Antifungal Agents Introduction
A fungus is a colorless plant lacking chlorophyll. Fungi that cause disease in humans may be like yeast or hyphae (mould) and are called mycotic infections or fungal infections. The demand for antifungal drug was small since most humans with normally functioning immune system are able to ward off the invading fungi. Recently, research on newer antifungal has increased due to onset of AIDS epidemic, cancer chemotherapy and organ transplantation which increased the incidence of life threatening fungal infections.
Table of Contents
Fungal infections may be any one of the two types
- Superficial mycotic infection.
- Systemic mycotic infection.
Superficial mycotic infections are those occurring on the surface or just below the skin or nail. Systemic mycotic infections are those occurring inside the body, such as in lungs and other body organs.
Fungal infections are common, not only as primary disease but also secondary to therapy with oral antibiotics. Individuals suffering from malignancy, diabetes mellitus, those on corticosteroids and immune compromised subjects are more prone to develop fungal infections.
Candida albicans is normally found as part of flora of the gastrointestinal tract and vagina and it causes diseases like ring worm and athlete’s food. Trichophyton rubrum is also a causative agent form ring worm. Dermatophytes are fungi causing infections on skin, hair and nails.

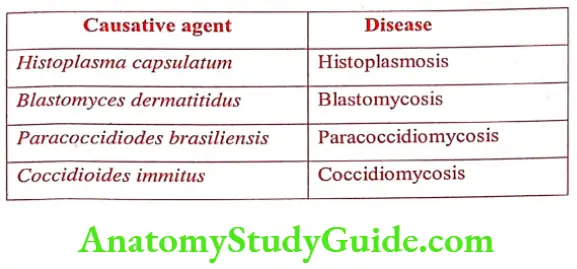
Dermatophytic infections known as tinea are caused by Trichophyton, Microsporum and Epidermophyton. Thermally dimorphic fungi are saprophytes which grow in one form at room temperature and in different form in host at 37° C. Some of the most common infectious disease and causative agents (thermally dimorphic fungi) are:
Aspergillus spores are present everywhere, inhalation is the most common route of inoculation, but infection through wounds, burns and implanted device such as catheters is also possible. Aspergillus is a major source of infection in persons with leukemia, receiving organ transplants and bone marrow transplants.
Fungal Cell Structure and Targets
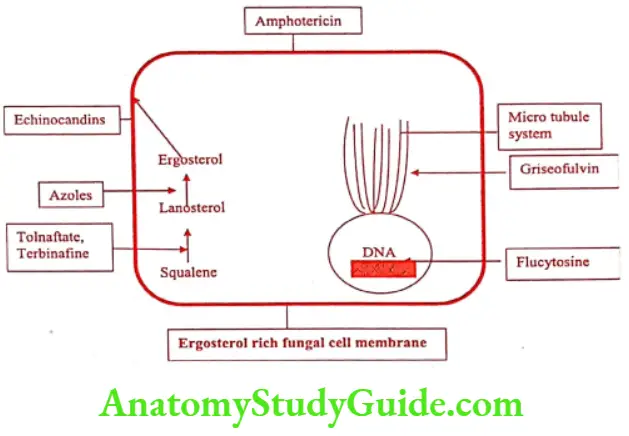
- Antifungal chemotherapy depends on biochemical difference between fungi and mammals. Like mammalian cells, fungi are eukaryotes with many similar biochemical structures, especially cell membranes to mammalian cells. At the cellular level, the greatest difference between fungal cells and mammalian cells is that fungal cells have cell walls but the mammalian cells do not. The fungal cell inhibition is a target for some antifungal agents. Other targets for antifungal include inhibition of DNA biosynthesis, disruption of mitotic spindles and general interference with intermediary metabolism.
- The mammalian cell contains cholesterol as sterol component whereas fungi contain ergosterol which is important for proper functioning of many cell membrane enzymes and ion transport proteins. This difference in the sterol is the basis for the most of the currently available antifungal drug i.e., inhibits ergosterol biosynthesis.
- DNA is organized into chromosomes within the cell nucleus and has distinct cytoplasmic organelles organelles including endoplasmic reticulum, golgi apparatus, mitochondria and storage vacuoles.
- This homology to mammalian cells also extends to biosynthetic pathways, where fungi share similar mechanisms for DNA replication and protein synthesis.
- The similarity of fungal and mammalian cells creates designing drugs that are selectively toxic to fungal cells but not the human host.
Antifungal Agents Classification
- Antifungal agents are classified according to chemical structure as:
- Fatty acids and carboxylic acid: eg. Sodium caprylate, Triacetin, Undecylenic acid, Benzoic acid, Salicylic acid, Propionic acid.
- Phenols and their derivatives : eg. Resorcinol, Haloprogin, Clioquinol, Ciclopirox.
- Nucleoside antifungal agent: eg. Flucytosine.
- Antifungal antibiotics:
- Polyenes : eg. Amphotericin B, Nystatin, Natamycin.
- Other antifungal antibiotic: eg. Griseofulvin.
- Allylamine and related compounds: eg. Naftifine, Tolnaftate, Terbinafine.
- Azole antifungal agents: eg. Clotrimazole, Econazole, Butoconazole, Miconazole, Ketoconazole, Fluconazole, Sulconazole, Oxiconazole, Tioconazole, Terconazole, Itraconazole.
- Newer antifungal agents: eg. Echinocandins, Caspofungin, Anidulafungin, Micafungin.
- According to the mechanism of action antifungal agents are classified as:
- Inhibition of cell wall synthesis : eg. Polyoxins, Nikkomycin Z, Echinocandins.
- Inhibition of ergosterol biosynthesis : eg. Polyenes azoles, Amorolfine, Allyamines, Thiocarbamates, Butenafine.
- Inhibition of protein synthesis: eg. Sordarins.
- Inhibition of RNA/DNA synthesis : eg. Griseofulvin, Flucytosine.
Fatty Acids
An acidic substance in and on the skin called as sebum which is a natural antifungal agent. Substances similar to sebum like fatty acid act as fungicidal agent. Dermatophytosis is called tinea or ring worm. Since these infections tend to be topical, their treatment has been directed to surface area of the skin. Mainly fatty acid derivatives are used as dermatophytosis.
Phenols and Their Derivatives
Phenols interfere with cell membrane integrity and function in susceptible fungi.
Clioquinol (Vioform, Dermoquinol)
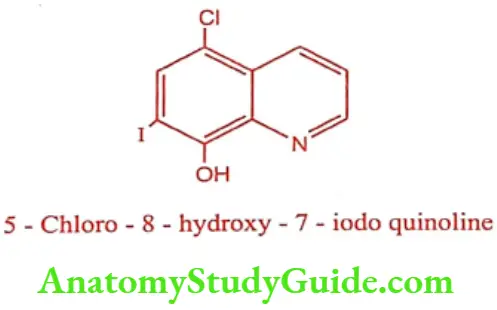
ADR: Severe irritation or hypersensitivity.
Dose: Topically as 3% cream/ointment; Apply 2 to 4 times /day. Duration: Athlete’s foot: 4 weeks and Jock itch: 2 weeks.
Use: It is used in the form of powder for many skin infections such as atopic dermatitis, eczema, psoriasis and impetigo. It is used vaginally for the treatment of Trichomonas vaginitis. It is best in the topical treatment of fungal infection such as athlete’s foot and jock itch.
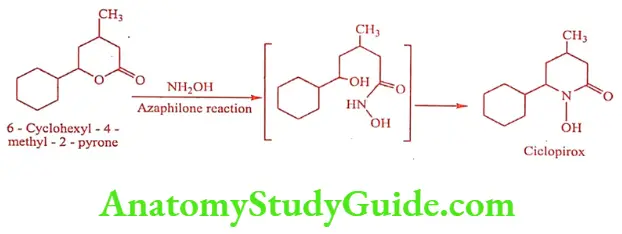
Ciclopirox (Olamin, Onylac)
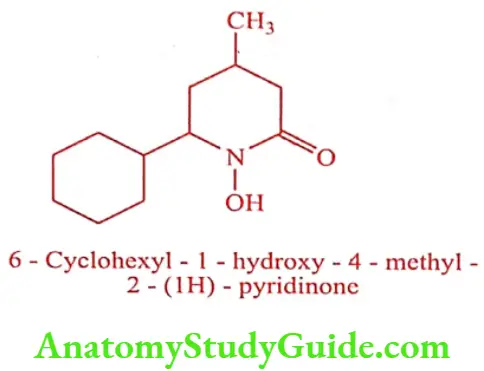
Ciclopirox is a hydroxylated pyridinone and active against dermatophytes and pathogenic yeast (Candida albicans) that are causative agents for superficial fungal infections. It acts on the cell membranes of susceptible fungi and block the transport of amino acids into the cells. It chelates with polyvalent cation such as Fe3+ which causes inhibition of number of metal dependent enzymes within the fungal cells.
Synthesis
ADR: Pruritus and burning sensation.
Dose: Topical seborrheic dermatitis as 1% shampoo; apply twice weekly. Nail fungal infections as 8% lacquer; apply once daily. Skin fungal infections as infections as 0.77% cream/gel/suspension/solution/powder; apply twice daily.
Use: It is used in the treatment of cutaneous candidiasis, Tinea corporis, Tinea cruris, Tinea pedis and Tinea versicolor. It is a second line agent for the treatment of onychomycosis (ring worm of the nails).
Haloprogin (Halotex)
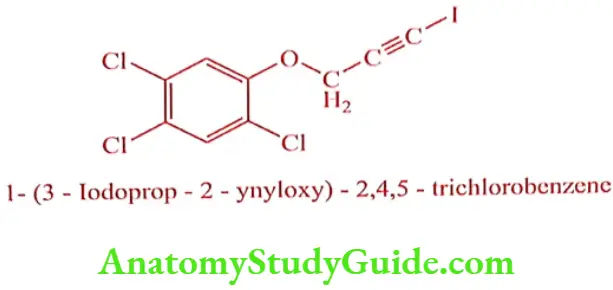
Haloprogin is iodinated acetylene active against dermatophytes. It interferes with DNA biosynthesis and leads to non specific metabolic disruption.
ADR: Unusual blistering, itching, redness, peeling, dryness or irritation of the skin.
Dose: Apply liberally twice daily for 2 to 3 weeks. Available as 1% cream (15g or 30g).
Use: It is used to treat skin infections such as athlete’s foot, jock itch, ringworm and Tinea versicolor.
Nucleoside Antifungals
Flucytosine (Ancobon)
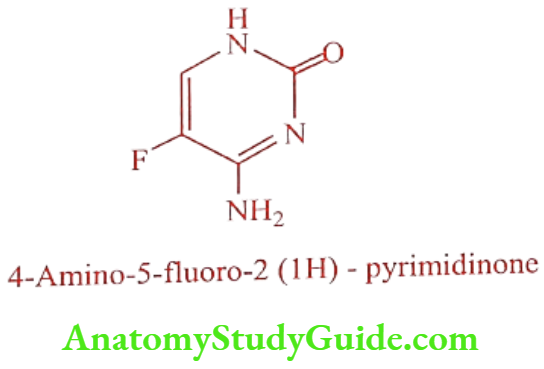
Flucytosine is a prodrug, fluorinated pyrimidine related to Fluorouracil and Floxuridine.
Synthesis
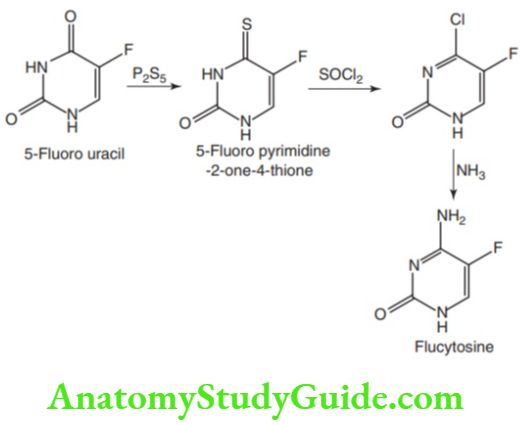
Mechanism of Action: Flucytosine is only available antimetabolite drug having antifungal activity. It inhibits fungal protein synthesis by replacing the uracil with 5- Flurouracil in fungal RNA and also inhibits thymidine synthetase by interfering with fungal DNA synthesis.

5-Flucytosine is transported by cytosine permease into the fungal cell, where it is deaminated to 5-Fluoro uracil (5FU) by cytosine deaminase. Then 5-FU is converted to 5-Fluorouracil- ribose monophosphate (5-FUMP) and then is either converted into 5-Fluorouridine triphosphate (5-FUTP) and incorporated into RNA or converted into 5-Fluoro-2-deoxyuridine-5′-monophosphate by ribonucleotide reductase, which is a potent inhibitor of thymidylate synthase results in the inhibition of DNA synthesis. Flucytosine is selectively toxic to fungi as mammalian cells lack cytosine deaminase.
ADR: Bone marrow depression.
Dose: 50 to 150mg/kg/day administered in divided doses at 6 hrs interval.
Use: It is used for the treatment of systemic infections caused by susceptible strains of Candida and Cryptococcus and clinically used in combination with Amphotericin B.
Antifungal Antibiotics
Polyenes
These complex antifungal antibiotics are isolated from soil bacteria of the genus Streptomyces. Polyenes are divided into two groups
- 26-membered ring polyene, eg. Natamycin.
- 38-membered ring polyenes. eg. Amphotericin, Nystatin.
Polyenes are macrocylic lactones with distinct hydrophilic and lipophilic region. The lipophilic region contains conjugated double bonds, in macrocyclic lactone ring. Hence they are called as polyene antibiotics. The hydrophilic region contains a hydroxy group on the acid derived portion of the ring.
- a glycosidically linked deoxy amino hexose called mycosamine.
Mechanism of Action: They bind to fungal membrane, act as a false membrane component, bind closely to ergosterol and produce a change in cell permeability. This .leaks out the cytoplasmic content and causes cell lysis.
Amphotericin B (Amfotex, Mycol)
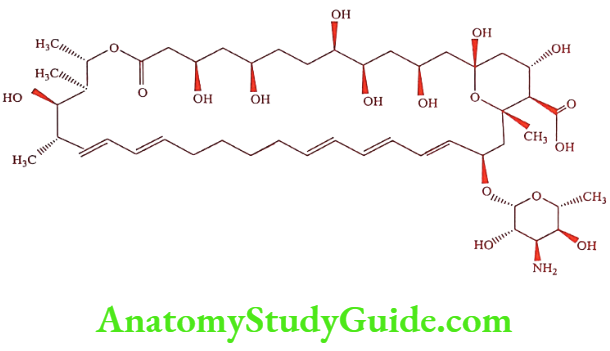
Amphotericin B was isolated from Streptomyces nodosus. It interacts with ergosterol in fungi and forms a trans membrane channel. Intermolecular hydrogen bond formed among the OH, COOH and -NH2 group in moiety stabilize the channel in its open form, destroy activity and allowing the cytoplasmic content to leak out. The low water solubility of Amphotericin B has led to the following formulations:
- Colloidal suspensions which used deoxycholate as a solubilizing agent, Amphotericin B deoxycholate (Fungizone).
- Amphotericin B colloidal dispersion (ABCD; Amphocil, Amphotec)
- Amphotericin lipid complex (ABLC; Abeleet)
- Liposomal amphotericin B (L- AMB; Ambisome)
ADR: Fever, shaking chills, hypokalemia, hypotension and kidney toxicity.
Dose: 100 to 200mg tablet/suspension 4 times daily.
Use: Amphotericin B is the only polyene used in systemic infection. Topically it is used to treat mycoses caused by Candida albicans. The drug cannot cross the blood brain barrier and must be administered intrathecally for treatment of fungal infections of central nervous system.
Nystatin (Mycostatin TM)
Nystatin is an effective topical antifungal agent. Nystatin is isolated from the strain of the actinomycete called Streptomyces noursei.
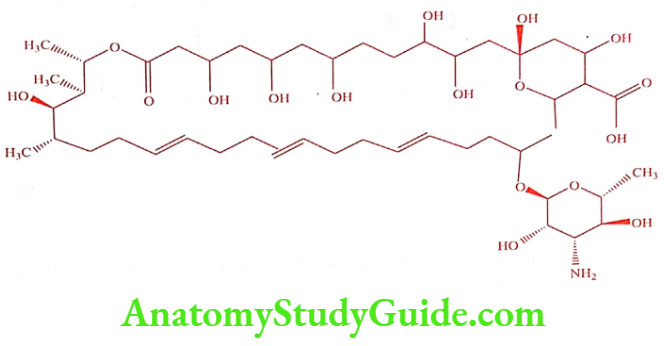
Nystatin is a mixture of four different tetraenes, Nystatin A, A2, A3 and polyfungin B. The aglycone portion of Nystatin called nystatinolide consists of a 38-membered macrolide lactone ring containing single tetracene and diene moieties separated by two methylene groups. The aglycone contains eight hydroxyl groups, one carboxyl group and lactone ester functional group. This entire aglycone is linked to the glycone mycosamine.
ADR: Nephrotoxicity (decreased by change in formulation).
Dose: 1 to 4mg/kg/day.
Use: Nystatin is a valuable agent for the treatment of local and gastro intestinal infection caused by Candida albicans and other Candida species. Nystatin is too toxic to be used systematically, but due to its poor absorption used to treat mouth and GIT infections, fever, myalgia, hypotension and bronchospasm.
Natamycin (Pimafusin)
It is also known as Pimaricin, is a polyene natural antibiotic obtained from the cultures of Streptomyces natalensis.
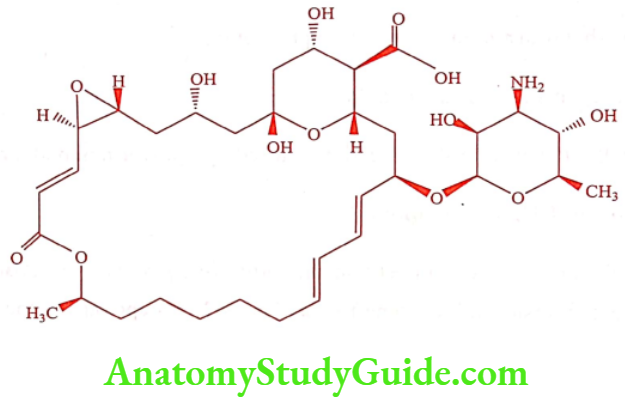
The Natamycin structure consist of 26-membered lactone ring containing a tetraene chromophore, an a, ẞ-unsaturated lactone carbonyl group, three hydroxyl groups, a carboxyl group, a trans epoxide and a glycosidically linked mycosamine.
ADR: Muscles spasms, vomiting, dyspnoea, head ache and hypotension.
Dose: 100mg 4 times daily.
Use: Natamycin is active against yeast and fungi, including Candida, Aspergillus, Cephalosporium, Penicillium and Fusarium spp. It is used for fungal conjunctivitis, blepharitis and keratitis.
Other Antifungal Antibiotics
Griseofulvin (Gris OD, Fluvin)
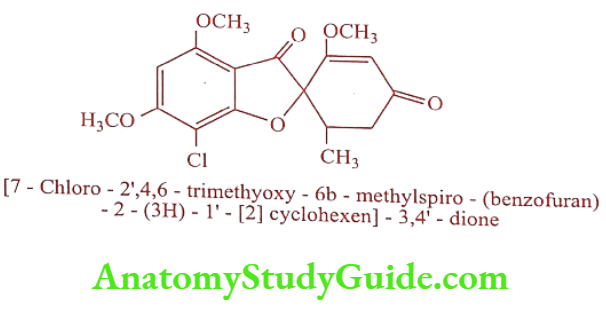
Griseofulvin is an example of spiro compound. It is isolated from the fungus Penicillium griseofulvum.
Mechanism of Action: Griseofulvin inhibits fungal mitosis by disrupting the mitotic spindle through interaction with polymerized microtubules. By interfering with tubulin polymerization, Griseofulvin stops mitosis at metaphase. The destruction of cytoplasmic microtubules. interferes with the transport of secretory material, which inhibits cell wall synthesis.
ADR: Oral thrush, GI disturbances and taste prevention.
Dose: 0.5-1g daily in single or divided dose.
Use: Systemically it is used for the infections caused by ringworm in body, hair and nail.
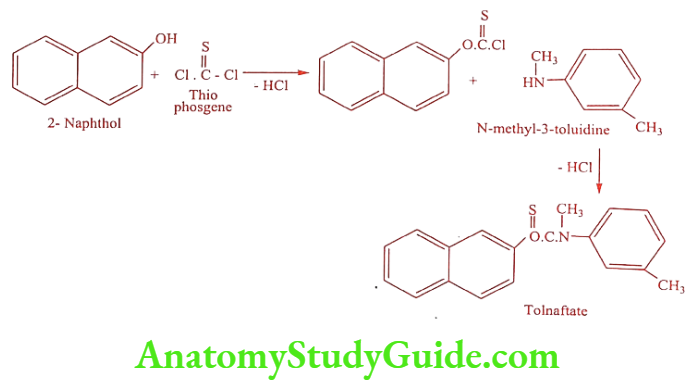
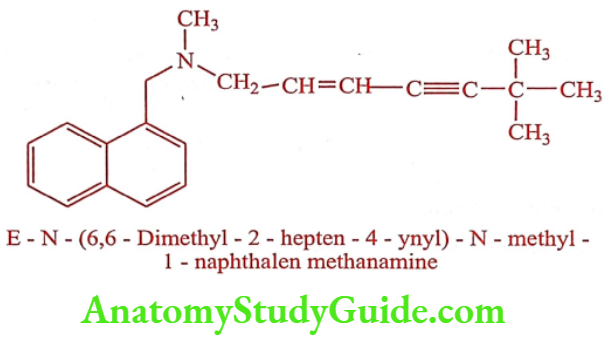
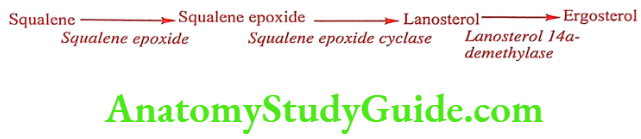
Allylamine and Related Compounds
All allylamines act as competitive inhibitors of squalene epoxidase, the enzyme involved in the conversion of squalene to squalene 2, 3 – epoxide in the early steps of ergosterol biosynthesis. Inhibition of this enzyme accumulates squalene in the fungal cell and disrupts the cellular organization.
Tolnaftate (Tinaderm-M, TINACTIN)
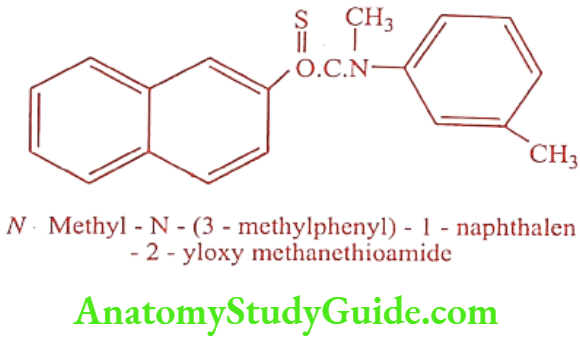
Synthesis
ADR: Irritation and pruritus.
Dose: 1% gel/solution/ powder/cream bid for 2 to 6 weeks.
Use: It is a fungicidal, effective against dermatophytes, ring worm, jock itch and athlete’s foot.
Terbinafine (Lamisil, Tefdin)
ADR: Anorexia, nausea, abdominal pain, taste disturbances, diarrhea, rash and urticaria.
Dose: 250mg once daily. Duration: 2 to 4 weeks (Tinea cruris), 4 weeks (Tinea corporis), 6 weeks (Tinea pedis) and 6 to 12 weeks (nail infections).
Use: It is a topical antifungal agent effective against Tinea pedis, Tinea corporis and Tinea cruris.
Azole Antifungal Agents
Azole antifungal agents are the largest class of antifungals available today with more than 20 drugs in the market. Azoles are five membered aromatic rings containing either two nitrogen (imidazole) or three nitrogen (triazole) with a side chain at N, containing at least one aromatic ring. The azoles with slow first pass metabolism like Ketoconazole, Fluconazole, Itraconazole, and Posaconazole are used systematically. The other azoles (Clotrimazole, Oxiconazole, Terconazole, Econazole, Sulconazole and Ketoconazole) are available as creams and ointments for topical treatment of dermatophytic infection and intravaginal use for vaginal yeast infections.
Azole can be further classified as
- Imidazole containing azole: eg. Clotrimazole, Oxiconazole, Lanoconazole, Ketoconazole, Miconazole, Sulconazole, Isoconazole, Tioconazole.
- Triazole containing azole: eg. Fluconazole, Voriconazole, Terconazole, Itraconazole, Posaconazole.
Mechanism of Action: All azoles act by inhibiting ergosterol biosynthesis through the inhibition of 14a-demethylase. Inhibition of this enzyme, results in accumulation of sterol bearing 14a-methyl group. This results in permeability changes and leaky membrane- imbedded protein, together causes fungal cell death.
Structure Activity Relationship
- A basic imidazole or 1, 2, 4 – triazole with pKa value of 6.5 to 6.8 is essential for antifungal activity.
- N3 of imidazole and N4 of imidazole of triazole bind to P450 iron.
- The most active ones have two or three aromatic rings, at least one of them is substituted with halogens or other non-polar groups (2, 4 – dichlorophenyl – 1, 4 -dichlorophenyl or 2, 4 – difluorophenyl).
- The most active azoles have fluoro in the structure.
- Ring substitution at other positions makes the azole inactive.
- The big non-polar part resembles the steroid molecule in binding to the enzyme.
Clotrimazole (Candial, Statum)
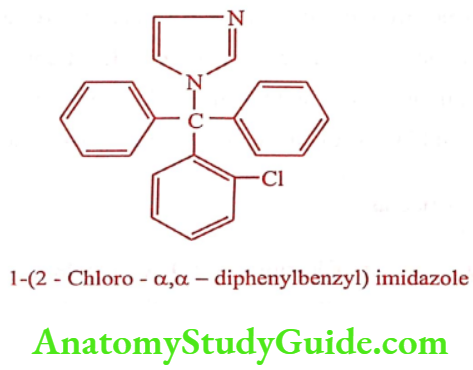
Synthesis
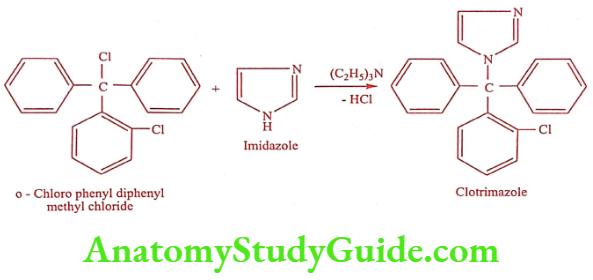
ADR: GI disturbances, erythema and irritation.
Dose: 100mg daily for 6 days.
Use: Effective against tinea pedis, tinea cruris, tinea capitis, tinea vesicular, cutaneous candidiasis and vulvo vaginal candidiasis.
Econazole (Ecanol Vaginal, Ecodax- G)
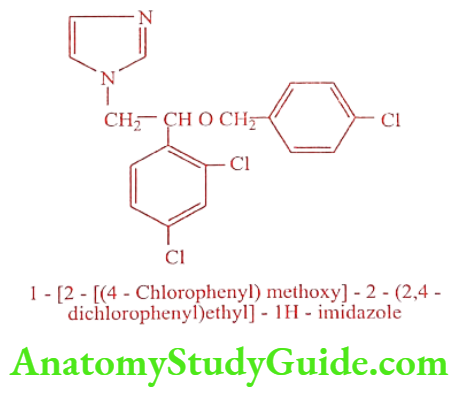
Synthesis
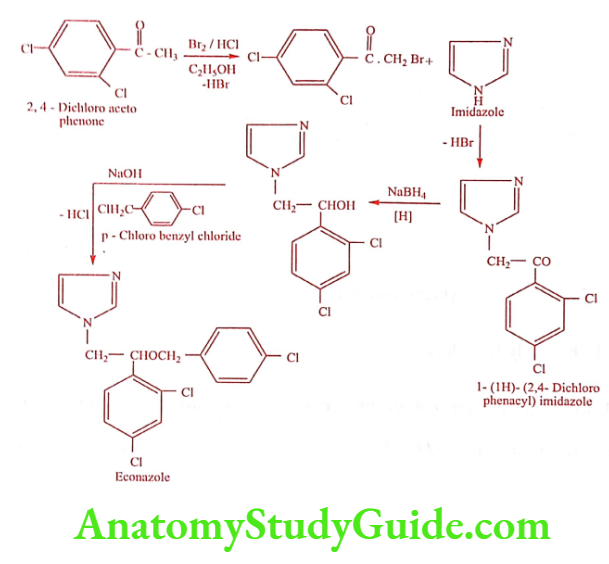
ADR: Vulvar/Vaginal burning and erythema.
Dose: 150mg pessaries once daily at bed time for 3 consecutive nights.
Use: It is used for the topical Tinea infection and Cutaneous candidiasis.
Oxiconazole (Zoderm-E)
Oxiconazole is available as nitrate salt.
![]()
ADR: Pruritus, burning and irritation.
Dose: 1% cream once daily for 2 weeks.
Use: It is used for the treatment of tinea pedis, tinea corporis and tinea capitis.
Miconazole (Micogel, Zole)
![]()
Synthesis
![]()
ADR: Nausea, vomiting, rash and drowsiness.
Dose: 2% cream or gel, sufficient quantity or about 5gm to be applied.
Use: It is used in systemic fungal infections such as Candidiasis, Coccidioidomycosis, Cryptococcosis, Petriellidiosis and Paracoccidioidomycosis.
Ketoconazole (Ketozole, Ketovate)
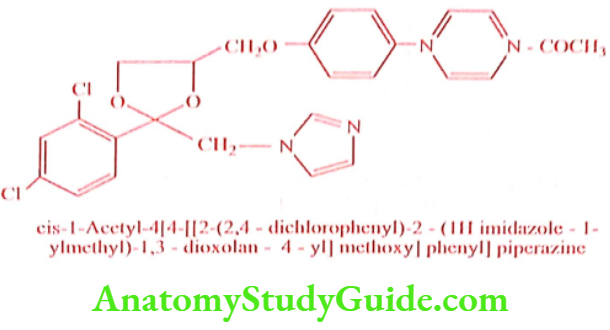
It is a broad spectrum imidazole antifungal agent used for systemic fungal infection. Bioavailability of Ketoconazole decreases when administered with antacid or drugs which raises stomach pH. It is a powerful inhibitor of CYP3A4 and causes interaction with other drugs (triazolam and cyclosporine).
ADR: GI disturbances, rash and dermatitis. In high dose it inhibits adrenocorticoids and testosterone results in gynaecomastia in male patients.
Dose: 200mg once daily.
Use: It is recommended for systemic fungal infections namely Candidiasis, Coccidioidomycosis, Blastomycosis and Histoplasmosis. It is used topically in the form of cream and shampoo for the management of Cutaneous candidiasis and Tinea infection. It has little effect on Aspergillus or Cryptococcus.
Itraconazole (Canditral, Fulcover)
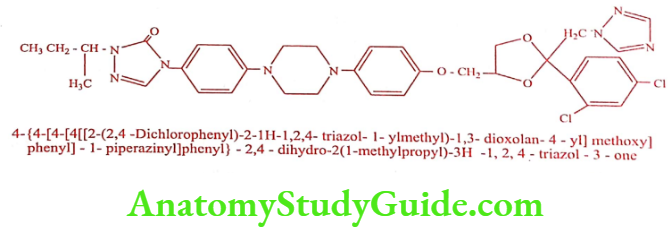
ADR: Dyspepsia and abdominal pain.
Dose: 100mg daily for 15 days.
Use: It is an orally active, broad spectrum antifungal agent. It is an important alternative to Ketoconazole.
Terconazole (Gyno-Terazol)
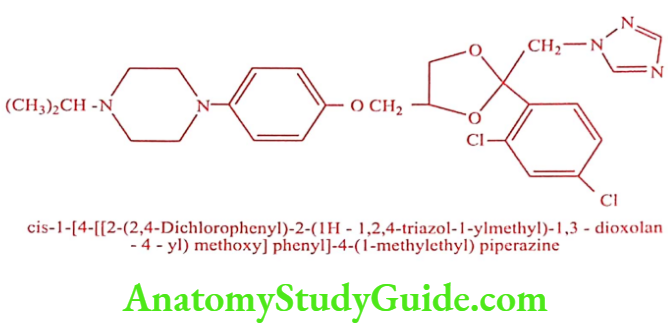
ADR: Vulvovaginal burning and vulvar itching.
Dose: 40mg (as 0.8% vaginal cream) or 80mg (as pessary) at bed time for three consecutive nights or 20mg at bedtime for seven consecutive nights.
Use: It is a triazole derivative used for the control of Vulvovaginal moniliasis caused by Candida albicans.
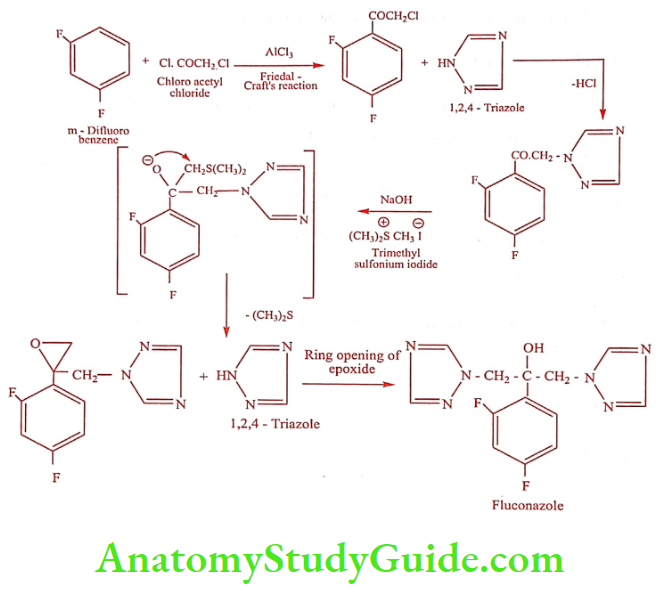
Fluconazole (Fluka, Fluzon)
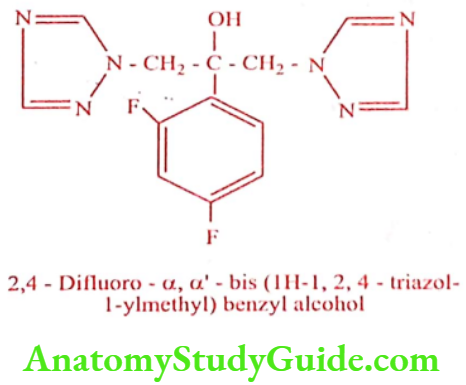
It has two advantages over other antifungal agents: (a) It can cross the blood brain barrier and (b) It has efficacy against Cryptococcus neoformans.
Synthesis
ADR: Nausea, abdominal pain and vomiting.
Dose: 50 to 100mg daily.
Use: It is used to control esophageal and oropharyngeal candidiasis.
Newer Antifungal Agents
Echinocandins
Echinocandins are newer antifungal agents. Drugs that interfere with cell wall biosynthesis would be expected to be relatively non-toxic to mammals. It interferes with cell wall biosynthesis through inhibition of the enzyme ẞ -1, 3- glucan synthase. B Glucan is an important polymer component of many fungal cell walls and reduction in the glucan content weakens the cell wall, leading to rupture of the fungal cell. Echinocandins, a group of cyclic peptides with long lipophilic side chain called as lipopeptides.
ADR: Fever, thrombophlebitis, head ache and elevated amino transferase.
Dose: 200mg loading dose followed by 100mg daily orally.
Use: It is used in the treatment of Candidiasis and Aspergillosis.
Caspofungin (Cancidas)
Caspofungin is a polypeptide antifungal related to pneumonia used in life threatening systemic fungal infections. It is effective against a variety of Candida species that are resistant to other agents as well as effective against Cryptococcus neoformans. It is orally inactive and administered by IV infusion.
ADR: Fever, nausea, vomiting, anaphylaxis and pulmonary edema.
Dose: 50mg daily.
Use: It is used to treat oesophageal Candidiasis and invasive Aspercillosis.
Leave a Reply