Bioceramics In Endodontics
- The term “bioceramic” refers to biocompatible material which is composed of ceramic as one of its constituents.
- These materials mainly consist of alumina and zirconia, bioactive glass, glass ceramics, coatings and composites, hydroxyapatite, and resorbable calcium phosphates.
- In dentistry, they are used as compositions of implants and periodontal surgeries, such as alveolar ridge augmentation.
- In endodontics, first use of bioceramics was mineral trioxide aggregate (MTA) which was used for perforation repair and root end filing.
- The promising clinical results achieved during the last two decades by MTA encouraged the evolution of new endodontic materials with improved biological, physical, and chemical properties.
- At present, there are more than 20 types of bioceramic materials which with properties comparable to MTA.
Read And Learn More: Endodontics Notes
Table of Contents
Bioceramics In Endodontics Classification
Bioceramics can be classified as:
- Bioinert
- These are noninteractive with biological systems, i.e., they do not demonstrate osteoconductive or osteoinductive properties but allow the growth of fibrous tissues around the material, for example, alumina, and zirconia.
- Bioactive
- The show interfacial interactions with surrounding tissue, i.e., they have osteoinductive and osteoconductive properties, for example, hydroxyapatites, bioactive glasses, and glass ceramics.
- Biodegradable, Soluble, or Resorbable
- These are broken down by the body and degraded; the resorbed material is eventually replaced by endogenous tissue, for example, tricalcium silicates and calcium phosphate.
Rationale Of Using Bioceramics
- Currently, bioceramics are used in most of the treatments like pulp capping, apexification, root-end filings, perforation repair, and pulp regeneration.
- The main rationale of using bioceramics in endodontics is their positive involvement in dental pulp pathology.
- When pulp experiences trauma or injury or pulp capping is done, growth factors released both by injury and protective pulp dressing play an essential role in organizing the cell differentiation and whole dentin-pulp complex regeneration.
- Within 24 hours after injury, there occurs an increased release of growth factors like FGF-2, VEGF, and PDGF in pulp tissue.
- The cause of neoangiogenesis is important for recovering the locally destroyed blood vessels and for stem cell recruitment. In this, mainly fibroblasts are involved though endothelial cells also interact.
- MTA and MTA-based materials have the capability to join to fibroblasts, endothelial cells, and growth factors by discharging transforming growth factor (TGF)-β 1 from injured pulp cells.
- Since pulp damage causes loss of primary odontoblasts, other cells are required for dentinogenesis, which is done by the differentiation of DPSC into odontoblast-like cells.
- MTA and MTA-like materials are conducive in promoting the proliferation and differentiation of DPSC and subsequently reparative dentinogenesis.
- During the setting of MTA, calcium ions are released that stimulate signaling molecules like interleukins (IL-1α and IL-1β), TGF-β, etc. which control cell growth and differentiation.
- Moreover, MTA acts as bioactive material due to the release of calcium hydroxide and calcium silicate hydrate during the hydration reaction of calcium silicates.
Advantages of Bioceramics
-
- Act as a regenerative scaffold of resorbable lattices which provide a framework that eventually dissolves as the body rebuilds tissue
- Intrinsic osteoinductive ability because of their tendency to absorb osteoinductive chemicals if bone healing is taking place adjacent to it
- Biocompatible due to their similarity with hydroxyapatite
- Antibacterial properties due to the release of calcium ions
- Ability to achieve an optimal hermetic seal and form a chemical bond with the tooth structure
- Radiopaque in nature.
Bioceramics Available In Endodontics
- Calcium silicate-based cement: Portland cement (PC), MTA, dentine.
- Sealers: Endo CPM Sealer, MTA Fillapex, BioRoot RCS, TechBiosealer.
- Calcium phosphates/tricalcium phosphate/hydroxyapatite based: Mixture of calcium silicates and calcium phosphates—iRoot BP, iRoot BP Plus, iRoot FS EndoSequence BC Sealer, BioAggregate
Portland Cement
Portland cement (PC) is obtained from the calcination of the mixture of limestones and silicon-argillaceous materials.
The calcined product is then fully grounded and mixed with water for use.
- Portland Cement Composition
- Portland cement consists of:
- Tricalcium silicate 50%
- Dicalcium silicate 25%
- Tetracalcium aluminoferrite 10%
- Tricalcium aluminate 10%
- Gypsum 5%
- Portland Cement Advantages
- Ealing ability is almost the same as that of MTA if used as root-end filling material
- Antibacterial properties—It shows antibacterial and antifungal properties similar to MTA against Enterococcus faecalis, Staphylococcus aureus, Pseudomonas aeruginosa, and Candida albicans
- Particle size—It is larger than MTA.
- Portland Cement Disadvantages
- Safety concerns due to higher amount of lead and arsenic released from PC
- Higher solubility endangers the long-term seal of the restoration
- Excessive sitting expansion may cause crack formation in the tooth
- Biomineralization is not as effective as with MTA
- Very low radiopacity, cannot be appreciated on the radiograph.
Mineral Trioxide Aggregate (MTA)
It was introduced by Dr. Torabinejad in 1993 as the first bioceramic material used in endodontics. It is osteoconductive, inductive, and biocompatible.
Till 2002, only gray MTA was available, later white MTA was introduced as ProRoot MTA (Dentsply) so as to overcome discoloration of teeth due to gray MTA.
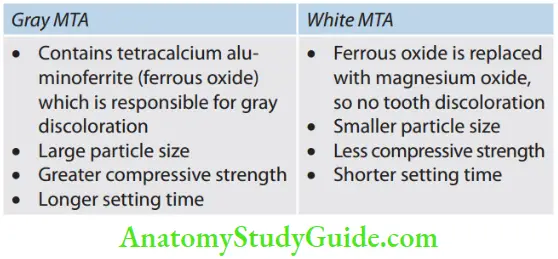
- Types of MTA
- It is available as gray and white MTA.
- Gray MTA: It contains tetra calcium aluminoferrite which is responsible for gray discoloration in gray MTA
- White MTA: It is tooth-colored with a smaller particle size
- Composition of MTA
- Portland cement (responsible for setting and biologic properties) 75%
- Bismuth oxide (provides radiopacity) 20%
- Gypsum (determines setting time) 5%
- Portland cement consists of:
- Tricalcium silicate: It is the main component in the formation of calcium silicate hydrate which gives early strength, to the cement
- Dicalcium silicate: It hydrates slower than tricalcium silicate and is responsible for late strength
- Tetracalcium aluminoferrite: It is present in gray MTA. It balances the heat which occurs during setting
- Tetracalcium aluminate: It forms 20% of the cement. During hydration, it reacts with calcium sulfate.
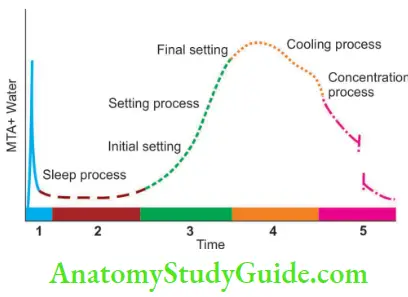
- Setting of MTA
- MTA is called hydraulic silicate cement because it sets and is stable underwater. It primarily relies on hydration reaction for setting. When mixed with water, MTA sets by process of hydration. The chemical reaction leading to the setting of the cement is called “hydration.” Hydration reaction is divided into different steps including the mixing process, sleep process, setting process, cooling process, and condensation process.
- During mixing, aluminate and gypsum dissolve in water and react. The aluminates dissociated from cement form a gel-like layer around the powder particles to prevent a fast reaction of aluminates and, thus, rapid setting of cement.
- During the sleep process, cement can be transported, placed, or processed. In this, cement components dissolve and saturate with water calcium in the cement and hydroxyl ions.
- The setting process starts when the water of cement is oversaturated with soluble calcium ions, new hydration products begin to form. The amount of new products formed in the setting period increases constantly resulting in solidification of the cement.
- The cooling process occurs when the cement has become saturated in terms of components. Cement gains strength in this period.
- In the concentration process, the reaction slows down and the heat output is reduced. Hydration products continue to generate and develop slowly and cement reaches the most rigid state.
- Manipulation of MTA
- To prepare MTA, a small amount of liquid and powder are mixed to putty consistency. Since MTA mixture is a loose granular aggregate (like concrete cement), it does not stick very well to any instrument. It cannot be carried out in a cavity with a normal cement carrier, and thus has to be tried with messing gun, amalgam carrier, or especially designed carrier. Once MTA is placed, it is compacted with burnishers and microbloggers. Unless compacted very lightly, the loosely bound aggregate will be pushed out of the cavity. Next, a small damp
cotton pellet is used to gently clean the resected surface and to remove any excess MTA from the cavity.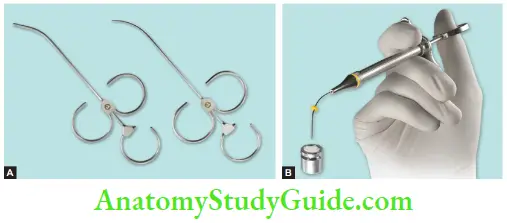
- To prepare MTA, a small amount of liquid and powder are mixed to putty consistency. Since MTA mixture is a loose granular aggregate (like concrete cement), it does not stick very well to any instrument. It cannot be carried out in a cavity with a normal cement carrier, and thus has to be tried with messing gun, amalgam carrier, or especially designed carrier. Once MTA is placed, it is compacted with burnishers and microbloggers. Unless compacted very lightly, the loosely bound aggregate will be pushed out of the cavity. Next, a small damp
- Mineral Trioxide Aggregate Properties
- Compressive strength: It takes 3–4 hours to set MTA. Compressive strength is 40 MPa immediately after setting and 70 MPa after 21 days. It is equal to IRM and super EBA but less than that of amalgam
- pH of MTA is 12.5 (when set), so it has properties similar to calcium hydroxide
- The setting time is 2 hours and 45 minutes
- In contrast to Ca(OH)2, it produces hard setting non-resorbable surface
- It sets in a moist environment (hydrophilic in nature)
- It has low solubility
- It shows resistance to marginal leakage
- It also reduces bacterial migration due to the release of calcium ions and high pH
- It exhibits excellent biocompatibility in relation to vital tissues.
- Difference between Gray and White MTA
- Gray MTA White MTA
Differences between Gray MTA and White MTA
- Advantages of MTA
- Water-based chemistry requires moisture for setting
- Excellent biocompatibility
- Normal healing response without inflammation
- Least toxic of all the filing materials
- More radiopaque than calcium hydroxide
- Bacteriostatic in nature due to high pH
- Resistance to marginal leakage
- Excellent sealing ability
- Produces artificial barrier against which obturating material can be condensed
- Vasoconstrictive, so benefiial for hemostasis, especially in cases of pulp capping.
- Disadvantages of MTA
- Difficult handling characteristics due to its sandy nature
- Long setting time (2 hours 45 minutes)
- Expensive
- Discoloration potential of gray MTA
- The known solvent is present so difficult to remove after curing.
- Precautions to Be Taken for MTA
- MTA material should be kept in a closed container to avoid moisture contamination
- MTA must be stored in a dry area
- MTA material should be immediately placed after mixing with liquid to prevent dehydration during setting
- Do not irrigate after placing MTA, and remove excess water with a moist cotton pellet
- Adding too much or too little liquid will reduce the ultimate strength of the material
- MTA material usually takes 3–4 hours but the working time is about 5 minutes. If more working time is needed, the mixed material should be covered with a moist gauze pad to prevent evaporation.
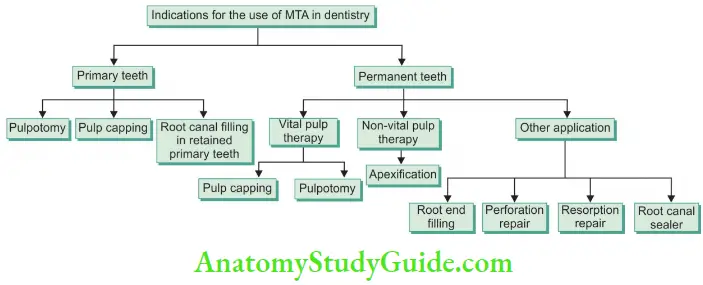
- Indications of Use of MTA The use of MTA in dentistry is described in the following flowchart:
- Contraindications of Use of MTA
- It is not indicated for obturation of primary teeth which are expected to exfoliate because it resorbs very slowly.
- Clinical Applications of MTA
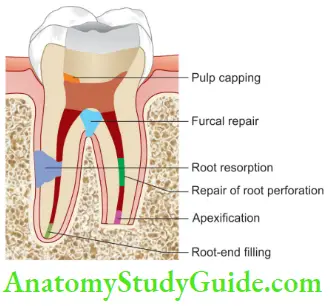
- Pulp Capping
- By placing MTA over the exposed area allows healing and preservation of vital pulp without further treatment. Rinse the cavity with sodium hypochlorite to disinfect the area. Mix the MTA with enough sterile water to give it a putty consistency. Apply it over the exposed pulp and remove the excess. Blot the area dry with a cotton pellet and restore the cavity with an amalgam or composite filling material.
- Apexogenesis
- Vital pulp—isolate the tooth with a rubber dam and perform a pulpotomy procedure. Place the MTA over the pulp stump and close the tooth with temporary cement until the apex of the tooth close.
- Pulp Capping
-
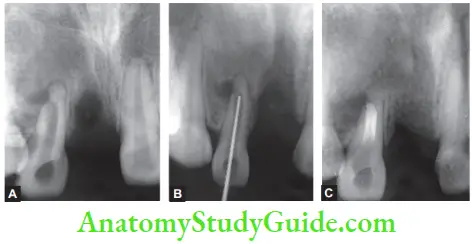
- Apexification
- Nonvital pulp—isolate the tooth with a rubber dam and perform root canal treatment. Mix the MTA and compact it to the apex of the tooth, creating a 2 mm thickness of the plug.Wait for it to set; then fill in the canal with cement guttapercha.

- Internal and External Root Resorption
- In internal resorption cases, after cleaning and shaping, prepare a putty mixture of MTA and fill the canal with it, using a plugger or gutta-percha cone, and obturate the canal.
- In the case of external resorption, complete the root canal therapy for that tooth. Raise a flap and remove the defect on the root surface with a round bur. Mix the MTA in the same manner as above and apply it to the root surface. Remove the excess cement and condition the surface with tetracycline. Graft the defect with decalcified freeze-dried bone allograft and a calcium sulfate barrier.
- Perforation
- Complete the cleaning and shaping of the perforated canal. If perforation is at mid-to-apical third, then follow the directions for treating internal resorption. If the perforation is closer to the coronal third, then obturate the canal with guttapercha, remove the gutta-percha below the perforation, and fil MTA in the canal with a plugger.
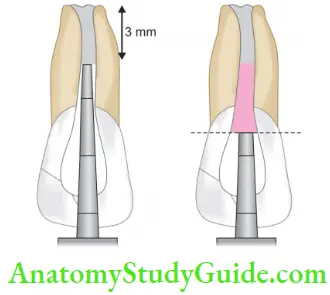
- Root-End Filling
- Prepare a class I cavity at the root end, mix MTA, and condense it into the cavity using a small plugger. Remove the excess cement with the help of a moist gaug
- Apexification
Bioceramics In Endodontics Conclusion
- When compared to conventional materials used in endodontic treatments, bioceramic cement are not only biocompatible but also bioactive as they proved to be involved in controlling tissue healing and pulp regeneration.
- Seeing the advantages of bioceramics, recent studies favor bioceramic materials even if not many products are available for use.
- Being biocompatible and bioactive materials, these are used in root perforations, large apical foramen, and root resorptions. MTA or MTA-like cement have been used as materials of choice in regenerative endodontics, vital pulp therapy, and periradicular surgery due to their clinical success rate.
- Based on the in-progress technology of fabrication, it is expected that the newer bioceramic cement will overcome the drawbacks of previous ones, mainly the discoloration problem. With further research, bioceramics have the potential to become the preferred materials for various endodontic procedures.
Leave a Reply