Diagnostic Procedures In Endodontics Notes
Diagnosis is defined as the utilization of scientific knowledge for identifying a diseased process and to differentiate from other disease processes. It is the procedure of accepting a patient, recognizing his/ her problem, finding the cause, and planning the treatment which would solve the problem.
Table of Contents
The diagnostic process in Endodontics actually consists of four steps:
- First step: Assemble all the available facts gathered from chief complaint, medical and dental history, diagnostic tests, and investigations.
- Second step:Analyze and interpret the assembled clues to reach the tentative or provisional diagnosis.
- Third step:Make differential diagnosis of all possible diseases which are consistent with signs, symptoms, and test results collected.
- Fourth step:Select the closest possible choice Th importance of making an accurate diagnosis cannot be overlooked. To avoid irrelevant information and to prevent errors of omission in clinical tests, the clinician should establish a routine for examination, consisting of chief complaint, past medical and dental history, and any other relevant information in the form of case history.
Read And Learn More: Endodontics Notes
Endodontics Case History
The purpose of the case history is to know whether the patient has any general or local condition that might alter the treatment plan.
Chief Complaint:
It consists of information which encourages the patient to visit a clinician. It should be noted in the patient’s own words. After recording the chief complaint, the history of the present illness is recorded. History tells the severity and urgency of the treatment.
Case History Symptoms:
Symptoms are defined as signs of deviation from the normal. Symptoms can be subjective and objective.
Endodontics Subjective Symptoms:
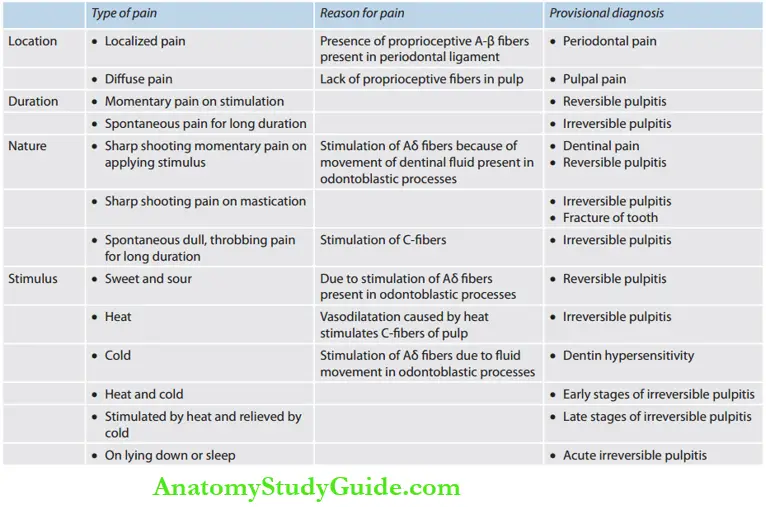
Subjective symptoms are perceived by the patient only and not evident to the examiner. The most common subjective symptom is pain. One should ask about following questions regarding pain:
- Quality: Dull, sharp, throbbing, constant
- Location: Localized, diffuse, referred, radiating
- Duration: Constant or intermittent lasting for seconds, minutes or hours
- Onset: Stimulation required, intermittent, spontaneous
- Initiated: Cold, heat, palpation, percussion
- Relieved: Cold, heat, any medications, sleep
If a chief complaint is a toothache but symptoms are too vague to establish a diagnosis, then analgesics should be prescribed to help the patient in tolerating the pain until the toothache localizes. A history of pain that persists without exacerbation may indicate a problem of nonodontogenic origins.
Pulpal pain can be sharp, piercing, and lancinating. It is due to stimulation of Aδ fiers. Dull, boring, excruciating, or throbbing pain occurs if there is stimulation ofC-fiers. Pulp vitality tests are usually done to reach the most probable diagnosis. If pain is from the periodontal ligament, the tooth will be sensitive to percussion, chewing, and palpation.
Localization of pain also tells the origin of pain since the pulp does not contain proprioceptive fiers; it is difficult for the patient to localize the pain unless it involves the periodontal ligament.
Endodontics Medical History:
There are no medical conditions which specifially contraindicate endodontic treatment, but there are several which require special care. Scully and Cawson have given a checklist of medical conditions which are needed to be taken special care.
Checklist for medical history (Scully and Cawson)
- Anemia
- Bleeding disorders
- Cardiorespiratory disorders
- Drug treatment and allergies
- Endocrine disease
- Fits and faints
- Gastrointestinal disorders
- Hospital admissions and attendance
- Infections
- Jaundice
- Kidney disease
- Likelihood of pregnancy or pregnant itself
If there is any doubt regarding the state of health of the patient, consult a medical practitioner before initiating endodontic treatment. Care should also be taken whether the patient is on medication such as corticosteroids or anticoagulant therapy.
According to the standards of the American Heart Association, patients should be given antibiotic prophylaxis if there is a high risk of developing bacterial endocarditis for example, in patients with prosthetic cardiac valves, history of infective endocarditis, cardiac transplant, congenital heart disease, etc.
Endodontics Objective Findings:
Subjective findings are obtained by questioning and performing tests on the basis of the patient’s symptoms. Following examination and tests should be performed by the clinician to get objective findings:
- Visual and tactile inspection
- Percussion test
- Palpation
- Periodontal examination
- Diffrential diagnosis
- Radiographs
- Pulp vitality tests
Visual and Tactile Inspection:
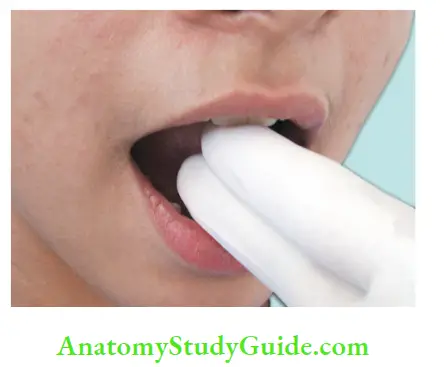
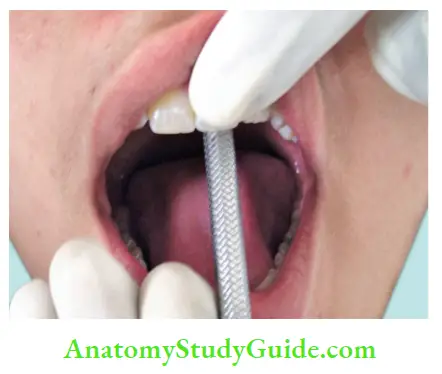
Before conducting an intraoral examination, check the degree of mouth opening. For a normal patient, it should be at least two figures. During an intraoral examination, look at the following structures systematically:
- Buccal, labial, and alveolar mucosa
- Hard and soft palate
- The floor of the mouth and tongue
- Retromolar region
- Posterior pharyngeal wall and faucial pillars
- Salivary glands
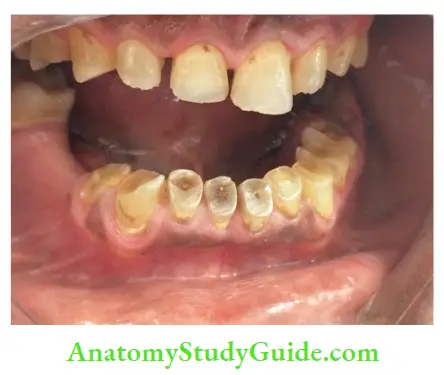
After examining this, the general dental state should be recorded, which include
- Oral hygiene status
- Amount and quality of restorative work
- Prevalence of caries
- Missing tooth
- Presence of soft or hard swelling
- Periodontal status
- Presence of any sinus tracts
- Discolored teeth
- Tooth wear and facets
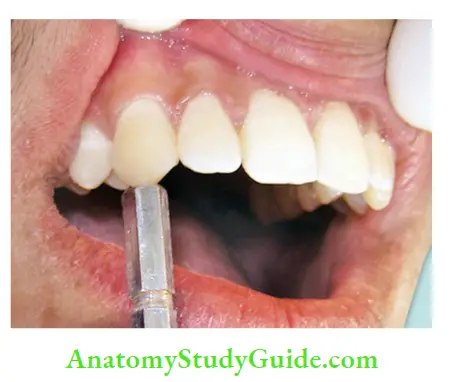
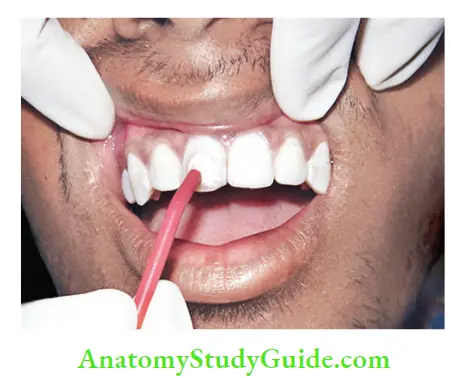
Percussion Test:
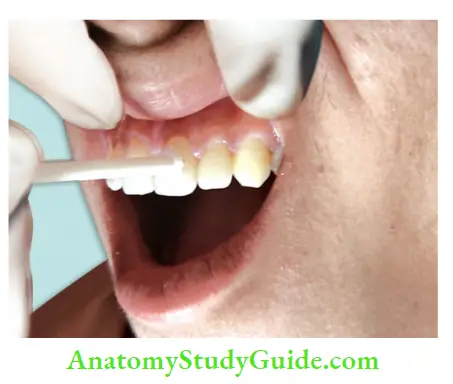
Percussion test helps to evaluate the status of periodontium surrounding a tooth. Pain on percussion indicates inflammation in the periodontal ligament which could be due to trauma, sinusitis, and/or periodontal (PDL) disease. Percussion can be carried out by gentle tapping with a gloved finger or the blunt handle of a mouth mirror.
Each tooth should be percussed on all the surfaces of the tooth until the patient is able to localize the tooth with pain.
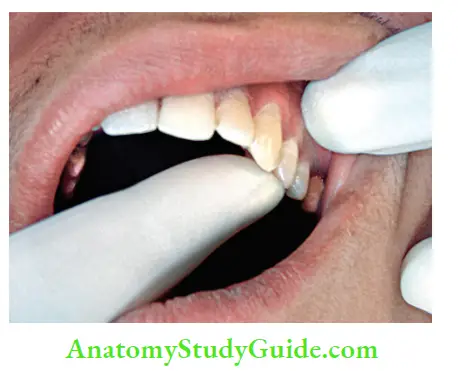
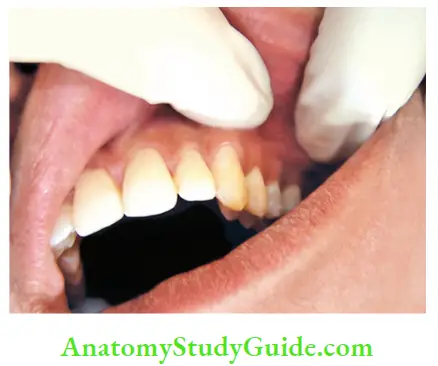
Palpation:
Palpation is done using digital pressure to check any tenderness in soft tissue overlying the suspected tooth. Sensitivity may indicate inflammation in periodontal tissues surrounding the affected tooth. Further palpation can tell any other information about fluctuation or fixation or induration of soft tissue, if any.
If any localized swelling is present, then look for:
- The local rise in temperature
- Tenderness
- Extent of lesion
- Induration
- Fixation to underlying tissues, etc.
Palpation Periodontal Examination:
It can be assessed from palpation, percussion, mobility of the tooth, and probing. The mobility of a tooth is tested by placing a finger or blunt end of the instrument on either side of the crown and pushing it and assessing any movement with other fingers.
Miller Tooth Mobility Index:
- Grade I: Distinguishable sign of tooth movement more than normal
- Grade II: Horizontal tooth movement not >1 mm
- Grade III: Movement of tooth >1 mm or when a tooth can be depressed.
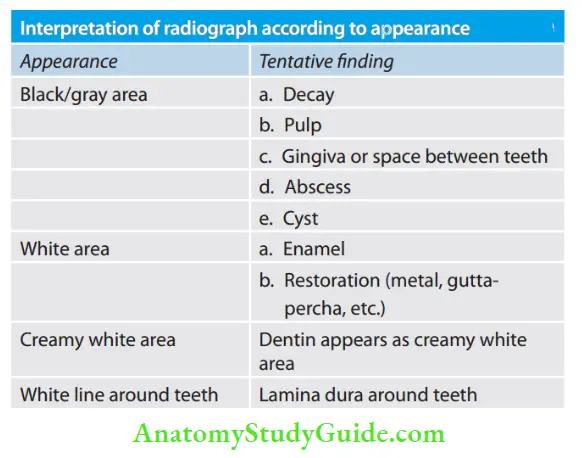
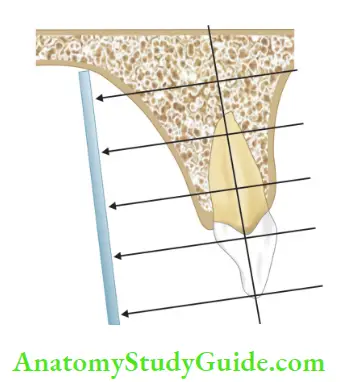
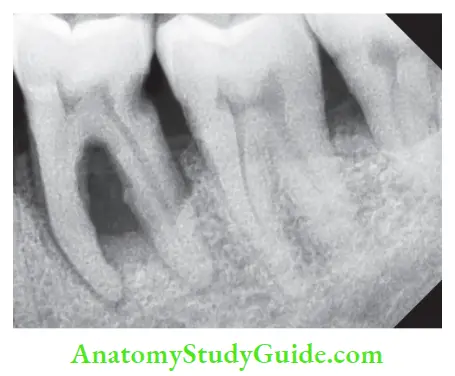
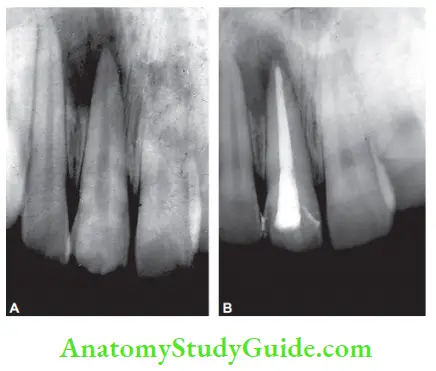
Palpation Radiograph:
A good radiograph helps in diagnosing and treatment planning. But it should be kept in mind that it is a two-dimensional picture of a three-dimensional object. Though it has many limitations, an appropriately taken and processed radiograph can give enough information to aid in diagnosis.
A perfect periapical radiograph must have adequate contrast with minimal processing error. It should include a minimum of 3 mm of the adjacent periapical area so as to have an accurate assessment of the target tooth.
Radiographs help us in the following ways:
- Establishing diagnosis
- Determining the prognosis of the tooth
- Disclosing the presence and extent of caries
- Check the thickness of the periodontal ligament
- To see the continuity of lamina dura
- To look for any periodontal lesion associated with tooth
- To see the number, shape, length, and pattern of the root canals
- To check any obstructions present in the pulp space
- To check any previous root canal treatment if done
- To look for the presence of any intraarticular pins or posts
- To see the quality of previous root canal filling
- To see any resorption present in the tooth
- To check the presence of calcification in pulp space
- To see root-end proximal structures
- Help in determining the working length, length of the master gutta-percha cone, and quality of obturation
- During the course of treatment, radiographs help in knowing the level of instrumental errors like perforation, ledging, and instrumental separation
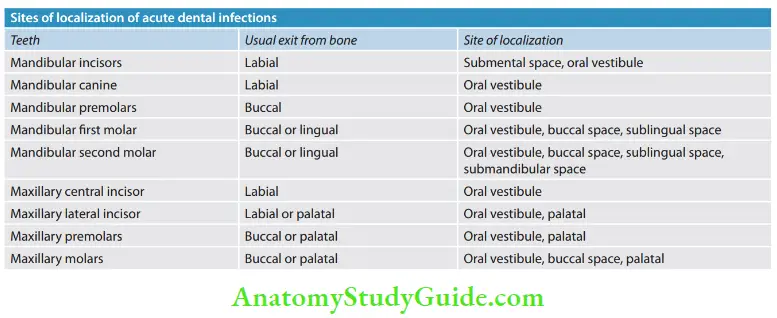
Characteristic features of periapical lesions of endodontic origin :
- Loss of lamina dura in the apical region
- Apparent etiology of pulpal necrosis
- Radiolucency remains at the apex even if the radiograph is taken by changing the angle
The following lesions should be differentiated from the lesions of endodontic origin while interpreting radiographs:
- Periodontal abscess
- Idiopathic osteosclerosis
- Cementomas
- Giant cell lesions
- Cysts
- Tumors.
Pulp Vitality Tests
Pulp Vitality Testing is often referred to as vitality testing. Pulp vitality tests play an important role in diagnosis because these tests not only determine the vitality of tooth but also the pathological status of pulp.
Objectives of Pulp Testing:
- To assess health of pulp based on its qualitative sensory response prior to restorative, endodontic procedures
- To differentially diagnose periapical pathologies of pulpal or periodontal origin
- To assess status of the pulp as a follow-up after trauma to teeth
- To check status of the tooth especially one that has past history of pulp capping or deep restoration
- To diagnose oral pain whether it is of pulpal or periodontal origin or because of other reason
Various types of pulp tests performed are:
- Thermal test
- Cold test
- Heat test
- Electrical pulp testing
- Test cavity
- Anesthesia testing
- Bite test
Most commonly used vitality testers evaluate the integrity of Aδ fiers by applying stimulus to the outer surface of the tooth surface. A positive response means functional nerve fiers but does not indicate status of blood supply.
Pulp Vitality Testing – Thermal Test:
In the thermal test, the response of pulp to heat and cold is noted. The basic principle for pulp to respond to thermal stimuli is that the patient reports sensation, but it disappears immediately. Any other type of response, that is, painful sensation even after the removal of stimulus or no response is considered abnormal.
Pulp Vitality Testing Cold test:
It is the most commonly used test for assessing the vitality of pulp. Cold causes contraction of dentinal tubules resulting in outward flow of fluid from tubules and thereby pain. This test is used to differentiate reversible and irreversible pulpitis.
If pain persists after removal of cold stimuli, it is irreversible pulpitis, but if pain disappears on removal of stimulus, it is reversible pulpitis. Cold test is more reliable than heat test.
Cold testing can be done in a number of ways.
- Wrap an ice piece in the wet gauge and apply to the tooth. Ice sticks can be prepared by filing the discarded anesthetic carpules with water and placing them in the refrigerator
- Spray with cold air directed against the isolated tooth
- Use of ethyl chloride (boiling point −41°C) in the form of
- Cotton pellet saturated with ethyl chloride
- A spray of ethyl chloride: After isolation of tooth with a rubber dam, ethyl chloride spray is employed.
- The ethyl chloride evaporates so rapidly that it absorbs heat and thus cools the tooth
- Frozen carbon dioxide (dry ice) is available in the form of a solid stick which is applied to the facial surface of the tooth. The advantage of using dry ice is that it can penetrate.
Pulp Vitality Tests Clinical Tips:
Use of a rubber dam is especially recommended when performing the test using the ice sticks because melting ice will run onto adjacent teeth and gingivae resulting in a false-positive result
While performing the cold test, one should begin with the posterior tooth and then move toward the anterior teeth. It will prevent melted ice water from dripping in a posterior direction, thus giving false results
Pulp Vitality Testing Heat test:
It is most advantageous in the condition where the patient’s chief complaint is intense dental pain upon contact with any hot object or liquid. The preferred temperature for the heat test is 150°F (65.5°C).
Different methods used for heat tests are:
- Direct warm air to the exposed surface of the tooth and note the patient’s response
- Apply heat to the gutta-percha stick. The tooth is coated with a lubricant such as petroleum jelly to prevent gutta-percha from adhering to the tooth surface.
- The heated gutta-percha is applied at the junction of the cervical and middle third of the facial surface of the tooth. Guttapercha softens at 65°C and can deliver up to 150°C.
- The disadvantage of using a gutta-percha stick is that because of high-temperature pulpal damage can occur.
- Heat test should not be done for >5 s because prolonged heat application causes biphasic stimulation of Aδ fiers followed by C fiers, which can result in persistent pain full coverage restoration and can elicit a pulpal reaction to the cold because of its very low temperature (−78°C)
- Dichlorodifluoromethane (Freon) (−21°C) and 1,1,1,2- tetrafluoromethane (−15 to−26°C) are also used as cold testing material.
- Application of hot burnisher, hot compound, or any other heated instrument
- Use of frictional heat produced by rotating polishing rubber disk against the tooth surface
- Use of warm water from a syringe on a rubber dam isolated tooth
- The use of a laser beam (Nd: YAG laser) is done to stimulate pulp.
Electric Pulp Testing:
- Electric pulp tester stimulates Aδ nerve fiers by applying electrical current. Pain occurs because of an ionic shift in the dentinal fluid resulting in depolarization of Aδ fiers.
- Pulp testers are battery-operated or available with cords which plugs into electric outlets for a power source.
- It acts by generating pulsatile electrical stimuli and stimulation of Aδ nerve fiers.
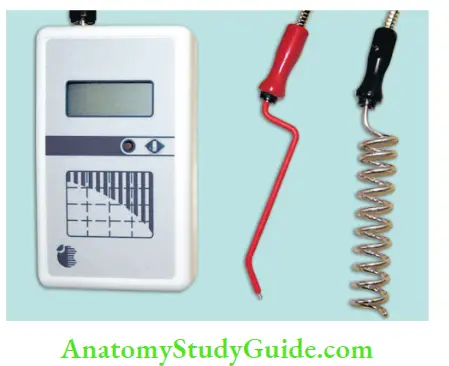
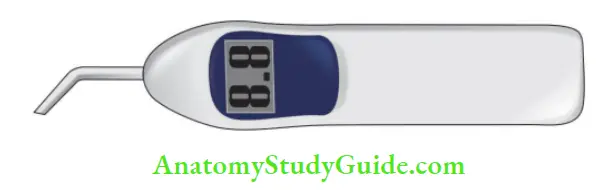
Electric Pulp Testing Procedure:
- Before starting the procedure, the patient must be explained about the method to reduce anxiety.
- Isolate the teeth to avoid any type of false-positive response. This can be done by use of an interproximal plastic strip, drying tooth surface, and rubber dam application.
- Apply an electrolyte on the tooth electrode and place it on the facial surface of the tooth. Commonly used electrolytes are Nichollas-colloidal graphite and Grossman toothpaste. To have a fast response, electrodes should be applied at the area of high neural density like incisal one-third of anterior teeth (it’s close to pulp horns) and middle third of posterior teeth.
- Precaution should be taken to avoid it contacting adjacent gingival tissue or metallic restorations to avoid a false-positive response
- Confirm the complete circuit from the electrode through the tooth to the body of the patient and then back to the electrode. If gloves are not used, the circuit gets completed when the clinician finger contact with the electrode and the patient’s cheeks. But with gloved hands, it can be done by placing patient’s finger on metal electrode handle or by clipping a ground attachment onto the patient’s lip
- Once the circuit is complete, slowly increase the current and ask the patient to point out when the sensation occurs
- Each tooth should be tested two to three times, and the average reading is noted. If the vitality of a tooth is in question, the pulp tester should be used on the adjacent teeth and the contralateral tooth, as a control
Disadvantages of Electric Pulp Testing
- False-positive response in
- Teeth with acute alveolar abscess because gaseous or liquefied products within the pulp canal can transmit electric current
- The electrode may contact gingival tissue, thus giving the false-positive response
- In multirooted teeth, pulp may be vital in one or more root canals and necrosed in others, thus eliciting a false positive response
- False-negative response in
- Recently traumatized tooth
- Recently erupted teeth with immature apex
- Patients with high pain threshold
- Calcified canals
- Poor battery or electrical deficiency in plug-in pulp testers
- Teeth with extensive restorations or pulp-protecting bases under restorations
- Patients are premedicated with analgesics or tranquilizers, etc.
- Partial necrosis of pulp sometimes is indicated as total necrosis by an electric pulp tester
Test Cavity:
This method should be used only when all other test methods are inconclusive in results. Here a test cavity is made with high-speed number one or two round burs with appropriate air and water coolant. The patient is not anesthetized while performing this test. The patient is asked to respond if any painful sensation occurs during drilling.
The sensitivity or pain felt by the patient indicates pulp vitality. Here, the procedure is terminated by restoring the prepared cavity. If no pain is felt, cavity preparation may be continued until the pulp chamber is reached, and later on endodontic therapy may be carried out.
Anesthesia Testing:
It is indicated when the patient can’t differentiate whether pain is in the mandibular or maxillary arch. The main objective of this test is to anesthetize a single tooth at a time until the pain is eliminated. It should be accomplished by using intraligamentary injection. The injection is administered to the most posterior tooth in the suspected quadrant.
If the pain persists, even after the tooth has been fully anesthetized, then repeat the procedure to the next tooth mesial to it. It is continued until the pain disappears. If the source of the pain cannot be determined, repeat the same technique on the opposite arch. This test has an advantage over the test cavity because it later results in iatrogenic damage.
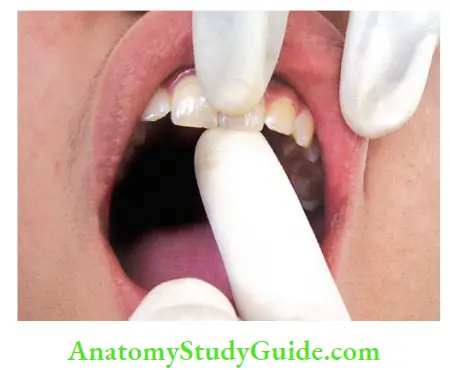
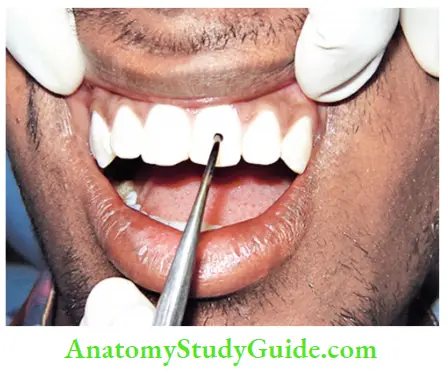
Bite Test:
A bite test helps in identifying a cracked or fractured tooth. This is done if the patient complains of pain on mastication. The tooth is sensitive to biting if pulpal necrosis has extended to the periodontal ligament space or if a crack is present in a tooth. In this, the patient is asked to bite on a hard object such as a cotton swab, toothpick, or orange wood stick with the suspected tooth and the contralateral tooth.
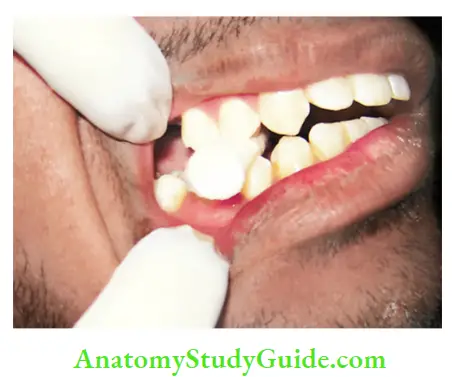
Tooth slooth is another commercially available device for bite tests. It has a small concave area on its top which is placed in contact with the cusp to be tested. Pain present on biting indicates apical periodontitis, and pain present on the release of biting force indicates a cracked tooth.
Recent Advances In Pulp Vitality Testing
Assessment of pulp vitality is a crucial diagnostic procedure in dental practice. Commonly used methods (thermal, electrical, or direct dentine stimulation) rely on stimulation of Aδ nerve fiers and give no direct indication of blood flow within the pulp. These tests can give false-positive and negative results.
Moreover, being subjective tests, the result depends on the patient’s perceived response to the stimulus and the dentist’s interpretation of that response. Recent studies have shown that blood circulation is the most accurate determinant in assessing pulp vitality as it provides an objective differentiation between necrotic and vital pulp tissue.
Recently Available Pulp Vitality Tests
- Laser Doppler flowmetry (LDF)
- Pulp oximetry
- Dual wavelength spectrophotometry (DWLS)
- Measurement of temperature of tooth surface
- Transillumination with a fiber-optic light
- Plethysmography
- Detection of interleukin-1 (IL-1)β
- Xenon-133
- Hughes Probeye camera
- Gas desaturation
- Radiolabeled microspheres
- Electromagnetic flowmetry
Laser Doppler Flowmetry:
LDF was first described by Gazelius in 1986. The technique depends on the Doppler principle in which a low-power light from a monochromatic laser beam of known wavelength along a fiber-optic cable is directed to the tooth surface. As light enters the tissue, it is scattered and adsorbed by stationary and moving tissues.
Photons that contact with moving red blood cells are scattered and shifted, and photon that interacts with stationary tissues is scattered but not shifted. Part of the light is returned back to the photon detector and a signal is produced. Since RBCs represent the main moving entity in the pulp, Doppler-shifted light is inferred as an index of pulpal blood flow.
Blood flow measured by laser Doppler technique is termed “flux,” which is proportional to the product of the average speed of blood cells and their concentration.
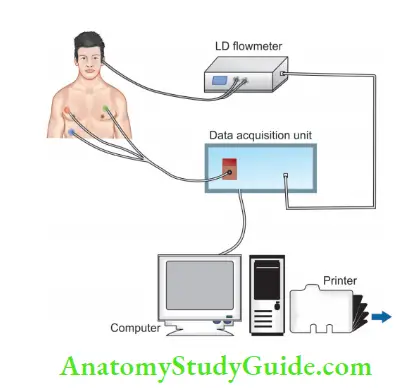
Pulp is a highly vascular tissue, and cardiac cycle blood flow in the supplying artery is transmitted as pulsations. These pulsations are apparent on the laser Doppler monitor of vital teeth and are absent in nonvital teeth.
Blood flux level in vital teeth is much higher than for nonvital teeth. Currently, available flowmeters display the signal on a screen, from which the clinician can interpret whether the pulp is vital or nonvital.
Laser Doppler Flowmetry Advantages
- An objective test
- Accurate to check the vitality
Laser Doppler Flowmetry Disadvantages
- Cannot be used in patients who cannot refrain from moving or if the tooth to be tested cannot be stabilized
- Medications used in cardiovascular diseases can affect the blood flow to the pulp
- Requires higher technical skills to achieve
- The use of nicotine affects blood flow to the pulp
- Expensive
Pulse Oximetry:
A pulse oximeter is a noninvasive oxygen saturation monitor widely used in medical practice for recording blood oxygen saturation levels during intravenous anesthesia. It was introduced in Aoyagi in the 1970s. The principle of this technique is based on a modification of Beer’s law. It tells the absorption of light by a solute to its concentration and optical properties at a given wavelength.
The pulse oximeter sensor consists of two light-emitting diodes, one to transmit red light (wavelength approximately 660 nm), the other to transmit infrared light (wavelength 850 nm), and a photodetector on the opposite side of the vascular bed.
When LED transmits light through the vascular bed, different amount of light is absorbed by oxygenated and deoxygenated hemoglobin. Pulsatile change in blood volume causes a change in the amount of light absorbed by the vascular bed. This change is analyzed in a pulse oximeter to evaluate the saturation of arterial blood.
Pulse Oximetry Advantages
- An effective and objective method to evaluate pulp vitality
- Useful in cases of traumatic injuries where the blood supply remains intact but the nerve supply is damaged
- Can detect pulpal circulation independent of gingival circulation
- Easy to reproduce pulp pulse readings
Pulse Oximetry Disadvantages
- If arterial pulsatile blood flow is low, readings can’t be obtained. For example, in peripheral vasoconstriction, hypovolemia, and hypothermia cases
- Background absorption associated with venous blood
- False-negative results in the cases of coronal calcification where the radicular pulp is vital
- Low specificity in the cases of deep restorations or traumatic injuries
Dual Wavelength Spectrophotometry:
DWLS is a method independent of pulsatile circulation. The presence of arterioles rather than arteries in the pulp and its rigid encapsulation by surrounding dentine and enamel make it difficult to detect a pulse in the pulp space. This method measures oxygenation changes in the capillary bed rather than arteries.
Advantages of DWLS:
- In the case of avulsed and replanted teeth with open apices where the blood supply is regained within the first 20 days, the nerve supply takes time. Repeated readings for 40 days in such teeth reveal the healing process
- It uses visible light which is filtered and guided to the tooth by faster optics
- Noninvasive objective test
- The instrument is small, portable, and inexpensive
Measurement of Surface Temperature of Tooth:
This method is based on the assumption that if the pulp becomes nonvital, the tooth no longer has an internal blood supply, and thus should exhibit a lower surface temperature than that of its vital counterparts.
Fanibunda in 1985 showed that it is possible to differentiate vital and nonvital teeth by means of crown surface temperature. He used a thermistor unit consisting of two matched thermistors connected back to back, one measuring the surface temperature of the crown (measuring thermistor) while the other acting as a reference thermistor.
Tooth to be tested was dried with gauze, and the thermistor unit was positioned so that the measuring thermistor contacted the center of the buccal surface of the crown. The reference thermistor was suspended in air, close to it, but not touching either the measuring thermistor or the enamel surface.
Equilibrium was then achieved between the temperatures of the thermistors, crown surface, and immediate environment by holding the measuring unit in the described position until a steady state was established for ≥20 s. Stimulation of the crown surface was carried out by means of a rubber-polishing cup fitted to a dental contra-angle handpiece. The recordings were continued for a period of time following the stimulation period.
It was found that a difference was obtained between the critical period for vital and nonvital teeth, and the difference corresponded with a specific temperature change.
Transillumination with Fiber-Optic Light:
In this, light is passed through fine glass or plastic fiers by a process known as total internal reflection. A nonvital tooth which is not discolored may show a difference in translucency when a shadow produced on a mirror is compared to that of adjacent vital teeth.
Detection of Interleukin-1β in Human Periapical Lesion:
The inflammatory periapical lesions are common sequelae of the infected pulp tissue. These areas contain PMN leukocytes, T and B lymphocytes, macrophages, plasma cells, etc. These inflammatory cells produce IL-1, which acts as a mediator of various immunologic and inflammatory responses.
This lymphocyte-activating factor IL-1 is responsible for osteoclast activation which results in bone resorption which is frequently a feature of inflammatory response.
Plethysmography:
In this, an analysis of the optical properties of selected tissue is done. It was introduced as a modification of pulp oximetry by adding light of a shorter wavelength.
Role of Ultrasound:
Images produced by ultrasound are three-dimensional and have high resolution. It does not expose patients to any radiation. It uses sound waves with frequency outside the audible range. Since different biological tissues have different acoustic and mechanical properties, ultrasound waves at the edge of two tissues of different acoustic impedance undergo reflection and refraction.
Ultrasound wave which is reflected back from the tissues appears as an echo. In a healthy state, alveolar bone appears as white(total reflection), and the roots of teeth appear whiter (hyperechoic). A flid-filed cavity appears dark (hypoechoic). The degree of reflection depends on the clarity of the fluid (hypoechoic).
Ultrasound can complement conventional radiographs since it can differentiate between cystic and non-cystic lesions.
Fiber-Optic Fluorescent Spectrometry:
In this, ultraviolet light is projected toward dental tissues to produce fluorescence. Teeth with vital pulps fluoresce normally, but the teeth with necrotic nonvital pulp don’t fluoresce when exposed to ultraviolet light.
Differences in the inflorescence is due to the loss of mineralized tissue components and increased organic presence and water in various when compared to healthy dentin.
Cholesteric Liquid Crystals:
Cholesteric crystals are “liquid” crystals which are easily affected by changes in temperature or pressure because of their fluidity. These crystals are thermochromic (the color of crystals varies with change in pressure or temperature). Howell et al. and Lexington found when applied to the tooth surface, crystals showed color change when compared with adjacent or contralateral teeth.
This principle is used to detect pulp vitality because the vital pulp has a higher tooth-surface temperature due to the presence of vascular supply when compared with nonvital teeth that had no blood supply.
Ultrasound Doppler or Color Power Doppler:
Color Power Doppler flowmetry detects the presence and direction of the blood flow within the tissue. The intensity of the Doppler signal is shown by changes on the graph (Doppler). Positive Doppler shift (shown in red) is caused by blood moving toward the transducer, and negative Doppler shift (shown in blue) is caused by blood moving in the opposite direction.
In vital teeth, Doppler tells a “pulsating” waveform and sound characteristic, and nonvital teeth show linear nonpulsed waveform without pulsating sound.
Thermographic Imaging:
In this, a color image is produced due to changes in temperature in both superficial and deep areas. In 1989, Pogrel et al. found that Hughes Probeye 4300 Thermal Video System was sensitive to measure even 0.1°C of temperature differences. However, nowadays less cumbersome and easier methods are available to replace this.
Diffrential Diagnosis:
Differential diagnosis is distinguishing a particular disease from others that present similar clinical features. After differential diagnosis, to reach at a definitive diagnosis, the clinician should get investigations done like laboratory investigations, radiographs, and pulp vitality tests.
Diagnostic Perplexities:
There are certain conditions in which it is difficult to reach a proper diagnosis even after detailed history and examination. These conditions can be
- Idiopathic tooth resorption
- Treatment failures
- Cracked tooth syndrome
- Persistent discomfort
- Unusual radiographic appearances
- Paresthesia
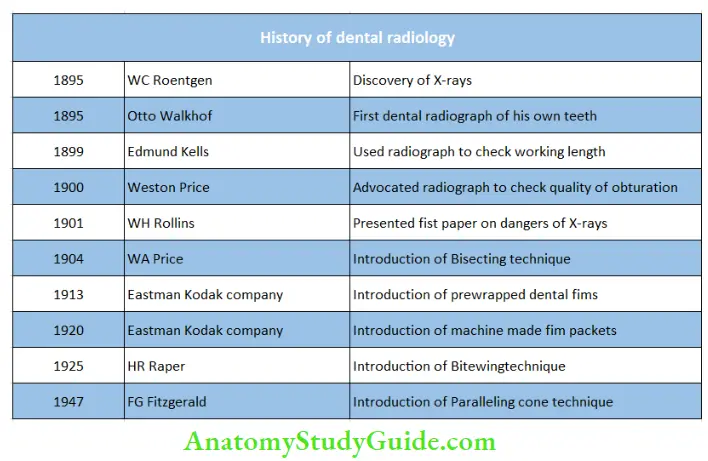
Role Of Radiographs In Endodontics
Radiographs play an important role in the diagnosis of endodontic problems. The clinician should be familiar with normal radiographic landmarks.
It should be kept in mind that radiographs should be of good quality because a poor-quality radiograph not only fails to yield diagnostic information but also causes unnecessary radiation to the patient.
In order to decrease radiation exposure, one should
The use of faster F-speed fim reduces exposure by 25% compared to E-speed film and 60% compared to D-speed fim
- Use rectangular collimation instead of the round collimator
- Use thyroid collar and lead apron
- Use of aluminum filters
- Use digital radiographic techniques
- Use electronic apex locator in endodontic treatment

Types of Radiographs
- Intraoral
- Intraoral periapical
- Occlusal
- Bitewing
- Extraoral
- Panoramic
- Lateral cephalograms
- Tomograms
- Computed tomography
Intraoral Periapical Radiographs:
Intraoral Periapical (IOPA) radiographs are used to detect any abnormalities in relation to roots and surrounding bone structures.
Techniques for exposing teeth:
- Bisecting Angle Technique
- Here, an X-ray beam is directed perpendicular to an imaginary plane which bisects the angle formed by the recording the plane of the X-ray film and the long axis of the tooth.
- Bisecting Angle Technique Advantages:
- Can be performed without using film holders
- More comfortable because the film is placed at an angle to the long axis of teeth, so it doesn’t impinge soft tissues
- Anatomical structures do not pose many problems because of angulated film placement
- Quick and comfortable for the patient when the rubber dam is in place
- Bisecting Angle Technique Disadvantages:
- Cone cutting
- Image distortion
- Since a film holder is not used, it’s difficult to visualize where the X-ray beam should be directed
- Superimposition of anatomical structures
- Diffilty to reproducing the periapical films
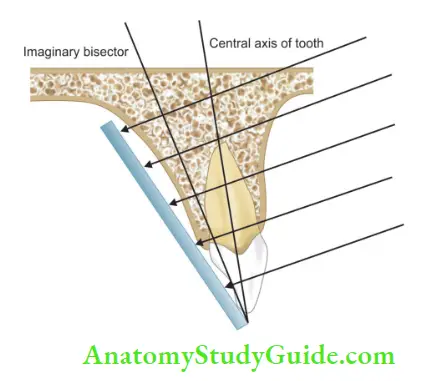
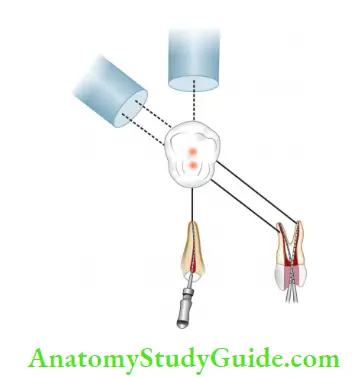
- Paralleling Technique:
Here X-ray film is placed parallel to the long axis of the tooth to be exposed, and the X-ray beam is directed perpendicular to the film. If the film is kept in an upright position, the patient won’t be able to close on the bite block, and the film will not be parallel. To aid fim placement, the film is tipped to 20° beyond parallel.
Since the palate and floor of the mouth are shallow, the film should be placed away from the teeth to achieve parallelism. If fim is placed at a distance, it results in an increase in magnification (size) but decreases in sharpness. To compensate it, the firm target distance should be increased. For this, Walton gave a modified paralleling technique in which the central beam is oriented perpendicular to the radiographic film but not to the teeth.
The modified paralleling technique covers the disadvantages of the paralleling technique.
- Paralleling Technique Advantages:
- Better accuracy of image
- A reduced dose of radiation
- Reproducibility
- Because of the paralleling the instrument with the aiming ring, the X-ray beam is easy to align irrespective of the position of head
- Better images of bone margins, interproximal regions, and maxillary molar region
- When using a paralleling instrument with an aiming ring, the alignment of the X-ray beam is simplified
- Paralleling Technique Disadvantages:
- Since fim is more upright in paralleling technique, it impinges more on the floor of the mouth or palate so more uncomfortable
- Difficult to use in patients with Shallow vault
- Gag reflex
- When the rubber dam is in place
- Extremely long roots
- Uncooperative patients
- Tori
Indications of IOPA Radiograph:
- To see apical inflammation
- Check periodontal status
- Check alveolar bone
- See unerupted teeth
- Check the status of a tooth after trauma
- During and after endodontic treatment
- Evaluation of implants postoperatively
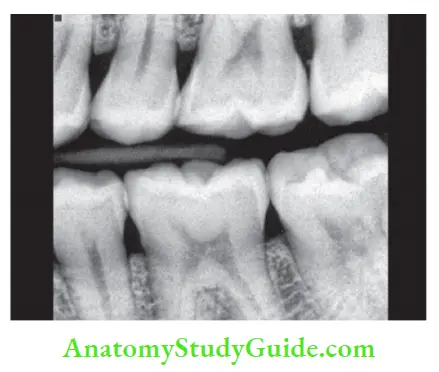
Bitewing Radiographs:
Bitewing radiographs include the crowns of maxillary and mandibular teeth and alveolar crest in the same film
Bitewing Radiographs Advantages:
- Helps in detecting interproximal caries
- Evaluate periodontal conditions
- Evaluate secondary caries under restorations
- Help in assessing alveolar bone crest and changes in bone height by comparing it with adjacent teeth
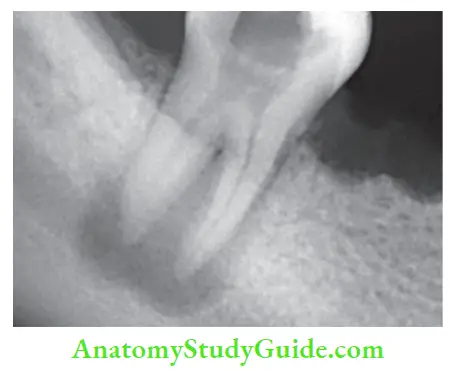
Cone Image Shift Technique:
A periapical film identifies the location of an object vertically and horizontally (mesiodistal) direction. However, the buccolingual position cannot be determined because fim is two-dimensional. To locate the buccolingual position, the same lingual opposite buccal (SLOB) rule is used.
The principle of the technique is that as the vertical or horizontal angulations of the X-ray tube head change, the object buccal or closest to the tube head moves to the opposite side of the radiograph when compared to the lingual object.
When two objects and a firm are in a fixed position and the tube head is moved, images of both objects move in opposite directions, the resultant radiograph shows a lingual object that moved in the same direction as the cone, and the buccal object moved in the opposite direction.
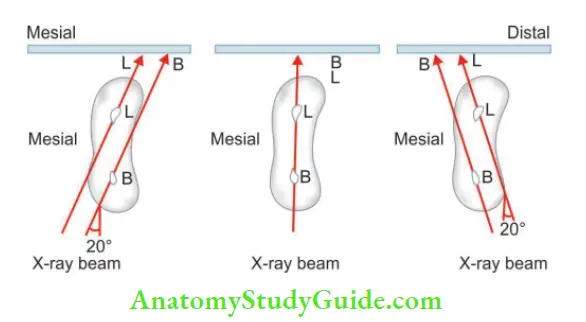
This is also known as the “SLOB” rule. To simplify the understanding of the SLOB rule, Walton gave an easy method. Place two figures directly in front of open eyes so that one finger is superimposed on the other.
By moving the head from one side to another, the relative position of the figures changes. The same effect is produced with two superimposed roots when the center beam is shifted.
Horizontal tube shift:
When tube head is moved mesially, the beam should be moved distally(from the mesial side) and vice versa.
Vertical tube shift:
It says the downward movement of the tube head requires the beam to be directed upward, and when the tube head is moved upward, the beam should be directed downwards.
Cone Image Shift Technique Advantages of “SLOB” Rule:
- Helps in the separation and identification of overlapping canals, for example, in maxillary premolars and mesial canals of mandibular molars
- Working length radiographs are better traced from the orifice to the apex by this technique
- Helps to locate the root resorption site in relation to the tooth
- Helps in locating the relationship of the canal to radiopaque margin, for example, the position of bur during access opening
- Helps in the identification of anatomic landmarks and pathosis
- Increases visualization of apical anatomy by moving anatomic landmarks such as zygomatic process or the impacted tooth
- Helps to identify the angle at which a particular radiograph was taken, even if the information was not recorded
- Helps to identify missed or calcified canals and canal curvature Helps to locate foreign bodies and anatomical landmarks in relation to the root apex such as the mandibular canal.
Cone Image Shift Technique Disadvantages of “SLOB” Rule:
- It results in the blurring of the object. The clearest radiograph is achieved by parallel technique, so when the central beam changes direction relative to the object and the film, the object becomes blurred
- It causes superimposition of the structures. Objects which have natural separation on parallel technique, with cone shift may move relative to each other and become superimposed.
- For example, in the case of maxillary molars, all three separate roots are visible on parallel radiographs, but an angled radiograph may move the palatal root over the distobuccal or mesiobuccal root and thus decreasing the ability to distinguish apices clearly.
Synonyms of cone image shift technique
- BOR (buccal object rule)
- SLOB
- BOMM (buccal object moves most)
- Tube shift technique
- Clark’s rule
- Walton projection
Advantages of Radiographs in Endodontics:
In endodontics, radiographs perform essential functions in three main areas, viz., diagnosis, treatment, and recall.
- Radiographs in Endodontics Diagnosis :
- Help to know the extent of caries, restoration, evidence of pulp capping or pulpotomy, etc.
- Useful to know the anatomy of the pulp cavity, the curvature of the canal, the number of roots and canals, variation in the root canal system, that is, the presence of fused or extra roots and canals, bifurcation or trifurcation in the canal system if present
- Help to know pulp conditions present inside the tooth like pulp stones, calcifications, internal resorption, etc.
- Provides information on orientation and depth of bur relative to the pulp cavity
- Help in knowing external resorption, thickening of the periodontal ligament, the extent of periapical, and alveolar bone destruction

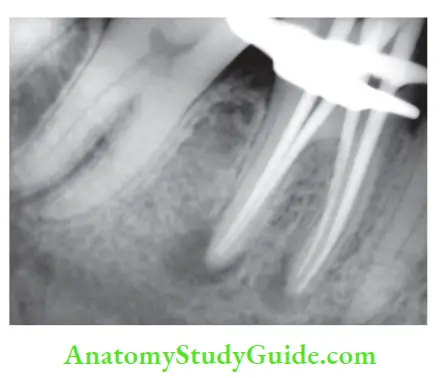
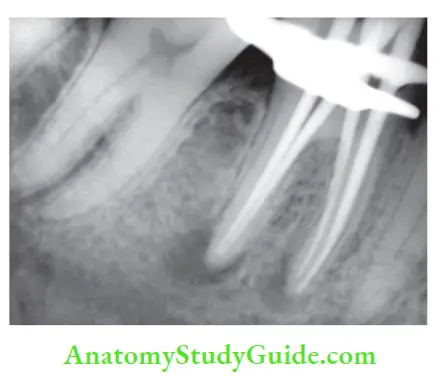
- Radiographs in Endodontics Treatment:
- Working length determination: In this, a radiograph is used to determine the distance from the reference point to the apex. By using different cone angulations, superimposed structures can be moved to give a clear image
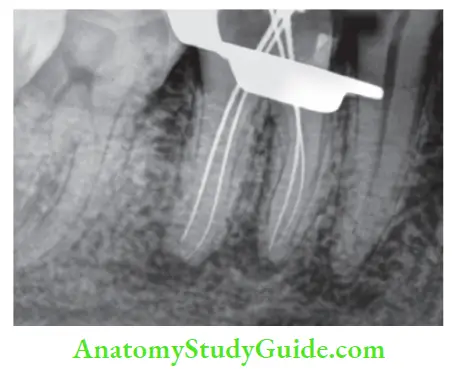
- Working length determination: In this, a radiograph is used to determine the distance from the reference point to the apex. By using different cone angulations, superimposed structures can be moved to give a clear image
-
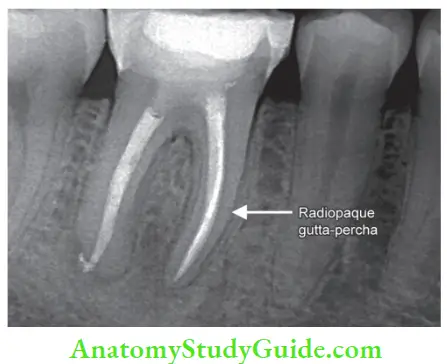
- Master cone radiographs: A master cone radiograph is used to evaluate the length and fit of the master gutta-percha cone.
- Obturation: Radiographs help to know the length, density, configuration, and quality of obturation.
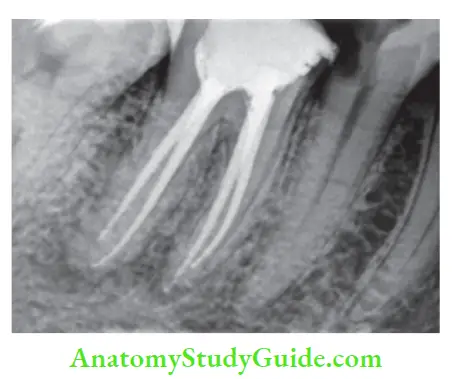
- Master cone radiographs: A master cone radiograph is used to evaluate the length and fit of the master gutta-percha cone.
- Radiographs in Endodontics Recall :
- Evaluate the post-treatment periapical status
- The presence and nature of the lesion (periapical, periodontal, or non-endodontic) that occurred after the treatment are best detected on radiographs
- Recall radiographs help to evaluate the success of treatment.
Disadvantages of Radiographs
- Radiograph represents a two-dimensional picture of a three-dimensional object
- For a hard tissue lesion to be evident on a radiograph, there should be at least a mineral loss of 6.6%
- Pathological changes in pulp are not visible in a radiograph
- Initial stages of periradicular disease produce no changes in the radiograph
- Radiographs do not help in the exact interpretation of the lesion, for example, radiographic picture of an abscess, inflammation, and granuloma is almost the same
- Misinterpretation of radiographs can lead to inaccurate diagnosis
- Radiographs can misinterpret anatomical structures like incisive and mental foramen with periapical lesions
- Chronic inflammatory lesions cannot be diffrentiated from healed fibrous scar tissue
- Buccolingual dimensions cannot be assessed from IOPA radiograph
To know the exact status of multirooted teeth, multiple radiographs are needed at different angles which further increases the radiation exposure.
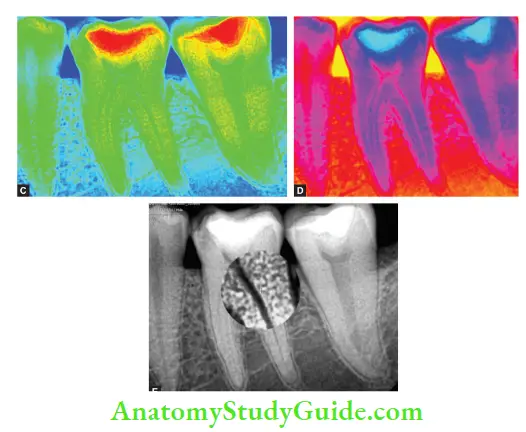
Digital Radiography
Digital imaging:
Digital imaging uses standard radiology techniques in which film is used to record the image, and then the final image is subjected to digital processing to produce the final result.
Digital radiography is obtained by two methods:
- Direct digital radiograph
- Video recording and digitization of conventional radiograph
Digital Dental Radiography:
Digital imaging systems require an electronic sensor or detector, an analog-to-digital converter, a computer, and a monitor or printer for the image of the components of the imaging system.
General Principles of Digital Imaging:
- A chemically produced radiograph is represented by data that is acquired in a parallel and continuous fashion known as analog
- Computers use binary (0 or 1) language, where information is usually handled in eight-character words called bytes
- Each character can be either 0 or 1, this results in 28 possible combinations (words) that is 256 words. These, digital dental images are limited to 256 shades of gray
- Digital images are made up of pixels (picture elements), each allocated a shade of gray
- The spatial resolution of a digital system is heavily dependent upon the number of pixels available per millimeter of image
CCD System:
CCD is a solid-state detector composed of an array of X-ray or light-sensitive phosphorus on a pure silicon chip. These phosphors convert incoming X-rays to a wavelength that matches the peak response of silicon.
Radiovisiography (RVG)
RVG is composed of three major parts:
- The radio part consists of a conventional X-ray unit and a tiny sensor to record the image. The sensor transmits information via a fiber-optic bundle to a miniature CCD
- The “Visio” portion of the system receives and stores incoming signals during exposure and converts them point by point into one of 256 discrete gray levels. It consists of a video monitor and a display processing unit.
- The “Graphy” part of the RVG unit consists of digital storage apparatus. It can be connected to various print out or mass storage devices for immediate or later viewing.
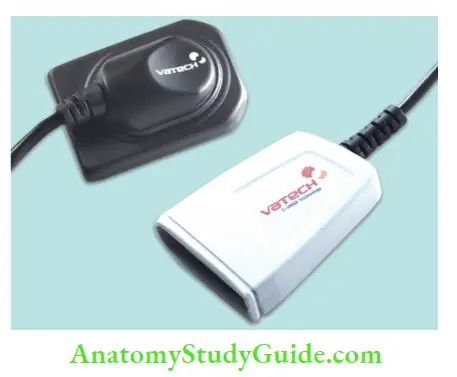
Radiovisiography Advantages:
- Low radiation dose
- Darkroom is not required as the instant image is viewed
- Image distortion from the bent radiographic film is eliminated
- The quality of the image is consistent
- Greater exposure latitude
- Elimination of hazards of film development
- Diagnostic capability is increased through digital
- enhancement and enlargement of specific areas for closer examination
- Contrast and resolution can be altered, and images can be viewed as greyscale or color
- Images are displayed instantly
- Full mouth radiographs can be made within seconds
- Storages and archiving of patient information
- Transfer of images between institutions (teleradiology)
- Infection control and toxic waste disposal problems associated with radiology are eliminated
Radiovisiography Disadvantages:
- Expensive
- Life expectancy of CCD is not fixed
- Solid state sensors when used for bitewing examination are small as compared to size-2 fim
- Large disk space required to store images
- Bulky sensor with cable attachment, which can make placement in mouth difficult
- Soft tissue imaging is not very nice
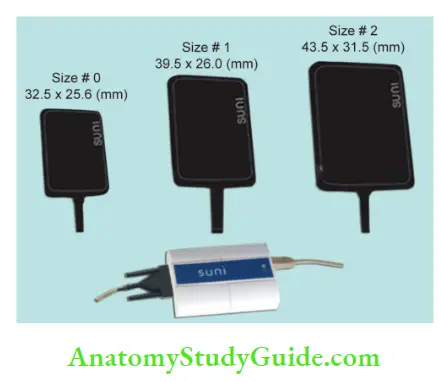
Phosphor Imaging System:
Imaging using a photostimulable phosphor can also be called as an indirect digital imaging technique. The image is captured on a phosphor plate as analog information and is converted into a digital format when the plate is processed.
Phosphor Imaging System Advantages:
- Low radiation dose (90% reduction)
- Almost instant image (20–30 s)
- Wide exposure latitude (almost impossible to burn out information)
- Same size receptor as films
- X-ray source can be remote from the PC
- Image manipulation facilities
Phosphor Imaging System Disadvantages
- Cost
- Storage of images (same as with CCD systems)
- The slight inconvenience of plastic bags
Cone-Beam Computed Tomography
Successful endodontic treatment depends on diagnostic imaging techniques to provide critical information about the teeth and their surrounding tissues. Though conventional radiography has been used for ages, modern techniques of imaging have also been successfully utilized.
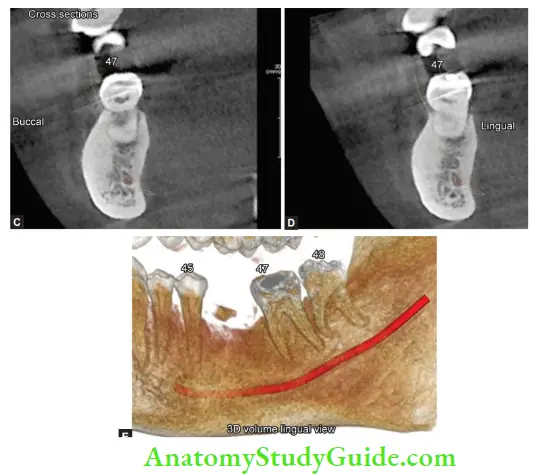
The introduction of maxillofacial cone-beam computed tomography (CBCT) in 1996 provided the first clinically practical technology demonstrating the application of 3D imaging for endodontic considerations. CBCT has a cone-shaped X-ray beam that captures a cylindrical or spherical volume of data, described as the field of view.
Here, a 3D volume of data is achieved with a single sweep of the scanner, using a simple and direct relationship between the beam source and sensor; the latter rotating 180–360° around the patient’s head. During the exposure sequence, hundreds of planar projection images are obtained from the field of view, in an arc of ≥180°.

Thus, we get accurate and immediate 3D radiographic images. To have better resolution of images, radiation exposure is increased by two to threefolds but CBCT systems utilize a pulsatile X-ray beam, therefore, actual patient exposure time can be very low as 2–10 s.

Radiation Dose Considerations:
For a significant comparison of radiation risk, radiation exposures are converted to an effective dose, measured in sieverts (Sv). The Sv is a large unit; so in maxillofacial imaging, milli-[10−3 mSv] or micro-[10−6 μSv] sieverts are used.
Advantages of CBCT
- CBCT overcomes the shortcomings of conventional radiography by producing 3D images that show accurate anatomy and spatial relationship of the pathosis and anatomical structures
- The clinician can choose and view slices of the volumetric data in all the planes, eliminating the anatomical noise
- CBCT voxels are isotropic, ensuring the geometrical accuracy of the images
- Reduced patient exposure to ionizing radiation and superior image quality of dental hard tissues
- Since, the X-ray source can be collimated so that the radiation is limited to the target area, further reducing the radiation exposure to the patient.
Limitations of CBCT:
- Spatial resolution and the contrast resolution of CBCT is lower than that of intraoral radiography
- Chances of radiographic artifacts are more with CBCT, for example, when a CBCT X-ray beam encounters a very high-density object, like enamel or metallic restorations, lower energy photons in the beam are absorbed by the structure. By this, the mean energy of the X-ray beam increases producing two types of artifacts that can reduce the diagnostic yield of the images
- The patient has to stay absolutely still because the movement can affect the sharpness of the final image during the scan.
Applications of CBCT in Endodontics:
Though there are many advantages of CBCT, due to the higher effective dose of ionizing radiation in comparison to conventional radiographs, in endodontics, CBCT should be used for the evaluation and management of complex endodontic conditions. It can be used for the following cases.
Preoperative Evaluation:
- Tooth morphology:
- CBCT helps in detecting the accurate degree of curvatures of roots of teeth, aberrations present in teeth, and anomalies such as dens invaginatus or tooth fusion. It can detect MB2 better than 2D conventional radiography.
- Dental periapical pathosis and apical periodontitis:
- CBCT gives more accurate images for the identification of apical periodontitis. It can demonstrate bone defects of the cancellous bone and cortical bone separately. It can also tell invasion of lesions into the maxillary sinus, thickening of the sinus membrane, and missed canals
- Diagnosis of different types of root resorption:
- CBCT helps in the detection of small lesions, localizing and differentiation of the external root resorption from external cervical resorption, internal resorption, and other conditions
- Root fracture:
- CBCT provides an accurate assessment of dentoalveolar trauma, especially root fractures as compared to conventional radiography
- In surgical endodontics:
- It tells the accurate spatial relationship of the target tooth to adjacent anatomical structures like the inferior alveolar nerve, mental foramen, and maxillary sinuses
- Assessment of traumatic dental injuries:
- It helps in the accurate detection of horizontal root fractures, the degree and direction of displacement related to luxation injuries than multiple periapical radiographs.
- Postoperative Assessment:
- It helps in monitoring the healing of apical lesions accurately as compared to conventional radiography
- CBCT is used to initial and subsequent monitoring of the integrity of root canal obturation
- CBCT helps in determining the precise nature of perforation and healing on subsequent treatment.
Leave a Reply