Large Blood Vessels of the Gut
Branches of splenic artery
1. Pancreatic branches: They are many in number.
Table of Contents
- Arteria pancreatica magna: This is large branch to the body of pancreas.
- Arteria caudae pancreatis: This is the large branch to the tail of pancreas.
2. Short gastric arteries: They are 5 to 7 in number.
3. Left gastroepiploic artery.
Read And Learn More: General Histology Question And Answers
Splenic artery
Introduction: It is the largest artery of coeliac trunk supplying the spleen and pancreas.
1. Origin: It arises from the coeliac trunk.
2. Course and relations:
- It courses behind the peritoneum, undulating at upper border of the body of pancreas in a wavy course.
- The crests of its waves appear above the pancreas, the troughs lie hidden behind its upper border.
- It crosses successively the left crus, left psoas muscle, and reaches the hilum of the left kidney.
- From the hilum of the left kidney to the hilum of the spleen.
- It passes through the lienorenal ligament where it divides into a handful of branches.
- These branches along with veins penetrate the spleen.
3. Peculiarities:
1. It is interesting to note that spleen is supplied only by splenic artery but splenic artery does not supply only spleen.
2. Apart from these structures, splenic artery also supplies blood to
- Fundus part of stomach
- 1/4th part of greater curvature, and
- Greater omentum
3. Splenic branches of the splenic artery are end arteries, but the other branches of the splenic artery are not end arteries.
4. The branches of splenic artery are segmental in distribution. But tributaries of splenic vein are intersegmental in drainage.
4. Branches: Splenic artery gives numerous
Pancreatic branches that supply blood to the body and the tail of the pancreas.
1. One of the branches of the body of pancreas, a large one, is known as arteria pancreatica magna. It accompanies the main pancreatic duct.
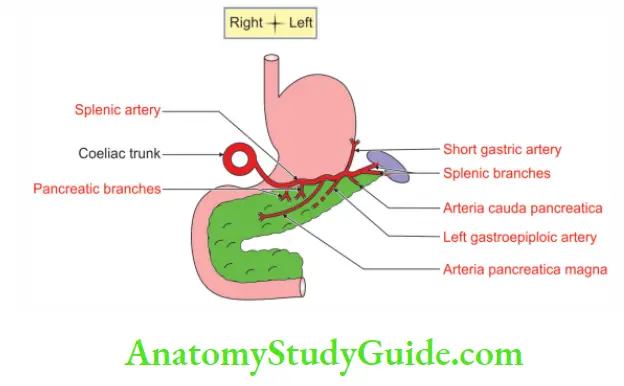
2. Just before its terminal, splenic artery gives rise to the
Left gastroepiploic artery: It is the largest branch of splenic artery.
- First, it runs between two layers of gastrosplenic ligament and then between two layers of greater omentum.
- It anastomoses with right gastroepiploic artery which is a branch of gastroduodenal artery.
- These arteries supply blood to greater omentum but not to transverse colon.
Short gastric arteries: They are about half a dozen in number and supply the fundus of stomach.
5. Applied anatomy:
1. A posterior gastric ulcer or cancer may erode the splenic artery and cause torrential haemorrhage.
2. Kehr’s sign: It is occurrence of acute pain in the left shoulder.
3. It is due to presence of blood or other irritant in the peritoneal cavity when the person is lying down and legs are elevated. It is classic sign of rupture of spleen.
Interesting about spleen:
1. Let us now look at some of the interesting and important features of the splenic artery.
One: It is the largest artery of coeliac trunk. The large size of the splenic artery indicates the volume of blood that passes through the capillaries and sinuses of the spleen.
Two: It is one of the most important structures that forms the stomach bed.
And three: It is very tortuous.
2. After understanding important features, let us know the reasons of tortuosity.
One: Tortuosity helps to regulate the blood flow to the spleen in different metabolic activities of life.
Two: It allows free movements of the spleen in respiration without rupture.
Three: It permits distension of the stomach without obstruction to the splenic blood flow.
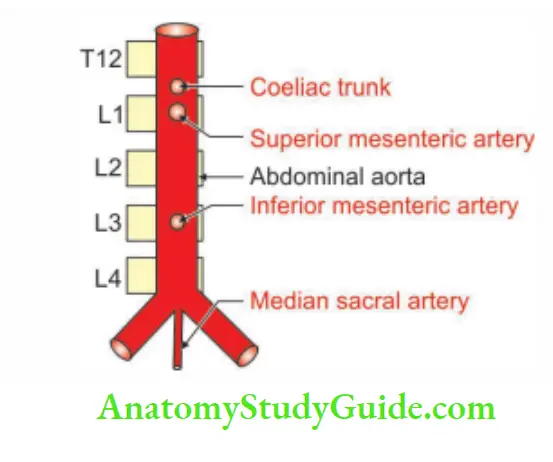
Question-1: Describe inferior mesenteric artery under
1. Origin
2. Course
3. Branches, and
4. Applied anatomy
Answer:
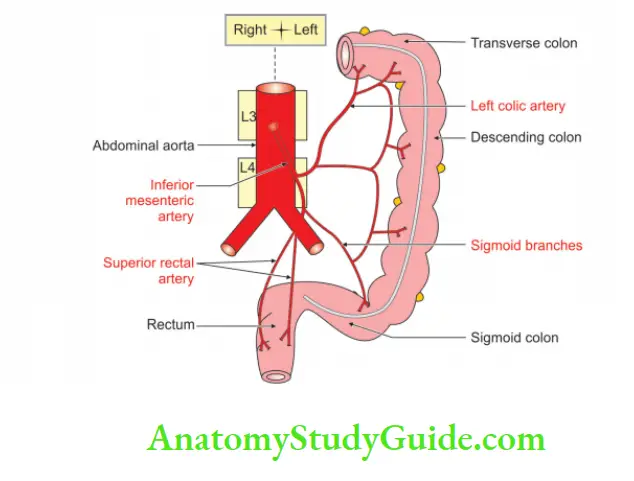
Introduction: It is the artery of hindgut.
1. Origin
It arises from front part of the abdominal aorta. It is deep up to the lower border of third part of the duodenum. It is much smaller in diameter than superior mesenteric artery.
2. Course
1. It runs obliquely downwards and to the left of the aorta.
2. It passes retroperitoneally beneath the peritoneal floor of the left infracolic compartment.
3. It crosses the pelvic brim over the sacroiliac joint at the bifurcation of the left common iliac vessels.
4. It changes its name to superior rectal artery as the latter crosses the common iliac artery.
5. In its course, it lies on the
Abdominal aorta, and left
- Psoas major muscle
- Sympathetic trunk
- Common iliac artery, and
Hypogastric nerves: Please bear in mind, inferior mesenteric artery in its course lies medial to the left ureter, and does not cross it, although all its branches do.
3. Branches
There are mainly three branches. They are
1. Left colic artery: It divides into two branches—the upper and the lower branches.
- The upper branch passes upwards to the splenic flexure.
- The lower branch passes transversely to the descending colon and supplies blood to it.
2. Sigmoid arteries: They are three in number. They pass forward between the layers of sigmoid colon and sink into the walls and supply it. The last sigmoid branch anastomoses with the 1st branch of superior rectal artery.
3. Superior rectal artery: It is the chief artery of the rectum. It descends up to 3rd sacral vertebra and divides into two branches.
- About the middle of the rectum, each of these branches divides into smaller vessels.
- They pierce rectal wall and descend vertically through the submucous coat.
- At the level of the internal anal sphincter, these branches anastomose with one another to form loops around the lumen.
- They supply the upper part of rectum.
4. Each branch of the superior and inferior mesenteric arteries anastomoses with its adjacent arteries.
- These anastomotic branches form a continuous vascular arcade along the whole length of the gastrointestinal canal.
- This is called marginal artery. It begins at the ileocaecal junction.
- It begins by anastomosing with the ileal branches of the superior mesenteric artery.
- It ends by anastomosing with the superior rectal artery, branch of inferior mesenteric artery.
4. Applied anatomy
1. In the event of a block in the inferior mesenteric artery, blood reaches the left side of the colon through the marginal artery.
2. Occlusion of the aorta or common iliac arteries may also result in dilatation of the marginal and inferior mesenteric arteries.
- This is an important collateral supply to the legs.
- The blood reaches via dilated middle rectal vessels arising from the internal iliac artery.
3. The anastomosis at splenic flexure is between the
- Trunk of middle colic artery, and the
- Ascending branch of left colic artery.
4. This anastomosis is called arc of Riolan.
- If by any chance, this anastomosis is not well developed, the arterial supply of the splenic flexure is endangered.
- Therefore, it is called a critical point which lies at the splenic flexure.
5. There is anastomosis between the lowest sigmoid branch and the upper rectal branch. The point of origin of the lowest sigmoidal artery is called Sudeck critical point.
6. The inferior mesenteric artery is ligated proximal to Sudeck’s point to avoid ischaemia and necrosis of the sigmoid colon and rectum.
7. Occlusion of the inferior mesenteric artery does not always result in ischaemia of the descending and sigmoid colon. This is because of the marginal artery of the colon.
8. The ischaemia of the descending and sigmoid colon does occur. It is usually maximal in the proximal descending colon because this region is furthest from the collateral anastomosis
9. The ascent of the horseshoe shaped kidney is arrested at the inferior mesenteric artery, and results in urinary obstruction.
![]() Horseshoe shape
Horseshoe shape
10. In carcinoma of the colon, the related paracolic and intermediate lymph nodes are removed only after the ligature of the main branch of the superior or inferior mesenteric artery.
11. Embolism is uncommon in the inferior mesenteric artery due to better collateral circulation.
The beauty of 3 in inferior mesenteric artery:
- It is the artery of the 3rd part of gastrointestinal tract.
- It is 3 cm long.
- It supplies left 1/3rd of transverse colon.
- It arises from abdominal aorta at 3rd lumbar vertebra.
- It arises 3 cm above the bifurcation of abdominal aorta.
- It lies behind lower border of 3rd part of duodenum.
- It extends up to upper 1/3rd of anal canal.
- It gives 3 branches.
- The 3rd branch of the inferior mesenteric artery is superior rectal artery.
- Superior rectal artery extends up to the 3rd sacral vertebra.
Obturator artery
1. Origin It arises from anterior division of internal iliac artery. It is close to the origin of the umbilical artery.
2. Course and relations
- It passes along the lateral wall of the pelvic cavity.
- On its way to the obturator canal, it lies between the parietal pelvic fascia and the peritoneum.
- It passes between the obturator nerve above and its obturator vein below.
- In males ♂, it is crossed by the ureter and the ductus deferens.
- In females ♀, the ovarian vessels and broad ligament are present on medial side.
- On entering the obturator canal, the artery does not pierce the parietal pelvic fascia but passes over its upper border.
3. Branches
They are grouped as branches
1. Inside the pelvis: It gives three branches, namely
- Iliac branches to the iliac fossa
- Vesical branch to the urinary bladder, and
- Pubic branch to the pubis.
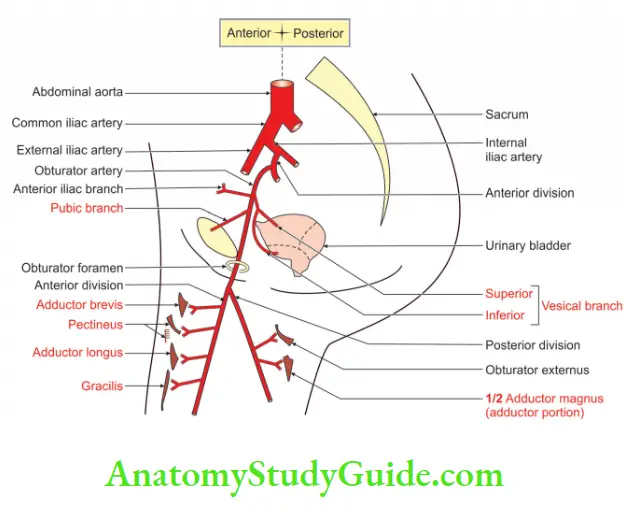
2. Outside the pelvis (in the thigh): The branches are
Anterior branch to:
- Obturator externus
- Pectineus
- Adductor longus
- Adductor brevis
- Adductor magnus, and
- Gracilis.
It anastomoses with the posterior branch and the medial circumflex femoral artery.
Posterior branches:
Form the arterial loop around acetabular circumference. The anastomosis takes place between the obturator externus and the obturator membrane.
It supplies the muscles attached to the ischial tuberosity. It anastomoses with the
1. Anterior branch, and the
2. Inferior gluteal artery.
- It gives an additional branch called acetabular branch. It enters the hip joint at the acetabular notch.
- It ramifies in the fat of the acetabular fossa and sends a branch to the ligament of head of femur.
- It is to be noted that the pubic branch runs over the pubis.
- It anastomoses with the pubic branch of the inferior epigastric artery with its fellow of the opposite side.
- Sometimes the anastomosis is large and then the obturator artery appears to be a branch of the inferior epigastric.
- This is called the abnormal obturator artery
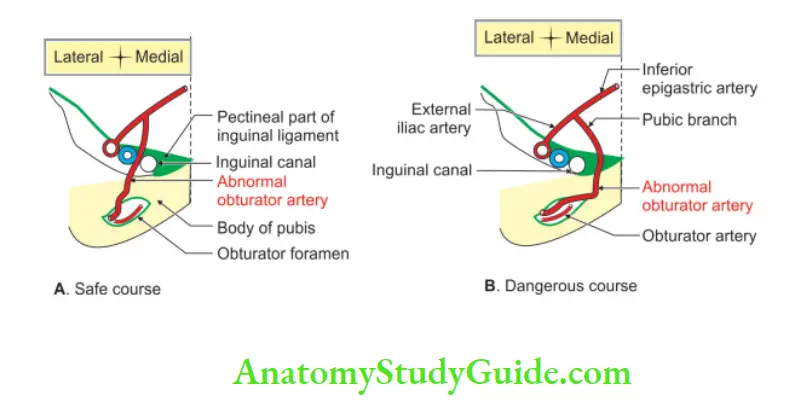
4. Applied anatomy
Usually, the abnormal obturator artery passes lateral to the femoral canal. This is safe in the operation of femoral hernia. Sometimes, however, it may lie along the medial margin of the femoral ring, along the free margin of the lacunar ligament. Such an artery is likely to be cut, if an attempt is made to enlarge the femoral ring.
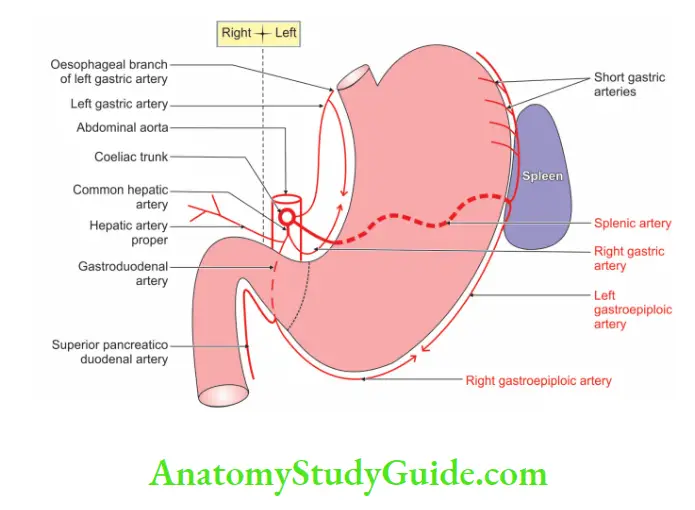
Enumerate the branches of the coeliac trunk
1. Left gastric artery
2. Splenic artery
3. Common hepatic artery
Introduction: There are three types of coeliac trunk
1. Left gastric artery
2. Splenic artery
It gives following branches.
- Left gastroepiploic artery
- Short gastric arteries.
3. Common hepatic artery
It gives the following branches.
1. Right gastric artery: It passes between two layers of lesser omentum and divides into two branches which anastomose with two branches of left gastric artery.
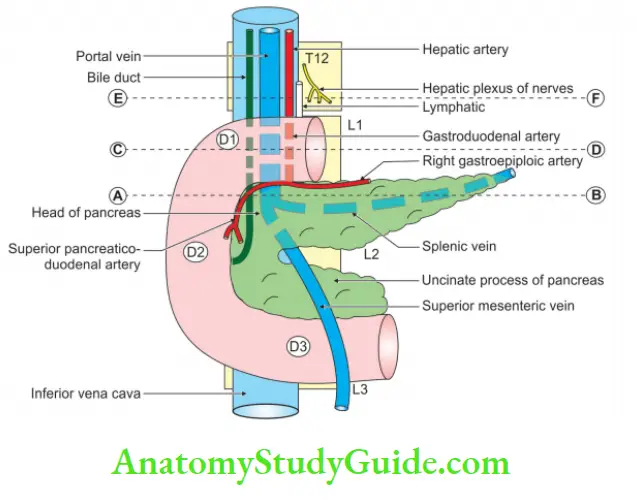
2. Gastroduodenal artery: It passes behind the 1st part of the duodenum and divides into two branches
- The right gastroepiploic artery
- Superior pancreaticoduodenal artery.
3. Cystic artery
Question – 2: Describe coeliac trunk (coeliac axis, coeliac artery) under following heads
1. Origin
2. Relations
3. Branches, and
4. Applied anatomy.
Answer:
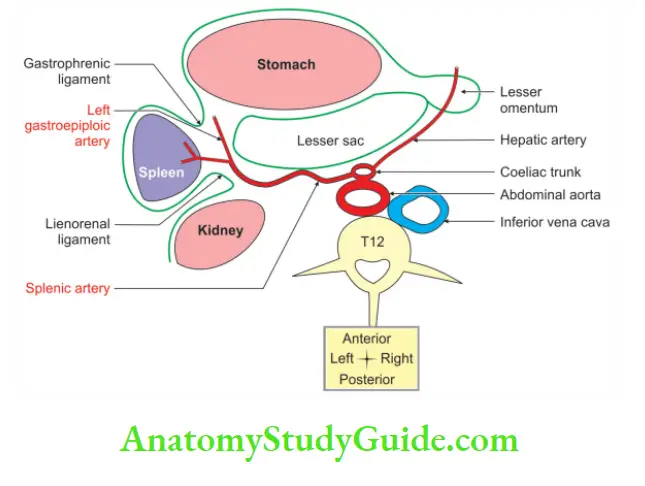
Introduction: It is the artery of the foregut. It supplies part of the alimentary canal from cardiac orifice of the stomach, to the opening of bile duct, in 2nd part of the duodenum. It also supplies the derivatives of the foregut, namely the liver, spleen and pancreas.
1. Origin
It arises from the front of abdominal aorta. It is present at the level of intervertebral disc of the T12 and L1 vertebrae. Its origin is just below the aortic opening of the diaphragm.
2. Relations
Anterior:
- Lesser sac, and
- Lesser omentum.
Right:
- Right crus of the diaphragm
- Right coeliac ganglion, and
- Caudate process of the liver.
Left:
- Left crus of the diaphragm
- Left coeliac ganglion, and
- Cardiac end of the stomach.
Inferior:
- Tuber omental of the pancreas, and
- Splenic vein.
- It is surrounded by a coeliac plexus.
Sandwiching, and hugging of coeliac trunk:
- The Coeliac trunk is sandwiched between papillary process of the liver which is present above and the tuber omental of the pancreas from below.
- It is hugged by a crus of diaphragm from each side.
- It is surrounded by the coeliac group of pre-aortic lymph nodes.
- Coeliac ganglia of the sympathetic system lie one on each side of it.
3. Branches
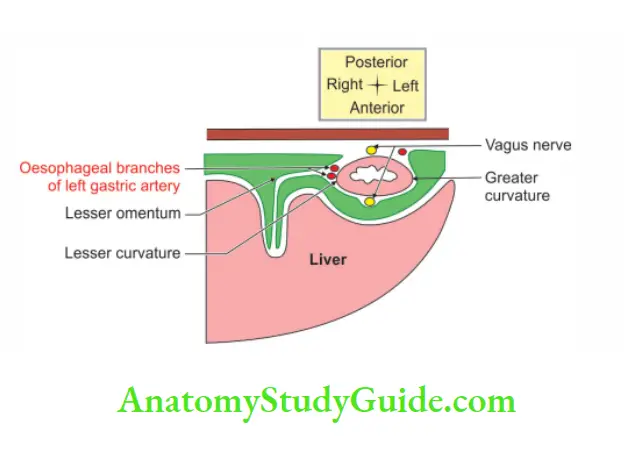
1. Left gastric artery:
1. It is the smallest branch of the coeliac trunk and supplies the largest area of the stomach.
2. It runs in the opposite direction of the hepatic artery.
3. It lies behind the peritoneum and gives an oesophageal branch.
4. The oesophageal branch:
- Supplies lower end of the oesophagus.
- It runs between two layers of lesser omentum.
- It breaks into two parallel branches, which are anastomose with two branches of the right gastric artery.
- It distributes the blood to the lesser curvature of the stomach.
2. Splenic artery:
- It is the largest, very tortuous branch of the coeliac trunk.
- It lies behind the peritoneum.
- It enters the hilum of the spleen through the lienorenal ligament.
- It breaks into 5 to 7 splenic branches.
- It is the main source of arterial supply to the pancreas.
- It gives the following branches
Left gastroepiploic artery: It runs on the greater curvature and anastomoses with the right gastroepiploic artery. It supplies blood to the greater curvature of the stomach.
Short gastric arteries: Practical definition: Those arteries arising at the level of the splenic artery are called short gastric arteries. They run upward and supply the fundus of the stomach and its greater curvature.
3. Common hepatic artery:
- It passes over the upper border of the pancreas.
- It runs forward at the opening into the lesser sac.
- It reaches the porta hepatis and divides into right and left branches to supply the left and right halves of the liver.
- It gives following branches.
Right gastric artery
1. It passes between two layers of lesser omentum and divides into two branches. Branches of right gastric artery anastomoses with the branches of left gastric artery.
2. It supplies
- Pylorus
- The proximal part of the duodenum
- Pancreas, and
- Nerve supplying stomach.
Gastroduodenal artery: It passes behind the first part of the duodenum and divides into two branches.
1. The right gastroepiploic artery
- It runs in the greater omentum.
- It anastomoses with the left gastroepiploic artery.
- It gives branches to the anterior and posterior walls of the stomach along greater curvature.
2. Superior pancreaticoduodenal artery
- It divides into two branches which encircle the head of pancreas.
- They anastomose with the inferior pancreaticoduodenal artery, a branch of superior mesenteric artery.
4. Applied anatomy
1. The obstruction of the common hepatic artery proximal to the right gastric artery may save the liver from necrosis.
2. It is due to an establishment of collateral circulation between the gastric and gastroepiploic arteries.
3. The obstruction at the hepatic artery proper always causes liver necrosis.
4. Occasionally the coeliac artery is compressed by the median arcuate ligament.
This may result in chronic ischaemia of the abdominal viscera. It is associated with postprandial pain and an epigastric bruit.
5. The site of origin of the coeliac artery is inconsistent. An abnormally high origin above the lower 1/3rd of the 12th thoracic vertebra is frequently associated with entrapment syndrome.
6. The coeliac artery arises at a higher level in women
than in men and the entrapment syndrome is more common in females
About coeliac trunk:
The word ‘coeliac’ means ‘related to abdomen’. It is short and wide. It belongs to the category of organs that have more width than length, such as caecum and prostate.
Left gastric artery
Introduction: It is the 1st branch of the coeliac trunk supplying two-thirds part of the stomach.
1. Origin
It is the smallest, direct branch of the coeliac trunk
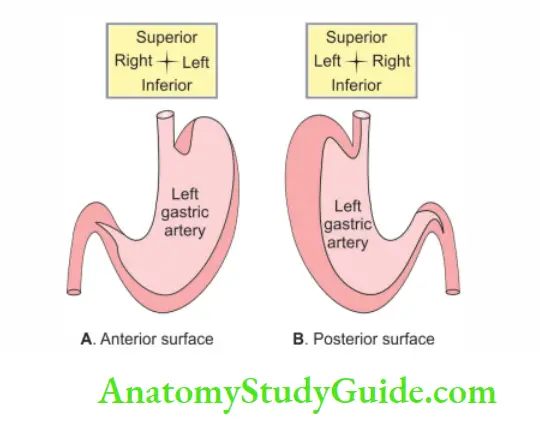
2. Course and relations
- It runs behind the peritoneum.
- It courses from the upper border of the pancreas across the left crus of the diaphragm to the oesophageal hiatus.
- It forms the left gastropancreatic fold.
- It enters at the junction of the two leaves of the lesser omentum.
- It turns to the right along the lesser curvature.
- It breaks into two parallel branches which anastomose with the two branches of the right gastric arteries
3. Branches
The left gastric artery gives off branches at right angles. These branches sink into the anterior and posterior walls of the stomach.
They anastomose very freely with similar branches from the arteries of the greater curvature. It supplies the largest area of the stomach.
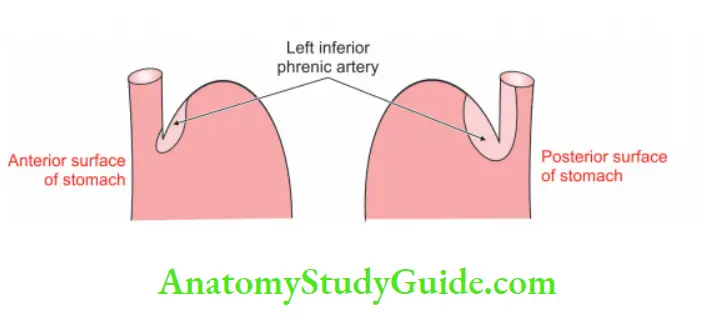
It provides the major route of blood supply to both surfaces of the stomach
- It bifurcates into the oesophageal and gastric branches.
- The oesophageal branches supply the lower end of the oesophagus and the cardiac end of the stomach.
- These branches are anastomose with the oesophageal branches of the thoracic aorta.
- The gastric branches supply the anterior and posterior surfaces of the upper 2/3rd part of the stomach.
Great things come in small packages:
Thus, two proverbs seem appropriate and befitting to signify its importance:
The old Hindi proverb, “Murthy chhoti lekin Kirti moti”, or the English proverb, “Great things come in small packages”. This rightly appeals to the left gastric artery.
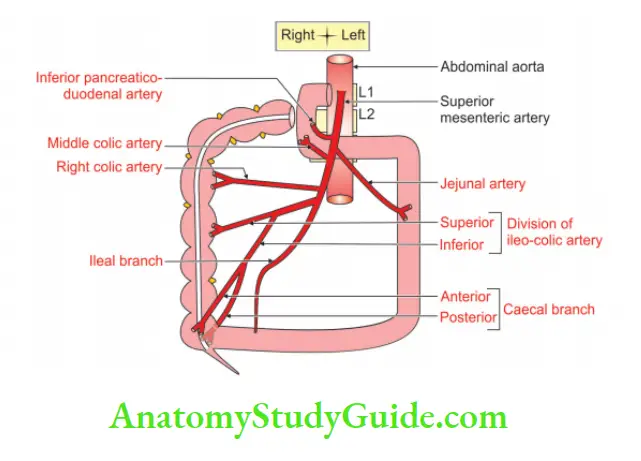
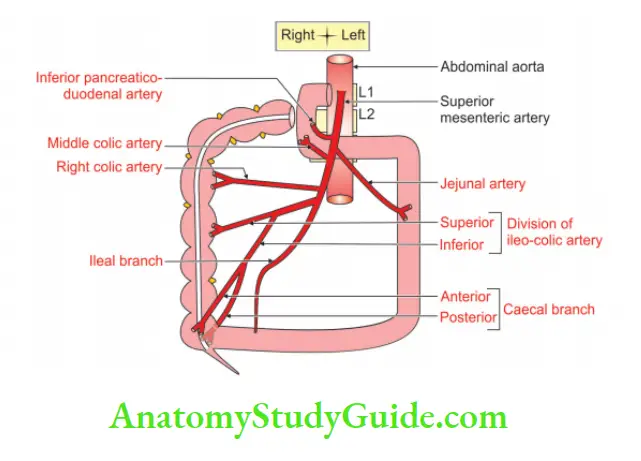
Branches of superior mesenteric artery
1. Branches from right side
- Inferior pancreaticoduodenal
- Middle colic
- Right colic
- Ileocolic
2. Branches from left side
- Jejunal, and
- Ileal
Enumerate the branches and distribution of the superior mesenteric artery.
Branches and distribution of superior mesenteric artery:
Question – 3: Describe the superior mesenteric artery under the following heads
1. Origin
2. Course and relations
3. Branches, and
4. Applied anatomy.
Answer:
Introduction: It is the artery of the midgut supplying all the structures derived from the midgut.
1. Origin
It is the unpaired artery arising from the front of the abdominal aorta, 1 cm below the coeliac trunk at the level of the 1st lumbar vertebra. Functionally, it is the end artery.
It arises behind the body of the pancreas so its origin cannot be seen. It is one of the important structures present at the level of the transpyloric plane. Its calibre progressively decreases as successive branches are given off to loops of jejunum and ileum.
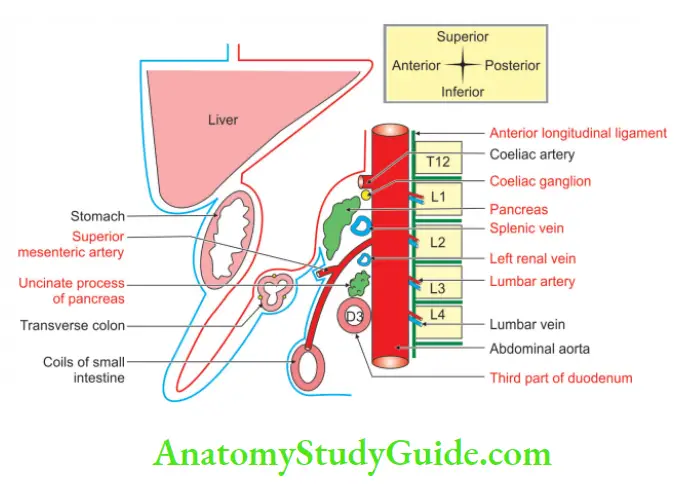
2. Course and relations
The superior mesenteric artery is directed steeply downwards, behind the splenic vein and the body of the pancreas. The superior mesenteric vein lies on the right side. It lies superficial to
- Abdominal aorta
- Left renal vein
- Uncinate process of the pancreas, and the
- 3rd part of the duodenum. It lies in that order downwards from above.
- The artery is surrounded by the superior mesenteric plexus of nerves.
It passes to the right along the root of the mesentery and ends at the ileum 2′ proximal to the caecum. The artery gives off numerous branches to the gut.
3. Branches
The branches are classified for convenience as
1. Branches given from left side: They are about a dozen in number. They pass through the mesentery to reach the gut.
1. The ileal mesentery contains three or more arches, whereas the jejunal mesentery presents 1 or 2 arterial arches.
2. They anastomose with each other to form a series of arches.
3. Straight vessels known as vasa recta arise from the terminal arches and supply the opposite surfaces of the jejunum and ileum in an alternate manner.
4. The vasa recta are end arteries. The branches are
- Jejunal: They arise from the left side, and
- Ileal branches arise from the left and anterior aspects of the superior mesenteric artery.
2. Branches from the right side are:
- Inferior pancreaticoduodenal
- Right colic
Middle colic, and - Ileocolic.
Ileal and jejunal arteries:
To be concise and precise. Ileal branches are longer, more numerous and smaller in calibre than the jejunal branches. But the ileal vasa recta are shorter than jejunal vasa recta.
3. Inferior pancreaticoduodenal artery: arises from the posterior aspect of the superior mesenteric artery at the upper border of 3rd part of the duodenum.
The branch is given before the superior mesenteric artery crosses 3rd part of the duodenum. It divides into
1. Anterior, and
2. Posterior branches.
- They run upwards on corresponding aspects of the head of the pancreas.
- They supply the pancreas and duodenum and anastomose with the branches of the superior pancreaticoduodenal arteries.
- Colic branches again are subdivided into branches arising from the highest, middle and lowest parts of the colon.
3. Right colic: The branch given from the middle part is the right colic artery. It is a small vessel that is highly variable in its anatomy. It runs to the right across all the structures on the right side. They are the
- Psoas muscle
- Gonadal vessels
- Ureter
- Genitofemoral nerve, and the
- Quadratus lumborum muscle.
It terminates by dividing into descending and ascending branches that anastomose with the ileocolic and middle colic arteries, respectively.
The artery supplies the upper two-thirds of the ascending colon.
4. Middle colic: The branch given from the highest part of the superior mesenteric artery is the middle colic artery.
It arises from the anterolateral aspect of the right side of the superior mesenteric artery just below the duodenum.
It runs downwards into the transverse mesocolon and divides into’
1. Right, and
2. Left branches.
- They run along the transverse colon.
- The right branch anastomoses with the ascending branch of the right colic artery.
- The left branch supplies the transverse colon almost to the splenic flexure.
- Here it anastomoses with a branch of the left colic artery.
5. Ileocolic artery: It is given from the lowest part of the superior mesenteric artery. It runs on the posterior abdominal wall a little above the parent vessel.
The ileocolic artery gives off various branches to the terminal part of the ileum
1. Caecum
2. Appendix
3. Lower one-third of the ascending colon. It ends by dividing it into
- The superior branch runs along the left margin of the ascending colon and anastomoses with the right colic artery.
- The inferior branch runs on the ileocolic junction and gives off
Caecal arteries which subdivide into:
Anterior caecal artery: It is the smaller of the two terminal branches and ramifies over the anterior surface of the caecum.
Posterior caecal artery: It is the largest branch of the ileocolic artery.
- It supplies the posterior wall of the caecum, as well as the medial and lateral walls of that part of the gut.
- It gives appendicular branches.
2. Ileal branches.
MCQ:
1. Practically, appendicular and ileal branches are end arteries.
2. Note, the following arteries have a retroperitoneal course
- Inferior pancreaticodoudenal
- Right colic
- Ileocolic
3. The middle colic artery runs in a transverse mesocolon.
4. Jejunal and ileal branches traverse the mesentery of the small intestine.
4. Applied anatomy
1. In an erect posture, the loops of the intestine may come down. This will drag the superior mesenteric artery. This compresses the left renal vein resulting in a varicocele of the left renal vein.
2. The superior mesenteric artery may compress the duodenum and give symptoms of chronic duodenal ileus (obstruction to the intestine) or superior mesenteric artery syndrome.
3. It is commonly called SMA syndrome or Wilke’s disease. This is suspected in persons who lose weight quickly in a very short time.
4. Symptoms include early satiety, nausea, vomiting, extreme “stabbing” postprandial abdominal pain, abdominal distention, eructation, tenderness of the abdominal area, and severe malnutrition accompanying spontaneous wasting.
5. Due to the close relation of the superior mesenteric artery with the pancreas, the infection of the pancreas may cause inflammation of the superior mesenteric artery.
6. Total or segmental infarction may occur due to occlusion of the superior mesenteric artery or one of its distal branches.
7. The occlusion may occur as the result of an embolus, a thrombus, an aortic dissection or an abdominal aneurysm.
8. The more distal the occlusion, the smaller the area of the bowel that becomes gangrenous.
9. Vascular stenosis may produce intestinal angina with colicky pain referred to the umbilical region.
10. As the middle colic artery lies to the right of the midline, it leaves a large avascular window to its left in the transverse mesocolon. This is the ideal site for surgical access to the lesser sac and the posterior wall of the stomach.
11. Terminal 8-10 cm of the ileum needs to be excised while dealing with the pathology of the caecum and descending colon. Failure of resecting this part will result in vascular necrosis of the terminal part of the ileum.
12 . The adhesion between the transverse mesocolon containing the middle colic artery and the greater curvature of the stomach must be detached with care.
13. The superior mesenteric artery arises from the abdominal aorta at an acute angle. This makes the cannulation of the superior mesenteric artery difficult.
14. The ileocolic artery is the most prominent vessel in the colic mesentery of the right lower side.
15. The traction of the caecum in the direction of the anterior superior iliac crest causes the tenting of the mesentery. This allows easy identification of the vessel during laparoscopic surgery.
Marginal artery
Introduction: It is a single arterial trunk formed by the anastomosis of the colic arteries.
1. Synonymous: Marginal artery of Drummond.
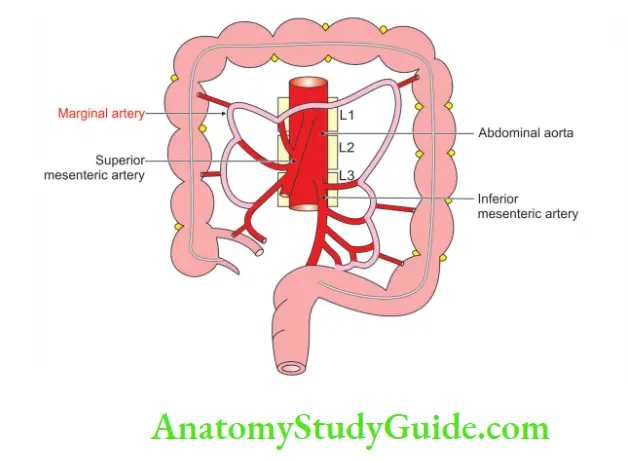
2. Site: It is around the concave margin of the large intestine.
3. Begin: It begins at the ileocaecal junction.
4. Anastomoses with:
- Ileal branches of the superior mesenteric artery.
- Superior rectal artery.
5. Applied anatomy:
In chronic, progressive occlusion of the superior mesenteric artery, the marginal artery of the colon may become massively dilated.
Question – 4: Describe the portal vein under the following heads
1. Gross anatomy
2. Development, and
3. Applied anatomy.
Answer:
Introduction: The portal system consists of all the veins which carry blood from the abdominal part of the alimentary canal.
The exceptions are the lower part of the rectum and the whole of the anal canal. It also drains blood from the pancreas, spleen and gallbladder. From all these viscera, blood is carried to the liver via one channel called the portal vein.
The blood of the portal system traverses two sets of capillaries.
They are as follows:
- Capillaries in the wall of the gut and other viscera.
- In the liver, it ends in the sinusoids.
- The blood is collected by the central vein and opens into the hepatic vein which drains into the inferior vena cava.
1. Gross anatomy
Formation:
1. Length: 8 cm.
2. Formation:
By the union of:
- Superior mesenteric vein, and
- Splenic vein.
Relation at formation:
- Behind the neck of the pancreas
- In front of inferior vena cava
- At the level of the 2nd lumbar vertebra.
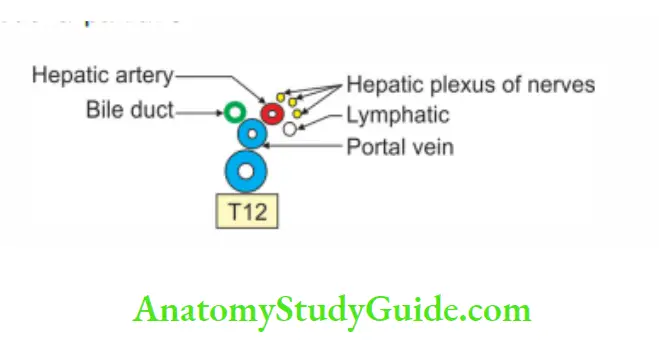
2. Course and relation:
1. Course: It runs upward and a little to the right. The course is described in three parts
- 1st part of the portal vein runs behind the neck of the pancreas
- 2nd part runs behind the 1st part of the duodenum.
- 3rd part runs in the right free margin of the lesser omentum.
2. Relations: Relations are described in three parts
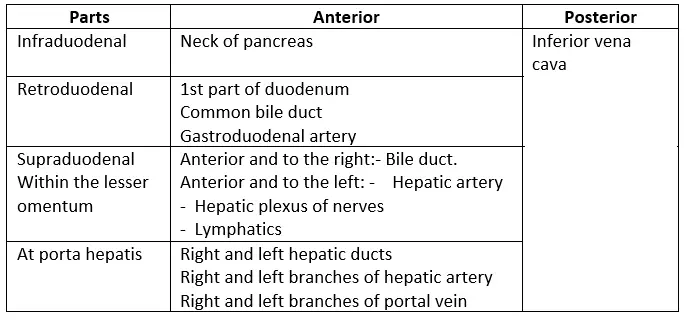
3. Branches:
Right branch
- It is shorter and wider.
- It enters the right lobe of the liver after receiving a cystic vein.
Left branch
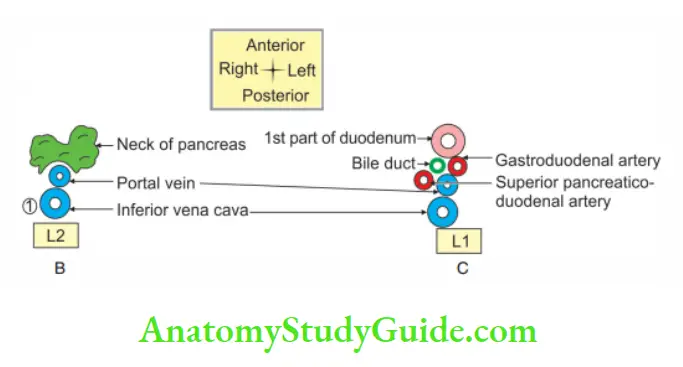
(B) Relations of intraduodenal part of portal vein at AB
(C) Relations of Retroduodenal part of portal vein at CD
- It is longer and narrower than the right.
- It traverses the porta hepatis from its right end to the left end.
- It gives branches to caudate and quadrate lobes.
- It receives the paraumbilical vein in the following ligaments. Ligamentum teres, and Ligamentum venosum.
4. Tributaries: It receives the following veins
At the origin
- Splenic vein, and
- Superior mesenteric vein.
From the main stem
- Left gastric vein
- Right gastric vein, and
- Superior pancreaticoduodenal vein.
From the right branch: Cystic vein.
From the left branch: Paraumbilical vein.
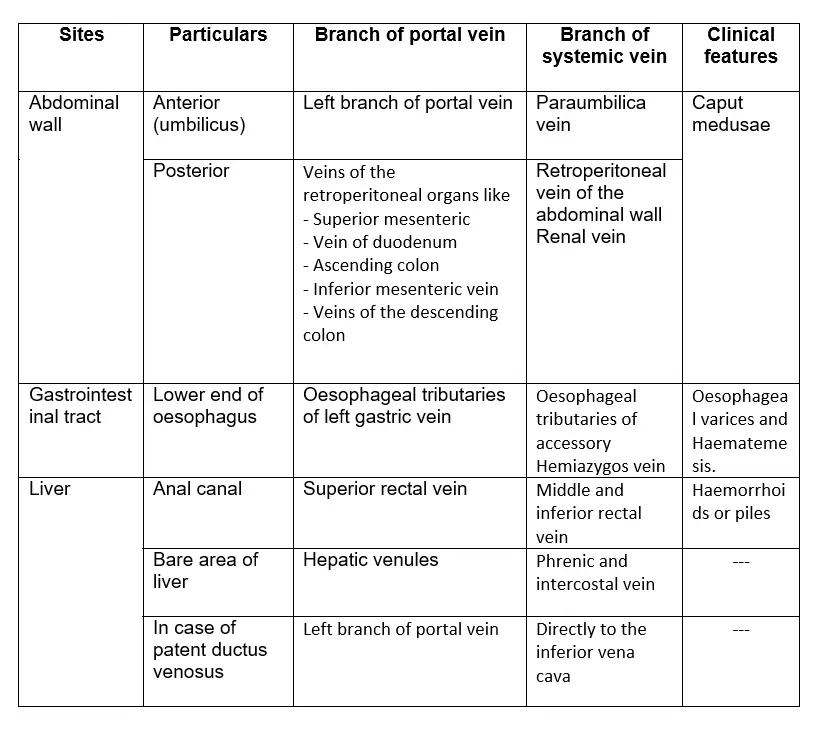
5. Portosystemic anastomosis
2. Development
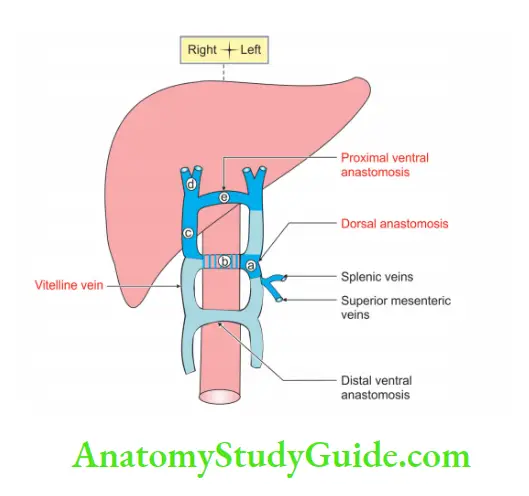
Chronological age: It develops in the 2nd and 3rd month of intrauterine life
Sources:
1. The intraduodenal part develops from the left vitelline vein between
- Joining of the splenic vein and superior mesenteric vein, and
- Dorsal intervitelline anastomosis.
Portosystemic anastomosis:
2. Retroduodenal part develops from dorsal anastomosis between
- Right vitelline, and
- Left vitelline veins
3. Supraduodenal part develops from the right vitelline vein between the
- Cephalic ventral anastomosis, and
- Dorsal anastomosis.
4. Right branch: From the part of the right vitelline vein cephalic to the ventral anastomosis.
5. Left branch: From
- Cephalic ventral anastomosis, and
- Part of the left vitelline vein cephalic to the ventral anastomosis
3. Applied anatomy
1. Portal pressure
- Normal pressure in the portal vein is about 5 to 15 mm Hg.
- Earlier it was measured by a splenic puncture.
- Presently, it is recorded by colour Doppler ultrasonography, a non-invasive method.
2. Portal hypertension: The causes are grouped as
Presinusoidal:
- Portal vein thrombosis
- Splenic vein thrombosis, and
- Congenital malformation of portal vein
Sinusoidal:
- Cirrhosis of the liver (hepatic)
- Portal fibrosis
Postsinusoidal:
- Thrombosis of hepatic vein
- Budd-Chiari syndrome, and
- Secondaries.
3. The effects of portal hypertension are
- Congestive splenomegaly
- Ascites
- Collateral circulation through portosystemic anastomosis, and
- Varix formation.
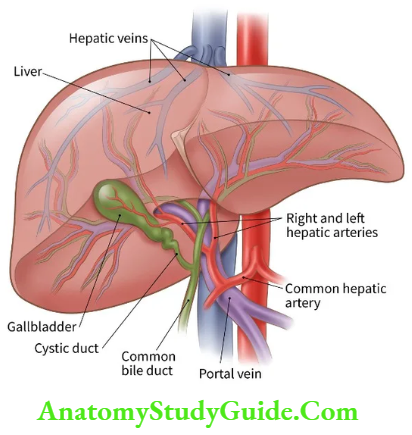
Enumerate the branches of the hepatic artery (hepatic artery proper)
1. Right hepatic artery: It gives cystic artery.
2. Left hepatic artery
Hepatic artery proper:
1. Definition
The part of the artery beyond the origin of the gastroduodenal artery is often called the hepatic artery proper.
2. Course
- It runs to the right and downwards on the posterior abdominal wall. It reaches the superior part of the duodenum.
- It turns upward to enter the free margin of the lesser omentum. It forms the anterior boundary of the epiploic foramen.
- It reaches the porta hepatis.
- It divides into the right and left branches for the corresponding lobes of the liver.
Liver:
Please note, that the terminal branches of the hepatic artery are functional end arteries, their anastomosis being insignificant.
1. It is important to remember that the caudate and quadrate lobes of the liver, physiologically, belong to the left lobe of the liver.
2. The quadrate lobe is supplied exclusively by the left hepatic artery while the caudate lobe is supplied by both arteries.
3. At times, the right hepatic artery crosses in front of the common hepatic duct, by taking a tortuous course.
4. Tortuosity of the right hepatic artery is known as caterpillar turn or Moynihan hump.
5. In most cases, the right hepatic artery is sandwiched between the hepatic duct and portal vein.
6. It’s good that it doesn’t get pinched off.
3. Branches
The right hepatic artery gives a branch to the gallbladder called the cystic artery.
It runs across the cystohepatic of Calot. It has important anatomical variations in its origin and course.
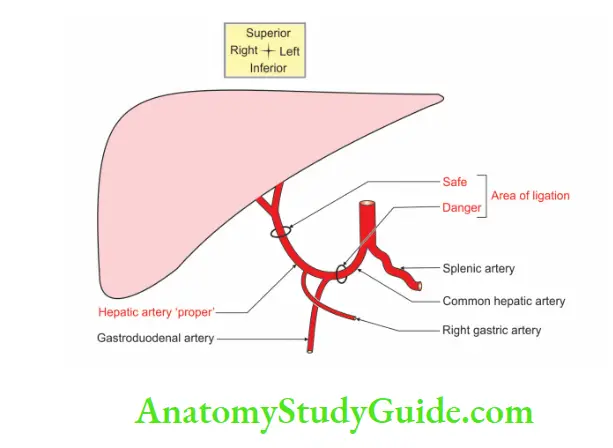
4. Applied anatomy
1. The ligation of the right and left hepatic arteries does not usually lead to infarction of the liver.
2. This is because about 75% of total hepatic blood flow is derived from the portal vein and only the remaining 25% comes from the hepatic artery.
3. It is pertinent to note that the obstruction of the common hepatic artery proximal to the right gastric artery may save the liver from necrosis.
4. This is due to an establishment of collateral circulation between the gastric and gastroepiploic arteries.
5. But when the occlusion affects the hepatic artery properly, liver necrosis is inevitable, as there is the least chance of development of collateral circulation to the liver.
6. The cystic artery may be thrombosed in case of cholecystitis but it will not result in gangrene of the gallbladder.
7. This is because of the rich blood supply coming from the liver bed.
8. In gallbladder surgery, 1st cystic artery must be identified and ligated.
9. A word of caution: Ligating the right hepatic artery and dividing it may cause profuse haemorrhage and death of the patient.
Cabot’s 
1. Synonymous:
Cystohepatic
![]()
2. Boundaries
- The upper border by the liver
- Left border by a common hepatic duct, and
- The inferior border is formed by the cystic duct.
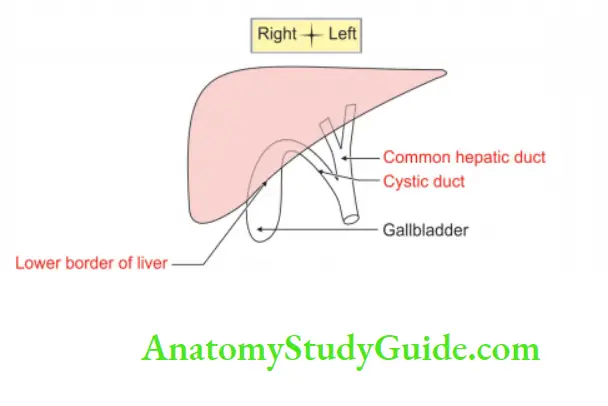
3. Applied anatomy
1. In gallbladder surgery, a surgeon controls the bleeding of the cystic artery.
He places the index finger in the epiploic foramen, the thumb anterior to the lesser omentum, and then compresses the hepatic artery. This is called Pringle’s Manoeuvre.
2. This technique is also useful in
- Palpation of gallstones in the bile duct
- Control of haemorrhage due to rupture of the cystic artery.
Branches of common hepatic artery
1. Right gastric artery
2. Gastroduodenal artery, and
3. Hepatic artery proper.
The common hepatic artery
1. Origin: It arises from the coeliac axis.
2. Branches: It divides into
- Right gastric artery,
- Gastroduodenal artery, and
- The hepatic artery is proper.
1. Right gastric artery: The right gastric artery runs between the two layers of the lesser omentum and anastomoses with the left gastric artery.
It supplies blood to the lesser curvature of the stomach and the 1st part of the duodenum.
2. Gastroduodenal artery: Gastroduodenal artery is a short but wide artery. It passes down behind the 1st part of the duodenum. It descends in front of the neck of the pancreas.
It remains to the left of the bile duct. At the lower border of the first part of the duodenum, it divides into two branches:
Right gastroepiploic artery: It passes ahead between the 1st part of the duodenum and the pancreas.
It turns to the left to enter between the two leaves of the greater omentum and anastomoses with the left gastroepiploic artery.
It gives off branches at right angles. They are to
- Anterior and posterior walls of the stomach
- The lower half circumference of the proximal half of the 1st part of the duodenum, and
- Greater omentum.
Superior pancreaticoduodenal artery: It runs along the pancreaticoduodenal groove and anastomoses with the inferior pancreaticoduodenal artery.
The pancreaticoduodenal groove is an extremely vascular region.
The duodenum often becomes ischaemic, if separated from the pancreas.
- In addition to these arteries, the
- Supraduodenal artery of Wilkie, and
- Retroduodenal arteries are the branches often arising from the gastro-duodenal artery.
The supraduodenal branch is an end artery, supplying upper
- Margin
- Two-thirds of the anterior surface, and
- One-third of the posterior surface of the proximal half.
3. Applied anatomy
1. The gastroduodenal artery denotes the junction of the
- Head with the neck of the pancreas, and
- Common hepatic artery and hepatic artery proper.
2. The gastroduodenal artery is clinically important because it is usually invaded by a posterior duodenal ulcer or tumour which results in severe haemorrhage in the peritoneal cavity.
3. Hence, the gastroduodenal artery is called the artery of duodenal haemorrhage.
4. The condition mentioned above should be suspected and looked into if the patient complains of pain in the lower lumbar region.
5. The thrombosis of the supraduodenal artery of Wilkie leads to the Curling’s ulcer in burns which may cause severe bleeding.
Interestingly, the anastomotic site between the superior and inferior pancreaticoduodenal artery represents the site of the junction of the foregut and the midgut at the level of the major duodenal papilla.
Enumerate the branches Of The Abdominal Aorta
1. Paired
- Inferior phrenic artery
- Middle suprarenal artery
- Renal artery
- Gonadal artery
- Common iliac artery
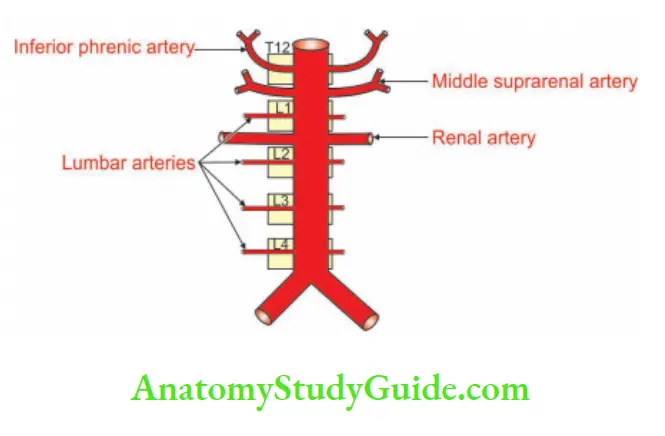
2. Unpaired
- Coeliac trunk
- Superior mesenteric artery
- Inferior mesenteric artery
- Median sacral artery
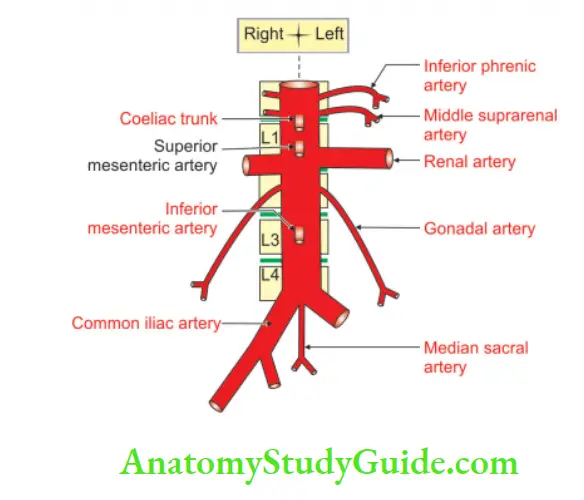
Abdominal aorta
Introduction: The abdominal aorta is the largest artery of the abdomen supplying oxygenated blood to the structures in the abdomen and pelvis. It is approximately 10-13 cm long and 2 cm in diameter. It continues as the artery of the lower limbs.
1. Origin
It is the continuation of the descending thoracic aorta at the level of the 12th thoracic vertebra.
2. Course and relations
1. It passes behind the median arcuate ligament.
2. It enters the abdomen between the crura of the diaphragm.
3. It passes downwards behind the peritoneum.
4. It passes in front of the upper 4 lumbar vertebrae.
5. It inclines slightly to the left. It leaves a sympathetic chain along its left margin.
6. Between the origins of the coeliac trunk and the superior mesenteric artery, it is crossed by the splenic vein and the body of the pancreas. These structures form the stomach bed.
7. Between the origins of superior and inferior mesenteric arteries, the structures present in front from above downwards are the
- Left renal vein
- Uncinate process of the pancreas, and
- 3rd part of duodenum.
3. Branches
They are grouped as 1st, 2nd and 3rd.
1. The first group consists of three anterior unpaired branches supplying blood to the viscera. They are
- Coeliac trunk
- Superior mesenteric artery, and the ventral
- Inferior mesenteric artery
2. The second group consists of three lateral paired branches which also supply the viscera. They are
- Suprarenal artery
- Renal artery, and
- Gonadal artery.
3. The third group consists of five lateral paired branches that supply the body wall. They are
- One inferior phrenic artery, and
- Four lumbar arteries.
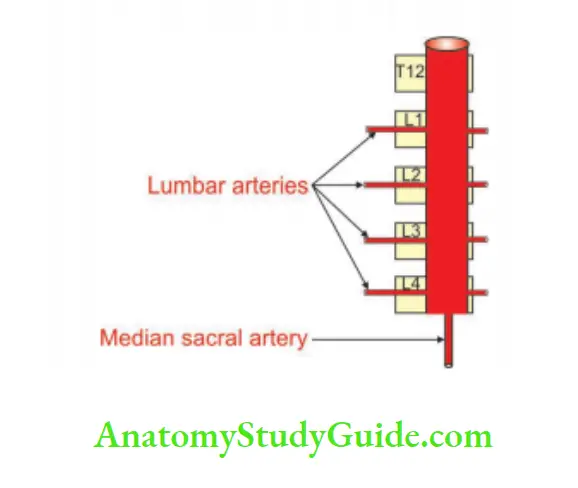
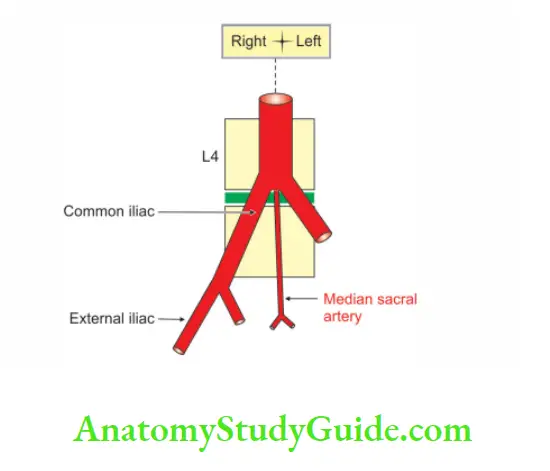
4. Abdominal aorta trifurcates, i.e. it gives off three branches at the lower border of the 4th lumbar vertebra into paired common iliac arteries and unpaired median sacral artery
4. Applied anatomy
1. Any tumour arising from the pancreas or stomach may transmit the pulsations of the aorta. These can be mistaken for an aneurysm of the abdominal aorta.
2. The dilatation of the artery is called an aneurysm. It appears as a pulsatile, palpable, painless abdominal swelling, left of midline.
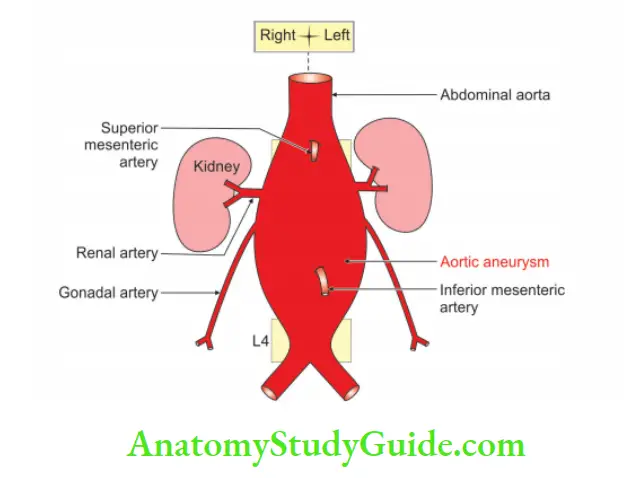
3. In case of rupture, the blood enters a third part of the duodenum. The patient vomits blood and also passes black stool or frank blood through the rectum.
4. It is diagnosed by aortography, ultrasound and CT scan.
5. The narrowing of the abdominal aorta is called coarctation or stenosis.
6. The abdominal aorta is one of the sites of atheromatous deposits.
7. Atheroma at the bifurcation of the aorta leads to the ischaemia of lower limbs. The patient feels pain while walking.
8. It is called claudication. It may end in gangrene of the leg.
9. The chronic atherosclerosis of the distal segment of the abdominal aorta is called Leriche syndrome.
10. It manifests as claudication and pallor. On examination, one does not get the femoral pulsations.
11. Lack of blood flow into the internal iliac arteries can lead to impotence.
Inferior phrenic arteries
Introduction: They are the main arteries of the abdominal surface of the diaphragm. They also supply blood to the anterior, posterior and lateral walls of the abdomen.
1. Origin
They are the 1st paired branches of the front part of the abdominal aorta.
2. Course and relations
1. Each passes upwards and laterally, in front of the corresponding crus of the diaphragm.
2. Each passes along the medial border of the suprarenal gland.
3. It supplies the main mass of the diaphragm arising from the crus.
4. The left phrenic artery passes behind the oesophagus and runs forward on the left side of the oesophageal opening.
5. The right inferior phrenic artery passes behind the inferior vena cava and runs on the right side of caval opening of the diaphragm.
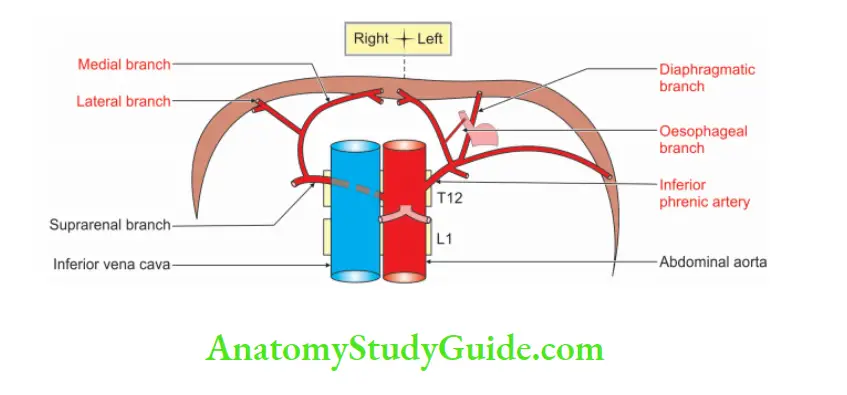
3. Branches
1. Each inferior phrenic artery gives off 2 or 3 small superior suprarenal branches to the suprarenal glands of its own side.
2. Each divides into medial and lateral branches near the posterior border of the central tendon of the diaphragm.
3. The medial branch curves forward and anastomoses with the three branches. They are with
- Opposite inferior phrenic artery
- Musculophrenic artery, and
- Pericardiacophrenic arteries.
The lateral branch on the right side supplies the inferior vena cava and liver, whereas on the left side, supplies to the oesophagus, liver and spleen.
Question 5: Describe the abdominal aorta under the following heads
1. Gross anatomy
2. Histology
3. Development, and
4. Applied anatomy.
Answer:
1. Gross anatomy
1. Origin: It is the continuation of the thoracic aorta below the diaphragm and behind the median arcuate ligament.
2. Termination: It terminates at the lower border of the L4 vertebra by dividing into two common iliac arteries.
3. Extent: It extends from the lower border of T12 to the lower border of L4.
4. Course: It descends in front of the bodies of L1 to L4 vertebrae. It lies slightly to the left of the midline.
5. Relations:
Anterior:
1. Vessels
- Coeliac artery
- Gonadal arteries
- Superior mesenteric artery
- Left renal vein
- Splenic vein
2. Coeliac plexus
3. Body of pancreas
4. Peritoneum
- Parietal peritoneum
- Root of mesentery
Posterior: Structures are related to lumbar vertebra. The key structure is the lumbar vertebra.
- The left border of L1 to L4 vertebrae
- Intervertebral disc
- Anterior longitudinal ligament
- The initial part of the lumbar arteries
- 3rd and 4th lumbar veins
- Left psoas major
Right:
1. Cisterna chyli
2. Lumbar azygos vein
3. Right
- Crus of the diaphragm
- Coeliac ganglion
4. IInferior vena cava
Left
1. Left
- Crus of the diaphragm
- Coeliac ganglion
- Sympathetic trunk
2. 4th part of duodenum
3. Duodenojejunal flexure
4. Inferior mesenteric vessels
6. Branches
Paired:
- Inferior phrenic artery
- Middle suprarenal arte
- Renal artery
- Gonadal artery
- Common iliac artery
Unpaired:
- Coeliac trunk
- Superior mesenteric artery
- Inferior mesenteric artery
- Median sacral artery
2. Histology
The histology of the abdominal aorta is the same as the elastic artery. It consists of three coats
1. Tunica intima consists of:
- Endothelium lined by simple squamous epithelium.
- Subendothelial connective tissue. It is prominent.
2. Tunica media is the thickest coat and consists of:
- Elastic fibres.
- Internal elastic lamina. It is fenestrated and is formed by elastic fibres. It is indistinguishable from the media.
3. Tunica adventitia, a thin-walled outer coat.’
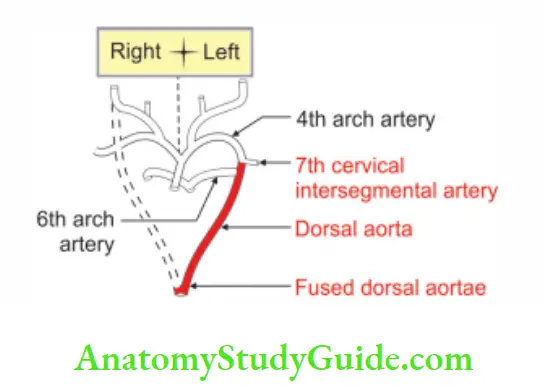
3. Development
1. Chronological age: The vascular system appears in the middle of 3rd week.
2. Germ layer: Mesoderm.
3. Source: The descending aorta is developed from the fusion of two primitive dorsal aortae.
The fusion extends from the 4th thoracic to 4th lumbar segments.
The median partition disappears and it becomes 1 tube which forms descending thoracic aorta and abdominal aorta.
The descending aorta is derived from the
- Left dorsal aorta below the attachment of 4th arch artery, and
- Fused median vessels
4. Applied anatomy
1. In thin individuals, the abdominal aorta can be palpated and auscultated.
2. Pre-renal coarctation (stenosis of the abdominal aorta) leads to a reduction of blood to the kidneys. It is more likely to be fatal.
3. Any tumour arising from the pancreas or stomach may transmit the pulsations of the aorta. This can be mistaken for an aneurysm of the abdominal aorta.
4. The dilatation of the artery is called an aneurysm.
1. Features:
- It usually results from a congenital or acquired weakness of the arterial wall.
- It is common in abdominal aorta.
2. Sites of aneurysm: Where the branches arise.
3. Clinical manifestations;
1. It appears as a
- Pulsatile
- Palpable
- Painless abdominal swelling, left of midline.
2. The large aneurysm may erode into the adjacent vertebra.
3. Acute rupture of aneurysm is associated with severe pain in the abdomen or back.
4. In case of rupture, the blood enters 3rd part of the duodenum.
5. The patient vomits blood and also passes black stool or frank blood through the rectum.
4. Diagnosis by:
- Aortography
- Ultrasound, and
- CT scan.
5. Treatment by:
- Synthetic graft.
- Without surgery, 80% of cases are likely to die within a year.
6. Atheromatous deposits: The abdominal aorta is one of the sites of atheromatous deposits.
- They make the walls rough and reduce the lumen.
- Atheroma at the bifurcation of the aorta leads to the ischaemia of lower limbs.
- The patient feels pain while walking.
- It is called claudication. It may end in gangrene of the leg.
7. Leriche syndrome: It is chronic atherosclerosis of the distal segment of the abdominal aorta.
1. Clinical manifestations:
- Claudication and pallor
- On examination, one does not get the femoral pulsations.
- Lack of blood flow into the internal iliac arteries can lead to impotence.
- Treatment by suitable surgical techniques.
8. An operation for the removal of the thickened lining of an artery is called an endarterectomy.
Removal of a thrombus is called thrombectomy.
In some cases, segments of the aorta may be replaced or bypassed using synthetic grafts.
Cartoon of abdominal aorta:
The cartoon of the abdominal aorta is a study aid to help you understand the branches of the abdominal aorta.
1. Let us depict a cartoon of a standing person having an eyebrow, nose, ears, mouth, nipple, 4 hands, umbilicus, legs and a tail.
2. The person would not look pretty.
3. However, You will most certainly remember not only this unusual image but also all the branches of the aorta.
4. So, here’s what we need to do:
5. Take an A4 size paper.
6. Divide the paper vertically into two equal halves.
7. Divide the paper horizontally into three equal parts.
8. Draw a face in the upper one-third of the paper equidistant from the midline.
9. Draw the middle part of the body in the middle one-third of the paper.
10. Draw legs in the lower one-third of the paper.
11. Draw eyebrows, each resembling a dome of the diaphragm.
12. Draw a nose in the midline resembling the shape of the stomach.
13. Sketch the mouth, resembling a midgut loop.
14. Draw small ears.
15. Trace the upper hands with closed fists resting below the respective ears.
16. Draw the nipples.
17. Map out the umbilicus resembling a hindgut loop.
18. Draw 4 fingers of the lower hands placing horizontally on the back. They are between the lumbar vertebrae.
19. Sketch a tail.
20. Docs
21. Now associate the body parts with various branches of the abdominal aorta.
22. The eyebrows represent inferior phrenic arteries.
23. The nose defines the coeliac trunk.
24. The mouth represents the superior mesenteric artery.
25. The ears exhibit suprarenal arteries.
26. The upper hands stand for renal arteries.
27. The nipples express gonadal arteries. the word used for male ♂ and female ♀ gonads.
28. The male ♂ gonad is the testis and the artery for the testis is the testicular artery.
29. The female ♀ gonad is the ovary and the artery for the ovary is the ovarian artery.
30. The umbilicus assumes the inferior mesenteric artery.
31. The 4 fingers on the back represent lumbar arteries.
32. The legs represent common iliac arteries.
33. And finally, the tail represents the median sacral artery.
34. Now we are ready with a cartoon of abdominal aorta (
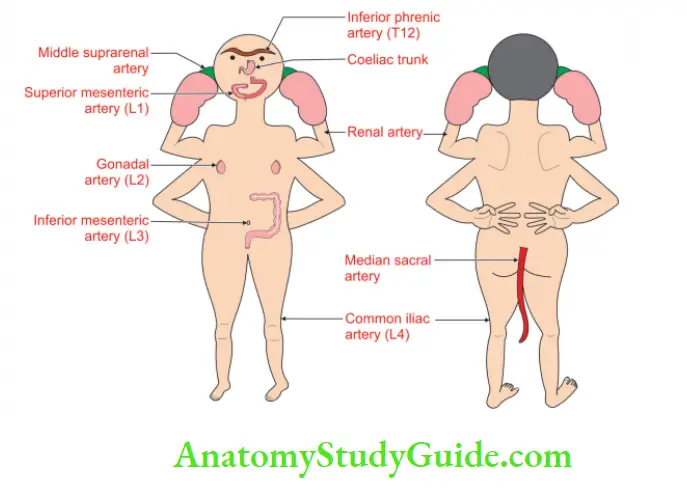
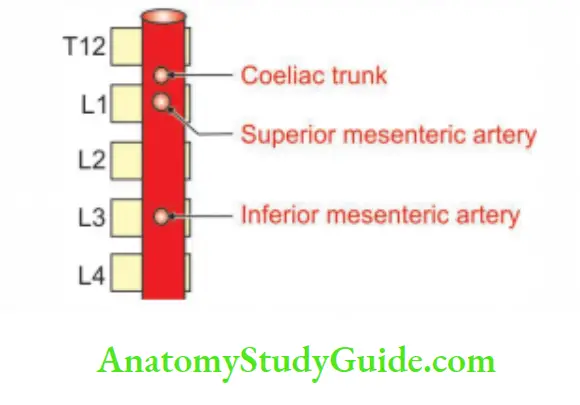
The information in the bracket following the label indicates the level of origin of the respective artery.
1. Coeliac trunk (between T12 and L1)
2.(Suprarenal (between T12 and L1)
3. Renal artery (between L1 and L2)
4. Lumbar arteries arise at the level of the body of the respective vertebra
5. Median sacral at the lower border of 4th lumbar vertebra
Question – 6: What is the vertebral level of suprarenal, renal, lumbar and median sacral arteries
Answer: Vertebral level of suprarenal, renal, lumbar and median sacral arteries
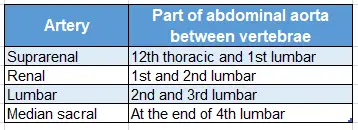
1. Technique to find out the vertebral level of suprarenal,
renal, lumbar and median sacral arteries:
Correlate the cartoon of the abdominal aorta from front and back to understand the branches of the abdominal aorta
For this,
We need to recollect the organs for which the arteries are correlating.
The ears represent suprarenal arteries.
The position of the ears is laterally and between the eyebrows and mouth.
Eyebrows represent inferior phrenic arteries which arise from the abdominal aorta at the 12th thoracic vertebra.
The mouth represents the superior mesenteric artery which arises from the abdominal aorta at 1st lumbar vertebra.
Suprarenal arteries arise from that part of the abdominal aorta which lies between the 12th thoracic vertebra and 1st lumbar vertebra.
The upper limbs represent renal arteries. Upper limbs are positioned between mouth and nipple.
Nipples represent gonadal arteries that arise from the abdominal aorta at the 2nd lumbar vertebra.
The mouth represents 1st lumbar vertebra and the nipples represent 2nd lumbar vertebra.
Hence, renal arteries arise from that part of the abdominal aorta which lies between the 1st and 2nd lumbar vertebrae.
The dorsal surfaces of 4 fingers are present at 1st, 2nd, 3rd and 4th lumbar vertebrae.
The median sacral artery arises from the dorsal surface of the abdominal aorta.
It is at the end part of the abdominal aorta, i.e. at the 4th lumbar vertebra.
Now try to answer this question:
What are the unpaired and ventral branches of the abdominal aorta?
For this
We need to perform a small trick.
We need to slide our fingers on the median plane touching the nose, mouth and umbilicus.
- The nose represents the coeliac trunk.
- The mouth represents the superior mesenteric artery.
- And finally, the umbilicus represents the inferior mesenteric artery.
2. To find the vertebral level of the branches of the abdominal aorta:
It is very simple, enjoyable and interesting to find the vertebral level of origin of the branches of the abdominal aorta.
Once you grasp the concepts clear and straight.
We need to observe three basic rules
- We have to begin from the terminal branches of the abdominal aorta.
- We need to follow the “rule of alternate”, “paired-unpaired” and so on.
- The counting of vertebrae should be from the lower vertebra to the higher vertebra.
To find out the reference point for the terminal branches of abdominal aorta
We need to appreciate the beauty of events occurring at the 4th vertebra of each series.
At the 4th cervical vertebra, the common carotid artery bifurcates into internal and external carotid arteries.
You can easily remember this by remembering “C” for “C”
in which the letter “C” refers to the Cervical vertebra and the Common carotid artery.
At the 4th thoracic vertebra, trachea bifurcates.
So, to make it easier, just remember “T” for “T” in which the letter “T” refers to the Thoracic vertebra as well as the Trachea.
At the 4th lumbar vertebra, the abdominal aorta bifurcates into the right and left common iliac artery.
Now take the 4th lumbar vertebra as a reference point and start visualizing the branches of the abdominal aorta.
Count the vertebrae from the 4th lumbar vertebra.
The vertebra of an even number is for paired branches of the abdominal aorta.
The vertebra of an odd number is for unpaired branches of the abdominal aorta.
The 4th lumbar vertebra: Vertebra with an even number has paired branches, namely common iliac arteries.
The 3rd lumbar vertebra: Vertebra with an odd number has an unpaired branch, namely the inferior mesenteric artery.
The 2nd lumbar vertebra: An even number, has paired branches, namely gonadal arteries.
The 1st lumbar vertebra: An odd number, has an unpaired branch, namely the superior mesenteric artery.
The 12th thoracic vertebra: An even number, has paired branches, namely inferior phrenic arteries
Median sacral artery
Introduction: The median sacral artery is the continuation of the abdominal aorta. Like the aorta, it clings to the vertebral column.
1. Comparative anatomy
In lower mammals, it is the anterior caudal artery that supplies the tail.
It is very prominent in reptiles like crocodiles, turtles, snakes, alligators and lizards.
It is vestigial in the tailless human species. In humans, it supplies the muscular part of the rectum and other structures.
2. Origin
It is a small, median, unpaired, parietal branch arising from the posterior part of the abdominal aorta. It arises just above the bifurcation, i.e. a little above the 4th lumbar vertebra.
3. Peculiarity
The median sacral artery is part of the posterior abdominal wall. That is to say, no organ, vessel, or nerve intervenes between a median sacral artery and the posterior abdominal wall.
4. Course and relations
1. It descends in the midline over the lower two lumbar vertebrae, the sacrum and the coccyx.
2. In its course, it is overlapped by the left common iliac vein, superior hypogastric plexus, and rectum, pairs of small arteries that run over the sacrum.
3. It provides the spinal branches that enter the pelvic sacral foramina and supply the contents of the sacral canal.
4. It may give a small lumbar artery called arteria lumbalis ima. The word ‘ima’ means the lowest. The branches of arteria lumbalis ima are visceral branches and supply the
- Rectum
- Back of anorectal junction
- Anococcygeal ligament, and
- Anal canal.
It anastomoses with the superior and middle rectal arteries.
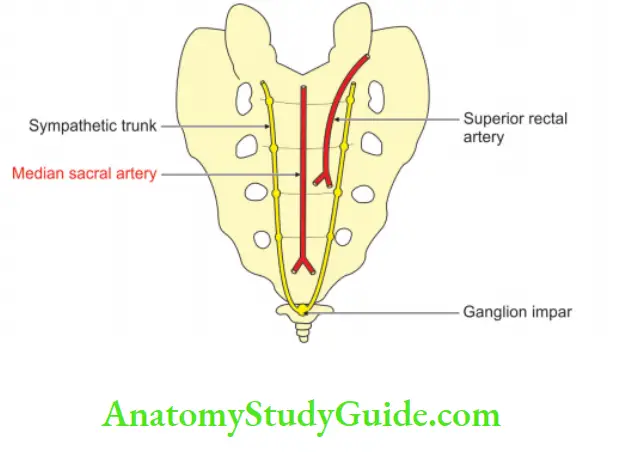
5. Termination
It ends in the coccygeal body present in front of the coccyx. It contains numerous arteriovenous anastomoses.
1. Anterior to the 5th lumbar vertebra, the median sacral artery anastomoses with a lumbar branch of the iliolumbar artery.
2. Anterior to the sacrum, it anastomoses with the lateral sacral arteries and sends branches into the anterior sacral foramina.
6. Applied anatomy
It may cause bleeding during the operation of the rectum or anal canal, hence should be handled with care.
Question- 7: What are the unpaired and ventral branches of the abdominal aorta?
Answer: Unpaired and ventral branches of the abdominal aorta:
- Coeliac trunk
- Superior mesenteric artery
- Inferior mesenteric artery
Ventral branches of abdominal aorta trick:
What are the unpaired and ventral branches of the abdominal aorta?
For this
We need to perform a small trick.
We need to slide our finger in the median plane touching the nose, mouth and umbilicus.
The nose represents the coeliac trunk.
The mouth represents the superior mesenteric artery.
And finally, the umbilicus represents the inferior mesenteric artery.
Leave a Reply