Morphology
Morphologies Features:
Table of Contents
The hallmark of lesions in systemic sclerosis is progressive fibrosis in affected tissues and organs.
The lesions are seen in the skin as well as there is disseminated visceral involvement:
- Skin changes: Skin is involved diffusely, beginning distally from fingers and extending proximally to arms, shoulders, neck, and face. In advanced stage, the fingers become claw-like and face mask-like.
Read And Learn More: General Pathology Notes
-
- Microscopically: Changes are progressive from early to late stage:
- Early stage shows edema and degeneration of collagen. The small-sized blood vessels are occluded and there is perivascular infiltration of mononuclear cells.
- The late stage reveals thin and flat epidermis. Dermis is largely replaced by compact collagen and there is hyaline thickening of walls of dermal blood vessels. In advanced cases subcutaneous calcification may occur.
- Kidney changes: Involvement of kidneys is seen in the majority of cases of systemic sclerosis. The lesions are prominent in the walls of interlobular arteries which develop changes resembling malignant hypertension. There is the thickening of tunica intima due to the concentric proliferation of intimal cells and fibrinoid necrosis of vessel wall.
- Smooth muscle of GIT: Muscularis of the alimentary tract, particularly the esophagus, is progressively atrophied and replaced by fibrous tissue.
- Skeletal muscle: The interstitium of skeletal muscle shows progressive fibrosis and degeneration of muscle fibres with associated inflammatory changes.
- Cardiac muscle: Involvement of interstitium of the heart by fibrosis may result in heart
failure. - Lungs Diffuse: fibrosis may lead to contraction of the lung substance. There may be epithelium-lined honey-combed cysts of bronchioles.
- Small arteries: The lesions in small arteries show enteritis due to intimal proliferation and may be the cause for Raynaud’s phenomenon.
Morphology Clinical Features:
Systemic sclerosis is more common in middle-aged women.
The clinical manifestations include:
- Claw-like flexion deformity of hands
- Raynaud’s phenomenon
- O esophageal fibrosis causing dysphagia and hypomotility
- Malabsorption syndrome
Respiratory distress - Malignant hypertension
- Pulmonary hypertension, and
- Biliary cirrhosis.
Inflammatory Myopathies
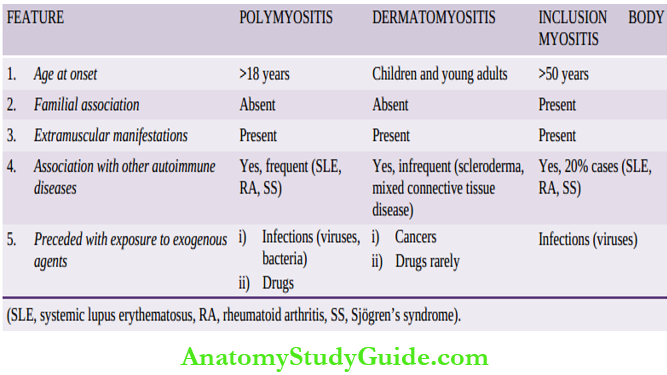
This group includes three conditions having overlapping clinical features of progressive skeletal muscle weakness: polymyositis, dermatomyositis, and inclusion body myositis, but distinctive age at presentation and some other features.
Contrasting features of inflammatory myopathies:
Etiology And Pathogenesis:
All three forms of inflammatory myositis appear to have an autoimmune etiology.
This is supported by the following:
Association with other autoimmune (collagen) diseases.
- Presence of various autoantibodies against nuclear and cytoplasmic antigens in 20% of cases.
- Presence of humoral immune mechanism in dermatomyositis as observed by B cell infiltration in the lesions.
- In polymyositis and inclusion body myositis, T-cell mediated cytotoxicity is implicated as seen by CD8+ T cells along with macrophages in the lesions.
- Some non-immune factors such as viral infection with coxsackie B, influenza, Epstein-Barr, CMV etc in triggering autoimmune mechanism has been suggested.
- Morphologic Features: There is symmetric involvement of skeletal muscles such as those of the pelvis, shoulders, neck, chest, and diaphragm.
- Histologically: Vacuolisation and fragmentation of muscle fibers and numerous inflammatory cells are present. In the late stage, muscle fibers are replaced by fat and fibrous tissue.
Inflammatory Myopathies Clinical Features:
- It is a multisystem disease characterized by:
- Progressive muscle weakness, mainly proximal
- Skin rash, typically with heliotropic erythema and periorbital oedema
- Dysphagia due to involvement of pharyngeal muscles
- Respiratory dysfunction, and
- Association with deep-seated malignancies.
Sjogren’s Syndrome
Sjögren’s syndrome is characterized by the triad of dry eyes (keratoconjunctivitis sicca), dry mouth (xerostomia), and rheumatoid arthritis. The combination of the former two symptoms is called Sicca syndrome.
Etiology And Pathogenesis:
Both humoral and cellular immune mechanisms have been implicated in the etiopathogenesis of lesions in Sjögren’s syndrome:
- There is B lymphocyte hyperactivity as seen by the rise of monoclonal immunoglobulins in 25% of cases.
- Presence of antinuclear antibodies in about 90% of cases.
- Positive rheumatoid factor in 25% of cases.
- Infiltration by T lymphocytes in exocrine glands.
- Association of disease with certain HLA class II genes.
- Association with other autoimmune diseases.
Morphologic Features:
In early stage, the lacrimal and salivary glands show periductal infiltration by lymphocytes and plasma cells, which at times may form lymphoid follicles (pseudolymphoma). In late stage, glandular parenchyma is replaced by fat and fibrous tissue.
The ducts are also fibrosed and hyalinised.
Morphologic Clinical Features:
The disease is common in women in 4th to 6th decades of life. It is clinically characterized by the following:
- Symptoms are referable to eyes such as blurred vision, burning, and itching.
- Symptoms referable to xerostomia such as fissure oral mucosa, dryness, and difficulty in
swallowing. - Symptoms due to glandular involvement such as an enlarged and inflamed lacrimal gland Mikulicz’s syndrome is involvement of parotid along with lacrimal gland).
- Symptoms due to systemic involvement referable to lungs, CNS, and skin.
IgG4-related Disease:
This is a recently described group of fibroinflammatory conditions which was initially described as autoimmune pancreatitis but now the condition has been seen affecting multiple organs.
Although the pathogenesis is still not fully clear, IgG4 production underlies the disease.
The salient features of the group are as under:
- Increased serum levels of IgG4
- Affects virtually every organ; pancreas, biliary tree, salivary glands, orbit and periorbital tissues, retroperitoneum, kidneys, lungs lymph nodes, etc
- Organ infiltration by IgG4-antibody-forming plasma cells, T lymphocytes
- Tumor-like fibrous lesions in the affected organ
- Clinical features depend upon the organs involved and thus manifestations are quite protean.
Types And Examples Of Autoimmune Diseases
Depending upon whether autoantibodies target a single organ or the disorder is systemic affecting multiple organs, autoimmune diseases are classified into 2 groups:
- Organ-specific (localized) and
- Organ non-specific (or systemic).
SLE is a classical example of systemic autoimmune or collagen disease. Autoantibodies against nuclear and nuclear components are demonstrable in plasma by immunofluorescence tests in almost all cases of SLE for example, ANA, anti-ds-DNA, and anti-Smetc.
- LE cell test is positive in 70% of cases. SLE is a multisystem disease and affects chiefly kidneys (lupus nephritis), skin, small blood vessels, and the heart.
- Scleroderma or systemic sclerosis may occur as diffuse form or as CREST syndrome. The disease involves the skin, kidneys, GIT, skeletal muscle, heart and lungs.
- Inflammatory myopathies are a group of 3 diseases having the common clinical features of progressive skeletal muscle weakness manifesting at different ages: polymyositis (>18 years), dermatomyositis (children and young adults) and inclusion body myositis (>50 years).
- Sjögren’s syndrome is characterised by the triad of dry eyes (keratoconjunctivitis sicca),
dry mouth (xerostomia), and rheumatoid arthritis. - The igG4-related disease is a recently described group of fibroinflammatory conditions affecting pancreas and extrapancreatic organs, characterised by high serum IgG4 levels and organ infiltration by IgG4-forming plasma cells and lymphocytes.
Leave a Reply