Dental Injuries To Permanent Teeth In Mixed Dentition Introduction
Injuries to permanent teeth in mixed dentition are synonymous with injuries to incisors.
Table of Contents
Fall-at-play, corridor collisions, and contact sports are the common modes of traumatic injuries to permanent incisors.
In permanent incisors, tooth fractures are more common than luxation injuries.
The alveolar bone is denser and mineralized to a higher degree when compared to the primary dentition.
Read And Learn More: Paediatric Dentistry Notes
Also, the alveolar spaces are lesser in volume leading to a decrease in resiliency.
So, a permanent incisor encounters trauma; the alveolar bone resists the impact.
The tooth is compelled to receive the force and undergo either a crown fracture or a crown–root fracture or a root fracture in this process.
Dental Injury
Luxation or displacement injuries are, however, not rare. An injury to the supporting bone presents a luxation injury.
The various types of traumatic injuries to permanent teeth in mixed dentition are as follows:
1. Tooth fractures
- Crown fractures
- Crown–root fractures
- Root fractures
2. Luxation injuries
- Concussion
- Subluxation
- Lateral luxation
- Intrusive luxation
- Extrusive luxation
- Avulsion
These injuries have been discussed with regard to primary teeth.
They are again discussed here as the treatment plan and prognosis are significantly different in the case of injury to permanent teeth in mixed dentition.
Fractured Tooth Symptoms
Tooth Fractures
Tooth fractures may involve only the crown or only the root or both the crown and the root.
These types are further classified as follows to decide upon the treatment.
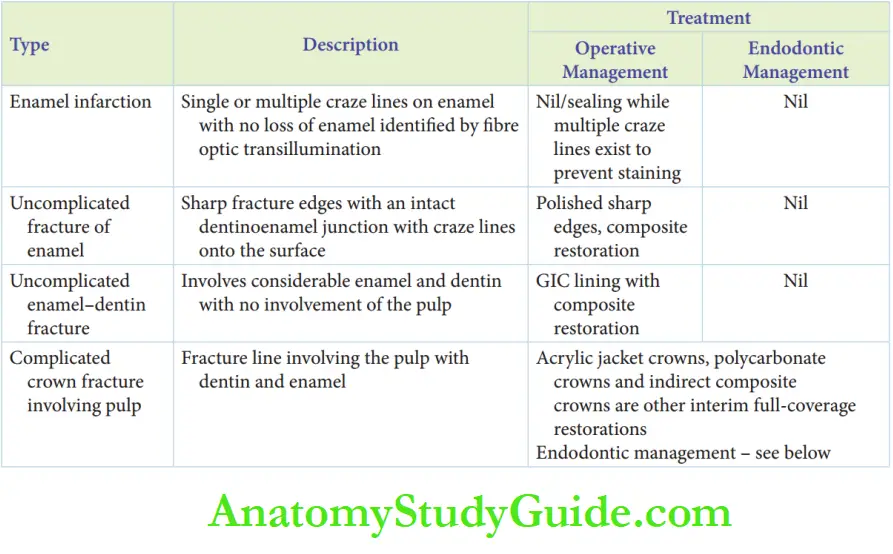
Fractured Tooth Symptoms – Crown Fractures
Crown fractures are the commonest of dental injuries to permanent teeth.
These fractures can manifest in four types, as follows:
1. Fractured Tooth Symptoms – Enamel infarction: It presents as single or multiple craze lines on enamel with no loss of enamel.
Enamel infarction may be missed on examination with normal illumination (dental chair light).
It can be identified when light is passed perpendicular to the enamel surface and by fire optic transillumination.
Enamel infarction craze lines are indicative of associated injuries to the supporting bone of the tooth involved.
Dental Injury
2. Uncomplicated fracture of enamel: It presents sharp fracture edges with an intact dentin enamel junction.
It may present craze lines extending from the fractured margins onto the surface.
3. Uncomplicated enamel–dentin fracture: Uncomplicated enamel–dentin crown fracture involves considerable enamel and dentin with no involvement of the pulp.
Dentin is clearly visible at the site of the fracture.
4. A complicated crown fracture involving pulp:
Complicated crown fracture implies the fracture line involving the pulp with dentin and enamel.
When the pulp is exposed, three parameters are assessed to formulate a treatment plan as follows:
- Size of exposure
- Duration of exposure
- Completeness of root formation
Tooth Fracture Treatment:
Treatment can be described under two heads, namely endodontic management and crown structure rehabilitation.
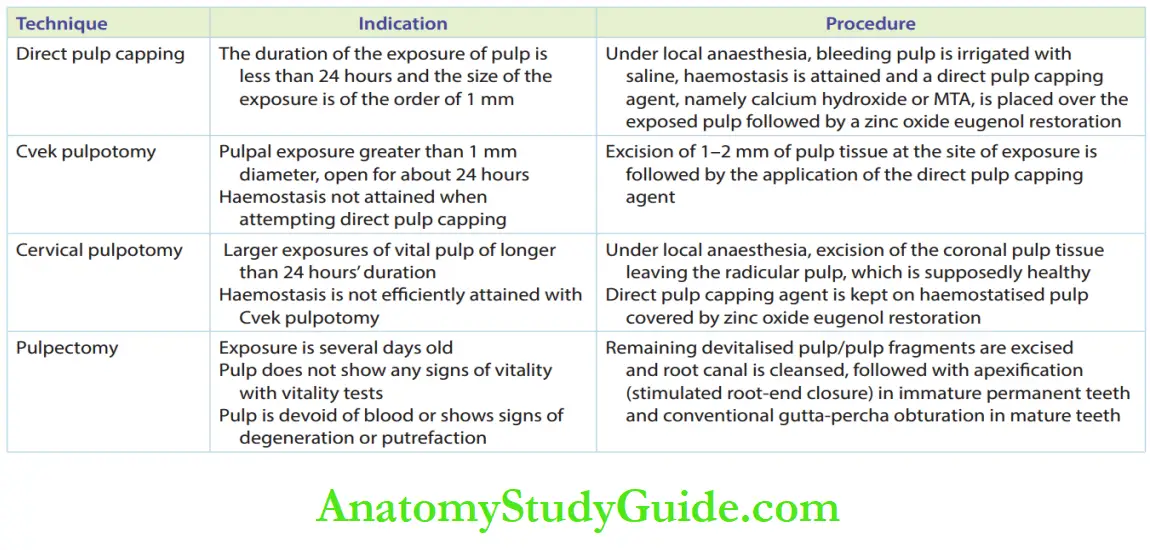
1. Endodontic management: The various treatment modes of managing traumatically exposed pulps are direct pulp capping, pulpotomy, and pulpectomy.
Direct pulp capping, Cvek pulpotomy, and cervical pulpotomy are conservative modes of endodontic management of traumatized incisors.
These methods are significant in immature permanent teeth as pulp tissue is the primary requisite for physiologic root-end closure (abiogenesis).
The status of the pulp has to be constantly reviewed for signs of pulpal degeneration.
Endodontic management techniques are enumerated.
Dental Injury
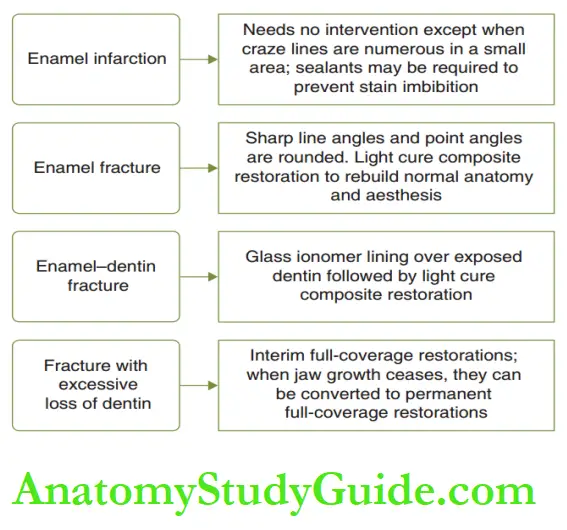
2. Crown structure rehabilitation: The objective of crown structure rehabilitation is to restore the form and pre-existed morphology of the tooth.
Crown fractures and their corresponding rehabilitation modes are described.
Interim full-coverage restorations usually serve for 1–3 years.
When the pulp would most probably require a re-entry, glass ionomer cement which is used as a lining can be used to build up the tooth surface.
This is called ‘bandage restoration’. Acrylic jacket crowns, polycarbonate crowns, and indirect composite crowns are other interim full-coverage restorations.
Permanent modes of crown rehabilitation, such as full ceramic crowns or metal-ceramic crowns, are resorted to on completion of jaw growth.
3. Incisal edge re-attachment technique (IERT): Apart from endodontic management and crown structure rehabilitation, another technique to restore a fractured tooth is the incisal edge reattachment technique.
When the fractured tooth fragment is retrieved, it can be bonded to the fractured tooth.
This has the advantage of maintaining positive patient psychology, and it would be the most biocompatible mode to rehabilitate the
crown structure.
Fractured Tooth Symptoms – Dental Injury
The procedure is as follows:
- The retrieved tooth fragment is washed with hydrogen peroxide and saline to clear the debris and blood stains.
- It is carried on a sticky wax stick.
- The fragment is trial fitted to the fractured tooth and the procedure is carried out only when a close adaptation is present.
- The sharp line and point angles are rounded in the fragment as well as in the fractured tooth.
However, this step should not be overzealous to compromise the adaptation.
The fractured tooth surface and the fragment are etched and a bonding agent is applied.
A flowable resin is used to bond the fragment with the tooth. Any leftover defect is reinforced with light cure composite resin.
The inlay wax stick is snapped off the fragment cautiously.
Dental Injury
The excess resin material is trimmed and the interface is polished. A case description of IERT.
Crown–Root Fractures:
The crown–root fractures are those that involve enamel, dentin, and cementum.
They may be described as uncomplicated when the pulp is not involved and complicated when the pulp is involved.
The outline of management of crown–root fractures is the same as that for crown fractures.
The decision of saving or sacrificing the fractured tooth depends on the storability of the tooth.
A tooth infected with crown–root fractures can usually be saved when the amount of residual crown structure is barely sufficient (possess the necessary resistance form) to hold on to the restoration.
Else, the fractured fragment can be extruded to improve the resistance form.
If enough marginal seal can be obtained, conservative modes are chosen to save the tooth, else the fragment is extracted.
When the fracture line runs too oblique, almost near a vertical fracture, endodontic therapy is contraindicated and the tooth is extracted.
Crown–Root Fractures Treatment:
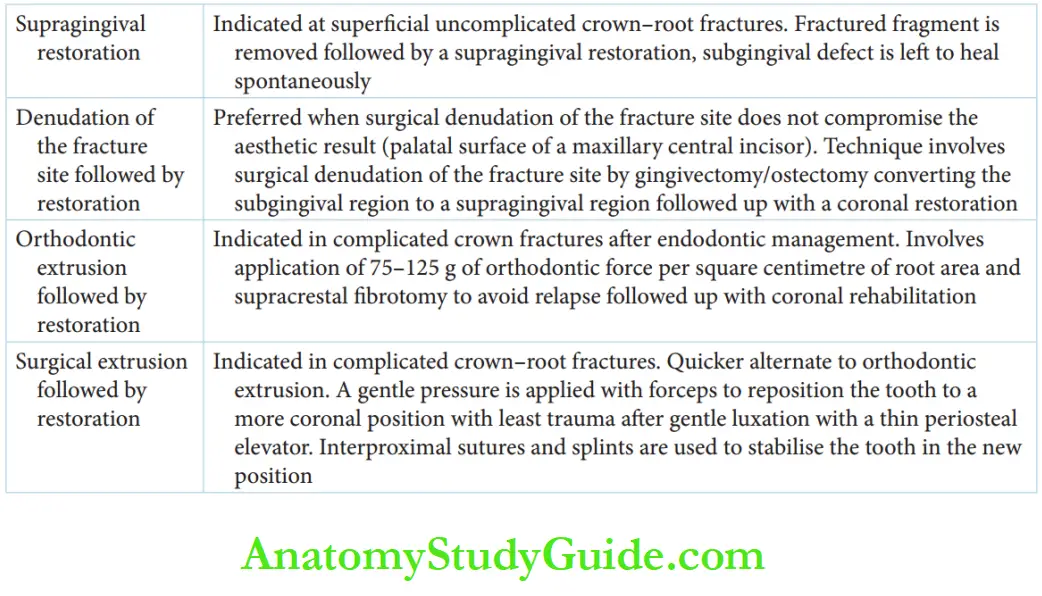
There are four distinct modes of management of crown–root fractures:
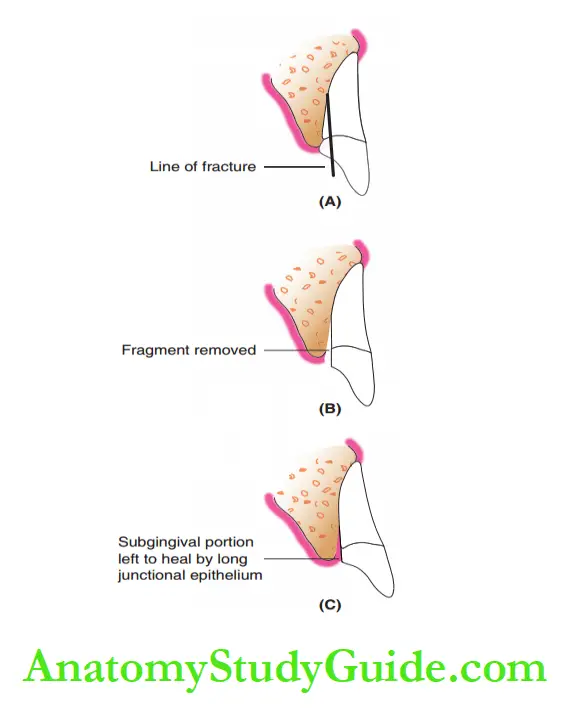
1. Supragingival restoration: It is indicated for the superficial uncomplicated crown–root fractures.
The fractured fragment is removed and a supragingival restoration is done immediately to establish the form of the tooth and to enhance aesthesis.
The subgingival defect is left to heal spontaneously by the organization of the marginal gingival fires and by the formation of a long junctional epithelium.
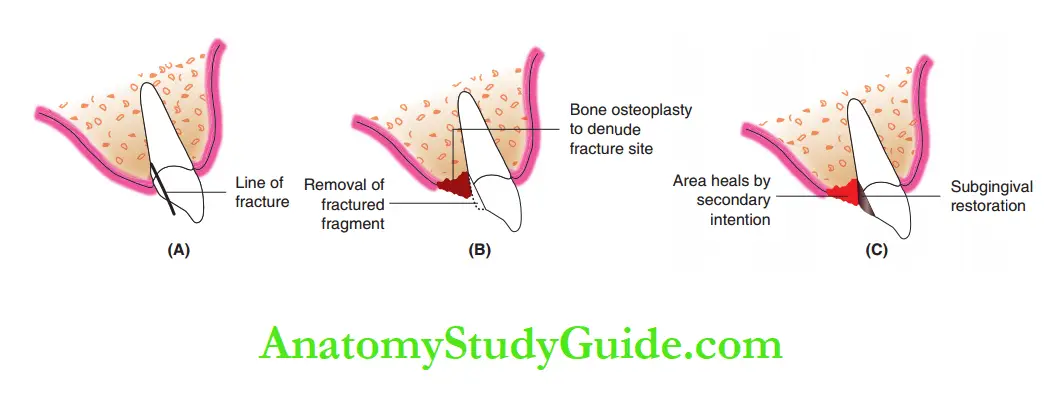
2. Denudation of fracture site followed by restoration:
This technique is usually preferred when surgical denudation of the fracture site does not compromise the aesthetic result.
For instance, a fracture of the maxillary central incisor involving the palatal surface subgingivally can be treated with this technique.
This technique involves surgical denudation of the apical end of the fracture site, by gingivectomy or by mastectomy sometimes.
By denudation, the subgingival region is converted into a supragingival region.
The exposure is followed by a coronal restoration leading to an increase in the clinical length of the crown of the involved tooth surface.
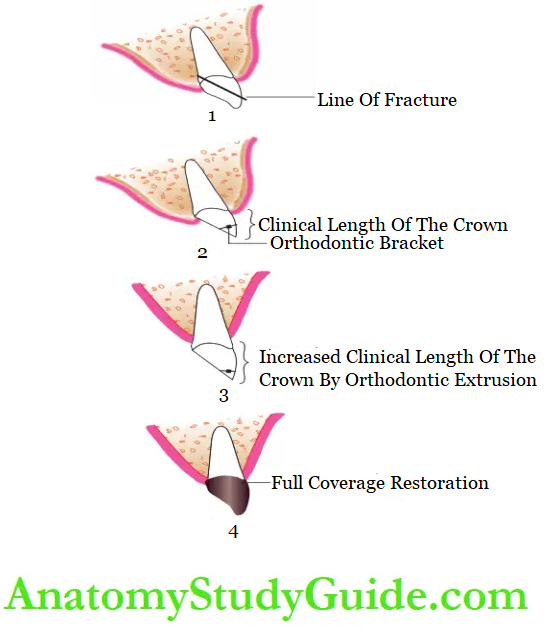
3. Orthodontic extrusion of the residual tooth structure followed by restoration: This procedure is the treatment of choice in complicated crown fractures after endodontic management of the exposed pulp.
It involves the application of 75–125 g of orthodontic force per square centimeter of root area by the mode of a bracket bonded to the residual crown structure.
A post-orthodontic suprarenal frenotomy is performed to avoid relapse.
This procedure involves time and delays aesthetic rehabilitation.
However, it ensures a stable position of the gingiva and optimal gingival health.
4. Surgical extrusion of the fragment followed by restoration: Surgical extrusion is a quicker alternative to orthodontic extrusion (mentioned in the preceding text).
The tooth fragment is luxated in the least traumatic manner with a thin, sharp periosteal elevator.
Gentle pressure is applied with forceps to reposition the tooth to a more coronal position.
The tooth is stabilized in the new position by interproximal sutures and splints.
Root canal therapy is instituted in 3–4 weeks and the final restoration rehabilitated with an intracanal post is given in 1–2 months’ time.
Orthodontic extrusion of the residual tooth structure followed by restoration at the site of the crown–root fracture.
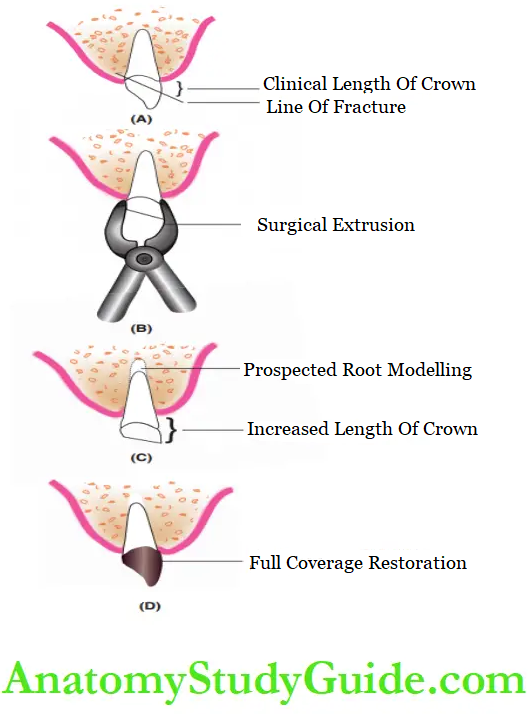
Although this is a rapid mode of restoring the tooth to a more stable position, it is indicated in complicated crown–root fractures and not in uncomplicated fractures.
This is because it may devitalize the uninvolved pulp in an uncomplicated fracture, thus making the usually unnecessary endodontic therapy mandatory.
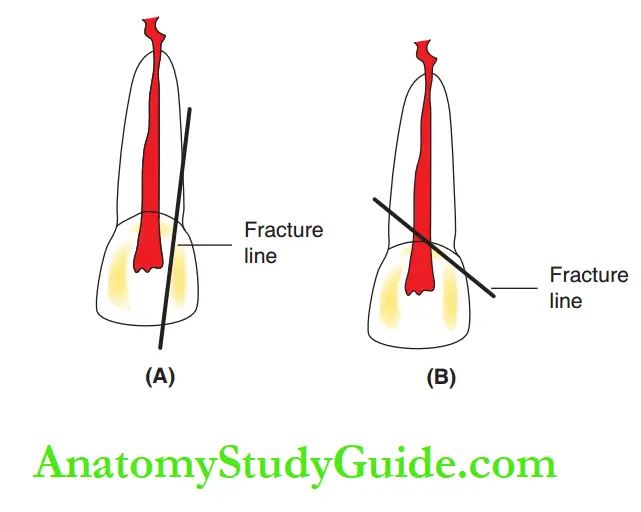
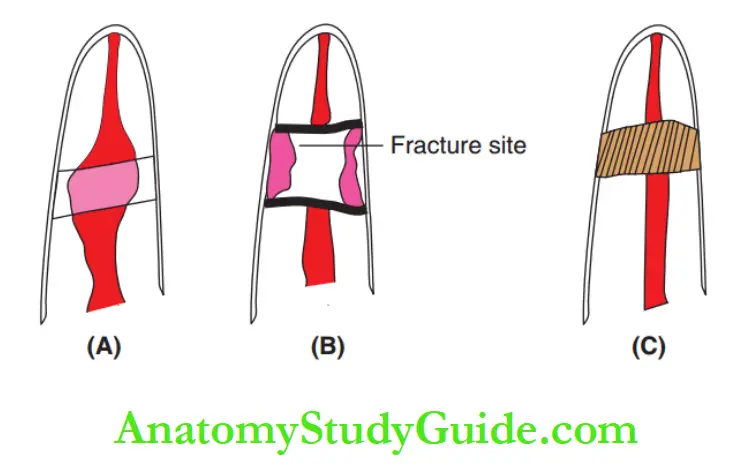
Root Fractures:
Root fractures are those involving cementum, dentin, and pulp.
They are relatively less common traumatic injuries; they form about 0.5–7% of all dental injuries to permanent teeth.
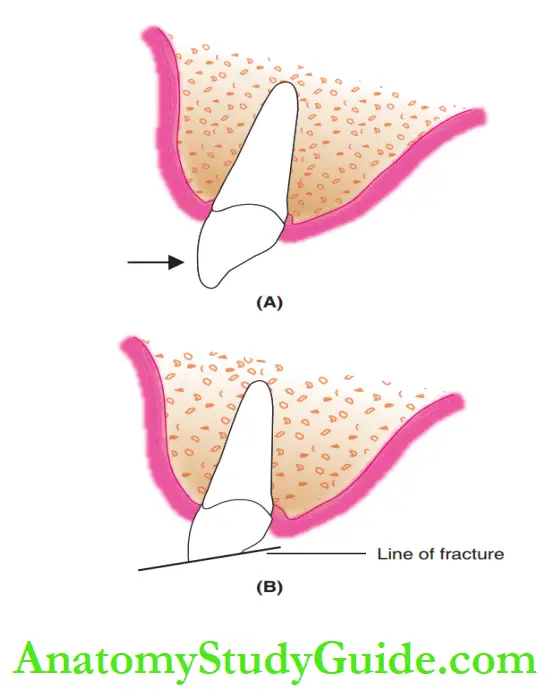
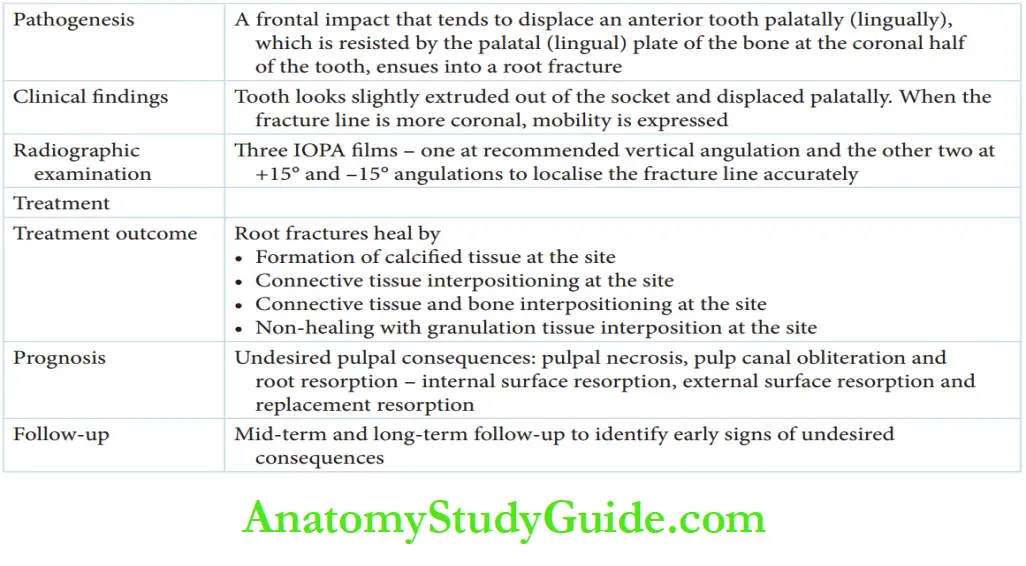
Dental Injury Pathogenesis:
A frontal impact displaces the tooth palatally. It is resisted by the palatal alveolar bone plate in the coronal half.
This tooth incurs a root fracture, most commonly in the middle third of the root.
Fractures of the apical and coronal third may also occur. A simple transverse fracture is the commonest presentation although oblique and multiple fractures are reported.
Dental Injury Clinical Features:
On clinical examination, the tooth looks slightly extruded from the socket and displaced palatally.
The formation of hemorrhage at the line of fracture is the reason for the displacement.
If the fracture line is more coronal, mobility is expressed, else it is immobile.
Luxation injuries and displacement during root fractures look strikingly similar clinically.
A radiographic examination is essential to differentiate between the two conditions and arrive at a diagnosis.
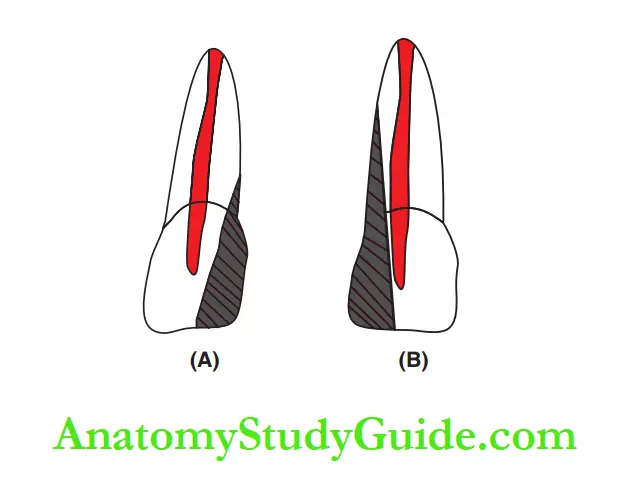
Dental Injury Radiographic Examination:
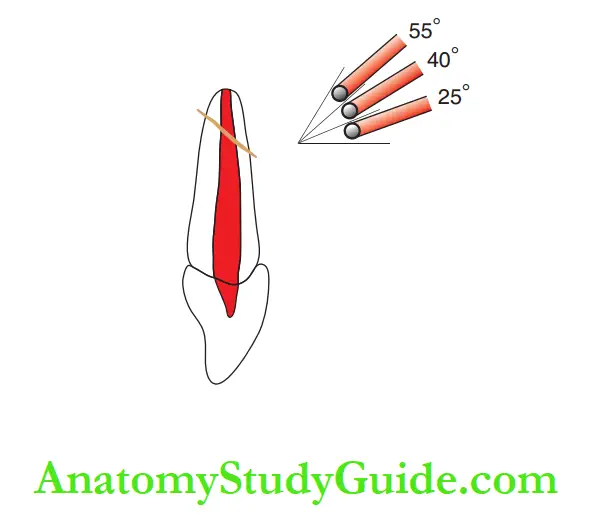
A radiographic examination done with three IOPA films is an appreciable mode of investigation.
The first IOPA fim is recommended at a vertical angulation (40° for central incisors), the second at a steeper angulation (55° vertical angulation), and the third at an angulation 15° lesser than the fist angle (25° vertical angulation).
These radiographs, taken consecutively, identify and localize the fracture line in the root more accurately.
Treatment:
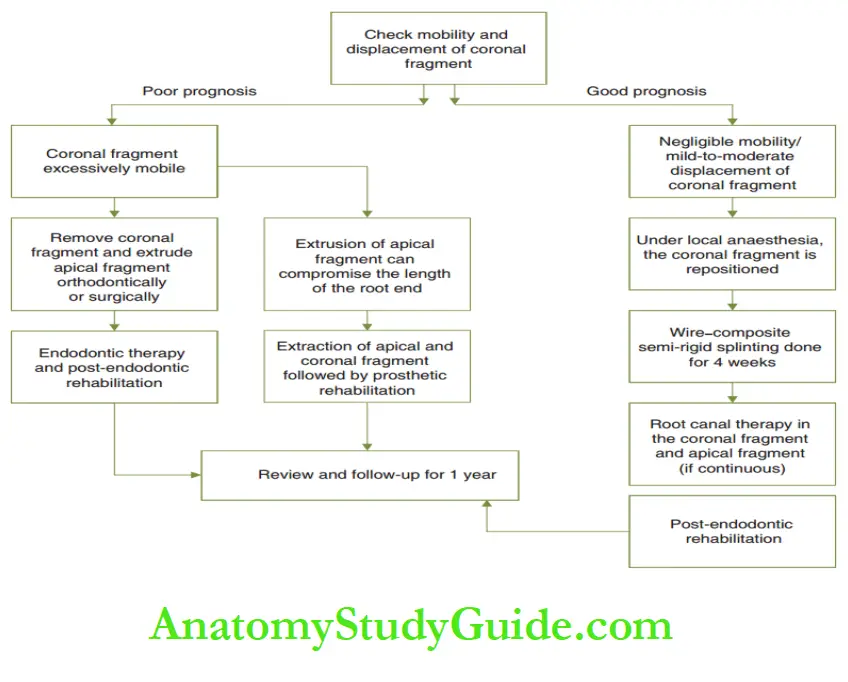
The outline of the management of root fractures.
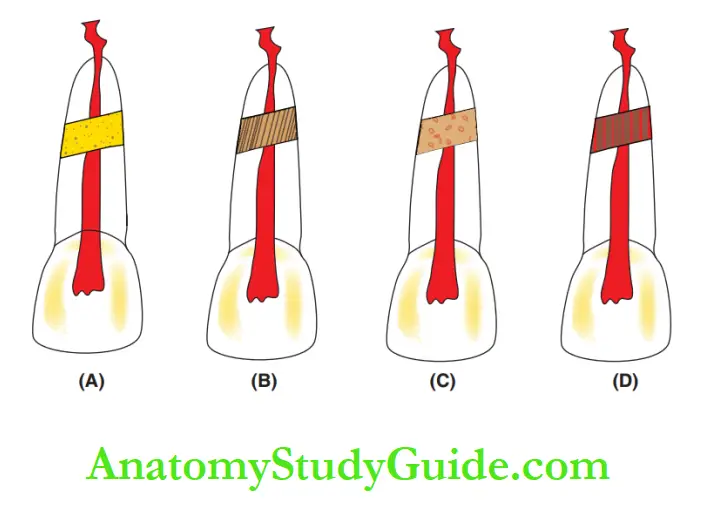
A treated root fracture can heal in the following four different patterns:
- Formation of calcified tissue at the site
- Connective tissue interposition at the site
- Connective tissue and bone interposition at the site
- Non-healing with granulation tissue interposition at the site.
A variety of undesired pulpal consequences are bound to occur which range from pulpal necrosis to pulp canal obliteration to root resorption.
A tooth salvaged after a root fracture necessitates a long-term follow-up to identify the early signs of undesired consequences.
The following three types of root resorption are reported:
- Internal surface resorption (internal resorption)
- External surface resorption (external resorption)
- Replacement resorption (ankylosis)
Luxation Injuries
Luxation injuries of permanent teeth in mixed dentition are serious as the preservation of the displaced tooth is the top priority.
Tooth Luxation
Lateral luxation and intrusive luxation.
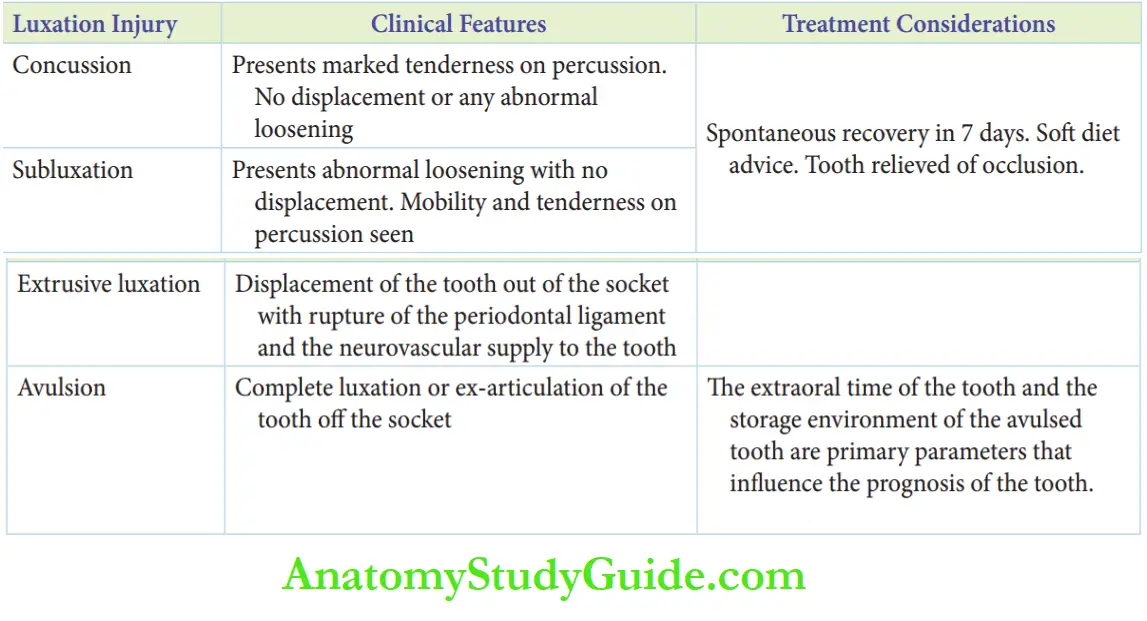
Concussion And Subluxation:
Concussion and subluxation are injuries to the supporting bone.
Concussion implies hemorrhage and edema in the periodontal ligament following an impact leading to NO displacement of the tooth or any abnormal loosening.
A concussion is associated with marked tenderness on percussion.
Subluxation implies tearing of the periodontal fires owing to an impact of greater force leading to abnormal loosening but with NO displacement of the tooth.
The tooth expresses mobility and tenderness on percussion. Both of these injuries undergo spontaneous remission in about 7 days.
The tooth is relieved of occlusion.
Tooth Luxation
Anti-inflammatory drugs are prescribed and splinting is not necessary.
The tooth is reviewed after 4 weeks.
Extrusive Luxation:
Extrusive luxation is the displacement of the tooth out of the socket with a rupture of the periodontal ligament and the neurovascular supply to the tooth.
The palatal gingival fires play a major role in preventing the avulsion of the tooth.
The tooth appears displaced with an increase in the clinical length of the crown.
Bleeding is expressed from the periodontal ligament and the tooth is dull on percussion.
An IOPA shows an expanded periodontal ligament space apically.
The treatment varies with the time of reporting of the patient following injury.
Either way, the tooth has to be reviewed for 1 year. Pulpal necrosis, pulp–canal obliteration, and external root resorption are undesirable late consequences of extrusive luxation.
The early signs of these consequences warrant a pulpectomy.
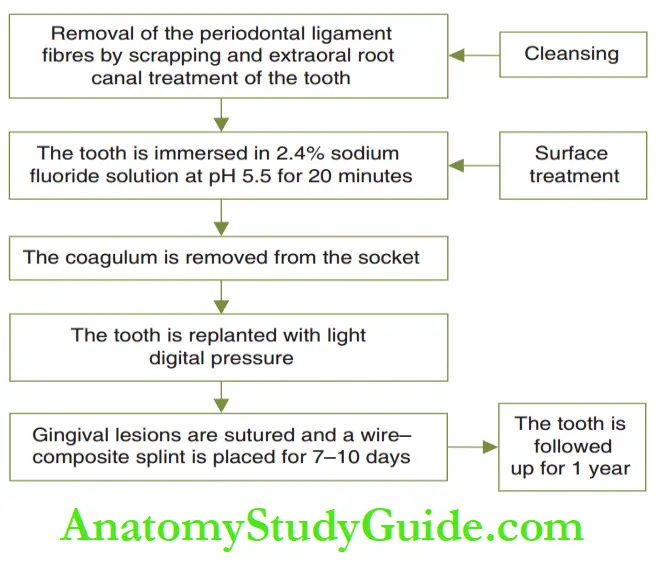
Avulsion Tooth
Avulsion or a complete luxation is synonymous with ex-articulation.
The Avulsion Tooth is completely out of the socket. It accounts for 0.5–3% of all dental injuries and is common in fall injuries and sports injuries.
The extraoral time of the tooth and the storage environment of the avulsed tooth are primary parameters that influence the prognosis of the tooth.
Associated alveolar bone fractures have to be suspected in avulsion injuries.
Ideal Mode Of Storage And Transport Of The Avulsed Tooth To The Dental Office:
The parents are advised (more commonly over the phone) to try to reposition the tooth into the socket.
Else, the child may be instructed to hold it in the vestibule pooled with saliva before reporting to the dental office.
If repositioning is not possible and the child is too young and apprehensive to hold it in the vestibule, milk, saline, or tender coconut water are the suggested media for storage and transport of an avulsed tooth.
They are asked to report as soon as possible.
Avulsion Tooth
Chances of saving the tooth after re-plantation are highest when done within 2 hours of the injury and the tooth has been appropriately stored and transported.
The favorable chances drop to one-half when the extra-alveolar time of the tooth crosses 6 hours and are almost nil at 24 hours.
Replantation of the avulsed tooth with short extraoral time and transported in an ideally wet storage medium is carried.
Management of an avulsed tooth.
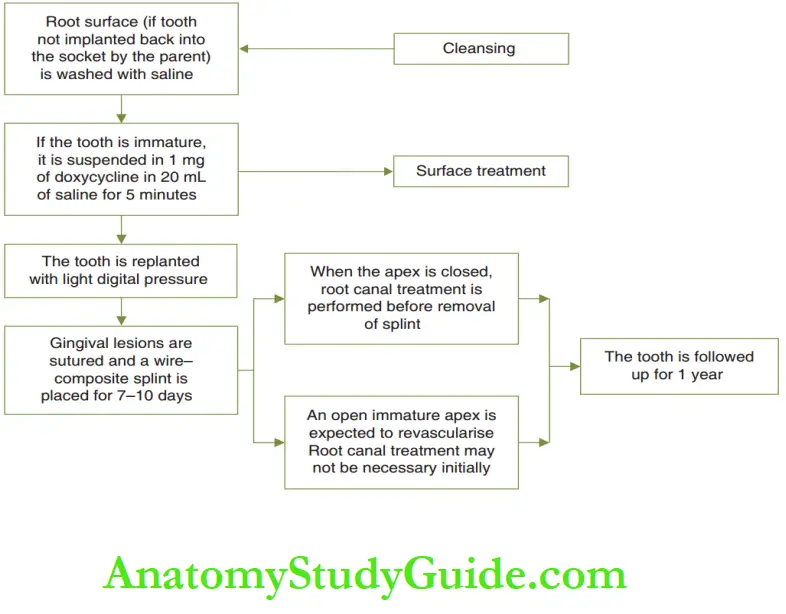
Avulsion Tooth Prognosis:
When the extra-alveolar time is short and the avulsed tooth is transported in an appropriate medium, the tooth is either re-accepted (mature tooth) or revascularized (immature tooth).
Success rates range from 21% to 89%.
Root resorption or replacement resorption are undesirable consequences.
Avulsion Tooth Case Description
Avulsion Tooth Case I
Avulsion Tooth Clinical Scenario: A 10-year-old male child reported broken upper front teeth.
the child fell 3 hours before and reported the broken fragments of the teeth.
Summary
1. In permanent incisors, tooth fractures are more common than luxation injuries as the alveolar bone is denser with low resiliency.
Luxation or displacement injuries are, however, not rare.
2. The various types of traumatic injuries to permanent teeth in mixed dentition are crown fractures, crown–root fractures, and root fractures.
3. Crown fractures:
The endodontic treatment plan for a complicated fracture is decided based on the following:
- Size of exposure
- Duration of exposure
- Completeness root formation
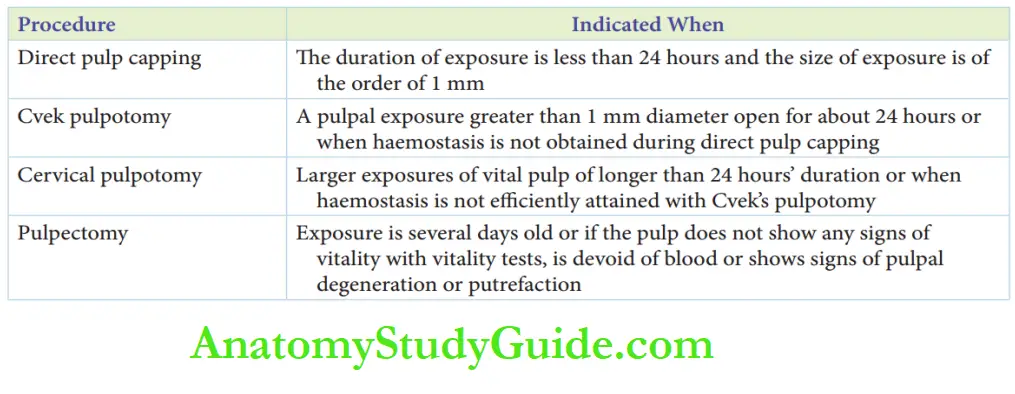
Direct pulp capping, Cvek’s pulpotomy, and cervical pulpotomy are conservative modes of endodontic management of traumatized incisors and are significantly important with immature permanent teeth as the salvaged pulp is the primary requisite for physiologic root-end closure (abiogenesis).
The incisal edge reattachment technique is the most biocompatible mode to rehabilitate crown structures where the retrieved (fractured) tooth fragment is bonded to the fractured tooth.
4. Crown–root fractures:
- Involve enamel, dentin, and cementum – may be uncomplicated/complicated
- The outline of management of crown–root fractures is the same as crown fractures
- The decision to save or sacrifice is based on the storability of the tooth structure.
- Modes of management:
Root fractures:
- Less common injuries involving cementum, dentin, and pulp
- The commonest type of root fracture is a simple transverse one
6. Luxation injuries of permanent teeth in mixed dentition
Leave a Reply