The Oral Cavity And Salivary Glands Oral Soft Tissues
Normal Structure:
Table of Contents
- The oral cavity is the point of entry for the digestive and respiratory tracts.
- The mucous membrane of the mouth consists of squamous epithelium covering vascularised connective tissue.
- The epithelium is keratinised over the hard palate, lips and gingiva, while elsewhere it is nonkeratinised.
- Mucous glands (minor salivary glands) are scattered throughout the oral mucosa.
- Sebaceous glands are present in the region of the lips and the buccal mucosa only.
- Lymphoid tissue is present in the form of tonsils and adenoids.
- The oral cavity is the site of numerous congenital and acquired diseases.
Read And Learn More: Systemic Pathology Notes
Besides, many systemic diseases have oral manifestations. Some commonly occurring conditions are discussed here.
Developmental Anomalies:
1. Facial Clefts: Cleft upper lip (harelip) and cleft palate, alone or in combination, are the commonest developmental anomalies of the face. These occur from the failure of the fusion of facial processes.
2. Fordyce’s Granules: Fordyce’s granules are symmetric, small, light yellow macular spots on the lips and buccal mucosa and represent collections of sebaceous glands. They remain undeveloped until puberty but occur quite commonly in adults.
3. Leukoedema: This is an oedematous white or grey-white lesion of the buccal and labial oral mucosa.
Histologically, there is pronounced intracellular oedema and no atypia. Unlike true leukoplakia, there is no increased malignant potential in leukoedema.
4. Developmental Defects Of The Tongue:
These are as under:
Macroglossia: is the enlargement of the tongue, usually due to lymphangioma or haemangioma, and sometimes due to amyloid tumour.
Macroglossia and aglossia: are rare congenital anomalies representing small-sized and absence of tongue respectively.
Fissured tongue (scrotal, furrowed or grooved tongue): is a genetically-determined condition characterised by numerous small furrows or grooves on the dorsum of the tongue. It is often associated with mild glossitis.
The bifid tongue: is a rare condition occurring due to the failure of the two lateral halves of the tongue to fuse in the midline.
Tongue tie: occurs when the lingual frenulum is quite short, or when the frenulum is attached near the tongue tip.
Hairy tongue: is not a true developmental defect but is mentioned here because of its similarity with other conditions discussed here.
The filiform papillae are hypertrophied and elongated. These ‘hairs’ (papillae) are stained black, brown or yellowish-white by food, tobacco, oxidising agents or oral flora.
Mucocutaneous Lesions:
Lesions of the oral mucosa occur in many diseases of the skin and they are similar in morphology.
Some of these are listed here but are described in cutaneous pathology:
Lichen Planus: Characteristically, oral lichen planus appears as an interlacing network of whitening or keratosis on the buccal mucosa but other oral tissues such as gingiva, tongue and palate may also be involved.
Vesicular Lesions:
A number of vesicular or bullous diseases of the skin have oral lesions.
Pemphigus vulgaris: Vesicular oral lesions appear invariably in all cases at some time in the course of pemphigus vulgaris.
In about half the cases oral lesions are the initial manifestations.
Pemphigoid: Vesicles or bullae appear on oral mucosa as well as on conjunctiva in pemphigoid and are seen more often in older women.
Erythema multiforme: Subepithelial vesicles may occur on the skin as well as mucosae.
Stevens-Johnson syndrome: It is a rather fatal and severe form of erythema multiforme involving oral and other mucous membranes occurring following ingestion of sulfa drugs.
Epidermolysis bullosa: It is a hereditary condition having subepidermal bullae on the skin as well as oral lesions.
Inflammatory And Pigmentary Diseases Stomatitis:
- Inflammation of the mucous membrane of the mouth is called stomatitis.
- It can occur in the course of several different diseases.
1. Aphthous, ulcers (Canker sores): These are the commonest form of oral ulcerations.
- The aetiology is unknown but may be precipitated by emotional factors, stress, allergy, hormonal imbalance, nutritional deficiencies, gastrointestinal disturbances, trauma etc.
- The condition is characterised by painful oral ulcers, 1 cm or more in size. Recurrent aphthae may form a part of Behcet’s syndrome and inflammatory bowel disease.
2. Herpetic stomatitis: is an acute disease occurring in infants and young children.
- It is the most common manifestation of primary infection with herpes simplex virus. The lesions are in the form of vesicles around the lips. Similar lesions may appear on the genital skin.
- Recurrent attacks occur due to stress, emotional upsets and upper respiratory infections.
Necrotising stomatitis (Noma or Cancrum oris): This occurs more commonly in poorly nourished children like in Kwashiorkor; infectious diseases such as measles, immunodeficiencies and emotional stress.
The lesions are characterised by necrosis of the marginal gingiva and may extend onto oral mucosa, causing cellulitis of the tissue of the cheek. The condition may progress to gangrene of the cheek.
Mycotic infections: Fungal infections commonly involving the oral mucosa are actinomycosis and candidiasis.
- Cervicofacial actinomycosis is the commonest form of the disease developing at the angle of the mandible. Candidiasis (moniliasis or thrush) is caused by Candida albicans which is a commensal in the mouth.
- It appears as an opportunistic infection in the immunocompromised host. There are erythematous lesions on the palate and angular cheilitis.
- Glossitis: Acute glossitis characterised by swollen papillae occurs in eruptions of measles and scarlet fever.
- In chronic glossitis, the tongue is raw and red without swollen papillae and is seen in malnutrition such as in pellagra, ariboflavinosis and niacin deficiency.
- In iron deficiency anaemia, pernicious anaemia and sprue, there is chronic atrophic glossitis characterised by atrophied papillae and smooth raw tongue.
Syphilitic Lesions: Oral lesions may occur in primary, secondary, tertiary and congenital syphilis.
- Extragenital chancre of primary syphilis occurs most commonly on the lips.
- Secondary syphilis shows maculopapular eruptions and mucous patches in the mouth.
- In tertiary syphilis, gummas or diffuse fibrosis may be seen on the hard palate and tongue.
- Oral lesions of congenital syphilis are fissures at the angles of the mouth and characteristic peg-shaped notched Hutchinson’s incisors.
Tuberculous Lesions:
Involvement of the mouth in tuberculosis is rare. The lesions are in the form of ulcers or elevated nodules.
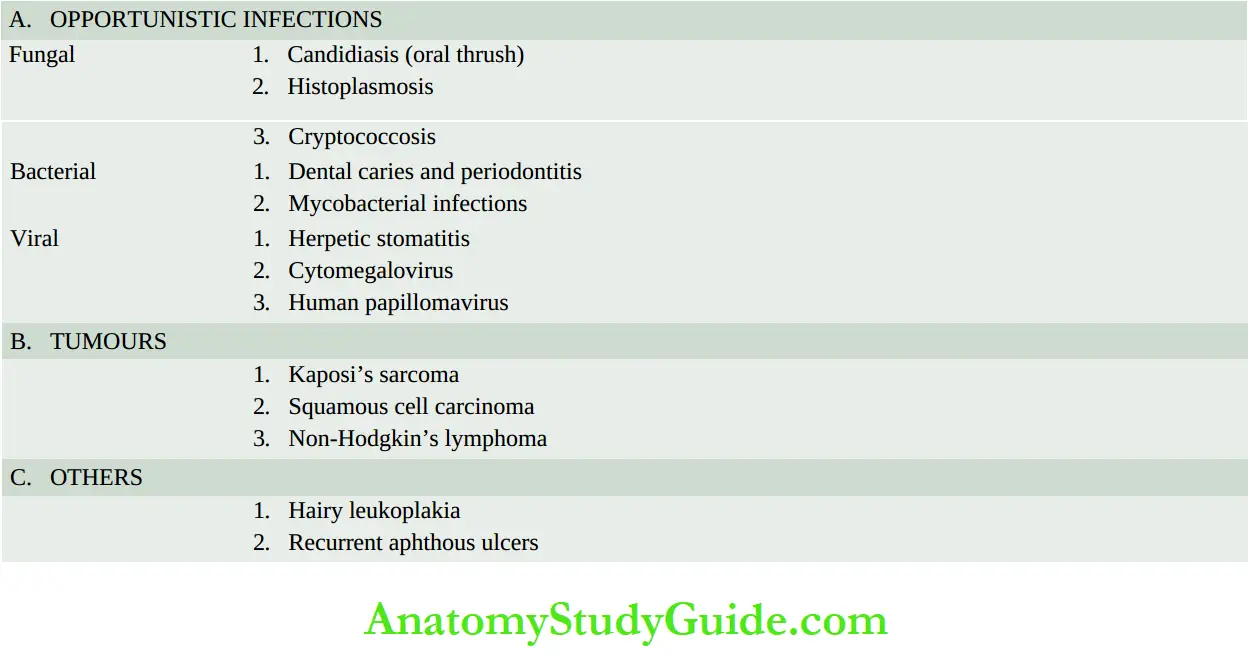
HIV Infection: HIV infection of low-grade as well as full-blown acquired immunodeficiency syndrome (AIDS) are associated with oral manifestations such as opportunistic infections, malignancy, hairy leukoplakia and others; these are listed in about half the cases of Kaposi’s sarcoma and have intraoral lesions as part of systemic involvement.
Pigmentary Lesions: Oral and labial melanotic pigmentation may be observed in certain systemic and metabolic disorders such as Addison’s disease, Albright syndrome, Peutz-Jeghers syndrome and haemochromatosis.
All types of pigmented naevi as well as malignant melanoma can occur in the oral cavity. Exogenous pigmentation such as due to the deposition of lead sulfide can also occur.
Tumours And Tumour-Like Lesions:
Benign and malignant tumours as also a number of tumour-like lesions and premalignant lesions are encountered in the oral soft tissues.
1. Tumour-Like Lesions
Fibrous growths (Fibroepithelial polyps, fibrous epulis, denture hyperplasia)
- Pyogenic granuloma
- Mucocele
- Ranula
- Dermoid cyst
- Fibromatosis gingivae
2. Benign Tumours
- Papilloma (variants: squamous papilloma, condyloma acuminatum)
- Haemangioma
- Lymphangioma
- Fibroma
- Tumours of minor salivary glands
- Granular cell tumour
3. Epithelial Precursor Lesions
- Leukoplakia
4. Malignant Tumours
- Squamous cell carcinoma (variants: verrucous, basaloid, adenoid, spindle cell, adenosquamous)
- Other malignant tumours
1. Tumour-Like Lesions:
A number of proliferative lesions arising from the oral tissues are tumour-like masses which clinically may resemble neoplasms.
Some of these are as under:
Fibrous Growths:
Fibrous growths of the oral soft tissues are very common. These are not true tumours (unlike intraoral fibroma and papilloma), but are instead inflammatory or irritative in origin.
A few common varieties are as under:
Fibroepithelial polyps: occur due to irritation or chronic trauma. These are composed of reparative fibrous tissue, covered by a thin layer of stratified squamous epithelium.
Fibrous epulis: a lesion occurring on the gingiva and is localised hyperplasia of the connective tissue following trauma or inflammation in the area.
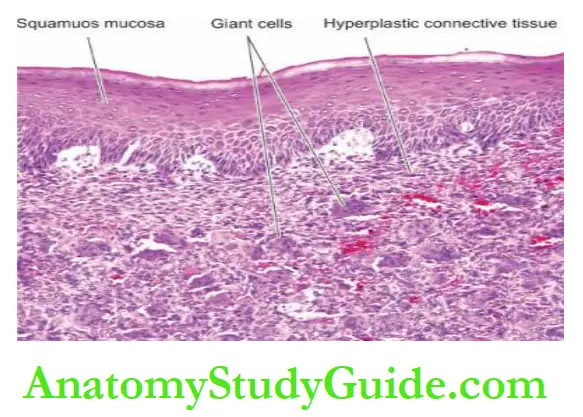
Giant cell epulis is a variant seen more commonly in females as a reactive change to trauma; the lesion shows numerous osteoclast-like giant cells and vascular stroma.
Denture hyperplasia: occurs in edentulous or partly edentulous patients.
The lesion is inflammatory hyperplasia in response to local irritation by an ill-fitting denture or an elongated tooth.
Fibromatosis gingivae: This is a fibrous overgrowth of unknown etiology involving the entire gingiva. Sometimes the fibrous overgrowth is so much that the teeth are covered by fibrous tissue.
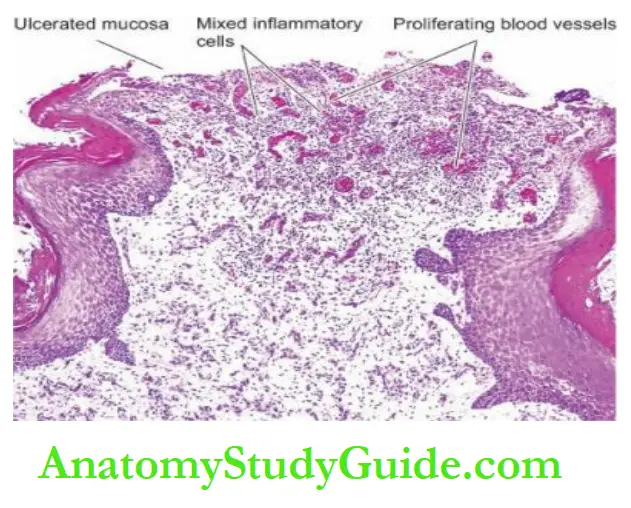
Pyogenic Granuloma: This is an elevated, bright red swelling of variable size occurring on the lips, tongue, buccal mucosa and gingiva. It is a vasoproliferative inflammatory lesion. A pregnancy tumour is a variant of pyogenic granuloma.
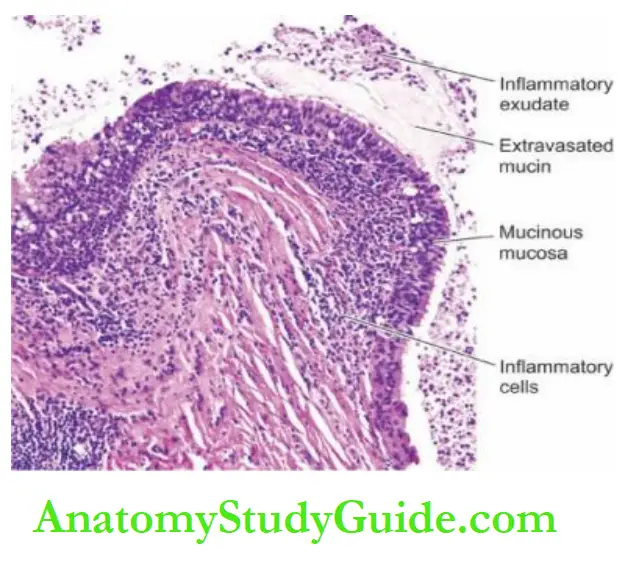
Mucocele: Also called mucous cyst or retention cyst, it is a cystic dilatation of the mucous glands of the oral mucosa. The cyst often ruptures on distension and incites inflammatory reactions due to mucous extravasation.
Ranula: It is a large mucocele located on the floor of the mouth. The cyst is lined by true epithelial lining.
Dermoid Cyst: This tumour-like mass in the floor of the mouth represents a developmental malformation.
The cyst is lined by stratified squamous epithelium. The cyst wall contains sebaceous glands, sweat glands, hair follicles and other mature tissues.
2. Benign Tumours:
Different parts of the mouth have a variety of mesodermal tissues and keratinising and non-keratinising epithelium. Therefore, the majority of neoplasms arising from the oral tissues are just like their counterparts in other parts of the body.
Some of the common benign tumours of the mouth are as under:
Papilloma: Oral squamous cell papilloma is common and can occur anywhere in the mouth and has the usual papillary or finger-like projections. Oral condyloma acuminatum is an HPV-induced sexually transmitted papillary lesion similar too genital warts.
Microscopically, oral squamous papilloma is composed of vascularised connective tissue cores covered by multiple layers of benign squamous epithelium.
Haemangioma: Haemangioma can occur anywhere in the oral cavity; when it occurs on the tongue it may produce macroglossia. It is most commonly capillary type, although cavernous and mixed types may also occur.
Lymphangioma: Lymphangioma may develop most commonly on the tongue-producing macroglossia; on the lips-producing macrocheilia, and on the cheek. Cystic hygroma is a special variety of lymphangiomas occurring in children on the lateral side of the neck.
Microscopically, lymphangioma is characterised by large lymphatic spaces lined by endothelium and containing lymph.
Fibroma: Although the most common benign oral mucous membrane mass is fibroma appearing as a discrete superficial pedunculated mass, it appears to be non-neoplastic in nature. It probably arises as a response to physical trauma.
Microscopically, fibroma is composed of collagenic fibrous connective tissue covered by stratified squamous epithelium.
Tumours Of Minor Salivary Glands: Minor salivary glands present in the oral cavity may sometimes be the site of origin of salivary tumours similar to those seen in the major salivary glands. Pleomorphic adenoma is a common example.
Granular Cell Tumour: Earlier called granular cell myoblastoma, it is a benign tumour which now by electron microscopic studies is known to be mesenchymal in origin.
The most common location is the tongue but may occur in any other location in the oral cavity. It occurs exclusively in females. A similar lesion seen in infants is termed a congenital epulis.
Microscopically, the tumour is composed of large polyhedral cells with granular, acidophilic cytoplasm. The covering epithelium usually shows pronounced pseudoepitheliomatous hyperplasia.
Other Rare Benign Tumours: Some other rare benign tumours which can occur in the oral soft tissues are neurilemmoma, neurofibroma, lipoma, giant cell granuloma, rhabdomyoma, leiomyoma, solitary plasmacytoma, osteoma, chondroma, naevi and vascular oral lesions seen in hereditary haemorrhagic telangiectasia (Osler-Rendu-Weber syndrome) and encephalofacial angiomatosis (Sturge-Weber syndrome).
3. Oral Leukoplakia (White Lesions)
Definition:
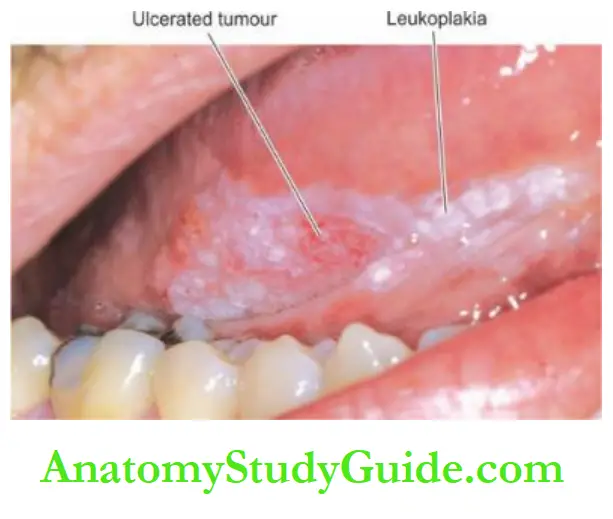
Leukoplakia (white plaque) may be clinically defined as a white patch or plaque on the oral mucosa, exceeding 5 mm in diameter, which cannot be rubbed off nor can be classified into any other diagnosable disease. A number of other lesions are characterised by the formation of white patches.
However, from the pathologist’s point of view, the term ‘leukoplakia’ is reserved for epithelial thickening which may range from completely benign to atypical and to premalignant cellular changes.
1. Benign
- Fordyce’s granules
- Hairy tongue
- Leukoedema
- Lupus erythematosus
- White sponge naevus
2. Precursor Lesions
- Leukoplakia
- Oral lichen planus
3. Malignant
- Squamous cell carcinoma
Incidence:
It occurs more frequently in males than females. The lesions may be of variable size and appearance.
The sites of predilection, in descending order of frequency, are cheek mucosa, angles of the mouth, alveolar mucosa, tongue, lip, hard and soft palate, and floor of the mouth. In about 4-6% of cases of leukoplakia, carcinomatous change is reported.
However, it is difficult to decide which white lesions may undergo malignant transformation, but the speckled or nodular form is more likely to progress to malignancy.
Therefore, it is desirable that all oral white patches be biopsied to exclude malignancy.
Etiology: The etiological factors are similar to those suggested for carcinoma of the oral mucosa (discussed below).
It has the strongest association with the use of tobacco in various forms, e.g.
in heavy smokers (especially in pipe and cigar smokers) and improves when smoking is discontinued, and in those who chew tobacco-containing products e.g. paan, paan masala, zarda, gutka etc.
The condition is also known by other names such as smokers’ keratosis and stomatitis nicotine.
Other etiological factors implicated are chronic friction such as with ill-fitting dentures or jagged teeth, and local irritants like excessive consumption of alcohol and very hot and spicy foods and beverages.
A special variety of leukoplakia called ‘hairy leukoplakia’ has been described in patients of AIDS and has a hairy or corrugated surface but is not related to the development of oral cancer.
Morphologic Features: Grossly, the lesions of leukoplakia may appear white, whitish-yellow, or red velvety of more than 5 mm diameter and variable in appearance.
They are usually circumscribed, slightly elevated, smooth or wrinkled, speckled or nodular.
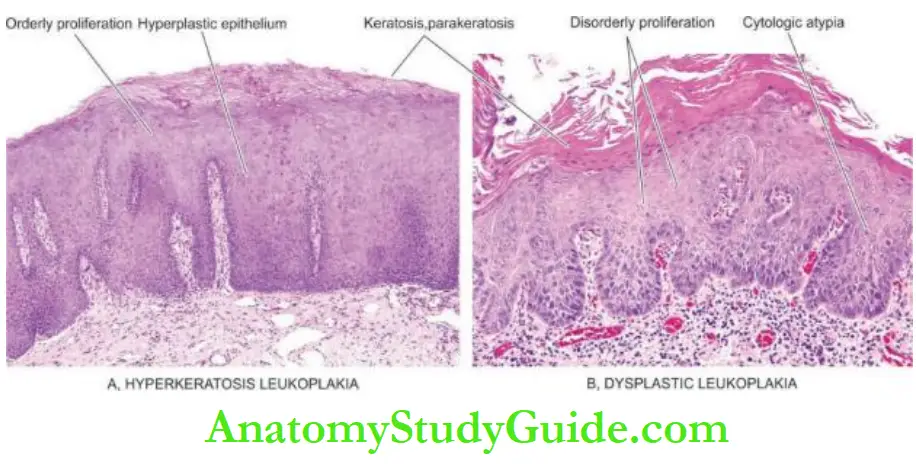
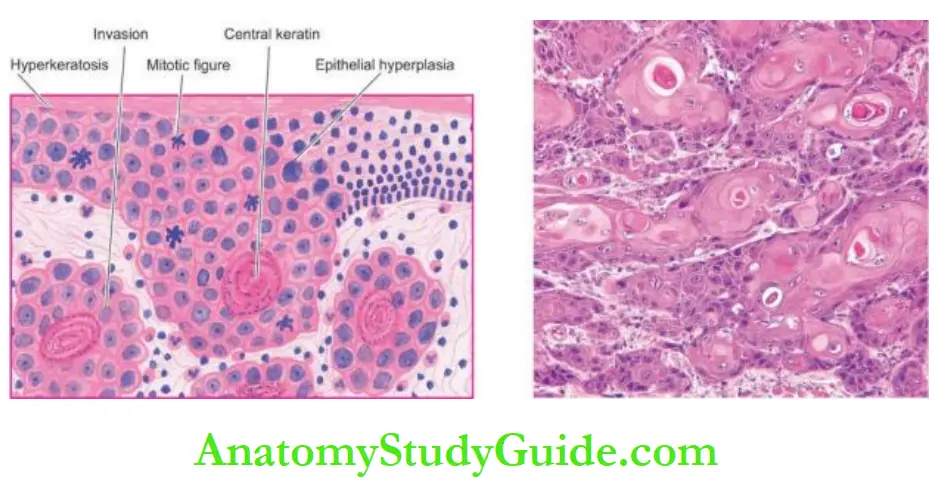
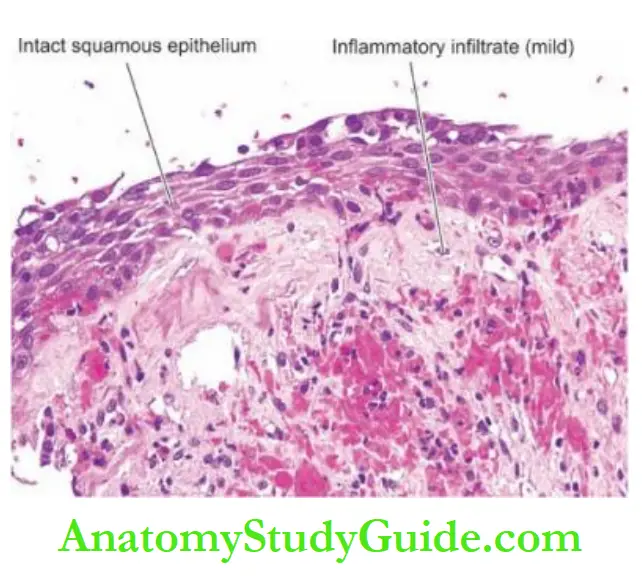
Histologically, leukoplakia is of 2 types:
1. Hyperkeratotic type: This is characterised by orderly and regular hyperplasia of squamous epithelium with hyperkeratosis on the surface.
2. Dysplastic type: When the changes such as irregular stratification of the epithelium, focal areas of increased and abnormal mitotic figures, hyperchromatism, pleomorphism, loss of polarity and individual cell keratinisation are present, the lesion is considered as epithelial
dysplasia.
The subepithelial tissues usually show an inflammatory infiltrate composed of lymphocytes and plasma cells.
The extent and degree of the epithelial changes indicate the degree of severity of the epithelial dysplasia.
Usually, mild dysplasia may revert back to normal if the offending etiologic factor is removed, whereas severe dysplasia indicates that the case may progress to carcinoma.
Erythroplasia is a form of dysplastic leukoplakia in which the epithelial atypia is more marked and thus has a higher risk of developing malignancy.
If the epithelial dysplasia is extensive so as to involve the entire thickness of the epithelium, the lesion is called carcinoma in situ which may progress to invasive carcinoma.
4. Malignant Tumours
Carcinoma Oral Cavity: Oral cancer is a disease with a very poor prognosis because it is not recognised and treated when small and early.
Incidence: Squamous cell or epidermoid carcinoma (SCC) comprises 90% of all oral malignant tumours and 5% of all human malignancies.
The peak incidence in the UK and the USA is from 55 to 75 years of age, whereas in India it is seen at a relatively younger age (40 to 45 years).
Oral cancer is a very frequent malignancy in India, Sri Lanka and some Eastern countries, probably related to habits of betel-nut chewing and reversed smoking.
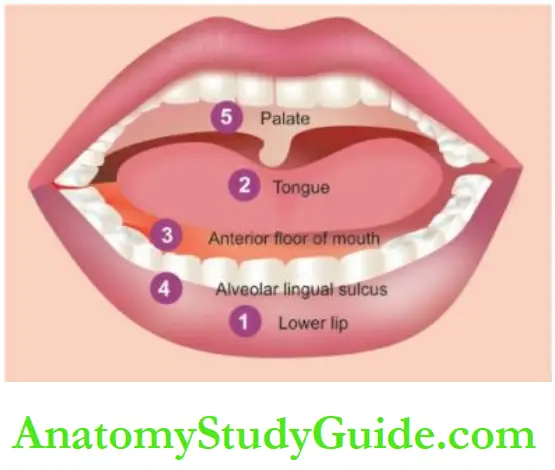
There is a definite male preponderance. It can occur anywhere in the mouth but certain sites are more commonly involved.
These sites, in descending order of frequency, are the lips (more commonly lower), tongue, the anterior floor of the mouth, buccal mucosa in the region of the alveolar lingual sulcus, and palate.
Etiology:
As with other forms of cancer, the etiology of SCC is unknown.
But a number of etiological factors have been implicated: Strong association
- Tobacco smoking and tobacco chewing causing leukoplakia is the most important factor as discussed above.
- Chronic alcohol consumption.
- Human papilloma virus infection, particularly HPV 16, 18 and 33 types.
Weak association
- Chronic irritation from ill-fitting dentures or jagged teeth.
- Submucosal fibrosis is seen in Indians consuming excess chillies.
- Poor or dental hygiene.
- Nutritional deficiencies.
- Exposure to sunlight (in relation to lip cancer).
- Exposure to radiation.
- Plummer-Vinson syndrome is characterised by atrophy of the upper alimentary tract. The most common molecular alterations in oncogenes seen in the SCC of the oral cavity are in p16, p53, p63, cyclin D, PTEN, and EGFR.
Morphologic Features: Grossly, SCC of the oral cavity may have the following types; the vicinity of the tumour may show a leukoplakic area.
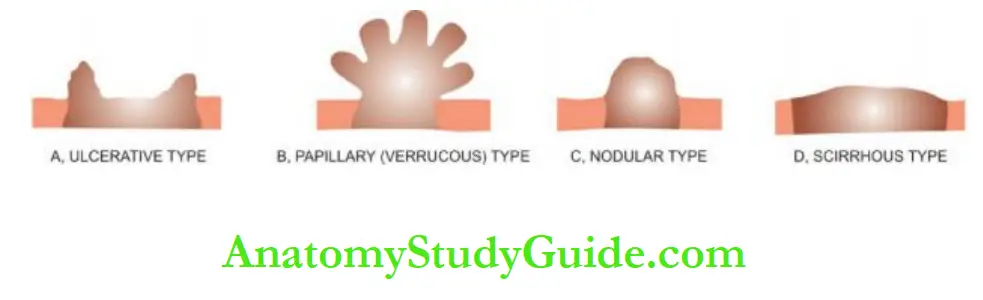
- Ulcerative type—is the most frequent type and is characterised by indurated ulcers and firm everted or rolled edges.
- Papillary or verrucous type—is soft and wart-like growth.
- Nodular type—appears as a firm, slow-growing submucosal nodule.
- Scirrhous type—is characterised by infiltration into deeper structures.
All these types may appear on a background of leukoplakia or erythroplasia of the oral mucosa.
Enlarged cervical lymph nodes may sometimes be present.
Histologically, conventional oral SCC ranges from well-differentiated keratinising carcinoma
to highly-undifferentiated neoplasm.
Changes in epithelial dysplasia are often present in the surrounding areas of the lesion. Carcinoma of the lip and intraoral squamous carcinoma are usually always well-differentiated.
A few histologic variants of oral SCC have been described which have varying prognoses:
- Verrucous carcinoma is composed of very well-differentiated squamous epithelium having broad bulbous pushing rete ridges and minimal atypia. It generally does not metastasise and hence has a very good prognosis.
- Basaloid squamous cell carcinoma shows a basaloid malignant palisade arrangement in keratinising SCC and areas of comedo necrosis. It is a high-grade tumour with distant metastases.
- Adenoid squamous cell carcinoma occurs more often on sun-exposed areas such as the lip. It shows acantholytic tumour cells projecting into a pseudo glandular pattern of SCC. It has a worse prognosis as compared to conventional SCC.
- Spindle cell carcinoma is composed of spindled malignant cells having a sarcomatoid appearance. It metastasises to regional lymph nodes frequently.
- Adenosquamous carcinoma is a biphasic tumour, having true glandular differentiation and squamous differentiation. This is an aggressive variant with distant metastases and has a poor prognosis.
Carcinoma of the lip has a more favourable prognosis due to its visible and easily accessible location and less frequent metastasis to the regional lymph nodes.
However, intraoral squamous carcinomas have a poor prognosis because they are detected late and metastasis to regional lymph nodes occur early, especially in the case of carcinoma of the tongue and soft palate.
Other Malignant Tumours: Other less common malignant neoplasms which may be encountered in the oral cavity are malignant melanoma, lymphoepithelial carcinoma,
Malignant lymphoma, malignant tumours of minor salivary glands, and various sarcomas like rhabdomyosarcoma, liposarcoma, alveolar soft part sarcoma, Kaposi’s sarcoma and fibrosarcoma. Metastatic tumours can also occur in the soft tissues of the mouth.
Diseases of Oral Soft Tissues:
- Mucocutaneous lesions of the oral cavity are similar in morphology to those in the skin and include lichen planus and vesicular lesions (pemphigus vulgaris, pemphigoid,
erythema multiforme, Stevens-Johnson syndrome etc). - Inflammatory lesions of the face are common and include aphthous ulcers, herpes, necrotising stomatitis, fungal infections, glossitis, syphilis, tuberculosis etc.
- Tumour-like lesions in the oral cavity are several types of fibrous overgrowths, pyogenic granuloma, mucocele, ranula and dermoid cyst.
- Benign lesions of the oral soft tissues are haemangioma, lymphangioma, fibroma, minor salivary gland tumours and granular cell tumours.
- Oral leukoplakia is a white patch, commonly due to the use of tobacco. It is of two types:
- hyperkeratotic or dysplastic.
- Squamous cell carcinoma (SCC) is the most common oral malignant tumour.
- Its locations, in descending order of frequency, are the lower lip, tongue, anterior floor of the mouth, buccal mucosa and palate.
- Besides conventional SCC, a few histologic variants have been
described which have varying prognoses. - Overall, intraoral cancer has a bad prognosis compared to that of lip.
Teeth And Periodontal Tissues
Normal Structure:
The teeth are normally composed of 3 calcified tissues, namely: enamel, dentin and cementum; and the pulp which is composed of connective tissue.
The teeth are more peculiar than other calcified tissues of the body by being surrounded by the portion of oral mucosa called the gingiva or gum. And that they are part of a highly specialised odontogenic apparatus; other parts of this apparatus being the mandible and maxilla.
Embryologically, odontogenic development takes place from primitive structures,
The dental lamina or primitive oral cavity, as follows:
The inner epithelial layer of the dental lamina is ectoderm-derived columnar to cuboidal oral epithelium called ameloblasts which secrete enamel matrix, also called enamel organ.
Mesoderm-derived connective tissue gives rise to structures in the dental papilla (i.e. dental pulp or core of loose connective tissue, blood vessels and nerves).
The outer margin of the dental papilla differentiates into odontoblasts, which continue with ameloblastic epithelium; odontoblasts secrete dentin.
The normal structure of a tooth in an adult is as follows:
Enamel is the outer covering of teeth composed almost entirely of inorganic material (as in bone) which can be demonstrated in ground sections only because it is lost in decalcified section.
Dentin lies under the enamel and comprises most of the tooth substance.
It is composed of organic material in the form of collagen fibrils as well as inorganic material in the form of calcium phosphates as in bone.
Dentin is composed of odontoblasts or dentin cells which are counterparts of osteocytes in bone but differ from the latter in having odontoblast processes.
Dentin in the crown of the tooth is covered with a thicker layer of enamel.
Cementum is the portion of a tooth which covers the dentin at the root of the tooth and is the site where the periodontal ligament is attached.
Cementum is similar to bone in morphology and composition.
The dental pulp is inner to dentine and occupies the pulp cavity and root canal.
It consists of connective tissue, blood vessels and nerves. Nests of odontogenic epithelium are normally present in the jaw and may develop into cysts and tumours.
Although care of the teeth belongs to the field of the dental profession, a few main diseases of teeth, jaw and periodontal tissues are briefly discussed here; these are inflammatory diseases, odontogenic cysts and odontogenic tumours of the jaw.
Inflammatory Diseases:
Dental Caries:
Dental caries is the most common disease of dental tissues, causing destruction of the calcified
tissues of the teeth.
Etiopathogenesis: Dental caries is essentially a disease of modern society, associated with a diet containing a high proportion of refined carbohydrates.
It has been known for almost 100 years that a mixture of sugar or bread with saliva in the presence of acidogenic bacteria of the mouth, especially streptococci, produces organic acids which can decalcify enamel and dentin.
Enamel is largely composed of inorganic material which virtually disintegrates.
Dentin contains organic material also which is left after decalcification.
Bacteria present in the oral cavity cause proteolysis of the remaining organic material of dentin, completing the process of destruction.
Diets rich in carbohydrates do not require much chewing and thus the soft and sticky food gets clung to the teeth rather than being cleared away, particularly in the areas of occlusal pits and fissures. ‘Bacterial plaques’ are formed in such stagnation areas.
If these plaques are not removed by brushing or by vigorous chewing of fibrous foods, the process of tooth decay begins.
There is evidence that the consumption of water containing one part per million (ppm) of fluoride is sufficient to reduce the rate of tooth decay in children.
Morphologic Features: Caries occurs chiefly in the areas of pits and fissures, mainly of the molars and premolars, where food retention occurs, and in the cervical part of the tooth.
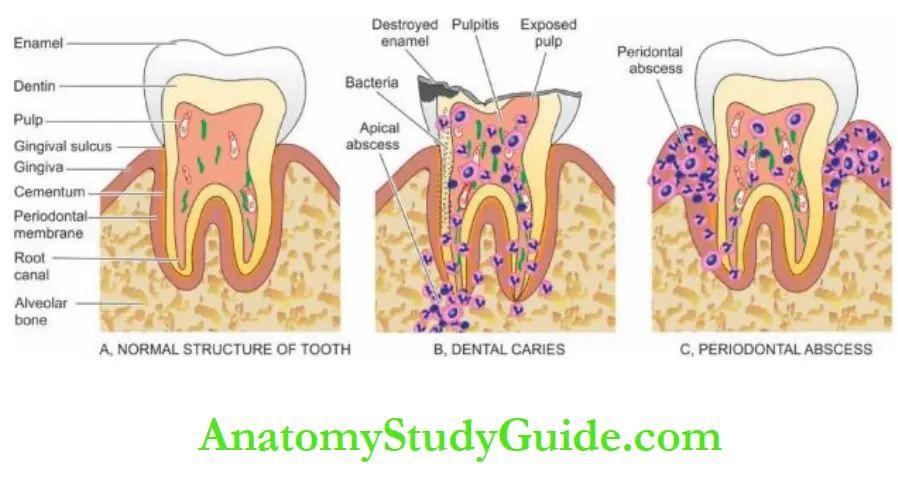
Grossly, the earliest change is the appearance of a small, chalky-white spot on the enamel which subsequently enlarges and often becomes yellow or brown and breaks down to form a carious cavity.
Eventually, the cavity becomes larger due to fractures of enamel.
Once the lesion reaches the enamel-dentin junction, the destruction of dentine also begins.
Microscopically, inflammation (pulpitis) and necrosis of the pulp take place.
There is evidence of the reaction of the tooth to the carious process in the form of secondary dentin, which is a layer of odontoblasts laid down under the original dentin
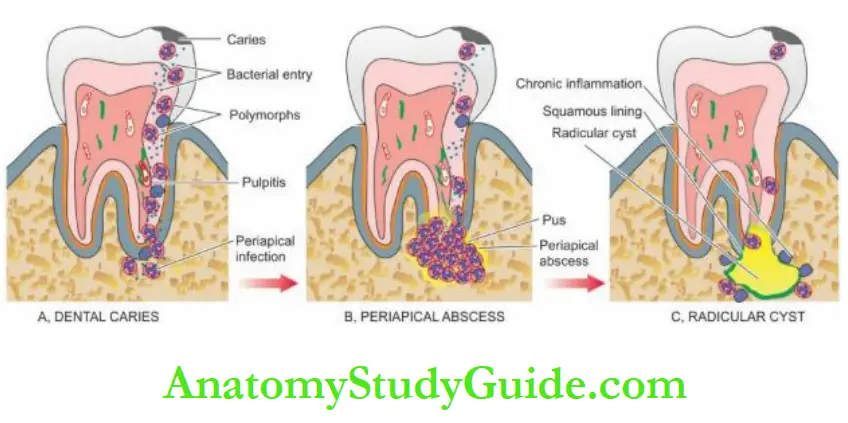
Sequelae Of Caries:
Carious destruction of dental hard tissues frequently produces pulpitis and other inflammatory lesions like apical granuloma and apical abscess.
Less common causes of these lesions are fractures of the tooth and accidental exposure to the pulp by the dentist.
1. Pulpitis: Pulpitis may be acute or chronic.
Acute pulpitis is accompanied by severe pain which may be continuous, throbbing or dull, and is accentuated by heat or cold. It is often accompanied by mild fever and leucocytosis.
Chronic pulpitis occurs when the pulp is exposed widely. It is often not associated with pain. Chronically inflamed pulp tissue may protrude through the cavity forming polyp of the pulp. It may be partly covered by implanted squamous epithelium.
2. Apical granuloma: Pulpitis may lead to the spread of infection through the apical foramen into the tissues surrounding the root of the tooth.
Histologically, there is a chronic inflammatory reaction with the formation of granulation tissue and inclusion of nests or strands of squamous epithelium derived from remnants of odontogenic epithelium normally present in the periodontal membrane.
An apical granuloma may develop into a dental (radicular) cyst as discussed below.
3. Apical abscess: An apical granuloma or acute pulpitis may develop into an apical abscess.
Acute abscess is very painful, while pus in chronic abscess may escape through the root canal and cause further complications like osteomyelitis, cellulitis, cerebral abscess, meningitis and cavernous sinus thrombosis.
Periodontal Disease:
Chronic inflammation and degeneration of the supporting tissues of teeth resulting in teeth loss is a common condition.
Besides inflammation, other diseases associated with gingival swelling are leukaemia, scurvy, fibrous hyperplasia and epulis.
Inflammatory periodontal disease affects adults more commonly.
Pregnancy, puberty and the use of drugs like Dilantin are associated with periodontal disease more often.
The disease begins as chronic marginal gingivitis, secondary to bacterial plaques around the teeth such as due to calculus (tartar) on the tooth surface, impacted food, uncontrolled diabetes, tooth decay and ill-fitting dental appliances.
The gingival sulcus acts as a convenient site for the lodgement of food debris and bacterial plaque leading to the formation of a periodontal pocket from which purulent discharge can be expressed by digital pressure.
Microscopically, chronic marginal gingivitis is characterised by heavy chronic inflammatory cell infiltrate, destruction of collagen, and epithelial hyperplasia so as to line the pocket. The periodontal abscess is the localised abscess in the gingival soft tissues.
Untreated chronic marginal gingivitis slowly progresses to chronic periodontitis or pyorrhoea in which there is inflammatory destruction of deeper tissues.
At this stage, progressive resorption of alveolar bone occurs and the tooth ultimately gets detached.
Odontogenic Cysts:
The epithelium-lined cysts of dental tissue and jaw may have an inflammatory or developmental origin. The WHO classification (2017) of odontogenic cysts.
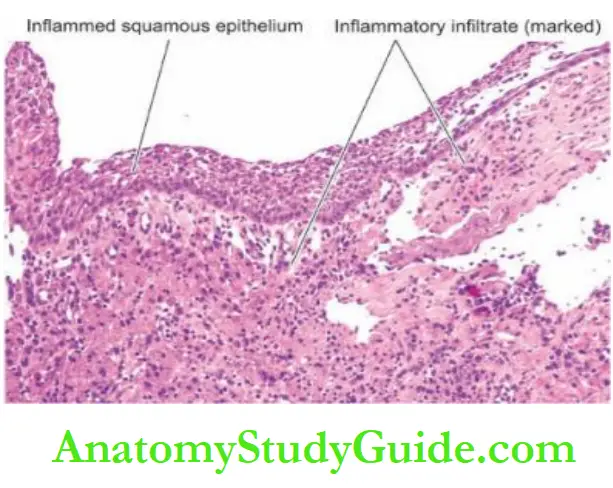
1. Inflammatory Cysts:
Radicular Cyst:
A radicular cyst, also called as apical, periodontal or simply dental cyst, is the most common cyst originating from the dental tissues.
It arises consequent of dental caries. As a result, bacteria gain entry into the pulp inciting inflammation and destruction of dental pulp producing pulpitis and periapical abscess. A periapical abscess is a collection of pus at the root of the tooth.
The epithelial cells of Malassez, which are nests of odontogenic epithelium embedded in the periodontium, proliferate within apical granuloma under the influence of inflammation, leading to the formation of an epithelium-lined cystic cavity.
Most often, the radicular cyst is observed at the apex of an erupted tooth and sometimes contains thick pultaceous material.
1. Inflammatory Odontogenic Cysts
- Radicular (apical, periodontal, dental) cyst
2. Developmental Odontogenic Cysts
1. Odontogenic cysts
- Dentigerous (follicular) cyst
- Eruption cyst
- Gingival cyst
- Primordial cyst (odontogenic keratocyst)
2. Non-odontogenic and fissural cysts
- Nasopalatine duct (Incisive canal, median anterior maxillary) cyst
- Nasolabial (nasoalveolar) cyst
- Globulomaxillary cyst
- Dermoid cyst
Adapted from Naggar et al. WHO classification of head and neck tumours (4th edition) 2017. Chapter 8, 204-260, IARC, Lyon.
Histologically, the radicular cyst is lined by nonkeratinised squamous epithelium.
Epithelial rete processes may penetrate the underlying connective tissues. The radicular cyst of the maxilla may be lined by respiratory epithelium.
The cyst wall is fibrous and contains chronic inflammatory cells (lymphocytes, plasma cells with Russell bodies and macrophages) hyaline bodies and deposits of cholesterol crystals which may be associated with foreign body giant cells.
2. Developmental Cysts:
Odontogenic Cysts Dentigerous (Follicular) Cyst: Dentigerous cyst arises from the enamel of an unerupted tooth.
The mandibular third molars and the maxillary canines are most often involved.
Dentigerous cysts are less common than radicular cysts and occur more commonly in children and young individuals.
These cysts are more significant because of the reported occurrence of ameloblastoma and carcinoma in them.
Histologically, the dentigerous cyst is composed of a thin fibrous tissue wall lined by stratified squamous epithelium.
Thus, the cyst may resemble a radicular cyst, except that chronic inflammatory changes so characteristic of the radicular cyst, are usually absent in dentigerous cysts.
Eruption Cyst:
This is a cyst lying over the crown of an unerupted tooth and is lined by stratified squamous epithelium. It is thus a form of dentigerous cyst.
Gingival Cyst: It arises from the epithelial rests in the gingiva and is lined by keratinising squamous epithelium.
Primordial Cyst (Odontogenic Keratocyst): Primordial cyst, like a dentigerous cyst, also arises from the tooth-forming epithelium. The common location is the mandibular third molar.
Multiple primordial cysts occur in association with naevoid basal cell carcinoma syndrome. Primordial cysts have a marked tendency to recur (50%).
Histologically, the cyst wall is thin and is lined by a regular layer of keratinising stratified squamous epithelium. Inflammatory changes are generally absent. Non-odontogenic and Fissural Cysts
Nasopalatine Duct (Incisive Canal, Median, Anterior Maxillary) Cyst:
This is the most common non-odontogenic (fissural) cyst and arises from the epithelial remnants of the nasopalatine duct.
Histologically, the cyst is lined by stratified squamous epithelium, respiratory epithelium, or both.
Nasolabial (Nasoalveolar) Cyst: This cyst is situated in the soft tissues at the junction of median nasal, lateral nasal and maxillary processes, at the ala of the nose, and sometimes extending into the nostril.
Histologically, the cyst is lined by squamous or respiratory epithelium or both.
Globulomaxillary Cyst: This is an intraosseous cyst and is rare.
Dermoid Cyst: The dermoid cyst is common in the region of the head and neck, especially on the floor of the mouth. The cyst arises from remains in the midline during the closure of mandibular and branchial arches.
Odontogenic Tumours:
Odontogenic tumours are a group of uncommon lesions of the jaw derived from the odontogenic apparatus. These tumours are usually benign but some have malignant counterparts. The WHO classification of odontogenic tumours (2017) is presented Major examples are discussed below.
Benign Odontogenic Tumours:
Ameloblastoma:
Ameloblastoma is the most common benign but locally invasive epithelial odontogenic tumour. It is most frequent in the 3rd to 5th decades of life. Preferential sites are the mandible in the molar-ramus area and the maxilla.
The tumour originates from the dental epithelium of the enamel itself or its epithelial residues.
Sometimes, the tumour may arise from the epithelial lining of a dentigerous cyst or from the basal layer of the oral mucosa.
Radiologically, the typical picture is of multilocular destruction of the bone.
Variants of ameloblastoma are unicystic type, extraosseous (peripheral) type and metastasising type.
Tumours with histologic resemblance to ameloblastoma can occur occasionally in the long bone, like adamantinoma of the tibia.
Grossly, the tumour is greyish-white, usually solid, sometimes cystic, replacing and expanding the affected bone.
Histologically, ameloblastoma can show different patterns as follows:
The follicular pattern is the most common. The tumour consists of follicles of variable size and shape and are separated from each other by fibrous tissue.
The structure of follicles is similar to that of an enamel organ consisting of a central area of stellate cells resembling stellate reticulum, and a peripheral layer of cuboidal or columnar cells resembling epithelium.
The central stellate areas may show cystic changes.
1. Benign Odontogenic Tumours
1. Benign epithelial odontogenic tumours
-
- Ameloblastoma
- Squamous odontogenic tumour
- Calcifying epithelial odontogenic tumour
- Adenomatoid odontogenic tumour
2. Benign mesenchymal tumours
-
- Odontogenic myxoma
- Odontogenic fibroma
- Cementoblastoma
- Cemento-ossifying fibroma
3. Benign mixed epithelial-mesenchymal tumours
- Ameloblastic fibroma
- Primordial odontogenic tumour
- Odontoma
- Dentigerous ghost cell tumour
2. Malignant Odontogenic Tumours
1. Malignant odontogenic tumours
- Odontogenic carcinoma
- Odontogenic carcinosarcoma
- Odontogenic sarcoma
2. Malignant mesenchymal tumours
- Odontogenic sarcoma
3. Malignant mixed epithelial-mesenchymal tumours
- Odontogenic carcinosarcoma
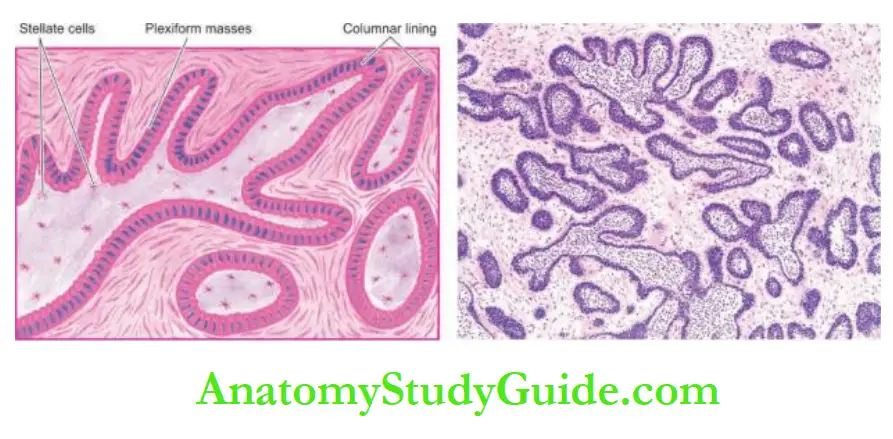
- The plexiform pattern is the next common pattern after the follicular pattern.
- The tumour epithelium is seen to form irregular plexiform masses or a network of strands.
- The stroma is usually scanty. Microcyst formation can occur in the stroma.
- The acanthomatous pattern is squamous metaplasia within the islands of tumour cells.
- The basal cell pattern of ameloblastoma is similar to basal cell carcinoma of the skin.
- The granular cell pattern is characterised by the appearance of acidophilic granularity in the cytoplasm of tumour cells. A combination of more than one morphologic pattern may also be seen. Tumour cells in ameloblastoma exhibit positive immunostaining for cytokeratin and laminin as are seen in developing teeth.
Adenomatoid Odontogenic Tumour (Adeno-ameloblastoma): This is a benign tumour seen more often in females in their 2nd decade of life. The tumour is commonly associated with an unerupted tooth and thus closely resembles a dentigerous cyst radiologically.
Unlike ameloblastoma, the adenomatoid odontogenic tumour is not invasive nor does it recur after enucleation.
Histologically, the lesion has extensive cyst formations. The wall of the cyst contains scanty fibrous connective tissue which are present characteristic tubule-like structures composed of epithelial cells and hence the name ‘adenomatoid’ (gland-like).
Calcifying Epithelial Odontogenic Tumour:
This is a rare lesion which is locally invasive and recurrent like ameloblastoma. It is seen commonly in the 4th and 5th decades and occurs more commonly in the region of the mandible.
Histologically, the tumour consists of closely packed polyhedral epithelial cells having features of nuclear pleomorphism, giant nuclei and rare mitotic.
The stroma is often scanty and appears homogenous and hyalinised in which small calcified deposits are seen which are a striking feature of this tumour.
Odontogenic Myxoma:
Odontogenic myxoma or myxo fibroma is a locally invasive and recurring tumour.
Microscopically, it is characterised by abundant mucoid stroma and loose stellate cells which are seen a few strands of odontogenic epithelium.
Ameloblastic Fibroma:
This is a benign tumour consisting of epithelial and connective tissues derived from odontogenic
apparatus.
It resembles ameloblastoma but can be distinguished from it because ameloblastic fibroma occurs in younger age groups (below 20 years) and the clinical behaviour is always benign.
Histologically, it consists of epithelial follicles similar to those of ameloblastoma, set in a very cellular connective tissue stroma.
Odontomas:
Odontomas are hamartomas that contain both epithelial and mesodermal dental tissue components.
There are 3 subtypes:
Complex odontoma: is always benign and consists of enamel, dentin and cementum which are not differentiated, so that the structure of the actual tooth is not identifiable.
Compound odontoma: is also benign and is comprised of differentiated dental tissue elements forming a number of denticles in fibrous tissue.
Ameloblastic fibro-odontoma is a lesion that resembles ameloblastic fibroma with odontoma formation.
Cementomas:
Cementomas are a variety of benign lesions which are characterised by the presence of cementum or cementum-like tissue.
Five types of cementomas are described:
Benign cementoblastoma (true cementoma) is a solitary lesion of the jaw, characterised by features comparable to those of osteoid osteoma and osteoblastoma.
Cementifying fibroma consists of cellular fibrous tissue containing calcified masses of cementum-like tissue.
Periapical cemental dysplasia (Periapical fibrous dysplasia) is the most common and resembles cementifying fibroma except that it contains more fibrous tissue as well as cementumlike tissue.
Multiple apical cementomas are found on the apical region of teeth and detected incidentally in postmenopausal women.
Gigantiform cementoma is a large lobulated mass of cementum-like tissue. Sometimes, there are multiple such masses in the jaw.
Malignant Odontogenic Tumours:
Odontogenic Carcinoma:
Odontogenic carcinoma is a rare malignant tumour having varied histologic entities: Ameloblastic carcinoma is a malignant counterpart of ameloblastoma having cytologic features of malignancy in the
primary tumour: cytologic atypia, high N: ratio, increased mitoses and areas of necrosis.
Primary intraosseous carcinoma, NOS, may develop within the jaw from the rest of the odontogenic epithelium.
Sclerosing odontogenic carcinoma is characterised by strands and islands of epithelium invading the dense fibrosclerotic stroma.
Clear cell odontogenic carcinoma is distinct due to the clear cell morphology of nests and islands of tumour cells and EWSR1-ATF1 translocation.
Ghost cell odontogenic carcinoma is rare and malignancy arises from calcifying odontogenic cysts with features of calcifying odontogenic tumour or dentigerous ghost cell tumour.
Odontogenic Sarcoma:
Odontogenic sarcoma is rare and has the appearance of ameloblastic fibrosarcoma.
his tumour resembles ameloblastic fibroma but the mesodermal component in it is malignant (sarcomatous) whereas the ameloblastic epithelium remains differentiated and benign.
Odontogenic Carcinosarcoma:
It is rare and consists of a combined growth pattern of malignant connective tissue elements and malignant ameloblastic epithelial areas.
Diseases of Teeth and Periodontal Tissues:
- The normal tooth is composed of enamel, dentin, cementum, and central pulp.
- In dental caries, there is the destruction of enamel and the occurrence of pulpitis.
- Chronic periodontal inflammation causes periodontitis and pyorrhoea.
- A common inflammatory cyst of the jaw is a radicular cyst while a common developmental cyst is a dentigerous cyst.
- Benign odontogenic tumours of the jaw originate from epithelium (e.g. ameloblastoma) or mesenchyme (e.g. myxoma).
- Odontogenic carcinoma and sarcoma are uncommon malignant tumours.
Salivary Glands
Normal Structure:
There are two main groups of salivary glands major and minor. The major salivary glands are the three paired glands: parotid, submandibular and sublingual.
The minor salivary glands are numerous and are widely distributed in the mucosa of the oral cavity.
The main duct of the parotid gland drains into the oral cavity opposite the second maxillary molar, while the ducts of submandibular and sublingual glands empty in the floor of the mouth.
At times, heterotopic salivary gland tissue may be present in lymph nodes near or within the parotid gland.
Histologically, the salivary glands are tubuloalveolar glands and may contain mucous cells, serous cells, or both.
The parotid gland is purely serous. The submandibular gland is a mixed type but is predominantly serous, whereas the sublingual gland, though also a mixed gland, is predominantly mucous type.
Similarly, minor salivary glands may also be serous, mucous or mixed type.
The secretory acini of the major salivary glands are drained by ducts lined by:
Low cuboidal epithelium in the intercalated portion, tall columnar epithelium in the intralobular ducts, and simpler epithelium in the secretory ducts.
The product of major salivary glands is saliva which performs various functions such as lubrication for swallowing and speech and has enzyme amylase and antibacterial properties too.
Major pathologic conditions of salivary glands, inflammation and neoplasms, are discussed here.
Inflammatory And Salivary Flow Diseases:
Sialorrhoea (Ptyalism):
The increased flow of saliva is termed sialorrhoea or ptyalism. It occurs commonly due to:
stomatitis, teething, mentally retarded state, schizophrenia, neurological disturbances, increased gastric secretion and sialosis (i.e. uniform, symmetric, painless hypertrophy of salivary glands).
Xerostomia:
Decreased salivary flow is termed xerostomia. It is associated with the following conditions:
Sjogren’s syndrome, sarcoidosis, mumps parotitis, Mikulicz’s syndrome, megaloblastic anaemia, dehydration, and drug intake (e.g. antihistamines, antihypertensives, antidepressants).
Sialadenitis:
Inflammation of salivary glands, sialadenitis, may be acute or chronic; the latter being more common.
Etiology: Sialadenitis can occur due to the following causes:
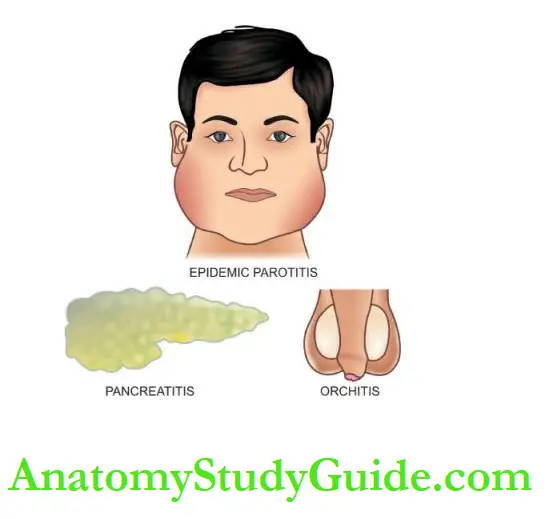
1. Viral infections: The most common inflammatory lesion of the salivary glands particularly of the parotid glands, is mumps occurring in children of school age.
It is characterised by a triad of pathological involvement—epidemic parotitis (mumps), orchitis-oophoritis, and pancreatitis.
Involvement of the testis and pancreas may lead to their atrophy.
Less commonly, cytomegalovirus infection may occur in the parotid glands of infants and young children.
2. Bacterial and mycotic infections: Bacterial infections may cause acute sialadenitis more often.
Sometimes there are recurrent attacks of acute parotitis when parotitis becomes chronic.
Acute sialadenitis These conditions are as follows:
- Acute infectious fevers
- Acute postoperative parotitis (ascent of microorganisms up the parotid duct from the mouth)
- General debility
- Old age
- Dehydration.
2. Chronic sialadenitis:
This may result from the following conditions:
- Recurrent obstructive type Recurrent obstruction due to calculi (sialolithiasis), stricture, surgery, injury etc. may cause repeated attacks of acute sialadenitis by ascending infection and then chronicity.
- Recurrent non-obstructive type Recurrent mild ascending infection of the parotid gland may occur due to non-obstructive causes which reduce salivary secretion due to intake of drugs causing hyposalivation (e.g. antihistamines, antihypertensives, antidepressants), the effect of irradiation and congenital malformations of the duct system.
- Chronic inflammatory diseases Tuberculosis, actinomycosis and other mycoses may rarely occur in the salivary glands.
3. Autoimmune disease Inflammatory changes are seen in salivary glands in 2 autoimmune diseases:
- Sjogren’s syndrome is characterised by a triad of dry eyes (keratoconjunctivitis sicca), dry mouth (xerostomia) and rheumatoid arthritis.
- Mikulicz’s syndrome is the combination of inflammatory enlargement of salivary and lacrimal glands with xerostomia.
Morphologic Features:
Irrespective of the underlying aetiology of sialadenitis, there is swelling of the affected salivary gland, usually restricted by the fibrous capsule.
The acute stage is generally associated with local redness, pain and tenderness with purulent ductal discharge.
Late chronic cases may be replaced by firm fibrous swelling.
Microscopically, acute viral sialadenitis in mumps shows swelling and cytoplasmic vacuolation of the acinar epithelial cells and degenerative changes in the ductal epithelium.
There is interstitial oedema, fibrinoid degeneration of the collagen and dense infiltration by mononuclear cells (lymphocytes, plasma cells and macrophages).
Chronic and recurrent sialadenitis is characterised by increased lymphoid tissue in the interstitium, progressive loss of secretory tissue and replacement by fibrosis.
Tumours Of Salivary Glands:
The major, as well as minor salivary glands, can give rise to a variety of benign and malignant tumours.
The major glands, particularly the parotid glands (85%), are the most common sites.
The majority of parotid gland tumours (65-85%) are benign, while in the other major and minor salivary glands 35-50% of the tumours are malignant.
Most of the salivary gland tumours originate from the ductal lining epithelium and the underlying myoepithelial cells; a few arise from acini.
Recurrent tumours of the parotid glands, due to their location, are often associated with facial palsy and obvious scarring following surgical treatment.
The current WHO classification of salivary gland tumours (2017) is summarised.
This classification has several newer entities and includes key molecular alterations in these tumours. Major examples are discussed below.
1. Benign Epithelial Tumours
- Pleomorphic adenoma (50%)
- Warthin’s tumour (8%)
- Oncocytoma (1%)
- Others (myoepithelioma, basal cell adenoma, sebaceous adenoma)
2. Borderline Epithelial Tumours
- Sialoblastoma
3. Malignant Epithelial Tumours
- Mucoepidermoid carcinoma (15%)
- Adenocarcinoma (polymorphous, basal cell, and NOS) (10%)
- Carcinoma ex pleomorphic adenoma (5%)
- Adenoid cystic carcinoma (5%)
- Acinic cell carcinoma (3%)
- Squamous cell carcinoma (1%)
- Others (secretory carcinoma, intraductal carcinoma, salivary duct carcinoma, epithelial-myoepithelial carcinoma, clear cell carcinoma, carcinosarcoma)
4. Mesenchymal Tumours
- Haemangioma
- Lipoma
5. Haematolymphoid Tumours
- Extranodal marginal zone MALT lymphoma
1. Benign Epithelial Tumours:
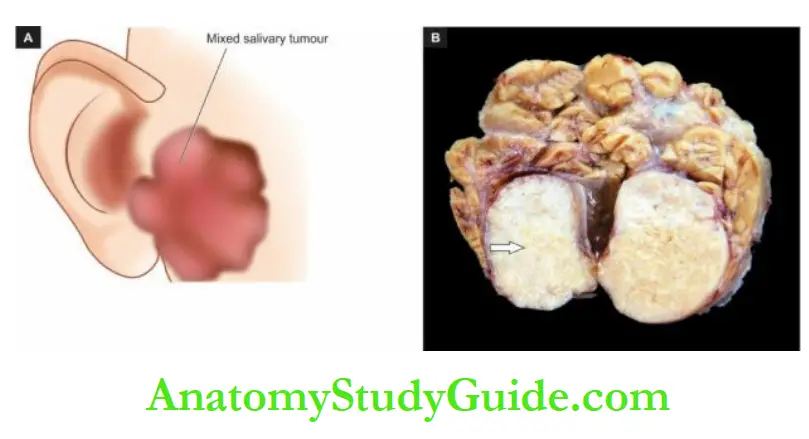
Pleomorphic Adenoma (Mixed Salivary Tumour):
This is the most common tumour of major (60-75%) and minor (50%) salivary glands.
Pleomorphic adenoma is the commonest tumour in the parotid gland and occurs less often in other major and minor salivary glands.
The tumour is commoner in women and is seen more frequently in 3rd to 5th decades of life. The tumour is solitary, smooth-surfaced, sometimes nodular, painless and slow-growing.
It is often located below and in front of the ear.
In >50% of cases of pleomorphic adenoma, 8q12 translocation as a fusion gene has been identified which is quite diagnostic.
Morphologic Features: Grossly, pleomorphic adenoma is a circumscribed, pseudoencapsulated, rounded, at times multilobulated, firm mass, 2-5 cm in diameter, with a bosselated surface.
The cut surface is grey-white and bluish, variegated, semitranslucent, usually solid but occasionally may show small cystic spaces. The consistency is soft and mucoid.
Microscopically, pleomorphic adenoma is characterised by a pleomorphic or ‘mixed’ appearance in which there are epithelial elements present in a stromal matrix of mucoid, myxoid and chondroid tissue:
Epithelial component: may form various patterns like ducts, acini, tubules, sheets and strands of cells of ductal or myoepithelial origin.
The ductal cells are cuboidal or columnar, while the underlying myoepithelial cells may be polygonal or spindle-shaped resembling smooth muscle cells.
The material found in the lumina of duct-like structures is PAS-positive epithelial mucin.
Focal areas of squamous metaplasia and keratinisation may be present.
Immunohistochemically, the tumour cells are immunoreactive for epithelial (cytokeratin, EMA, CEA) as well as myoepithelial (actin, vimentin and S-100) antibodies.
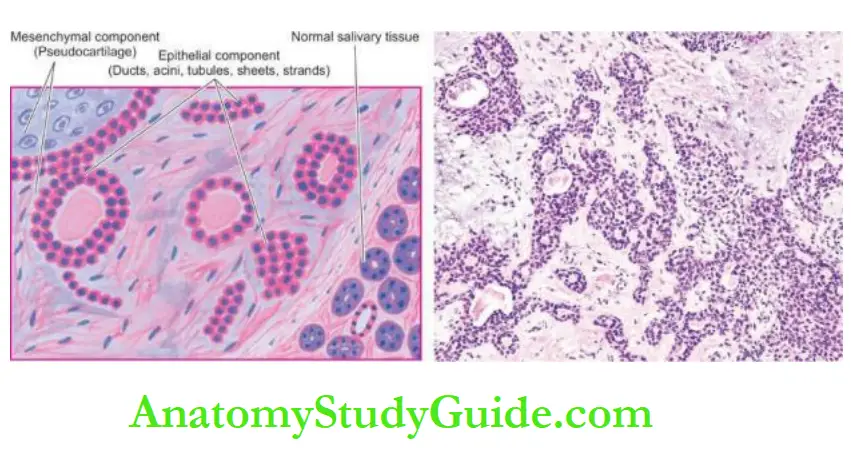
Stromal elements are present as loose connective tissue, and as a myxoid, mucoid and chondroid matrix, which simulates cartilage (pseudocartilage).
However, true cartilage and even bone may also be observed in a small proportion of these tumours.
Based on morphology, immunohistochemistry, ultrastructure and molecular characteristics, the mesenchymal matrix of the tumour has been assigned as a product of epithelial origin and is actually modified myoepithelial cells as seen by S-100 immunostain positivity.
The epithelial and mesenchymal elements are intermixed and either of the two components may be dominant in any tumour.
Prognosis:
Pleomorphic adenoma is notorious for recurrences, sometimes after many years.
The main factors responsible for the tendency to recur are incomplete surgical removal due to proximity to the facial nerve, multiple foci of the tumour, pseudo encapsulation, and implantation in the surgical field.
Although the tumour is entirely benign, an ordinary pleomorphic adenoma may sometimes be more aggressive and metastasise to distant sites which too has a benign appearance as the original tumour (metastasising pleomorphic adenoma).
However, actual malignant transformation can also occur in a pleomorphic adenoma as discussed below.
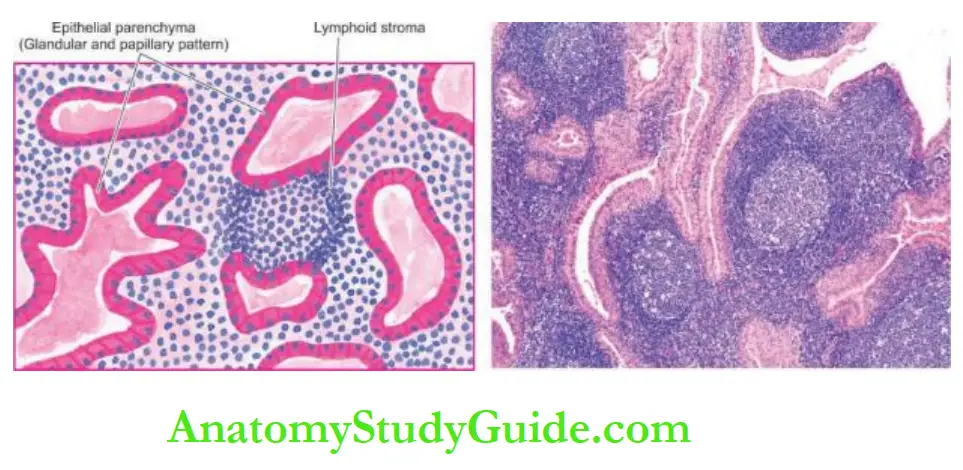
Warthin’s Tumour:
Warthin’s tumour, also given a more descriptive name of papillary cystadenoma lymphomatous, is a benign tumour of the parotid gland comprising about 8% of all parotid neoplasms, seen more commonly in men from the 4th to 7th decades of life.
Rarely, it may arise in the submandibular gland or in minor salivary glands.
The Histogenesis of the tumour has been much debated; the most accepted theory is that the tumour develops from parotid ductal epithelium present in lymph nodes adjacent to or within the parotid gland.
Morphologic Features: Grossly, the tumour is encapsulated, round or oval with a smooth surface. The cut surface shows characteristic slit-like or cystic spaces, containing milky fluid and having papillary projections.
Microscopically, the tumour shows 2 components: epithelial parenchyma and lymphoid stroma:
Epithelial parenchyma: is composed of glandular and cystic structures having papillary arrangement and is lined by characteristic eosinophilic epithelium. Variants of epithelial patterns include the presence of mucous goblet cells and sebaceous differentiation.
Lymphoid stroma: is present under the epithelium in the form of prominent lymphoid tissue, often with germinal centres.
Oncocytoma:
Oncocytoma or oxyphil adenoma is a benign slow-growing tumour of the major salivary glands.
The tumour consists of parallel sheets, acini or tubules of large cells with glandular eosinophilic cytoplasm (oncocytes).
It is also called mitochondria because of cytoplasmic granularity due to mitochondria.
Other Benign Epithelial Tumours:
- Myoepithelioma is an adenoma composed exclusively of myoepithelial cells which may be arranged in a tubular, alveolar or trabecular pattern. The tumour cells are plasmacytoid, spindled or clear.
- Basal cell adenoma is characterised by the type and arrangement of cells resembling basal cell carcinoma of the skin.
- Sebaceous adenoma has nests of benign squamous cells with sebaceous differentiation lining a cyst. The background contains prominent lymphoid infiltrate; that is why it is also called lymphadenoma.
Malignant Epithelial Tumours:
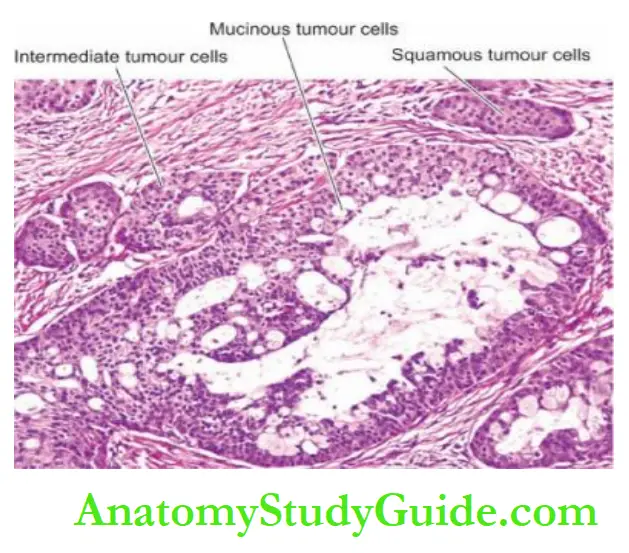
Mucoepidermoid Carcinoma:
Mucoepidermoid carcinoma is the most common malignant salivary gland tumour (in both major and minor salivary glands) (15%) having the following peculiar features:
The parotid gland among the major salivary glands (two-third of cases) and the minor salivary
glands in the palate are the most common sites.
It has a wide age range (15-86 years) i.e. occurs at both extremes of age: mean age is 5th decade in adults and is the most common malignant salivary gland tumour affecting children and adolescents.
It is the most common example of radiation-induced malignant tumours, especially therapeutic radiation.
Common genetic rearrangements (40-80% cases) described in mucoepidermoid carcinoma are t(11;19)((q21;13).
Morphologic Features:
Grossly, the tumour is usually circumscribed but not encapsulated. It varies in size from 1 to 4 cm.
Microscopically, the tumour is classified into low, intermediate and high grades depending on the degree of differentiation and tumour invasiveness.
The tumour is composed of a combination of 4 types of cells: mucin-producing, squamous, intermediate and clear cells.
Well-differentiated tumours have a predominance of mucinous cells, while poorly differentiated have a more solid and infiltrative pattern.
Prognosis varies according to the grade of the tumour: high-grade tumours have a 25% recurrent rate, while low-grade tumour has a 15% rate of recurrence.
Adenocarcinoma:
Adenocarcinoma of the salivary gland is the next most frequent malignant salivary gland tumour (10%). The common age of occurrence is 5th to 6th decades although it can also occur in children.
The diagnosis is made after excluding metastatic deposits in the salivary gland from another primary tumour.
Morphologic Features:
A few variants of adenocarcinoma of the salivary gland have been described:
Polymorphous adenocarcinoma is Previously known as polymorphous low-grade adenocarcinoma, it is a more frequent tumour in minor salivary glands, the palate being the most common site.
Morphologically, it shows a cribriform pattern of adenocarcinoma having mild anaplasia.
Basal cell adenocarcinoma It is a low-grade malignant counterpart of basal cell adenoma and may actually arise in basal cell adenoma. It is a locally destructive tumour.
Adenocarcinoma, not otherwise specified is a tumour of adults having infiltrative borders.
The tumour consists of typical glandular spaces and cyst formation but lacks specific features.
Carcinoma Ex-Pleomorphic Adenoma:
Carcinoma ex-pleomorphic adenoma is not an uncommon malignant salivary gland tumour (5%).
The slow-growing adenoma may have been present for a number of years when suddenly it undergoes a rapid increase in its size, becomes painful and the individual may develop facial palsy.
Malignant transformation occurs at a later age (6th decade) than the usual age for pleomorphic adenoma (4th to 6th decades). It may occur in primary tumours but more often occurs in its recurrences.
Common genetic alteration in this tumour is the same as in pleomorphic adenoma (i.e. 8q;12 translocations) involving fusion genes.
Morphologic Features:
Grossly, the tumour is poorly circumscribed with an irregular infiltrating margin. The cut section may show haemorrhages, necrosis and cystic degeneration.
Microscopically, besides the typical appearance of pleomorphic adenoma, malignant areas show cytologic features of carcinoma such as anaplasia, nuclear hyperchromatism, large nuclearisation, mitoses and evidence of invasive growth.
All types of usual salivary gland carcinomas may develop in pleomorphic adenoma.
Prognosis depends upon several variables: an adequate sampling of the tumour, the extent of invasion beyond the capsule, histologic grade and type carcinoma, pathologic stage, tumour size and proliferation index.
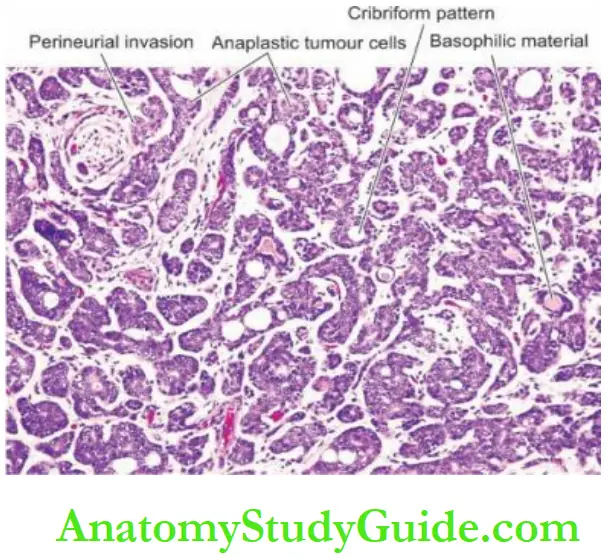
Adenoid Cystic Carcinoma:
Adenoid cystic carcinoma, also called cylindroma, comprises 5% of all malignant salivary tumours.
The common age of occurrence is 50-60 years and may occur in both major and minor salivary glands. It is a slow-growing but aggressive tumour.
Histologically, adenoid cystic carcinoma is characterised by cribriform appearance i.e.
the epithelial tumour cells of duct-lining and myoepithelial cells are arranged in duct-like structures or masses of cells, having typical fenestrations or cyst-like spaces and hence the name ‘adenoid cystic’.
These cystic spaces contain PAS-positive basophilic material.
Typically, adenoid cystic carcinoma has infiltrative nature and tends to spread along the nerve sheaths.
Acinic Cell Carcinoma:
Acinic cell carcinoma comprises 3% of all malignant salivary gland tumours.
Acini cell carcinoma is the second most frequent childhood salivary gland malignancy after mucoepidermoid carcinoma.
It is seen in both major and minor salivary glands as an encapsulated tumour.
Histologically, it is composed of acinic cells resembling serous cells of normal salivary glands.
These cells are arranged in solid sheets, acini or ductal patterns and have characteristic basophilic granular cytoplasm.
The degree of atypia may vary from a benign cytologic appearance to cellular features of malignancy.
80-90% of tumours recur after excision but the tumour is relatively less aggressive in minor salivary glands.
Squamous cell Carcinoma:
This rare tumour has features of squamous cell carcinoma with keratin formation and has intercellular bridges similar to its appearance elsewhere in the body.
The tumour commonly infiltrates the skin and involves the facial nerve early.
Other Malignant Tumours:
Some rare malignant epithelial tumours are secretory carcinoma, intraductal carcinoma, salivary duct carcinoma, epithelial-myoepithelial carcinoma, clear cell carcinoma and carcinosarcoma.
Besides, marginal zone lymphoma of MALT type and sarcomas are uncommon tumours in salivary glands.
All these tumours are similar in morphology to such tumours elsewhere in the body.
Besides, metastatic involvement of major salivary glands or the adjacent lymph nodes is common, especially from epidermoid carcinoma and malignant melanoma.
Diseases of Salivary Glands:
- Salivary flow disturbances include sialorrhoea (hypersalivation) and xerostomia(decreased salivation).
- Sialadenitis is inflammation of the parotid glands, commonly due to mumps in children, and may be accompanied by orchitis-oophoritis and pancreatitis.
- The most common benign tumour of the salivary glands is pleomorphic adenoma. It is composed of epithelial and stromal elements.
- Warthin’s tumour is a monomorphic adenoma and has cystic spaces lined by papillary arrangement lined by epithelial cells with eosinophilic cytoplasm and lymphoid stroma.
- Mucoepidermoid carcinoma is the most common malignant salivary tumour in both adults and children (15%).
- Adenocarcinoma (10%) has a few variants such as polymorphous type, basal cell type, and not-otherwise specified type.
- Carcinoma ex pleomorphic adenoma occurs in about 5% of mixed salivary tumours and shows malignant change.
- Acinic cell carcinoma is the second most common childhood malignant salivary tumour after mucoepidermoid carcinoma. Adenoid cystic carcinoma occurs in adults and is an aggressive tumour.
Leave a Reply