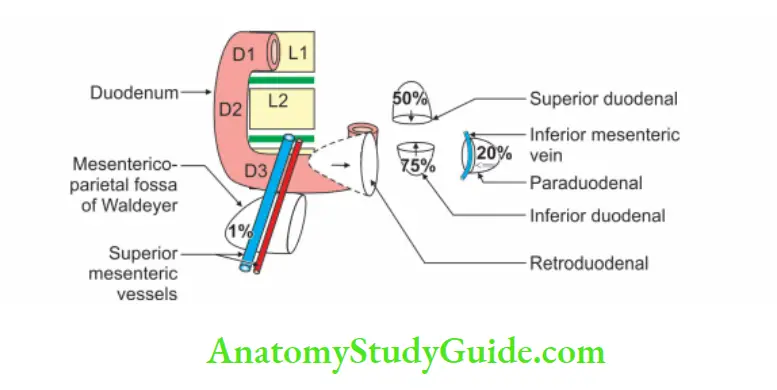
Peritoneal Recesses Around Duodenum
Peritoneal recesses around the duodenum:
Question -1: Describe 2nd part of the duodenum under following heads
1. 2nd part of the duodenum Gross anatomy
2. 2nd part of the duodenum Histology
3. 2nd part of the duodenum Development, and
4. 2nd part of the duodenum Applied anatomy.
Answer:
2nd part of the duodenum Introduction: It is the junction of the foregut and midgut.
1. 2nd part of the duodenum Gross anatomy
2nd part of the duodenum Internal features: The interior of the 2nd part of duodenum shows the following special features.
2. 2nd part of the duodenum Location: It is present in umbilical region on the right margin of 2nd lumbar vertebra.
Plica circularis: It is longitudinal fold present below major duodenal papilla.
The major duodenal papilla:
- It is an elevation present posteromedially.
- It is 8 to 10 cm distal to the pylorus.
- The hepatopancreatic ampulla opens at the summit of the papilla.
The minor duodenal papilla:
- It is present 6 to 8 cm distal to the pylorus.
- It has the opening of the accessory pancreatic duct.
3. Relations: It is described as
Peritoneal relations: It is retroperitoneal and most fixed part of duodenum.
- The anterior surface is related to
- Transverse colon.
- Above and below the transverse colon, it is covered by peritoneum of greater sac.
- The posterior surface is non-peritoneal.
Visceral relations:
1. Anterior surface: It is divided into
Area above the transverse colon is related to
- Inferior surface of the right lobe of liver.
- Body of the gallbladder.
Area below the transverse colon is related to coils of jejunum.
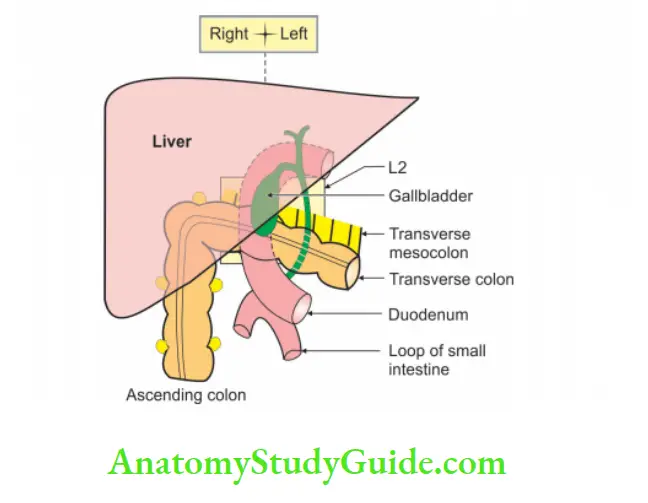
2. Posterior surface:
Anterior: Anterior surface of right kidney
Structures at hilum: Structures at hilum: of the right kidney (from anterior to posterior) — VAU
- Right renal Vein (V)
- Right renal Artery (A)
- Pelvis of right Ureter (U)
Right:
- Margin of inferior vena cava
- Psoas major
- Diaphragm
3. Right border: Right border is related to right colic flexure.
4. Left border: Left borde is related to head of pancreas in its entire course.
1. Anastomosis between the superior and inferior pancreaticoduodenal vessels.
2. Pancreaticoduodenal lymph nodes. It is pierced by
- Bile duct
- Pancreatic duct, and
- Accessory pancreatic duct.
4. 2nd part of the duodenum Blood supply:
2nd part of the duodenum Arterial supply:
Part of the duodenum above the opening of bile duct is – A.
- It belongs to foregut.
- The artery of the foregut is coeliac trunk.
- It gives hepatic artery> gastroduodenal artery > superior pancreaticoduodenal artery which supplies area A.
Part of the duodenum below the opening of bile duct is – B.
- It belongs to Midgut.
- The artery of the midgut is superior mesenteric artery > inferior pancreatico-duodenal artery which supplies B.
Venous drainage:
- Superior pancreaticoduodenal vein > portal vein.
- The inferior pancreaticoduodenal vein drains into a superior mesenteric vein.
5. 2nd part of the duodenum Nerve supply:
- Sympathetic nerves: They arise from spinal segments of T9 and T 10.
- Parasympathetic nerves: They arise from vagus nerves.
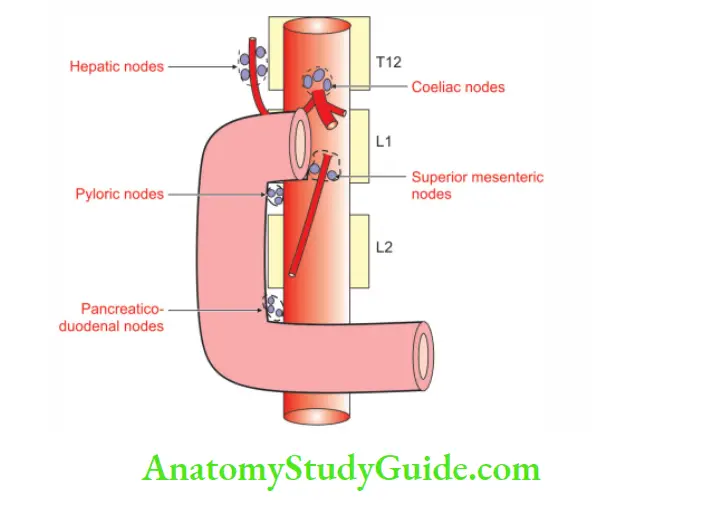
6. 2nd part of the duodenum Lymphatic drainage: Lymph vessels drain into
1. Pancreaticoduodenal lymph nodes.
2. Pyloric lymph nodes: The efferent lymphatics go to
- Coeliac group of lymph nodes.
- Superior mesenteric group of pre-aortic lymph nodes.
2. 2nd part of the duodenum Histology
1. 2nd part of the duodenum Features:
1. The luminal surface has numerous folds. They project into the lumen. They are called plicae circularis. These folds consist mucosa and submucosa.
2. The mucosa shows numerous fingers-like projections. They are called intestinal villi.
3. Each villus has
- Lamina propria, and
- Epithelium.
4. Brunner’s gland in submucosa is the feature of duodenum. It has columnar cells with flat nuclei.
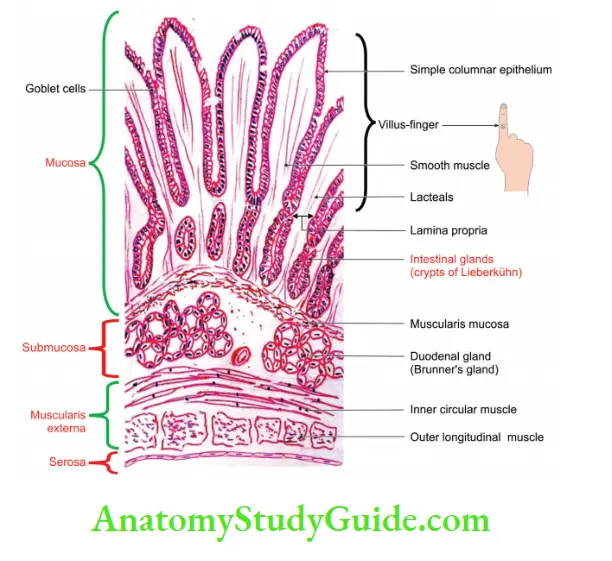
2. It has four coats:
Mucous coat containing:
- Simple columnar epithelium with intestinal glands.
- Lamina propria.
- Muscularis mucosa.
Submucosa containing Brunner’s glands: It secretes alkaline mucus which protects acidic chyli.
Muscularis externa: Muscularis externa containing smooth muscles, namely
- Inner circular, and
- Outer longitudinal.
Serous coat: Serous coat is lined by simple squamous epithelium or adventitia.
3. 2nd part of the duodenum Development
1. Chronological age: It develops in the 4th week of intrauterine life.
2. Germ layer: Endoderm and mesoderm.
3. Site: Caudal part of foregut.
4. Sources:
1. The epithelium of the 2nd part of duodenum
- Above the opening of bile duct develops from endoderm of the foregut.
- Below the opening of the bile duct develops from endoderm of the midgut.
2. All the coats of duodenum except epithelium and glands develop from intraembryonic splanchnopleuric mesoderm.
5. Sequence of events: During rotation, the dorsal mesentery disappears except 1”
near pyloric end and the duodenum becomes retroperitoneal organ.
6. Anomalies:
Abnormal fixation: There is no functional disturbance.
Excessive fixation: Excessive fixation may cause interference with mobility, kinks, and compression of the lower bowel.
Failure of fixation: Failure of fixation may cause ptosis, torsion or volvulus.
Abnormal rotation: Abnormal rotation predisposes to volvulus, which causes internal obstruction. Such obstruction is particularly likely to occur within the 1st few days of life (volvulus neonatorum).
During rotation: During rotation of the stomach, the duodenum also rotates to the right and forms a superior retention band, which fixes it at the junction of duodenum with jejunum. The superior retention band becomes the suspensory ligament of the duodenum.
Temporary blockage: There is temporary blockage of duodenal lumen by proliferation of endoderm. The lumen is re-established after some time. The failure of the formation of the lumen leads to atresia.
4. 2nd part of the duodenum Applied anatomy
1. Duodenal diverticula are fairly frequent. They are generally seen at the point of entry of arteries.
2. Congenital stenosis and obstruction may occur at the site of opening of the bile duct. Other causes of obstruction include
- Annular pancreas.
- Pressure by superior mesenteric artery.
- Constriction of suspensory muscle of duodenum.
3. Second part is most protected from the external injury, since it is situated behind the forward curvature of the vertebral column in the paravertebral gutter.
4. Sometimes Small bile stones may be impacted on the summit of the major papilla producing obstructive jaundice.
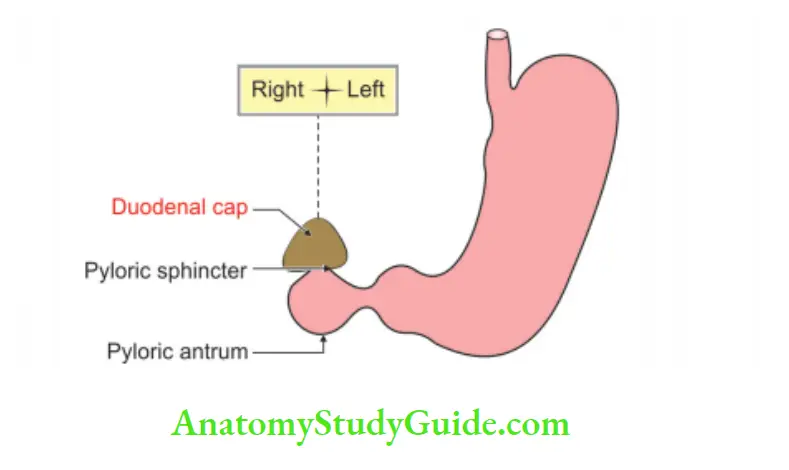
Duodenal cap
Duodenal Cap Definition: The barium meal X-ray of the digestive tract shows a smooth lar shadow. It is seen in the 1st part of duodenum. It is called duodenal cap. It has a base and an apex. The base is below and apex is above.
1. The following anatomical factors appear to be responsible for it.
2. The 1st part of the duodenum runs upward, backward and to the right to continue as the 2nd part.
3. The knob-like pylorus invaginates into the 1st part of the duodenum. This is kept open and filled with barium paste.’
4. The mucous membrane of proximal half of duodenum is devoid of circular folds.’
5. The proximal half of the 1st part of the duodenum is mobile. Because it has mesentery.
6. The viscosity of the barium sulphate coming out of a narrow pyloric canal gives a conical appearance.
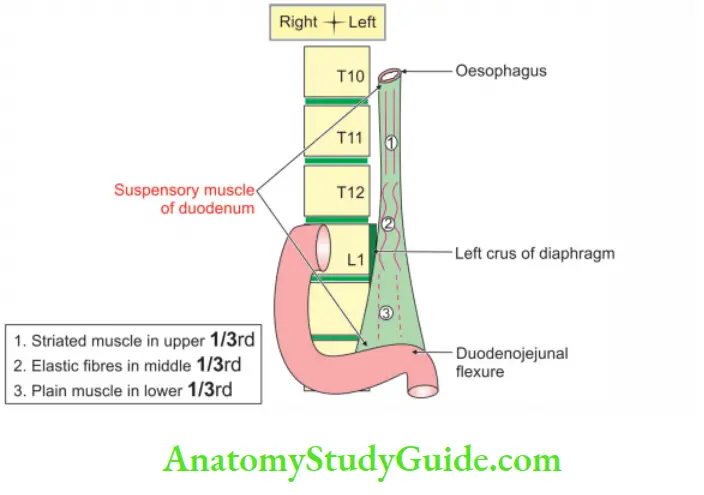
Ligaments of Treitz (suspensory muscle of duodenum)
Ligaments of Treitz Introduction: It is the fibromuscular band extending from right crus of the diaphragm to the duodenojejunal flexure.
1. Ligaments of Treitz Formation: It is formed in
- Upper part by striped muscle fibres.
- Middle part by elastic fibres.
- Lower part by smooth muscle fibres.
2. Ligaments of Treitz Importance:
- It marks the duodenojejunal junction.
- If it is attached only to flexure, its contraction may narrow the angle of flexure, causing partial obstruction of gut.
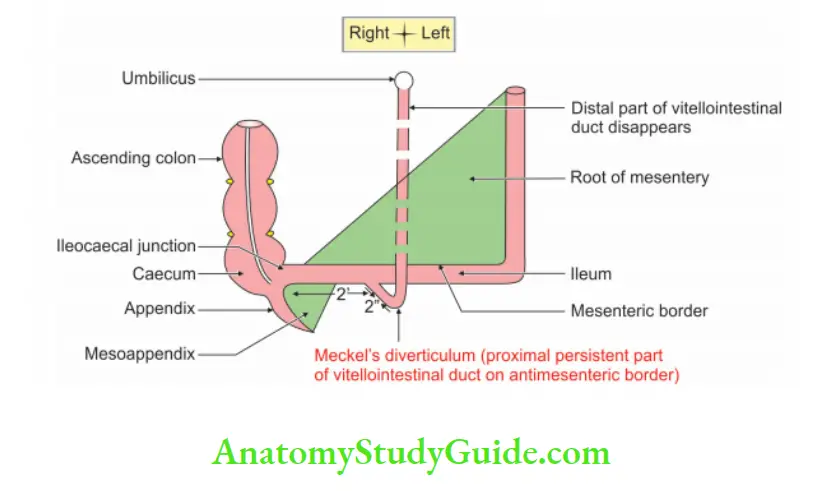
Meckel’s diverticulum
Meckel’s diverticulum Introduction: This is the persistent proximal part of the vitellointestinal duct.
1. Meckel’s diverticulum Gross anatomy:
1. Meckel’s diverticulum Situation: It is located at the anti-mesenteric border of the ileum.
2. Rule of 2
- Length: 2″
- Distance from the ileocaecal valve: 2′.
- Incidence: 2% of the population.
3. Its caliber is equal to that of ileum.
4. Its apex may be free or may be attached to the umbilicus or any other abdominal structure.
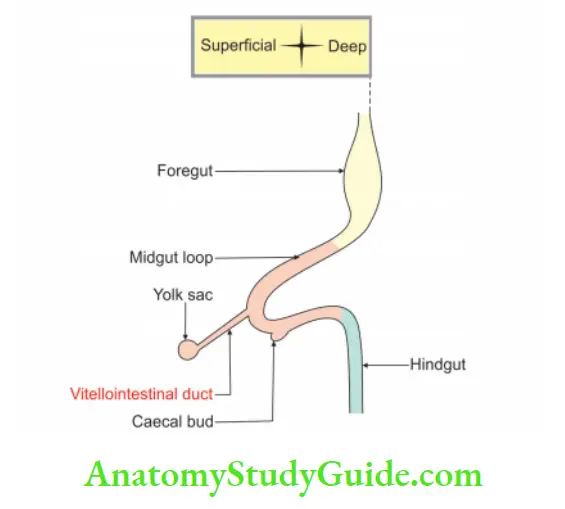
2. Meckel’s diverticulum Content: It contains
- Pancreatic tissue, and
- Gastric mucosa.
3. Meckel’s diverticulum Applied anatomy:
- It is one of the most common congenital anomalies of the gastrointestinal tract.
- It is responsible for intestinal obstruction and intussusception.
- It may enter into hernial sac.
- It is one of the differential diagnoses of appendicitis.
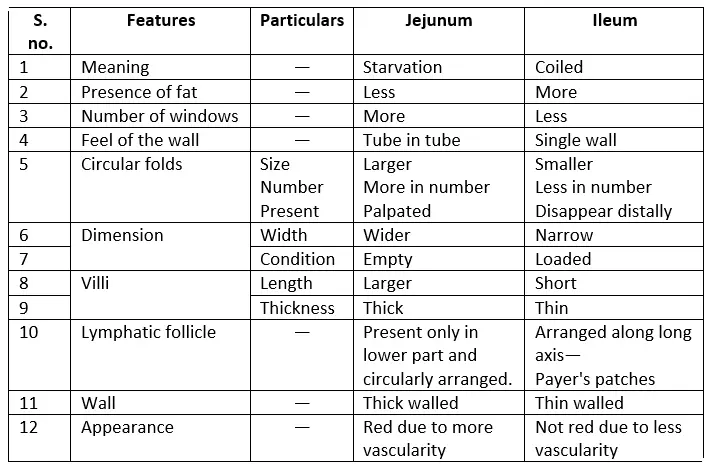
Question – 2: Differences between jejunum and ileum
Answer:
Differences between jejunum and ileum:
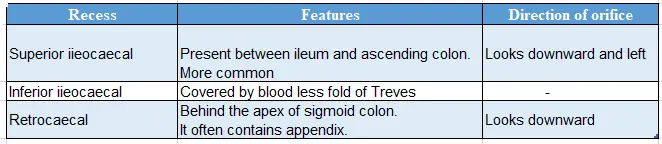
Peritoneal recesses around the caecum
Peritoneal recesses around caecum:
Question – 3: Describe Caecum under following heads
1. Caecum Gross anatomy, and
2. Caecum Applied anatomy.
Answer:
Caecum Introduction: It is the proximal end of the large intestine where the large and small intestines meet.
1. Caecum Gross anatomy
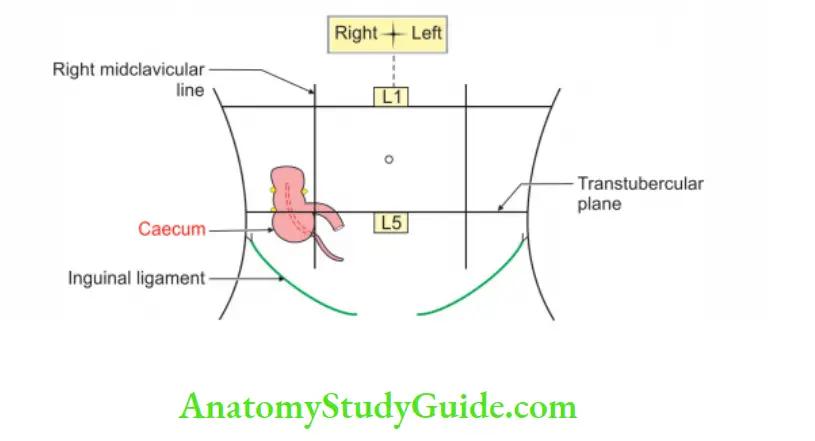
Caecum Location:
It is situated in right iliac fossa above the lateral half of inguinal ligament.
- Length x breadth = 6 cm x 7.5 cm.
- Shape: Usually asymmetrical cul de sac.
Organs betraying “width”:
Note: Organs having more width than length
- Prostate
- Caecum
- Isthmus of thyroid gland
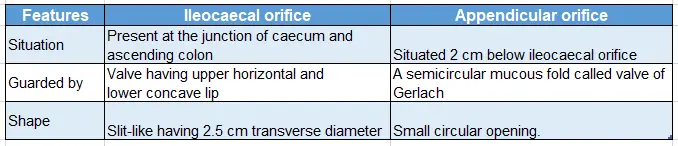
2. Caecum Internal structure: It shows two orifices.
- Ileocaecal orifice.
- Appendicular orifice.
- It is movable and bound to the lateral abdominal wall.
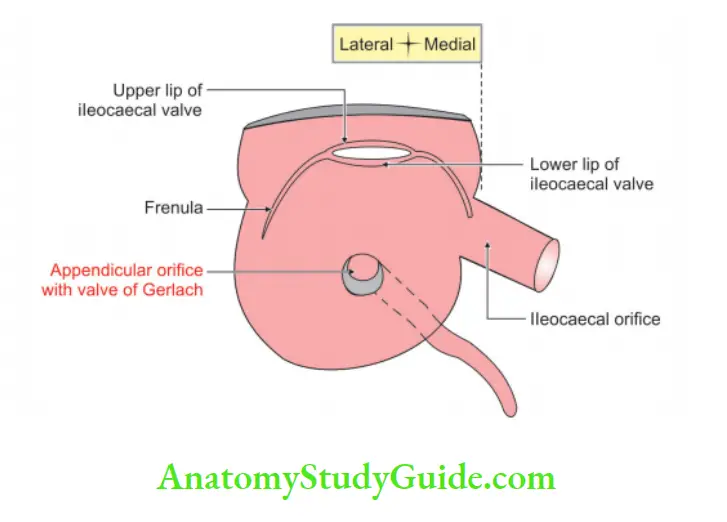
Orifices in the caecum:
3. Caecum Relations:
1. Peritoneal relatin:
- It is covered by peritoneum on all sides except posterior surface.
- It has no mesentery.
- It is movable and bound to the lateral abdominal wall by one or more caecal fold of peritoneum.
2. Visceral relations:
Anterior relations:
- Coils of the intestine.
- Anterior abdominal wall.
Posterior relations:
- Appendix in retrocausal recess.
- Right, psoas and iliacus muscle.
- The genitofemoral, femoral and lateral cutaneous nerve of thigh.
- Right gonadal and right external iliac vessels.
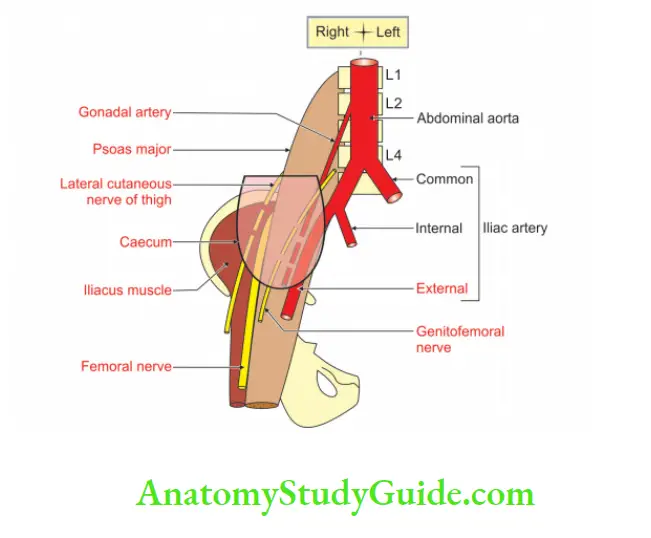
Medial:
- Appendix
- The terminal part of ileum
- Inferior ileocaecal recess.
4. Caecum Blood supply:
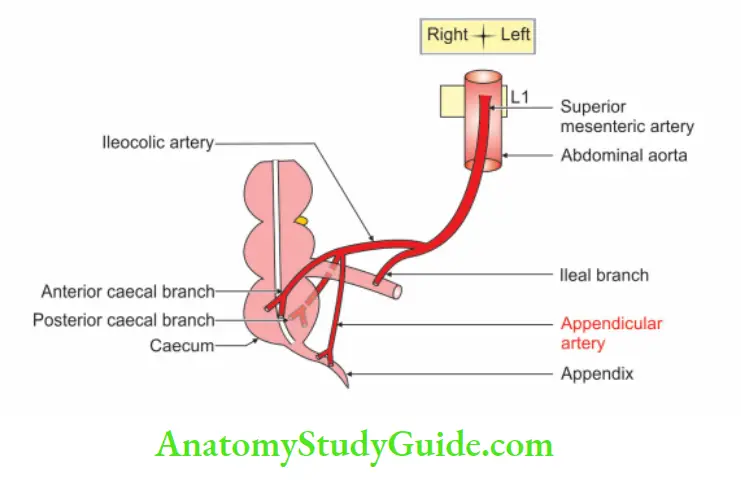
Arerial supply: Anterior and posterior caecal arteries (branches of the ileocaecal artery which are terminal branches of superior mesenteric artery).
Venous drainage: Ileocaecal vein drains into superior mesenteric vein which drains into portal vein
5. Caecum Nerve supply: From superior mesenteric plexus
- Sympathetic fibres arise from T10 to L1 segments of spinal cord.
- Parasympathetic fibres arise from vagus nerve.
6. Lymphatic drainage: Ileocolic lymph nodes, which drain into superior mesenteric lymph nodes.
2. Caecum Applied anatomy
If distended with faeces or gas, the caecum may be palpable through anterior abdominal wall.
The caecum acts as a guideline for localization of obstruction.
If the caecum is distended, the obstruction is in the large intestine.
If the caecum is empty, the obstruction is in the small intestine.
Intussusception: Sometimes terminal part of ileum telescopically invaginates into caecum and ascending colon at ileocaecal junction. This phenomenon is known as intussusception.
The tuberculosis of intestine is common at ileocaecal junction.
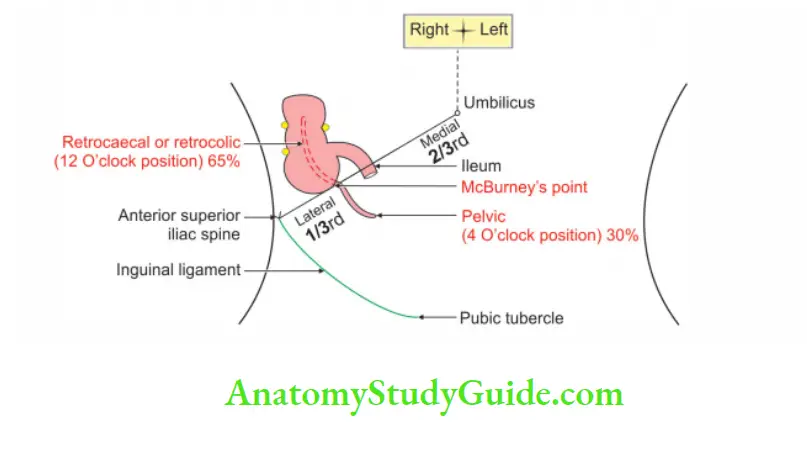
McBurney’s point
1. Mcburney’s Point Site: Junction of medial 2/3rd with lateral 1/3rd of right spinoumbilical line.
2. Mcburney’s Point Structure related: Base of appendix
3. Mcburney’s Point Applied anatomy : It is the area of maximum tenderness in appendicitis.
Question – 4: Describe Appendix under following heads
1. Appendix Gross anatomy
2. Appendix Histology
3. Appendix Development, and
4. Appendix Applied anatomy.
Answer:
Appendix Introduction: It is a narrow tubular diverticulum. It resembles a roundworm, hence called vermiform appendix. It arises from posteromedial wall of the caecum.
1. Appendix Gross anatomy:
1. Appendix Location: It is situated in the right iliac fossa. It is 2 cm below the intersection of transtubercular (upper part of 5th lumbar vertebra) and right lateral plane.
2. Appendix Length: It is 2 to 20 cm (average is 9 cm). Length increases in young adults and diminishes after mid-adult life.’
3. Appendix Peculiarities: Although appendix is the part of large intestine, it is devoid of SAT
- Sacculations (S)
- Appendices epiploicae, and (A)
- Taenia coli (T).
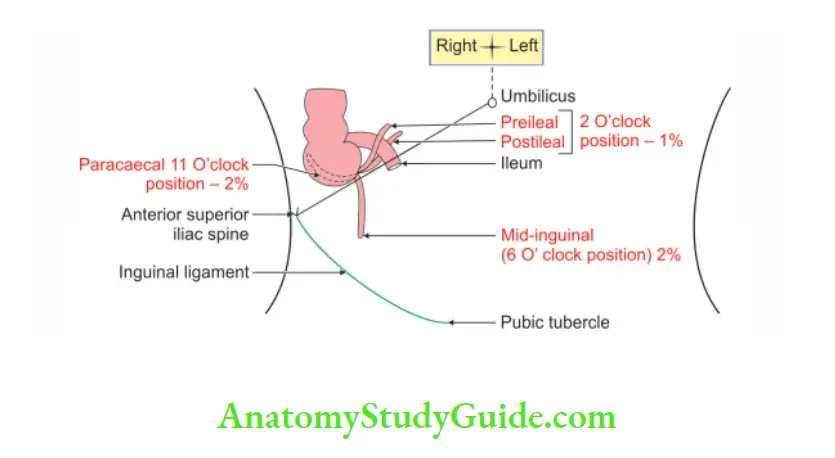
4. Position of appendix: The position of the appendix is extremely variable. According to the direction of the tip of the appendix, position of appendix is classified as retrocaecal appendix.
Retrocaecal or retrocolic: The appendix passes behind the caecum and ascending colon.
- It is 12 O’clock position.
- It is most common position of the appendix (75%).
- It presents as pain and tenderness at McBurney’s point.
- The patient experiences pain in extension of hip joint.
Pelvic appendix:
The appendix is at 4 O’clock position.
It is 2nd common position of appendix.
It presents as pain and tenderness at McBurney’s point and hematuria due to pressure of inflamed appendix on the right ureter.
In Pelvic Appendix, the patient experiences Pain in Medial Rotation and Flexion and of hip joint.( Pe App), Pain is MRF.
Splenic appendix:
- 2 O’clock position.
- It is rare position of the appendix.
- It presents as pain and tenderness at McBurney’s point.
- It is most dangerous because infection spreads to the general peritoneal cavity.
5. Appendix Internal features:
- Appendicular orifice
- It is situated on the posteromedial aspect of the caecum 2 cm below the ileocaecal orifice.
- It is occasionally guarded by a semilunar fold of mucous membrane, known as valve of Gerlach.
6. Appendix Relations: Peritoneal relations
Mesoappendix: It is a small lar fold of the peritoneum suspending appendix.
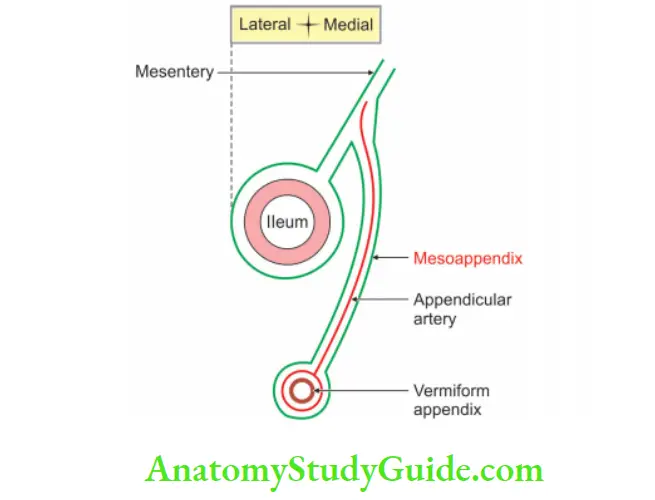
7. Appendix Blood supply:
1. Arterial supply: Appendicular artery, a branch of inferior division of the ileocolic artery. It gives a recurrent branch, which anastomoses with the posterior caecal artery. It is an end artery, and hence the tip is least vascular.
2. Venousdrainagel: Appendicular vein drains into superior mesenteric vein which joins with splenic vein and forms the portal vein.
Recall memory:
Note: Examples of an end artery
- Appendicular artery
- The central artery of retina
- Cortical arteries of the cerebrum
8. Nerve supply:
- Sympathetic nerves are derived from superior mesenteric plexus.
- Preganglionic fibres arise from T10 segment of the spinal cord.
- Therefore, the pain is referred to skin over umbilicus which has the same segmental innervation.
- Parasympathetic nerve: Vagus.
Lymphatic: Superior mesenteric lymph nodes via ileocolic nodes.
2. Appendix Histology
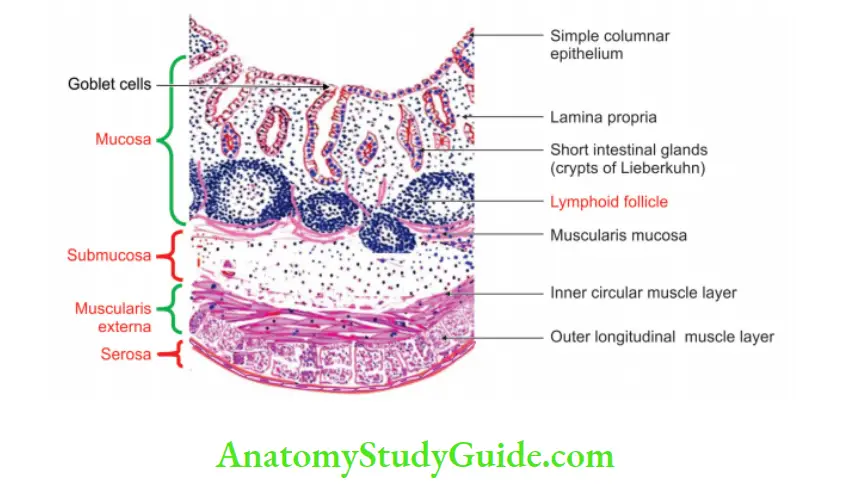
Appendix has 4 coats. They are described from inside out as
1. Mucosa: It has following features
- Simple columnar epithelium with numerous goblet cells.
- Occasional enterochromaffin cells are present.
- Absence of villi.
- Muscularis mucosae and lamina propria are present.
- Lamina propria shows lymphocytes.
- Presence of glands.
- Hiatus muscularis: It is deficient area in muscularis externa.
2. Submucosa: It shows lymphatic follicle, which are in ring form.
3. Muscularis externa: It has
- Inner circular muscle.
- Outer longitudinal muscle.
4. Serosa: Serosais derived from peritoneum and covers the entire tube—except the border where mesoappendix is attached. It is lined by simple squamous epithelium.
3. Development
Chronological age: It develops in the early 8th week of intrauterine life.
Germ layer: Endoderm and mesoderm.
Source:
- Epithelium and glands develop from lower narrow part of caecal diverticulum. It arises from midgut. It is endoderm in origin.
- The remaining coats develop from intraembryonic splanchnic pleuric mesoderm.
Anomalies:
- Subhepatic appendix: It mimics the symptoms of the acute cholecystitis.
- Appendicectomy is difficult in subhepatic appendix.
4. Applied anatomy
1. Inflammation of the appendix is known as appendicitis. It is manifested by Murphy’s triad.
- Pain is first felt at the umbilical region because the appendix and the skin of the umbilicus are supplied by 10th thoracic segment of spinal cord.
- It is then localized at the right iliac fossa due to local peritonitis. It is associated with the tenderness and rigidity at McBurney’s point.
- Vomiting.
- Temperature because of the infection.
2. Anatomical factors for appendicitis.
- The appendix is a blind tube.
- A faecolith may obstruct the lumen and precipitate the attack of appendicitis.
- It is supplied by an end artery.
- It shows the presence of hiatus muscularis.
- It shows numerous lymphatic follicles in the submucosa.
3. In the retrocausal appendix, the patient experiences pain on the extension of the right hip joint due to irritation of the right psoas major muscle.
4. In the pelvic appendix, the patient experiences.
- Pain in Medial Rotation and Flexion and of hip joint.
- In in MRF. Pain is due to the irritation of obturator internus muscle.
- Hematuria is due to pressure of inflamed appendix on right ureter.
5. During appendicectomy, the appendix can be located by tracing taenia coli, which converges at the base of the appendix.
6. Obstruction of the appendicular artery results into gangrenous appendix.
7. Ilioinguinal nerve supplies lower most fibres of the internal oblique and transversus abdominis muscle.
- During split muscle incision of appendix operation, ilioinguinal nerve may be damaged.
- It reduces the tone of the muscles of anterior abdominal wall (internal oblique and transversus abdominis muscle).
- It results into direct inguinal hernia.
8. The damage to the ilioinguinal nerve in the inguinal canal does not paralyse the internal oblique and transversus abdominis muscle because the nerve is purely sensory at this site.
9. Appendicitis is less likely in extreme ages. This is because of following reasons.
- In children, the lumen of the appendix is wide.
- In old age, the lumen gets obliterated.
10. In neglected cases, a long appendix is known to ulcerate into the duodenum or perforate into left paracolic gutter.
Leave a Reply