Diagnosis and Removal Of Dental Caries Introduction
Early diagnosis requires minimal intervention for rehabilitation. When a sugary substrate is available for the plaque bacteria, acid production and cavitation become inevitable. Judicious use of fluorides, dietary modification and adequate plaque control can reduce the progress, arrest it or reverse the lesion.
Table of Contents
Early diagnosis of the carious process provides an opportunity to educate the patient. Teeth that show signs of early demineralisation require no restorative intervention. Cavitated lesions warrant restoration. Non-restorative intervention can be done only by early diagnosis of caries.
Read And Learn More: Paediatric Dentistry Notes
The WHO (1987) criteria for caries diagnosis describe different stages of caries demineralisation before cavitation. These stages may not be reliably diagnosed. The stages of pre-cavitation are as follows:
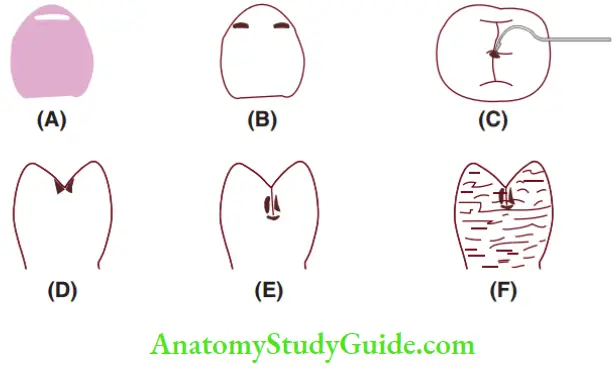 (A) Chalky white spot on incisor.
(A) Chalky white spot on incisor.- (B) Rough or brown spots.
- (C) Stained pit that catches the explorer.
- (D) Softening of enamel walls of pits/fissures.
- (E) Dark area around a buccal fissure showing decalcification.
- (F) Fluorotic enamel showing decalcification
- White or chalky spots
- Discoloured or rough spots
- Stained pits or fissures in the enamel that catch the explorer but do not have a detectably softened flor
- Undermined enamel or softening of the walls
- Dark, shiny, hard, pitted areas of enamel in a tooth showing signs of moderate decalcification
- Fluorotic enamel showing signs of decalcification
The WHO criteria describe the teeth with all these questionable lesions as ‘sound’, non-cavitated teeth.
A decayed or cavitated tooth is identified by the following:
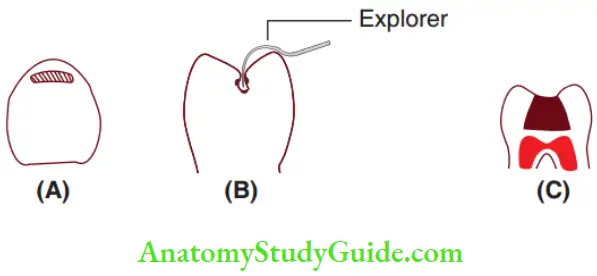
(A) Softened flor of enamel.
(B) Softened enamel at base and walls; allows entry of explorer.
(C) Deep decay with a temporary restoration.
- A lesion in a pit or fissure, or on a smooth surface, that has a detectably softened flor, undermined enamel or softened wall.
- A lesion that allows the entry of an explorer.
- A decay with a temporary filing is also included as restorative treatment is incomplete.
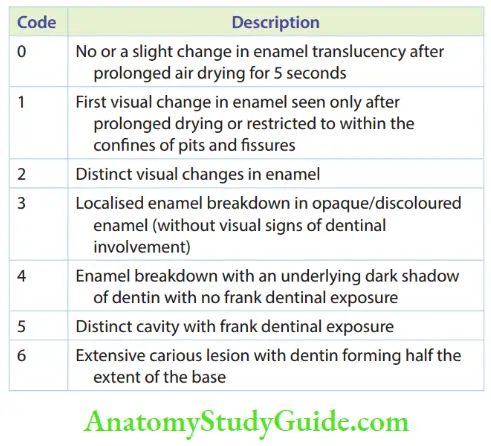
In 2007, the International Caries Detection and Assessment System (ICDAS) developed an evidence-based system to assess the severity stages of dental caries. It consists of seven categories from 0 to 6. The surface to be assessed should be a plaque-free tooth surface under both wet and dry conditions. The ICDAS codes are listed in Table.
Dental caries can be detected by conventional methods and recently developed, modern elaborate technical systems.
Conventional Modes Of Caries Detection
The methods of conventional modes of caries detection are as follows:

- Visual inspection
- Tactile inspection
- Radiography
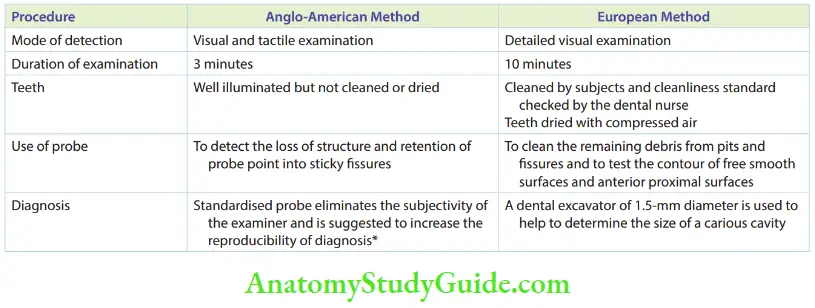
There are two fundamentally different systems of conventional modes of caries diagnosis, the Anglo-American system and the European system. The table elaborates on these methods. Both systems can be recorded with and without the use of radiographs.
- Visual Examination The visual examination of caries encompasses the detection of white spots and frank cavitation. Visual examination is best done under clean and dry conditions. A magnification loupe may be used as an aid in the process of visual examination. The loupes are comfortable to wear and freely available in various magnifications from various opticians. Teeth are cleaned and dried prior to diagnosis, as plaque and bubbles of saliva can obscure small cavities. White spot lesion is more obvious when teeth are dry because of the different refractive indices of enamel, water and air. The refractive index of enamel is 1.62, that of water is 1.33 and that of air is 1.0. When demineralised, the enamel becomes porous. If the teeth are wet, these pores are filled with water. When the enamel is dried, the water is replaced with air. The difference in the refractive indices between air and enamel (1.0 versus 1.62) is greater than that between water and enamel (1.33 versus 1.62). Hence, the lesion is more obvious when dried. The results may be quite unreliable when visual examination is the sole method of examination used.
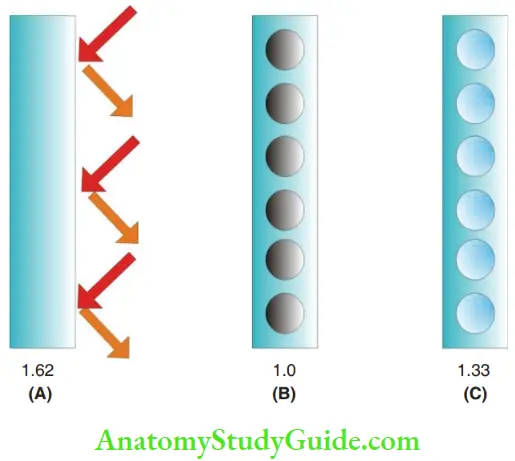 1. (A) Intact enamel,
1. (A) Intact enamel,
2. (B) porous enamel filed with air and
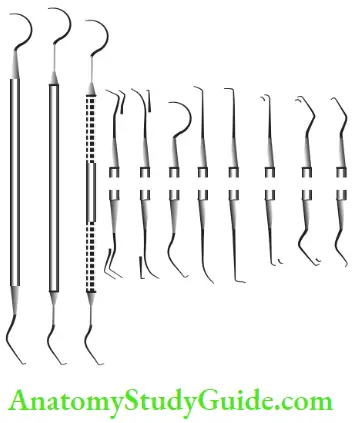
3. (C) pores in enamel filed with water. The numbers indicate the refractive indices. - Tactile Examination Tactile examination during a dental examination connotes to palpation in medical examination. The tactile examination is performed with handheld
instruments, especially explorers. The dental floss is useful in performing a tactile examination of proximal caries.- The different designs of explorers used for tactile examination are as follows:
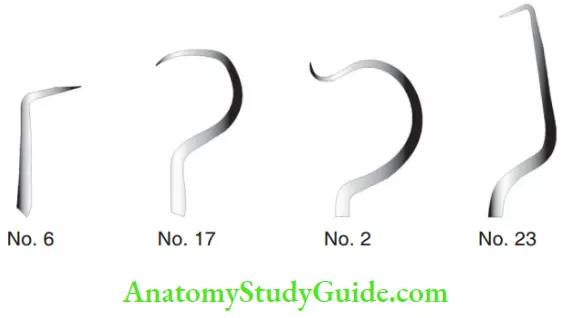
- Right angle probe (No. 6)
- Back action probe (No. 17)
- Shepherd’s Crook (No. 2)
- Cow horn with curved ends (No. 23)
- The different designs of explorers used for tactile examination are as follows:
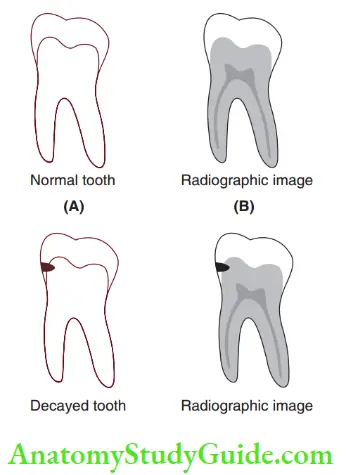
- Radiographs Radiography is primarily used for the detection of lesions on the proximal surfaces of teeth. These are not clinically visible for inspection. Radiographs are also recommended as a supplement to the clinical examination of occlusal surfaces for the detection of pit and fissure caries. Radiographic diagnosis of dental caries is fundamentally based on the fact that as the caries process proceeds, the mineral content of enamel and dentin decreases. This results in a decrease in the attenuation of the X-ray beam as it passes through the teeth. It is recorded on the image receptor as an increase in radiographic density. Hypomineralised structures allow more radiation to pass through, making the area look dark in the radiograph. This increase in radiographic density (darkness) must be detected by the clinician as a sign of a carious lesion. Different factors can affect the ability to detect these lesions accurately. They include exposure parameters, type of image receptor, image processing, display system, viewing conditions and ultimately the training and experience of the human observer.
Modern Techniques Of Caries Detection
Mechanised modes of caries detection have been used to enhance the efficiency of conventional modes of caries detection. Research on these techniques had begun in the 1980s and research findings have been more elaborate and conclusive for over a decade now. More recently, developed techniques aim to achieve the following:
- Enhance the accuracy of the diagnosis
- Detect early carious lesions that may probably be missed in conventional diagnosis. Hence, they are more sensitive
- Eliminate subjective bias. All the techniques have objective readings/findings
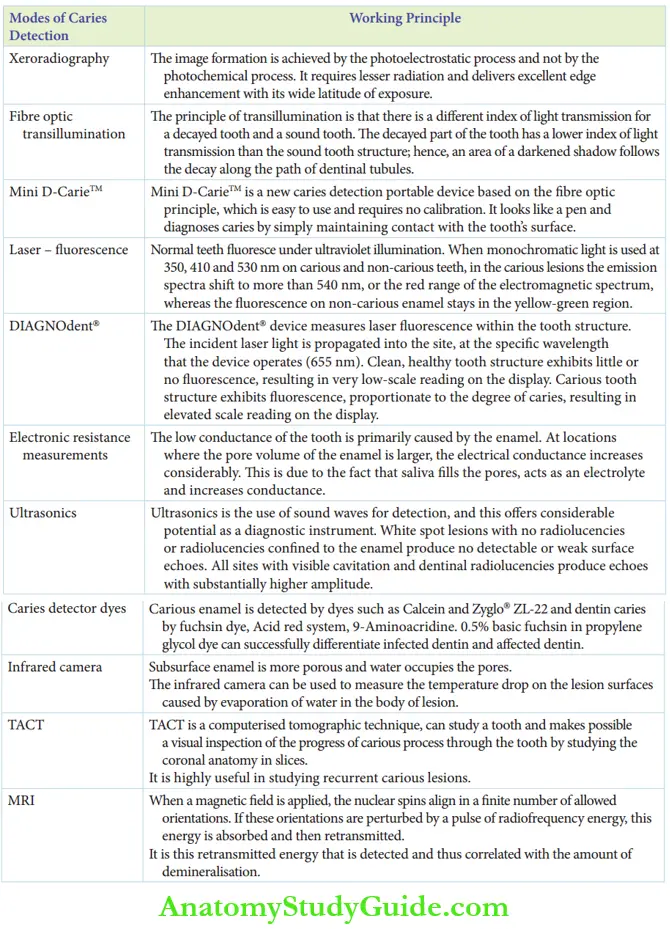
However, the conventional modes of diagnosis form the primary basis of caries examination till date. All the other modern/recent techniques are adjuvants, which may enhance relative convenience and diagnostic accuracy. They are not to be resorted as primary methods of caries detection and should always be associated with one or more conventional methods. The modern techniques of caries detection are as follows:
- Xeroradiography
- Fibre optic transillumination
- Mini D-Carie TM
- Laser – fluorescence
- Electronic resistance measurements
- Ultrasonics
- Caries detector dyes
- Infrared camera
- TACT
- Magnetic resonance microimaging
Dental Transillumination
- Xeroradiography was devised by Lothar S. Jeromin in 1980. In 1987, S. C. White demonstrated that the accuracy of xeroradiography was better than conventional radiography for diagnosing dental caries. It is a radiographic imaging process that uses the xerographic copying process to record images produced by diagnostic X-rays. It consists of a selenium plate inserted into a cassette, which is electrically charged. When radiation falls on this charged plate, an electrostatic charge image is formed. This image is processed by a liquid toner and fied onto a white plastic for viewing. The selenium plate can be washed and used again. This technique does not make use of the wet processing of the image receptor. The principal difference between xeroradiography and conventional radiography is that in xeroradiography, image formation is achieved by the photo electrostatic process and not by the photochemical process. It requires lesser radiation and demonstrates wide exposure. So, xeroradiography delivers better ‘edge enhancement’ than conventional radiography. Hence, it is distinctively better for caries detection than conventional radiography.
- Fibre Optic Transillumination In 1970, Friedman and Marcus suggested the use of fire optic transillumination (FOTI) in the detection of carious lesions. Fibre optics applied to transillumination of teeth and other oral structures is a useful technique for the detection of caries, calculus and soft tissue lesions. It permits a cold, high-intensity light source to be used anywhere in the oral cavity with ease and flexibility. The principle of transillumination is that there is a difference in the index of light transmission for a decayed tooth and a sound tooth. The decayed part of the tooth has a lower index of light transmission than the sound tooth structure. Hence, an area of a darkened shadow follows the decay along the path of dentinal tubules.
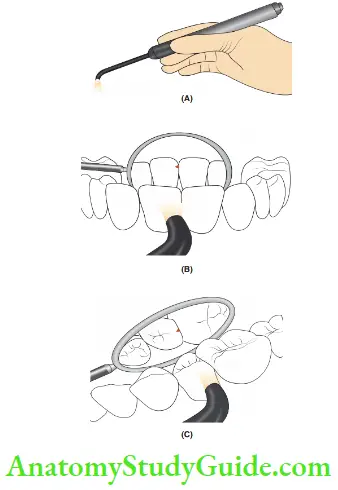
1. (A) FOTI probe emitting high-intensity light.
2. (B) FOTI probe used for caries detection in anterior teeth.
3. (C) FOTI probe used for caries detection in posterior teeth. - Mini D CarieTM is a new caries detection portable device manufactured by Neks Technologies, Montreal (Canada), in 2007. It is based on the fire optic principle. It is easy to use and requires no calibration. The device is a lightweight, pen-sized and cordless device that uses fire optic technology and light-emitting diodes (LEDs) to accurately detect both occlusal and interproximal caries, even when lesions are in their earliest stages. It diagnoses caries by simply maintaining contact with the tooth’s surface. The presence of both occlusal and interproximal caries is identified by two signals: audio and visual (green light turns to red). It is effective in a humid environment and does not essentially require a clean, dry environment.
Dental Transillumination
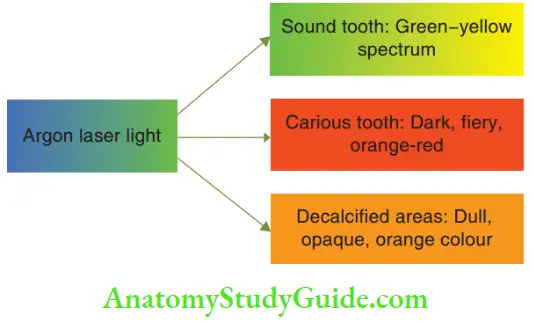
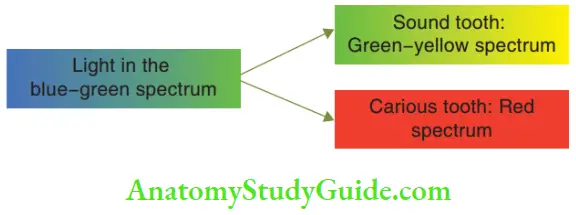
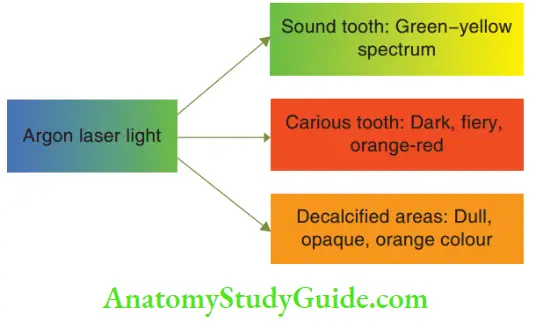
- Fluorescence Fluorescent light can be used to identify carious lesions as carious enamel and sound enamel transmit florescent light differently. Normal teeth fluoresce under ultraviolet illumination. If monochromatic light is used at 350-, 410- and 530-nm wavelengths on a carious lesion, the emission spectra shift to more than 540 nm. This is the red range of the electromagnetic spectrum. The fluorescence on non-carious enamel stays in the yellow-green region. Recently it has been found that when illuminated with argon laser light, the carious tissue has a clinical appearance of a dark, fiery, orange-red colour and can be easily differentiated from the sound tooth structure (green-yellow). Decalcifid areas appear as dull, opaque and orange colour regions.
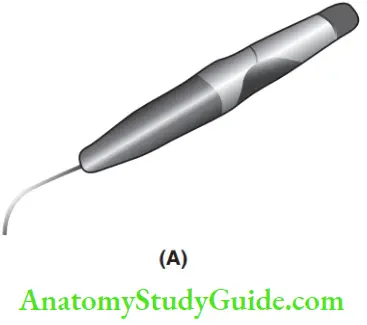
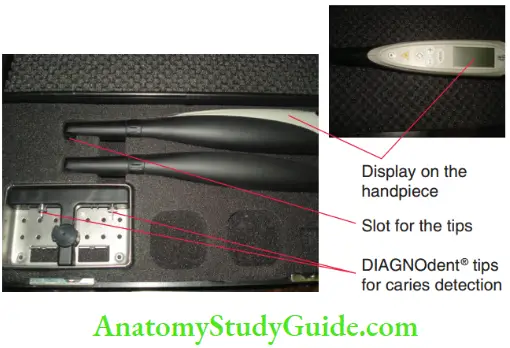
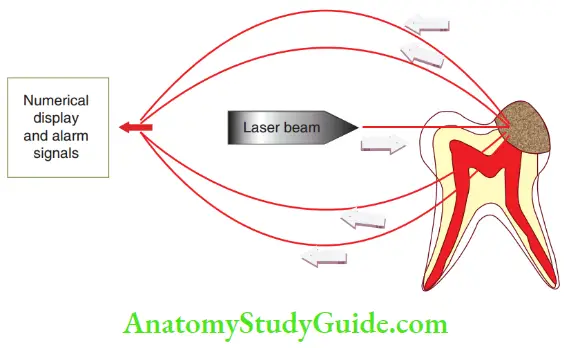
- Laser Fluorescence Caries Detection – Diagnodent Hibst et al. (2001) explored the use of laser immunofluorescence in caries detection. It became a highly sensitive methodology for the diagnosis of caries. DIAGNOdent from KaVo (Germany) is a chair-side, battery-powered, quantitative, diode laser-based florescent device. It is based on the principle of fluorescence generated by a laser light source. It can detect very small lesions with as high as 90% accuracy. The device is a pen-like probe. It has two types of fire optic tips: a tapered one (tip A) designed for fissure caries and a felt one (tip B) for smooth surface caries. It sends a safe, painless laser beam to the tooth. Simultaneously, it quantifies the reflected laser light energy and demonstrates a numeric display from 0 to 99 proportional to the reflected energy. The device delivers alarm signals when there are signs of hidden decay. The DIAGNOdent device measures laser florescence from the tooth structure. The incident laser light is propagated into the site, at the specific wavelength that the device operates (655 nm). Clean, healthy tooth structure exhibits little or no fluorescence, resulting in very low-scale readings on the display. Carious tooth structure exhibits fluorescence, proportionate to the degree of caries, showing elevated scale readings on the display. However, laser immunofluorescence measures demineralisation only. It can declare plaque laden in fissure also as caries. It lacks specificity.
- Electronic Resistance Measurements Electric resistance measurements (ERM) have been used for the detection of small caries lesions. They were first tried by Verdonschot et al. (1993). The low conductance of the tooth is primarily caused by the enamel. In areas where the pore volume of the enamel is larger, the electrical conductance increases considerably. This is due to the fact that saliva fills the pores, acts as an electrolyte and increases conductance. With increased conductance, electric transmission diffusivity is also higher. Since the conductance of the tooth and electric transmission diffsivity are inversely proportional to the resistance of the tooth, an increased conductance or decreased resistance is indicative of the presence of hypo and/or demineralisation. Hence, high electric transmission diffusivity is diagnostic of demineralisation or decay.
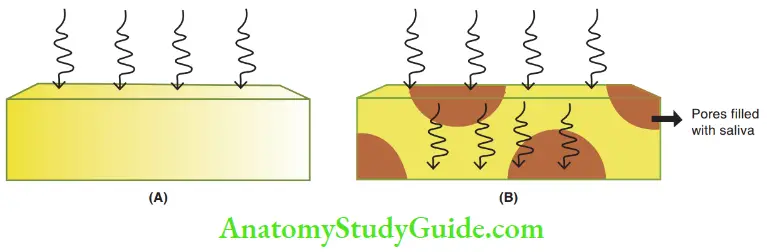 1. (A) Intact enamel with low conductance.
1. (A) Intact enamel with low conductance.
2. (B) Porous carious enamel with increased conductance.- Ultrasonic Equipment Ultrasonics is a considerable potential technology for diagnosing caries with sound waves. It is a mode of non-destructive testing. Caliskan et al. (2000) proved the efficacy and feasibility of caries detection with the ultrasonic system. An ultrasonic caries detector (UCD) system was proposed and evaluated by Matalon et al. (2007). The velocity of sound on the enamel surfaces has been found to be Vs = 3,143,121 m/s. White spot lesions with no cavitation or cavitation confined to enamel produce no detectable sounds or produce weak surface echoes. All sites with visible cavitation and dentinal radiolucencies produce echoes with substantially higher amplitude. The ultrasonic system is highly sensitive but with poor specificity.
- Dyes An object can be difficult to be distinguished from its background but the colour induced by a dye allows easy visualisation. Carious enamel is detected by dyes such as Calcein and Zyglo ZL-22. Dentin caries is detected by fuchsin dye, Acid red system and 9 Aminoacridine Dyes that help in the detection of carious enamel and dentin can also help to ensure complete removal of the same. However, considering the fact that infected dentin is best removed and affected dentin is best left behind (owing to its capacity to undergo remineralisation), a dye that can distinguish between infected and infected dentin would be more useful. 0.5% basic fuchsin in propylene glycol is one such dye for differentiating infected dentin from affected dentin.
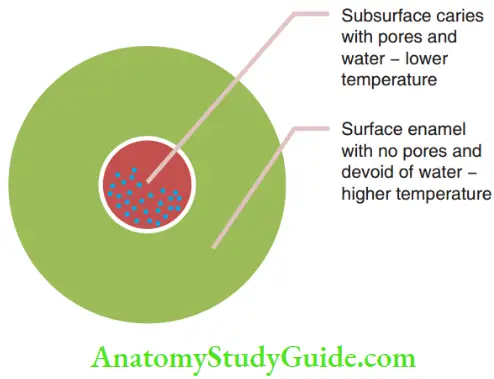
- Infrared Camera Matsuyama et al. (1998) used an infrared camera to detect subsurface lesions. It is well accepted that the subsurface enamel lesion has a distinctive degree of porosity and that water occupies the defect. Hence, there exists a discreet temperature difference between intact enamel and carious enamel. The temperature differences are visually discernible.
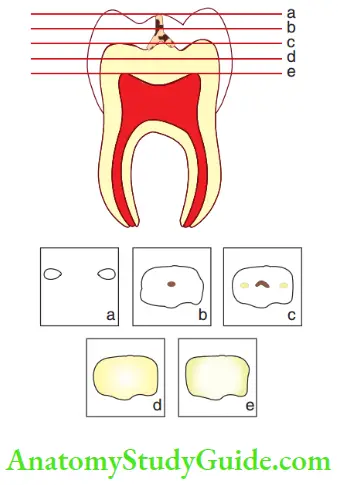
- Tuned Aperture Computed Tomography Tuned aperture computed tomography (TACT) is a computerised tomography technique that studies a tissue in various sections of varying slice thicknesses, as pre-set by the operator. It can be used to visually inspect the progress of the carious process through the tooth by studying the coronal anatomy in slices. Thus, an advantage of TACT is that a clinician can isolate and examine individual projections of a region, limiting intervention to the depth of decay. It is highly useful in studying recurrent carious lesions.
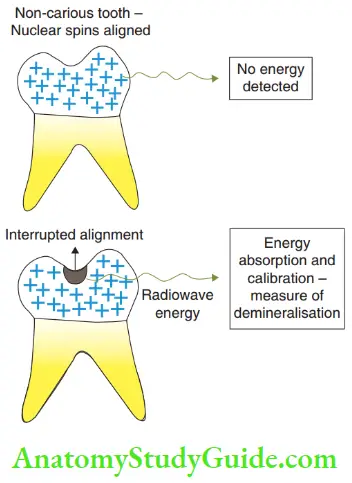
- Magnetic Resonance Micro-Imaging Magnetic resonance micro-imaging is a non-invasive and non-destructive technique of immense diagnostic value to study diseases of mineralised dental tissues. When a magnetic field is applied, the nuclear spins align in a finite number of allowed orientations. These orientations are perturbed by a pulse of radiofrequency energy, this energy is absorbed and then retransmitted. It is this retransmitted energy that is detected and thus correlated with the amount of demineralisation.
Modes Of Caries Removal
High-speed rotary instruments utilising diamond points are the most commonly used modes for the removal of carious and sound dental hard tissues. They are used at rotational speeds of 1.5–2 lakh rotations per minute. The turbine is driven by compressed air and the rotational force is transmitted to the diamond point through a handpiece with a rotary cartridge.
They are used to such an extent that high-speed rotary instruments have almost become synonymous with modes of caries removal. However, there are a few alternate modes of caries removal. They include the following:
- Excavation with hand instruments
- Slow-rotating air-motor equipment
- Air abrasion
- The chemomechanical caries removal system
- Excavation With Hand Instruments Children are highly anxious about being operated on with whistling rotary equipment spraying water. This anxiety is encountered more in pre-schoolers. Excavation is an efficient technique that fits the situation better. It primarily resorts before the use of rotary instruments. However, enamel caries cannot be excavated efficiently with hand instruments, thus necessitating rotary instruments. Dentinal lesions are open and relatively wide. These lesions are ideal candidates for excavation with hand instruments. Small, sharp spoon-shaped excavators are used for excavation. Blunt excavators do not incise dentin. Instead, they burnish it causing pain and discomfort to the child. Large excavators provide a poor convenience form, thereby making excavation inefficient. It can also lead to fracture of cusps undermined with caries.
- Slow-Rotating Air-Motor Equipment A slow-rotating air motor is used for technique sensitive situations involving the precise removal of caries. Removal of the remaining infected dentin at the flor in indirect pulp capping and removal of root caries are some indications. When caries removal lacks precision, it can probably cause pulp exposure. Air-motor instrumentation requires a copious water spray to prevent desiccation of dentin and pulpal injury.
- Micro-Abrasion Or Air Abrasion Micro-abrasion or air abrasion is an air abrasive system that uses a narrowly focused particle stream that abrades tooth structure in proportion to the particle size, air pressure and nozzle distance employed. It provides a more conservative means of removing pit and fissure caries than a bur or a diamond fistulotomy. It employs 27–37-nm aluminium oxide particles to abrade tooth structure when guided in a pressurised stream.
- Chemomechanical Caries Removal Chemomechanical caries removal systems were devised during the early 1970s. The first established chemomechanical system of caries removal was devised by Habib et al. in 1975. It was patented in the same year. The patent was released in 1987 after which it was marketed under the name C ar index. Chemomechanical modes of caries removal involve the use of certain chemical agents that potentiate/ augment mechanical removal. The chemicals that are used soften the disintegrated dentin (infected dentin). This softened dentin does not require the use of a high-speed rotary instrument for its removal. It can be excavated with hand instruments. The necessary hand instruments are sometimes provided with chemical agents by the manufacturer. These hand instruments are special in a way that they are designed to scrape dentin in two or more directions with very low friction levels. Chemomechanical systems displace the use of anaesthesia and drilling during cavity preparation. The initial chemomechanical caries removal reagent is Caridex. It eventually evolved into the Carisolv system. The established chemomechanical caries removal systems are as follows:
- N-monochloride-DL-2-aminobutyrate(NMAB system)
- Caridex
- Carisolv
- Papacarie
- N-monochloro-DL-2-aminobutyrate (NMAB system): Initially, sodium hypochlorite was studied if it could be used as a chemical agent to dissolve collagen. Owing to its corrosive nature, it was not taken further. A product was evolved by chlorination of glycine which was efficient in dissolving carious dentin. It was called the NMG system. The reagent was named GK-1019. Later, it was discovered that the reagent could be made more efficient by replacing glycine by amino butyric acid. This system was called NMAB. The system evolved into the Caridex system.
- Caridex system: This system is a twin-solution system – cardiac solution 1 and cardiac solution 2. The cardiac delivery system includes a pump, a heater, a solution reservoir and a handpiece to hold the applicator tip. The constitution, delivery mode, merits and demerits are described.
- Caridex solution 1
- Sodium hypochlorite
- Caridex solution 2
- Glycine, aminobutyric acid, sodium hydroxide, sodium chloride
- Basis/modus operandi
- Based on the softening effect of NMAB
- Delivery system
- Consists of a reservoir that stores the solution, a pump with a heater that warms the reagent to body temperature and pushes it through a tube, which is delivered through an applicator tip
- Delivery mode
- The two solutions are mixed together just before use; it forms a working reagent at a pH of 11 which is stable for 1 hour
- The solution is applied with an applicator tip which comes in various sizes/shapes
- Mechanical excavation
- The softened dentin is gently excavated by excavators and removed by aspiration
- It takes about 5–10 minutes to reach sound dentin in a moderate-sized cavity
- Merits
- Avoids painful removal of carious dentin
- Eliminates the requirement of anaesthetic administration
- Leaves sound dentin untouched
- Demerits
- It removes the carious dentin in its entirety, namely both the infected or turbid dentin as well as affected dentin
- It leaves a scaly surface with undercuts and overhangs that cannot be deciphered objectively if sound dentin is reached (no colour code for indication).
- Caridex solution 1
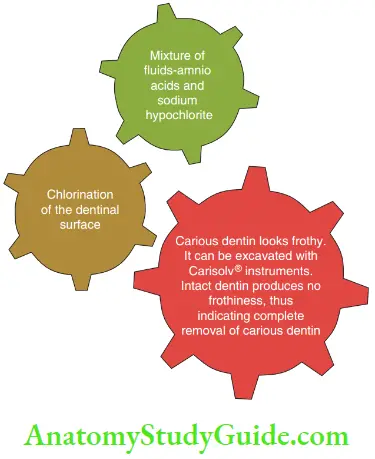
- Carisolv system: This is a twin-syringe gel system. One syringe contains a viscous gel, which is a mixture of three amino acids, and another syringe contains a transparent fluid consisting of low-concentration sodium hypochlorite. When the fluids are mixed, their caries-softening ability is released. The reaction between the mixture of amino acids and low-concentration sodium hypochlorite on the dentinal surface chlorinates dentin in 30 seconds. During chlorination, the following happens:
- The partially degraded collagen is further disintegrated by disruption of hydrogen bonding in its quaternary structure. The lesion looks frothy.
- The intact collagen (present in sound and affected dentin) is untouched.
- Thenufactures gives four instruments, which can excavate in two or more directions. The same procedure is repeated for three to four times till clear dentin is seen on the floor.
- When all infected dentin is removed, further addition of Carisolv produces no frothiness indicating that the removal is complete.
- The most appreciable advantage ofCarisolv system is that it cannot soften intact, sound and affected dentin. Hence, the caries removal leaves affected dentin behind (affected dentin has the capacity to remineralise).
- The most appreciable advantage ofCarisolv system is that it cannot soften intact, sound and affected dentin. Hence, the caries removal leaves affected dentin behind (affected dentin has the capacity to remineralise).
- Papacarie: It is a mix of papaya extracts. It is extensively used for softening meat in Indian kitchens. Papaya has the ability to soften tissues by denaturing altered collagen. It cannot disrupt intact collagen. The property of papaya has been put to use in caries excavation. Softened caries can then be scraped away using the Power DriveTM and/or the Carisolv hand instruments.
Summary
- Stages of pre-cavitation:
- White or chalky spots
- Discoloured or rough spots
- Stained pits or fissures in the enamel
- Undermined enamel or softening of the walls
- Dark, shiny, hard, pitted areas of the enamel
- Fluorotic enamel showing signs of decalcification
- Stages of cavitation:
-
- The softened floor of the enamel
- Softened enamel at the base and walls
- Deep decay with a temporary restoration
-
- Conventional modes of detection of dental caries
-
- Visual inspection
- Tactile inspection
- Radiography
-
- Modern modes of caries detection
- Modes of caries removal:
- High-speed rotary instruments: Uses diamond points and rotational speed of 1.5–2 lakh rpm. Children are anxious with such equipment, hence some alternate methods can be followed for caries removal.
- Excavation with hand instruments: Small, sharp, spoon-shaped excavators are best used. Enamel caries cannot be excavated efficiently with hand instruments. Dentinal, open, relatively wide lesions are ideal candidates for spoon excavation.
- Slow-rotating air-motor equipment: This technique is best used for the precise removal of caries, which when slightly overdone can cause pulp exposure or other undesired consequences.
- Air abrasion: It provides a more conservative means of removing pit and fissure caries. It employs 27–37-nm aluminium oxide particles that when guided in a pressurised stream abrade tooth structure.
- Chemomechanical caries removal system: Chemomechanical modes of caries removal involve the use of certain chemical agents that potentiate/augment the mechanical removal. The most appreciable advantage of chemomechanical systems is that they cannot soften intact sound and affected dentin. Hence, the caries removal leaves the affected dentin behind (which has the capacity to remineralise). The various systems are N-monochloro-DL-2-aminobutyrate, Caridex, Carisolv and Papacarie.
Leave a Reply